Abstract
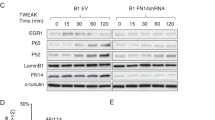
Prostate cancer metastases primarily localize in the bone where they induce a unique osteoblastic response. Elevated Notch activity is associated with high-grade disease and metastasis. To address how Notch affects prostate cancer bone lesions, we manipulated Notch expression in mouse tibia xenografts and monitored tumor growth, lesion phenotype, and the bone microenvironment. Prostate cancer cell lines that induce mixed osteoblastic lesions in bone expressed 5–6 times more Notch3, than tumor cells that produce osteolytic lesions. Expression of active Notch3 (NICD3) in osteolytic tumors reduced osteolytic lesion area and enhanced osteoblastogenesis, while loss of Notch3 in osteoblastic tumors enhanced osteolytic lesion area and decreased osteoblastogensis. This was accompanied by a respective decrease and increase in the number of active osteoclasts and osteoblasts at the tumor–bone interface, without any effect on tumor proliferation. Conditioned medium from NICD3-expressing cells enhanced osteoblast differentiation and proliferation in vitro, while simultaneously inhibiting osteoclastogenesis. MMP-3 was specifically elevated and secreted by NICD3-expressing tumors, and inhibition of MMP-3 rescued the NICD3-induced osteoblastic phenotypes. Clinical osteoblastic bone metastasis samples had higher levels of Notch3 and MMP-3 compared with patient matched visceral metastases or osteolytic metastasis samples. We identified a Notch3–MMP-3 axis in human prostate cancer bone metastases that contributes to osteoblastic lesion formation by blocking osteoclast differentiation, while also contributing to osteoblastogenesis. These studies define a new role for Notch3 in manipulating the tumor microenvironment in bone metastases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Ganguly SS, Li X, Miranti CK. The host microenvironment influences prostate cancer invasion, systemic spread, bone colonization, and osteoblastic metastasis. Front Oncol. 2014;4:364.
Siegel RL, MK, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29.
Karayi MK, Markham AF. Molecular biology of prostate cancer. Prostate Cancer Prostatic Dis. 2004;7:6–20.
Roudier MP, Morrissey C, True LD, Higano CS, Vessella RL, Ott SM. Histopathological assessment of prostate cancer bone osteoblastic metastases. J Urol. 2008;180:1154–60.
Sottnik JL, Keller ET. Understanding and targeting osteoclastic activity in prostate cancer bone metastases. Curr Mol Med. 2013;13:626–39.
Jin JK, Dayyani F, Gallick GE. Steps in prostate cancer progression that lead to bone metastasis. Int J Cancer. 2011;128:2545–61.
Frank SB, Miranti CK. Disruption of prostate epithelial differentiation pathways and prostate cancer development. Front Oncol. 2013;3:273.
Kopan R, Ilagan MX. The canonical Notch signaling pathway: unfolding the activation mechanism. Cell. 2009;137:216–33.
Zanotti S, Canalis E. Notch and the skeleton. Mol Cell Biol. 2010;30:886–96.
Wang XD, Shou J, Wong P, French DM, Gao WQ. Notch1-expressing cells are indispensable for prostatic branching morphogenesis during development and re-growth following castration and androgen replacement. J Biol Chem. 2004;279:24733–44.
Kwon OJ, Valdez JM, Zhang L, Zhang B, Wei X, Su Q, et al. Increased Notch signalling inhibits anoikis and stimulates proliferation of prostate luminal epithelial cells. Nat Commun. 2014;5:4416.
Bin Hafeez B, Adhami VM, Asim M, Siddiqui IA, Bhat KM, Zhong W, et al. Targeted knockdown of Notch1 inhibits invasion of human prostate cancer cells concomitant with inhibition of matrix metalloproteinase-9 and urokinase plasminogen activator. Clin Cancer Res. 2009;15:452–9.
Ye QF, Zhang YC, Peng XQ, Long Z, Ming YZ, He LY. Silencing Notch-1 induces apoptosis and increases the chemosensitivity of prostate cancer cells to docetaxel through Bcl-2 and Bax. Oncol Lett. 2012;3:879–84.
Frank SB, Berger PL, Ljungman M, Miranti CK. Human prostate luminal cell differentiation requires NOTCH3 induction by p38-MAPK and MYC. J Cell Sci. 2017;130:1952–64.
Zhang S, Chung WC, Wu G, Egan SE, Xu K. Tumor-suppressive activity of Lunatic Fringe in prostate through differential modulation of Notch receptor activation. Neoplasia. 2014;16:158–67.
Long Q, Johnson BA, Osunkoya AO, Lai YH, Zhou W, Abramovitz M, et al. Protein-coding and microRNA biomarkers of recurrence of prostate cancer following radical prostatectomy. Am J Pathol. 2011;179:46–54.
Ross AE, Marchionni L, Vuica-Ross M, Cheadle C, Fan J, Berman DM, et al. Gene expression pathways of high grade localized prostate cancer. Prostate. 2011;71:1568–77.
Danza G, Di Serio C, Ambrosio MR, Sturli N, Lonetto G, Rosati F, et al. Notch3 is activated by chronic hypoxia and contributes to the progression of human prostate cancer. Int J Cancer. 2013;133:2577–86.
Cui J, Wang Y, Dong B, Qin L, Wang C, Zhou P, et al. Pharmacological inhibition of the Notch pathway enhances the efficacy of androgen deprivation therapy for prostate cancer. Int J Cancer. 2018;143(3):645–56.
Cui D, Dai J, Keller JM, Mizokami A, Xia S, Keller ET. Notch pathway inhibition using PF-03084014, a gamma-secretase inhibitor (GSI), enhances the antitumor effect of docetaxel in prostate cancer. Clin Cancer Res. 2015;21:4619–29.
Zhang Z, Wang H, Ikeda S, Fahey F, Bielenberg D, Smits P, et al. Notch3 in human breast cancer cell lines regulates osteoblast-cancer cell interactions and osteolytic bone metastasis. Am J Pathol. 2010;177:1459–69.
Sethi N, Dai X, Winter CG, Kang Y. Tumor-derived JAGGED1 promotes osteolytic bone metastasis of breast cancer by engaging notch signaling in bone cells. Cancer Cell. 2011;19:192–205.
Gong Y, Chippada-Venkata UD, Oh WK. Roles of matrix metalloproteinases and their natural inhibitors in prostate cancer progression. Cancers. 2014;6:1298–327.
Srivastava P, Kapoor R, Mittal RD. Impact of MMP-3 and TIMP-3 gene polymorphisms on prostate cancer susceptibility in North Indian cohort. Gene. 2013;530:273–7.
Jung KNL, Lein M, Priem F, Schnorr D, Loening SA. Matrix metalloproteinases 1 and 3, tissue inhibitor of metalloproteinase-1 and the complex of metalloproteinase-1/tissue inhibitor in plasma of patients with prostate cancer. Int J Cancer. 1997;74:220–3.
Hong MH WH, Jin CH, Pike jw. The inhibitory effect of interleukin-10 on mouse osteoclast formation involves novel tyrosine-phosphorylated proteins. J Bone Miner Res. 2000;15:911–8.
Evans KE, Fox SW. Interleukin-10 inhibits osteoclastogenesis by reducing NFATc1 expression and preventing its translocation to the nucleus. BMC Cell Biol. 2007;8:4.
Boyce BF, Xing L. Biology of RANK, RANKL, and osteoprotegerin. Arthritis Res Ther. 2007;9(Suppl 1):S1.
Hudson RS, Yi M, Esposito D, Watkins SK, Hurwitz AA, Yfantis HG, et al. MicroRNA-1 is a candidate tumor suppressor and prognostic marker in human prostate cancer. Nucleic Acids Res. 2012;40:3689–703.
Gilkes DM. Implications of hypoxia in breast cancer metastasis to bone. Int J Mol Sci. 2016;17:pii: E1669.
Keller ET, Brown J. Prostate cancer bone metastases promote both osteolytic and osteoblastic activity. J Cell Biochem. 2004;91:718–29.
Frieling JS, Shay G, Izumi V, Aherne ST, Saul RG, Budzevich M, et al. Matrix metalloproteinase processing of PTHrP yields a selective regulator of osteogenesis, PTHrP1-17. Oncogene. 2017;36:4498–507.
Ibrahim T, Flamini E, Mercatali L, Sacanna E, Serra P, Amadori D. Pathogenesis of osteoblastic bone metastases from prostate cancer. Cancer. 2010;116:1406–18.
Garcia AJ, Tom C, Guemes M, Polanco G, Mayorga ME, Wend K, et al. ERalpha signaling regulates MMP3 expression to induce FasL cleavage and osteoclast apoptosis. J Bone Miner Res. 2013;28:283–90.
Mehner C, Nassar A, Bamlet WR, Radisky ES, Radisky DC, Miller E. Tumor cell expression of MMP3 as a prognostic factor for poor survival in pancreatic, pulmonary, and mammary carcinoma. Genes Cancer. 2015;6:480–9.
Huang Jie-Feng, W-XD, Chen Jun-Jie. Elevated expression of matrix metalloproteinase-3 in human osteosarcoma and its association with tumor metastasis. JBOUN. 2016;21:235–43.
Furic L, Rong L, Larsson O, Koumakpayi IH, Yoshida K, Brueschke A, et al. eIF4E phosphorylation promotes tumorigenesis and is associated with prostate cancer progression. Proc Natl Acad Sci USA. 2010;107:14134–9.
Lynch CC, Hikosaka A, Acuff HB, Martin MD, Kawai N, Singh RK, et al. MMP-7 promotes prostate cancer-induced osteolysis via the solubilization of RANKL. Cancer Cell. 2005;7:485–96.
Sasaki K, Takagi M, Konttinen YT, Sasaki A, Tamaki Y, Ogino T, et al. Upregulation of matrix metalloproteinase (MMP)-1 and its activator MMP-3 of human osteoblast by uniaxial cyclic stimulation. J Biomed Mater Res B Appl Biomater. 2007;80:491–8.
Kusano K, Miyaura C, Inada M, Tamura T, Ito A, Nagase H, et al. Regulation of matrix metalloproteinases (MMP-2, -3, -9, and -13) by interleukin-1 and interleukin-6 in mouse calvaria: association of MMP induction with bone resorption. Endocrinology. 1998;139:1338–45.
Ally MM, Hodkinson B, Meyer PW, Musenge E, Tikly M, Anderson R. Serum matrix metalloproteinase-3 in comparison with acute phase proteins as a marker of disease activity and radiographic damage in early rheumatoid arthritis. Mediat Inflamm. 2013;2013:183653.
Imamura Y, Sadar MD. Androgen receptor targeted therapies in castration-resistant prostate cancer: bench to clinic. Int J Urol. 2016;23:654–65.
Su Q, Xin L. Notch signaling in prostate cancer: refining a therapeutic opportunity. Histol Histopathol. 2016;31:149–57.
Thalmann GN, Sikes RA, Wu TT, Degeorges A, Chang SM, Ozen M, et al. LNCaP progression model of human prostate cancer: androgen-independence and osseous metastasis. Prostate. 2000;44:91–103. Jul 1;44(2).
Frank SB, Schulz VV, Miranti CK. A streamlined method for the design and cloning of shRNAs into an optimized Dox-inducible lentiviral vector. BMC Biotechnol 2017;17:24.
Yu XAJ, Chun JH, Friedman AD, Heimfeld S, Cheng L, Civin CI. HES1 inhibits cycling of hematopoietic progenitor cells via DNA binding. Stem Cells. 2006;24:876–88.
Dang LYK, Wang M, Gaiano N. Notch3 signaling promotes radial glial/progenitor character in the mammalian telencephalon. Dev Neurosci. 2006;28:58–69.
Campeau ERV, Rodier F, Smith CL, Rahmberg BL, Fuss JO, Campisi J, et al. A versatile viral system for expression and depletion of proteins in mammalian cells. PLoS ONE. 2009;4:e6529.
Li X, Sterling JA, Fan KH, Vessella RL, Shyr Y, Hayward SW, et al. Loss of TGF-beta responsiveness in prostate stromal cells alters chemokine levels and facilitates the development of mixed osteoblastic/osteolytic bone lesions. Mol Cancer Res. 2012;10:494–503.
Edick MJ, Tesfay L, Lamb LE, Knudsen BS, Miranti CK. Inhibition of integrin-mediated crosstalk with epidermal growth factor receptor/Erk or Src signaling pathways in autophagic prostate epithelial cells induces caspase-independent death. Mol Biol cell 2007;18:2481–90.
Acknowledgements
Funding for this project was provided by a DOD Postdoctoral Fellowship W81XWH-16-1-0136 (SSG), DOD W81XWH-14-1-0479 (SBF, LT, CKM), University of Arizona Cancer Center (UACC) NIH/NCI P30CA023074 (KS, CKM), the Van Andel Research Institute (VARI) (GH, XL), and the University of Arizona (CKM). The TMA obtained from the Prostate Cancer Biorepository Network (PCBN) was supported by funds from the DOD Prostate Cancer Research Program: W81XWH-14-2-0182, W81XWH-14-2-0183, W81XWH-14-2-0185, W81XWH-14-2-0186, and W81XWH-15-2-0062. We wish to thank the following: Dr Denise Roe, Director of Biostatistics Shared Resource at UACC for biostatistics support; Dr Chunyan Liu at Ventana Medical Services, Oro Valley, AZ for her pathology services; Dr Colm Morrissey in the Department of Urology, University of Washington, Seattle WA, for his assistance with providing pathological assessment of bone metastasis lesions in the PCBN TMA. Alexandra VanderArk, Veronique Schulz, and Ghada Y.T Mohsen at Van Andel Research Institute for their technical expertise; Zachary Madaj for statistical analysis expertise; Lisa Turner, Kristin Feenstra, and Bree Berghuis of the VARI Pathology and Biorepository Core for their pathology and Aperio expertise; Su Yanli and Staff of the VARI Vivarium and Transgenics core for technical assistance with animal experiments; David Nadziejka for technical editing of the paper; Jeanie Wedberg and Michelle Minard at the Van Andel Institute and David Alvarado at University of Arizona for their administrative support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ganguly, S.S., Hostetter, G., Tang, L. et al. Notch3 promotes prostate cancer-induced bone lesion development via MMP-3. Oncogene 39, 204–218 (2020). https://doi.org/10.1038/s41388-019-0977-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41388-019-0977-1
This article is cited by
-
Distinct DNA methylation patterns associated with treatment resistance in metastatic castration resistant prostate cancer
Scientific Reports (2021)
-
Autophagy provides a conceptual therapeutic framework for bone metastasis from prostate cancer
Cell Death & Disease (2021)