Abstract
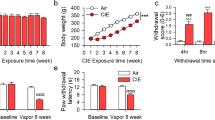
The role of lysophosphatidic acid (LPA) signaling in psychiatric disorders and drug abuse is significant. LPA receptors are widely expressed in the central nervous system, including the lateral habenula (LHb). Recent studies suggest that LHb is involved in a negative emotional state during alcohol withdrawal, which can lead to relapse. The current study examines the role of LHb LPA signaling in the negative affective state associated with alcohol withdrawal. Adult male Long-Evans rats were trained to consume either alcohol or water for eight weeks. At 48 h of withdrawal, alcohol-drinking rats showed anxiety- and depression-like symptoms, along with a significant increase in LPA signaling and related neuronal activation molecules, including autotaxin (ATX, Enpp2), LPA receptor 1/3 (LPA1/3), βCaMKII, and c-Fos. However, there was a decrease in lipid phosphate phosphatase-related protein type 4 (LPPR4) in the LHb. Intra-LHb infusion of the LPA1/3 receptor antagonist ki-16425 or PKC-γ inhibitor Go-6983 reduced the abnormal behaviors and elevated relapse-like ethanol drinking. It also normalized high LPA1/3 receptors and enhanced AMPA GluA1 phosphorylation in Ser831 and GluA1/GluA2 ratio. Conversely, selective activation of LPA1/3 receptors by intra-LHb infusion of 18:1 LPA induced negative affective states and upregulated βCaMKII-AMPA receptor phosphorylation in Naive rats, which were reversed by pretreatment with intra-LHb Go-6983. Our findings suggest that disturbances in LPA signaling contribute to adverse affective disorders during alcohol withdrawal, likely through PKC-γ/βCaMKII-linked glutamate signaling. Targeting LPA may therefore be beneficial for individuals suffering from alcohol use disorders.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 13 print issues and online access
$259.00 per year
only $19.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Koob GF, Volkow ND. Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry. 2016;3:760–73.
Koob GF. Neurobiological substrates for the dark side of compulsivity in addiction. Neuropharmacology 2009;56:18–31.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacol. 2010;35:217–38.
McHugh RK, Weiss RD Alcohol use disorder and depressive disorders. Alcohol Res Curr Rev. 2019;40. https://doi.org/10.35946/arcr.v40.1.01.
Rossetti ZL, Hmaidan Y, Gessa GL. Marked inhibition of mesolimbic dopamine release: a common feature of ethanol, morphine, cocaine and amphetamine abstinence in rats. Eur J Pharmacol. 1992;221:227–34.
Diana M, Pistis M, Carboni S, Gessa GL, Rossetti ZL. Profound decrement of mesolimbic dopaminergic neuronal activity during ethanol withdrawal syndrome in rats: electrophysiological and biochemical evidence. Proc Natl Acad Sci USA. 1993;90:7966–9.
Matsumoto M, Hikosaka O. Lateral habenula as a source of negative reward signals in dopamine neurons. Nature. 2007;447:1111–5.
Shabel SJ, Proulx CD, Trias A, Murphy RT, Malinow R. Input to the lateral habenula from the basal ganglia is excitatory, aversive, and suppressed by serotonin. Neuron. 2012;74:475–81.
Mondoloni S, Mameli M, Congiu M. Reward and aversion encoding in the lateral habenula for innate and learned behaviours. Transl Psychiatry. 2022;12:3.
Lammel S, Lim BK, Ran C, Huang KW, Betley MJ, Tye KM, et al. Input-specific control of reward and aversion in the ventral tegmental area. Nature 2012;491:212–7.
Stamatakis AM, Stuber GD. Activation of lateral habenula inputs to the ventral midbrain promotes behavioral avoidance. Nat Neurosci. 2012;15:1105–7.
Li J, Zuo W, Fu R, Xie G, Kaur A, Bekker A, et al. High frequency electrical stimulation of lateral habenula reduces voluntary ethanol consumption in rats. Int J Neuropsychopharmacol. 2016;19:pyw050.
Li J, Kang S, Fu R, Wu L, Wu W, Liu H, et al. Inhibition of AMPA receptor and CaMKII activity in the lateral habenula reduces depressive-like behavior and alcohol intake in rats. Neuropharmacology. 2017;126:108–20.
Li J, Chen P, Han X, Zuo W, Mei Q, Bian EY, et al. Differences between male and female rats in alcohol drinking, negative affects and neuronal activity after acute and prolonged abstinence. Int J Physiol Pathophysiol Pharmacol. 2019;11:163–76.
Kang S, Li J, Zuo W, Fu R, Gregor D, Krnjevic K, et al. Ethanol withdrawal drives anxiety-related behaviors by reducing m-type potassium channel activity in the lateral habenula. Neuropsychopharmacol. 2017;42:1813–24.
Sheth C, Furlong TM, Keefe KA, Taha SA. The lateral hypothalamus to lateral habenula projection, but not the ventral pallidum to lateral habenula projection, regulates voluntary ethanol consumption. Behav Brain Res. 2017;328:195–208.
Fu R, Tang Y, Li W, Ren Z, Li D, Zheng J, et al. Endocannabinoid signaling in the lateral habenula regulates pain and alcohol consumption. Transl psychiatry. 2021;11:220.
Shor C, Zuo W, Eloy JD, Ye JH The emerging role of LHb CaMKII in the comorbidity of depressive and alcohol use disorders. Int J Mol Sci. 2020;21:8123.
Shah A, Zuo W, Kang S, Li J, Fu R, Zhang H, et al. The lateral habenula and alcohol: role of glutamate and M-type potassium channels. Pharmacol Biochem Behav. 2017;162:94–102.
Sanchis-Segura C, Borchardt T, Vengeliene V, Zghoul T, Bachteler D, Gass P, et al. Involvement of the AMPA receptor GluR-C subunit in alcohol-seeking behavior and relapse. J Neurosci. 2006;26:1231–8.
Gass JT, Olive MF. Glutamatergic substrates of drug addiction and alcoholism. Biochem Pharmacol. 2008;75:218–65.
Salling MC, Faccidomo SP, Li C, Psilos K, Galunas C, Spanos M, et al. Moderate alcohol drinking and the amygdala proteome: identification and validation of calcium/calmodulin dependent kinase II and AMPA receptor activity as novel molecular mechanisms of the positive reinforcing effects of alcohol. Biol Psychiatry. 2016;79:430–42.
Cannady R, Fisher KR, Graham C, Crayle J, Besheer J, Hodge CW. Potentiation of amygdala AMPA receptor activity selectively promotes escalated alcohol self-administration in a CaMKII-dependent manner. Addict Biol. 2017;22:652–64.
Nimitvilai S, Lopez MF, Mulholland PJ, Woodward JJ. Chronic intermittent ethanol exposure enhances the excitability and synaptic plasticity of lateral orbitofrontal cortex neurons and induces a tolerance to the acute inhibitory actions of ethanol. Neuropsychopharmacol. 2016;41:1112–27.
Martínez-Rivera A, Hao J, Tropea TF, Giordano TP, Kosovsky M, Rice RC, et al. Enhancing VTA Ca(v)1.3 L-type Ca(2+) channel activity promotes cocaine and mood-related behaviors via overlapping AMPA receptor mechanisms in the nucleus accumbens. Mol Psychiatry. 2017;22:1735–45.
Schneider M, Levant B, Reichel M, Gulbins E, Kornhuber J, Müller CP. Lipids in psychiatric disorders and preventive medicine. Neurosci Biobehav Rev. 2017;76:336–62.
Yung YC, Stoddard NC, Chun J. LPA receptor signaling: pharmacology, physiology, and pathophysiology. J lipid Res. 2014;55:1192–214.
Yung YC, Stoddard NC, Mirendil H, Chun J. Lysophosphatidic acid signaling in the nervous system. Neuron 2015;85:669–82.
Choi JW, Herr DR, Noguchi K, Yung YC, Lee CW, Mutoh T, et al. LPA receptors: subtypes and biological actions. Annu Rev Pharmacol Toxicol. 2010;50:157–86.
Thalman C, Horta G, Qiao L, Endle H, Tegeder I, Cheng H, et al. Synaptic phospholipids as a new target for cortical hyperexcitability and E/I balance in psychiatric disorders. Mol Psychiatry. 2018;23:1699–710.
Mirendil H, Thomas EA, De Loera C, Okada K, Inomata Y, Chun J. LPA signaling initiates schizophrenia-like brain and behavioral changes in a mouse model of prenatal brain hemorrhage. Transl Psychiatry. 2015;5:e541.
Flores-López M, García-Marchena N, Araos P, Requena-Ocaña N, Porras-Perales O, Torres-Galván S, et al. Sex differences in plasma lysophosphatidic acid species in patients with alcohol and cocaine use disorders. Brain Sci. 2022;12:588.
Orio L, Pavón FJ, Blanco E, Serrano A, Araos P, Pedraz M, et al. Lipid transmitter signaling as a new target for treatment of cocaine addiction: new roles for acylethanolamides and lysophosphatidic acid. Curr Pharm Des. 2013;19:7036–49.
Flores-López M, García-Marchena N, Pavon FJ, Lara E, Porras-Perales O, Araos P, et al. Plasma concentrations of lysophosphatidic acid and autotaxin in abstinent patients with alcohol use disorder and comorbid liver disease. Biomedicines. 2021;9(9):1207.
García-Marchena N, Pizarro N, Pavón FJ, Martínez-Huélamo M, Flores-López M, Requena-Ocaña N, et al. Potential association of plasma lysophosphatidic acid (LPA) species with cognitive impairment in abstinent alcohol use disorders outpatients. Sci Rep. 2020;10:17163.
Sánchez-Marín L, Ladrón de Guevara-Miranda D, Mañas-Padilla MC, Alén F, Moreno-Fernández RD, Díaz-Navarro C, et al. Systemic blockade of LPA(1/3) lysophosphatidic acid receptors by ki16425 modulates the effects of ethanol on the brain and behavior. Neuropharmacology. 2018;133:189–201.
Castilla-Ortega E, Escuredo L, Bilbao A, Pedraza C, Orio L, Estivill-Torrús G, et al. 1-Oleoyl lysophosphatidic acid: a new mediator of emotional behavior in rats. PloS one. 2014;9:e85348.
Yamada M, Tsukagoshi M, Hashimoto T, Oka J, Saitoh A, Yamada M. Lysophosphatidic acid induces anxiety-like behavior via its receptors in mice. J Neural Transm (Vienna, Austria: 1996). 2015;122:487–94.
Birgbauer E. Lysophosphatidic acid signalling in nervous system development and function. Neuromol Med. 2021;23:68–85.
Pilpel Y, Segal M. The role of LPA1 in formation of synapses among cultured hippocampal neurons. J Neurochem. 2006;97:1379–92.
Moreno-Fernández RD, Rosell-Valle C, Bacq A, Zanoletti O, Cifuentes M, Pérez-Martín M, et al. LPA(1) receptor and chronic stress: effects on behaviour and the genes involved in the hippocampal excitatory/inhibitory balance. Neuropharmacology. 2020;164:107896.
González de San Román E, Manuel I, Ledent C, Chun J, Rodríguez de Fonseca F, Estivill-Torrús G, et al. CB(1) and LPA(1) receptors relationship in the mouse central nervous system. Front Mol Neurosci. 2019;12:223.
Hashikawa Y, Hashikawa K, Rossi MA, Basiri ML, Liu Y, Johnston NL, et al. Transcriptional and spatial resolution of cell types in the mammalian habenula. Neuron. 2020;106:743–58.e5.
Dubin AE, Bahnson T, Weiner JA, Fukushima N, Chun J. Lysophosphatidic acid stimulates neurotransmitter-like conductance changes that precede GABA and L-glutamate in early, presumptive cortical neuroblasts. J Neurosci. 1999;19:1371–81.
García-Morales V, Montero F, González-Forero D, Rodríguez-Bey G, Gómez-Pérez L, Medialdea-Wandossell MJ, et al. Membrane-derived phospholipids control synaptic neurotransmission and plasticity. PLoS Biol. 2015;13:e1002153.
Roza C, Campos-Sandoval JA, Gómez-García MC, Peñalver A, Márquez J. Lysophosphatidic acid and glutamatergic transmission. Front Mol Neurosci. 2019;12:138.
Newton PM, Ron D. Protein kinase C and alcohol addiction. Pharmacol Res. 2007;55:570–7.
Lu WY, Xiong ZG, Lei S, Orser BA, Dudek E, Browning MD, et al. G-protein-coupled receptors act via protein kinase C and Src to regulate NMDA receptors. Nat Neurosci. 1999;2:331–8.
Alexander KA, Cimler BM, Meier KE, Storm DR. Regulation of calmodulin binding to P-57. A neurospecific calmodulin binding protein. J Biol Chem. 1987;262:6108–13.
Wang JH, Kelly PT. Postsynaptic injection of CA2+/CaM induces synaptic potentiation requiring CaMKII and PKC activity. Neuron 1995;15:443–52.
Fu R, Zuo W, Shiwalkar N, Mei Q, Fan Q, Chen X, et al. Alcohol withdrawal drives depressive behaviors by activating neurons in the rostromedial tegmental nucleus. Neuropsychopharmacol. 2019;44:1464–75.
Fu R, Zuo W, Gregor D, Li J, Grech D, Ye JH. Pharmacological manipulation of the rostromedial tegmental nucleus changes voluntary and operant ethanol self-administration in rats. Alcohol, Clin Exp Res. 2016;40:572–82.
Slattery DA, Cryan JF. Using the rat forced swim test to assess antidepressant-like activity in rodents. Nat Protoc. 2012;7:1009–14.
Mezadri TJ, Batista GM, Portes AC, Marino-Neto J, Lino-de-Oliveira C. Repeated rat-forced swim test: reducing the number of animals to evaluate gradual effects of antidepressants. J Neurosci Methods. 2011;195:200–5.
Zuo W, Wu L, Mei Q, Zuo Q, Zhou Z, Fu R, et al. Adaptation in 5-HT(2) receptors-CaMKII signaling in lateral habenula underlies increased nociceptive-sensitivity in ethanol-withdrawn rats. Neuropharmacology. 2019;158:107747.
Li W, Ren Z, Tang Y, Fu Y, Sun S, Ding R, et al. Rostromedial tegmental nucleus nociceptin/orphanin FQ (N/OFQ) signaling regulates anxiety- and depression-like behaviors in alcohol withdrawn rats. Neuropsychopharmacology. 2022. https://doi.org/10.1038/s41386-022-01482-3.
Ma L, Matsumoto M, Xie W, Inoue M, Ueda H. Evidence for lysophosphatidic acid 1 receptor signaling in the early phase of neuropathic pain mechanisms in experiments using Ki-16425, a lysophosphatidic acid 1 receptor antagonist. J Neurochem. 2009;109:603–10.
Fu R, Mei Q, Shiwalkar N, Zuo W, Zhang H, Gregor D, et al. Anxiety during alcohol withdrawal involves 5-HT2C receptors and M-channels in the lateral habenula. Neuropharmacology. 2020;163:107863.
Gregor DM, Zuo W, Fu R, Bekker A, Ye JH. Elevation of transient receptor potential vanilloid 1 function in the lateral habenula mediates aversive behaviors in alcohol-withdrawn rats. Anesthesiology 2019;130:592–608.
Donaldson JG. Immunofluorescence staining. Curr Protoc cell Biol. 2015;69:4.3.1–7.
Jensen EC. Quantitative analysis of histological staining and fluorescence using ImageJ. Anat Rec (Hoboken, NJ: 2007). 2013;296:378–81.
Costes SV, Daelemans D, Cho EH, Dobbin Z, Pavlakis G, Lockett S. Automatic and quantitative measurement of protein-protein colocalization in live cells. Biophysical J. 2004;86:3993–4003.
Sando JJ, Chertihin OI. Activation of protein kinase C by lysophosphatidic acid: dependence on composition of phospholipid vesicles. Biochemical J. 1996;317:583–8.
Rosoff DB, Charlet K, Jung J, Lee J, Lohoff FW Lipid profile dysregulation predicts alcohol withdrawal symptom severity in individuals with alcohol use disorder. Alcohol (Fayetteville, NY). 2020;86:93–101.
Li W, Zuo W, Wu W, Zuo QK, Fu R, Wu L, et al. Activation of glycine receptors in the lateral habenula rescues anxiety- and depression-like behaviors associated with alcohol withdrawal and reduces alcohol intake in rats. Neuropharmacology. 2019;157:107688.
Schneider P, Petzold S, Sommer A, Nitsch R, Schwegler H, Vogt J, et al. Altered synaptic phospholipid signaling in PRG-1 deficient mice induces exploratory behavior and motor hyperactivity resembling psychiatric disorders. Behav Brain Res. 2018;336:1–7.
Liu X, Huai J, Endle H, Schlüter L, Fan W, Li Y, et al. PRG-1 regulates synaptic plasticity via intracellular PP2A/β1-integrin signaling. Dev Cell. 2016;38:275–90.
Vogt J, Yang JW, Mobascher A, Cheng J, Li Y, Liu X, et al. Molecular cause and functional impact of altered synaptic lipid signaling due to a prg-1 gene SNP. EMBO Mol Med. 2016;8:25–38.
Trimbuch T, Beed P, Vogt J, Schuchmann S, Maier N, Kintscher M, et al. Synaptic PRG-1 modulates excitatory transmission via lipid phosphate-mediated signaling. Cell. 2009;138:1222–35.
Unichenko P, Kirischuk S, Yang JW, Baumgart J, Roskoden T, Schneider P, et al. Plasticity-related gene 1 affects mouse barrel cortex function via strengthening of glutamatergic thalamocortical transmission. Cereb Cortex (N. Y, NY: 1991). 2016;26:3260–72.
Pedraza C, Sánchez-López J, Castilla-Ortega E, Rosell-Valle C, Zambrana-Infantes E, García-Fernández M, et al. Fear extinction and acute stress reactivity reveal a role of LPA(1) receptor in regulating emotional-like behaviors. Brain Struct Funct. 2014;219:1659–72.
Hama K, Aoki J. LPA(3), a unique G protein-coupled receptor for lysophosphatidic acid. Prog Lipid Res. 2010;49:335–42.
Aoki J, Inoue A, Okudaira S. Two pathways for lysophosphatidic acid production. Biochimica et Biophys Acta. 2008;1781:513–8.
Shah BH, Catt KJ. Roles of LPA3 and COX-2 in implantation. Trends Endocrinol Metab. 2005;16:397–9.
Solís KH, Romero-Ávila MT, Guzmán-Silva A, García-Sáinz JA The LPA(3) receptor: regulation and activation of signaling pathways. Int J Mol Sci. 2021;22:6704.
Tabbai S, Moreno-Fernández RD, Zambrana-Infantes E, Nieto-Quero A, Chun J, García-Fernández M, et al. Effects of the LPA(1) receptor deficiency and stress on the hippocampal LPA species in mice. Front Mol Neurosci. 2019;12:146.
Moreno-Fernández RD, Nieto-Quero A, Gómez-Salas FJ, Chun J, Estivill-Torrús G, Rodríguez de Fonseca F, et al. Effects of genetic deletion versus pharmacological blockade of the LPA(1) receptor on depression-like behaviour and related brain functional activity. Dis Models Mech. 2018;11(9):dmm035519.
Moreno-Fernández RD, Pérez-Martín M, Castilla-Ortega E, Rosell Del Valle C, García-Fernández MI, Chun J, et al. maLPA1-null mice as an endophenotype of anxious depression. Transl Psychiatry. 2017;7:e1077.
Nentwig TB, Vaughan DT, Braunscheidel KM, Browning BD, Woodward JJ, Chandler LJ. The lateral habenula is not required for ethanol dependence-induced escalation of drinking. Neuropsychopharmacol. 2022;47:2123–31.
Gilpin NW, Richardson HN, Cole M, Koob GF. Vapor inhalation of alcohol in rats. Curr Protoc Neurosci. 2008;Chapter 9:Unit 9.29.
Wagner CK, Silverman AJ, Morrell JI. Evidence for estrogen receptor in cell nuclei and axon terminals within the lateral habenula of the rat: regulation during pregnancy. J Comp Neurol. 1998;392:330–42.
González-Arenas A, Avendaño-Vázquez SE, Cabrera-Wrooman A, Tapia-Carrillo D, Larrea F, García-Becerra R, et al. Regulation of LPA receptor function by estrogens. Biochim et Biophys Acta. 2008;1783:253–62.
Borruto AM, Stopponi S, Li H, Weiss F, Roberto M, Ciccocioppo R. Genetically selected alcohol-preferring msP rats to study alcohol use disorder: Anything lost in translation? Neuropharmacology. 2021;186:108446.
Funding
This work is made possible by the National Natural Science Foundation of China (82071496 to Rao Fu), the Young Teacher Foundation of Sun Yat-sen University (59000-18841219 Rao Fu), Natural Science Foundation of Guangdong Province (2021A1515010463 to Rao Fu), the Shenzhen Science and Technology Program (202205303001697 to Rao Fu), the Fellowship of China Postdoctoral Science Foundation (2022M711491 to Ying Tang) and the Fund of Shenzhen Key Laboratory (ZDSYS20220606100803007) .
Author information
Authors and Affiliations
Contributions
ZHR, JWH and WFL established the AUD animal models; ZHR and WFL performed the animal stereotaxic surgery; ZHR, YT, YXF, YLM, and SLL performed behavioral tests; ZHR, JWH, MLW and RXD conducted molecular biology and histology experiments; ZHR analyze data and drafted the manuscript; JXX, WHZ, YT and JHY contributed to data interpretation and editing of the manuscript. LHZ is the supervisor of ZHR and JWH. RF contributed to experimental design and conception, data interpretation, editing, and final approval of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ren, Z., Hou, J., Li, W. et al. LPA1 receptors in the lateral habenula regulate negative affective states associated with alcohol withdrawal. Neuropsychopharmacol. 48, 1567–1578 (2023). https://doi.org/10.1038/s41386-023-01582-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-023-01582-8