Abstract
Tobacco use is the leading cause of preventable mortality worldwide. Since current smoking cessation aids show only modest efficacy, new interventions are needed. Given the evidence that stress is a potent trigger for smoking, the present randomized clinical trial tested whether stress could augment the effects of a memory updating (retrieval-extinction) intervention. Non-treatment seeking smokers (n = 76) were assigned to one of four conditions composed of either a stressful or non-stressful psychosocial challenge followed by either smoking or neutral cues. Ten minutes after this manipulation, all underwent a 60-minute extinction procedure during which they viewed smoking-related videos and images and manipulated smoking paraphernalia. Compared to participants who were not exposed to the laboratory stressor, the stressor-exposed groups exhibited greater psychophysiological responses during their intervention and greater decreases in cigarette use at two- and six-weeks follow-up independent of smoking cue exposure. Together, these findings suggest that the ability of stress to activate cigarette seeking processes can be exploited to decrease cigarette use. With replication, the stress-based intervention could become a novel strategy for decreasing cigarette use in non-treatment seeking smokers.
Clinicaltrials.gov identifier: NCT04843969.
Similar content being viewed by others
Introduction
Tobacco use is the primary cause of preventable death worldwide [1]. While most tobacco users are familiar with the consequences of smoking, abstinence remains challenging for many. Among the most commonly reported barriers are the perceived difficulties of quitting and coping with stress [2,3,4]. Cessation aids are available but are infrequently used [5] owing partly to their modest efficacy [6,7,8,9] and high cost [10, 11]. Together, these observations highlight the need for new treatments that can increase motivation to quit and improve remission rates.
A fundamental feature of smoking is the learned associations between smoking behaviors and cigarette-related cues [12]. Exposure to these cues can potently trigger both craving and relapse [13,14,15,16,17,18,19,20]. One potential treatment approach involves weakening the strength of these associations, such as through memory reconsolidation blockade. Memory reconsolidation theory postulates that stable (consolidated) memories become labile when recalled and are thus susceptible to modification. While in this labile state, it is possible to interfere with the restabilization (reconsolidation), a process known as memory reconsolidation blockade.
In the past two decades, memory reconsolidation blockade interventions have shown promise as treatments for stress and anxiety related disorders [21,22,23,24,25]. These interventions have typically used pharmacological agents to impair reconsolidation and weaken memory associations. More recent work has tested the potential of less invasive behavioral approaches. One such intervention, known as memory updating, involves three distinct phases: (1) a reactivation phase during which a brief reminder triggers the recall of target memories and renders them labile, vulnerable to modification; (2) a short interval without memory-eliciting stimuli; and (3) an extinction phase during which a lengthy cue exposure alters the elicited memories by disrupting their reconsolidation (restabilization), thereby reducing their potency [26].
Memory updating might also be applied to substance use problems by weakening the ability of drug-associated triggers to elicit substance use [27,28,29]. In recently abstinent heroin-addicted inpatients, two sessions of a memory updating intervention using drug-related cues decreased craving responses during re-exposure to the same cues [29]. A similar approach reduced both cravings and cigarette use in treatment-seeking smokers [27].
In the present study, we aimed to extend the previous findings and further decrease cigarette smoking using a novel procedure. Given the evidence that stress can potently trigger cigarette cravings [30, 31] and use [2,3,4, 32], and increase the retrieval of other drug-related memories [33], we hypothesized that a stress task could augment the effects of a memory updating procedure. To test this, we compared four different conditions (phase 1) as part of a single-session intervention: (1) a stress task followed by smoking cues, (2) a stress task followed by neutral cues, (3) a non-stressful task followed by smoking cues, and (4) a non-stressful task followed by neutral cues. Following a 10-minute period without smoking cues or stress task, participants in all four conditions underwent a 60-minute exposure to smoking-related cues (phase 2). Adding to the study’s novelty, all participants were non-treatment seeking.
Based on the literature described above, we made two main predictions. First, compared to all other groups, the combined stress and cue procedure would induce greater craving and physiological responses during phase 1 and larger decreases in cue reactivity and cigarette use at two- and six-week follow-up. Second, the stress-based intervention alone would be at least as effective as the cue-based intervention alone.
Methods
Participants
Non-treatment seeking smokers were recruited through online advertisements, flyers posted around Montreal, and word-of-mouth. Study eligibility was determined from telephone interviews using the Fagerström Test for Cigarette Dependence (FTCD) [34, 35] and the Mini International Neuropsychiatric Interview [36, 37]. Primary inclusion criteria included scoring 5 or higher on the FTCD, willingness to abstain from smoking for four hours prior to each laboratory visit and being between 18 and 65 years of age. Exclusion criteria included current use of cigarette cessation products, ß-blockers, antidepressant, anxiolytic or other psychotropic medications, pregnancy, and meeting diagnostic criteria for current (untreated) psychological disorders (see Supplementary Methods for additional details). The study was carried out in accordance with the Declaration of Helsinki and approved by the McGill University Research Ethics Board. All participants were informed that study participation could affect their smoking habits and cravings prior to providing written informed consent.
Procedures
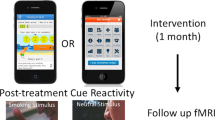
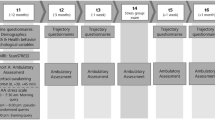
This randomized clinical trial took place between February 2019 and January 2020. The study comprised five in-person visits, including baseline, intervention, and three test sessions given 24 h, two weeks and six weeks post-intervention (Fig. 1). All visits were standardized and administered by the same experimenter (AB). Participants were asked to remain abstinent for four hours prior to each visit. To promote compliance, breath carbon monoxide (CO) measures were collected at the start of the session, but they were not analyzed as the breath monitor lacks sensitivity to detect short periods of abstinence [38, 39].
During the initial assessment and test sessions 1, 2 and 3, a novel smoking-related video was shown to participants. Physiological measures (heart rate (HR) and skin conductance (SC)) were collected prior to and during the last minute of each video presentation. During these same visits, blood pressure (BP) and self-reported cigarette craving and urge to smoke scores were collected pre- and post-video. On the day of the behavioral intervention, baseline physiological measures (HR, SC, and BP) and self-report data were gathered, followed by one of four conditions (phase 1): stress task and smoking cue, stress task and neutral cue, non-stressful task and smoking cue, or non-stressful task and neutral cue. Physiological and craving measures were collected and followed by a 10-minute break. All participants then went through the extinction protocol (phase 2) consisting of additional smoking videos, smoking images, and the manipulation of smoking-related paraphernalia. Immediately after phase 2, physiological and craving measures were gathered again.
Baseline
During the first study visit, participants provided demographic information, including age, sex, ethnicity, level of education, employment status, and history of cigarette use. They completed the Contemplation Ladder [40] to evaluate their readiness to quit smoking and the Cigarette Withdrawal Scale (CWS-21) [41] to assess symptoms of withdrawal on six dimensions: craving, insomnia, depression–anxiety, appetite–weight gain, irritability–impatience, and difficulty concentrating. They then had a baseline cue reactivity assessment during which they viewed a five-minute video containing ten 30-second smoking-related clips (see Supplementary Methods). Pre- and post-video conscious craving responses were measured using the Tobacco Craving Questionnaire––Short Form (TCQ-SF) [42] and the Questionnaire on Smoking Urges––Brief (QSU-Brief) [43]. Physiological measures, including heart rate (HR) and skin conductance (SC), were recorded for one minute pre-video and during the last minute of the five-minute video cue using the ProComp Infinity 5-channel, multi-modality encoder (Thought Technology Ltd, Montreal, Canada). Blood pressure (BP) was collected pre- and post-video cue presentation.
Intervention
Prior to the baseline session, participants were randomized to one of four conditions (phase 1) using a 2 × 2 factorial design: (1) stress task and smoking cue, (2) stress task and neutral cue, (3) control task and smoking cue, or (4) control task and neutral cue. The stress task was the Montreal Imaging Stress Test (MIST) [44], a validated psychosocial challenge consisting of competitive mental arithmetic combined with negative social evaluation (see Supplementary Methods). Participants were blind to group allocation and study hypotheses.
The MIST (or its control version) was immediately followed by a five-minute video cue presentation. For participants in the smoking cue condition, these video clips were similar but non-identical to those presented at baseline. For participants in the neutral cue condition, cues consisted of ten 30-second clips depicting non-smoking activities (see Supplementary Methods). Neutral and smoking cues were matched on number of people in each clip, their approximate age, ethnicity, distance from the camera, and lighting.
All four phase 1 conditions were followed by a 10-minute break during which participants remained seated in front of a black screen. They then underwent a 60-minute extinction protocol (phase 2). This entailed four rotations of: a five-minute video with smoking-related content (composed of similar but non-identical clips to those presented in the baseline visit), a five-minute presentation of smoking images (with each image presented for 3 seconds, see Supplementary Methods), and five minutes of manipulating smoking paraphernalia (e.g., lighter, cigarettes).
Immediately prior to and after phase 1, and immediately after phase 2, HR, SC and BP were measured, and participants completed the TCQ-SF and QSU-Brief. Participants remained in the laboratory for one hour following completion of the questionnaires to minimize the chance that they would reengage the association between cigarette use and smoking-related cues. Participants who underwent the stressful MIST were debriefed. All participants were asked to see how long they could go without smoking after the session.
Test sessions 1, 2 and 3
Participants returned to the laboratory for cue reactivity test sessions 24 h, two weeks, and six weeks following the intervention. During each of these sessions, SC, HR and BP were measured, and the CWS-21, Contemplation Ladder, FTCD (for tests 2 and 3), TCQ-SF and QSU-Brief were administered. Participants then viewed a new five-minute smoking cue video with SC and HR measured for one minute before video presentation and again during the last minute of the video. Immediately after the video, BP was measured and the TCQ-SF and QSU-Brief were administered again.
Between each of the test sessions, participants were asked to record their daily cigarette use in a journal provided by the experimenters. Data from the journals were collected at test sessions 2 and 3.
Statistical analyses
SPSS 26.0.0.1 (Chicago, IL) was used for all statistical analyses. Preliminary analyses indicated less than 1% missing data on all variables. Multiple imputation was used to impute missing scores. Chi square tests and analyses of variance (ANOVAs) were used to examine group differences in study characteristics at baseline for categorical and continuous variables, respectively. Daily cigarette use at test sessions 2 and 3 was calculated as the mean number of cigarettes smoked per day in the week prior to each test session. Repeated measures analyses of variance (ANOVA) were used to examine group differences in physiological and craving measures, daily cigarette use, Contemplation Ladder and FTCD scores. Partial eta squared were used to assess the magnitude of these effects. Greenhouse-Geisser corrections were applied when the assumption of sphericity was violated. Post-hoc analyses consisted of paired samples t-tests with Bonferroni corrections. Correlational analyses tested for potential predictors of cigarette use changes, and the Benjamini-Hochberg procedure with a false discovery rate of 5% was applied to decrease the risk of false positives.
Results
Participant characteristics
Seventy-six volunteers were deemed eligible for the study (Fig. 2). Of these, 14 withdrew or were withdrawn. Reasons for withdrawal included dyscalculia, scheduling conflicts, and not meeting study requirements. Of the remaining 62 participants, one did not attend test session 2 for medical reasons and another missed test session 3 due to relocating to another province. When the participants were randomly assigned to the subgroups, there were no significant differences in tobacco use (16.9 ± 5.9 cigarettes per day; n = 62) or other demographic or clinical characteristics (Table 1).
Experimental manipulation check
Since this was the first time stress and smoking cues were combined in a memory updating procedure, we initially examined whether they elicited their expected effects during phase 1 of the intervention session. As hypothesized, the stress task yielded the predicted effects within the smoking cue groups (Ps < 0.05 for SC, systolic BP and QSU-Brief scores) and the neutral cue groups (Ps < 0.05 for TCQ-SF and QSU-Brief scores). In contrast, the smoking cues, administered immediately after the stress and non-stress tasks, did not change either craving or physiological responses, not within the stress task groups (all Ps > 0.30) or the non-stressful task groups (all Ps > 0.10), nor were there any stress by cue interactions (all Ps > 0.30) (Supplementary Figs. 3 and 5). Based on these observations and an absence of cue effects on cigarette use at follow-up (all Ps > 0.25) (Supplementary Fig. 4), subsequent analyses combined the two stress subgroups (stress) and two non-stressful subgroups (controls), thus increasing statistical power to detect effects of stress.
Responses during the intervention
Phase 1
When comparing scores obtained immediately pre- and post-phase 1, there were main effects of time reflecting anticipated decreases in HR (F1,60 = 61.61, P < 0.001) and increases in SC (F1,60 = 63.04, P < 0.001) and craving (QSU-Brief: F1,60 = 14.90, P < 0.001; TCQ-SF: F1,60 = 14.32, P < 0.001). The increases in physiological and craving scores were larger in the stress group, compared to the controls (Fig. 3A), as reflected by stress condition by time interactions for SC (F1,60 = 8.22, P = 0.006), BP (systolic: F1,60 = 8.65, P = 0.005; diastolic: F1,60 = 5.52, P = 0.022), and craving (QSU-Brief: F1,60 = 13.58, P < 0.001; TCQ-SF: F1,60 = 7.72, P = 0.007). There were no group differences for HR.
During phase 1 (A), participants exposed to the stress task exhibited larger increases in physiological (SC and systolic BP) and craving measures (QSU-Brief and TCQ-SF scores). During phase 2 (B), physiological measures did not significantly differ between groups, but participants previously exposed to the control task exhibited greater smoking cue-induced craving responses (QSU-Brief). BP: blood pressure; SC: skin conductance; TCQ-SF: Tobacco Craving Questionnaire – Short Form; QSU-Brief: Questionnaire on Smoking Urges – Brief. EMM: estimated marginal mean; SEM standard error of the mean. *P < 0.05, ***P < 0.001.
Phase 2
Across groups, the extinction procedure significantly increased SC (F1,60 = 29.60, P < 0.001) and decreased both HR (F1,60 = 68.94, P < 0.001) and systolic BP (F1,60 = 5.85, P = 0.019). The stress and control groups were not significantly different on most measures but there was a stress condition by time interaction for QSU-Brief (F1,60 = 5.03, P = 0.029) reflecting a significant increase in craving during phase 2 only in the control group (P = 0.014) (Fig. 3B).
Cue reactivity assessments
Baseline
As expected, exposure to a smoking-related video led to a main effect of time revealing significant increases in craving (QSU-Brief: F1,60 = 15.01, P < 0.001; TCQ-SF: F1,60 = 13.96, P < 0.001) and SC responses (F1,60 = 46.67, P < 0.001) and decreases in HR (F1,60 = 39.11, P < 0.001) and systolic BP responses (F1,60 = 4.20, P = 0.045). There was a single stress condition by time interaction (systolic BP: F1,60 = 11.76, P = 0.001; Fig. S1C), which was likely spurious given that groups were not yet treated differently. This interaction was controlled for in subsequent analyses.
Tests 1, 2 and 3
Across groups, at each test session, exposure to a new smoking-related video led to increased SC response (all Ps < 0.001) and decreased HR (all Ps < 0.002). Increases in craving were seen at test sessions 1 (TCQ-SF: P < 0.05) and 2 (QSU-Brief: P < 0.001) but not at test session 3. See Supplementary Results and Supplementary Fig. 1 for additional details.
Across sessions
Across sessions, physiological responses to the video cues became less pronounced as shown by decreases in SC ((F3,180 = 5.52, P = 0.001) from baseline to test 1 (P = 0.008) and baseline to test 3 (P = 0.031)) and increases in HR ((F3,180 = 2.90, P = 0.036) from baseline to test 3 (P = 0.033)). No across session changes or group differences in craving were observed. See Supplementary Results and Supplementary Fig. 1 for additional details.
Smoking behavior
Over the period of the study, participants decreased their cigarette use as reflected by a significant main effect of session (F1.66,99.35 = 16.58, P < 0.001). Stress condition by session interactions were observed for baseline vs. test sessions 2 and 3 (F1.66,99.35 = 3.60, P = 0.039, ηp2 = 0.057) and baseline vs. test session 3 alone (F1,60 = 4.86, P = 0.031, ηp2 = 0.075) (Fig. 4A). These interactions reflected significant decreases in cigarette smoking in the stress group participants from baseline to test session 2 (P = 0.001) and baseline to test session 3 (P < 0.001) but not in the control group participants (all Ps > 0.05). This represented decreases of 14% and 26% in the stress group compared to 9% and 10% in the controls at test sessions 2 (F1,62 = 0.67, P = 0.42) and 3 (F1,62 = 3.94, P = 0.052), respectively (Fig. 4B). The magnitude of the intervention’s effect increased over time such that, in the stress group, cigarettes per day decreased from baseline and were lower at test session 3 compared to test 2 (P = 0.020). No significant changes in cigarette use were found in the controls.
A Participants in the stress-based intervention significantly decreased their average daily cigarette use from baseline to the tests 2 and 3 (two and six weeks after the intervention, respectively). B Cigarette use in the stress group participants decreased by 14% at two weeks (test 2) and by 26% at six weeks (test 3), while the control group showed decreases of 9% and 10%, respectively. EMM: estimated marginal mean; SEM: standard error of the mean. In the stress group: ***P ≤ 0.001 compared to baseline, #P < 0.05 compared to test 2.
Across study visits, there were progressive decreases in cigarette dependence (FTCD: F2,120 = 10.94, P < 0.001) and withdrawal symptoms due to craving (CWS-21 craving subscale: F3,180 = 8.05, P < 0.001), and increased motivation to quit smoking scores (Contemplation Ladder: F2.46,147.93 = 9.86, P < 0.001) (Supplementary Table 1). There were no significant group differences in these measures and no main effects of session on other CWS-21 subscales.
Predictors of decreased cigarette use
When participants from all groups were combined, higher systolic BP values following phase 1 of the intervention predicted larger decreases in cigarette use at test session 3 (r = −0.272, P = 0.033) (Supplementary Fig. 2A). Furthermore, larger decreases in systolic BP during phase 2 predicted greater decreases in cigarette use at test session 2 (r = 0.275, P = 0.030; Supplementary Fig. 2B) and test session 3 (r = 0.379, P = 0.002; Supplementary Fig. 2C). This latter result survived the Benjamini-Hochberg correction.
Discussion
The present study tested whether a laboratory stressor could augment the ability of a memory updating procedure to decrease cigarette use. While our predictions for the cue-based intervention were not supported, two hypotheses about the stressor were. First, during phase 1 of the intervention, greater craving and physiological responses were observed following exposure to the stressor as compared to the control task. Second, and more importantly, during the weeks following the intervention, larger decreases in cigarette use were seen in stress versus control group participants.
The failure to reproduce the effect of a previous smoking cue-based intervention on cigarette use [27] might be related to the inability of the present study’s smoking cues to elicit psychophysiological responses when they were combined with the arithmetic tasks (both stress and control versions). This was unexpected since our smoking cues yielded their anticipated effects [45, 46] when administered alone at the baseline and follow-up sessions. Several factors might explain this: (1) the arithmetic tasks may have served as distractors reducing the effectiveness of the smoking cues, (2) the stressful version of the task might have elicited near maximal responses that were not further augmented by exposure to the smoking cues, (3) habituation to the video cues from baseline to phase 1 could not be ruled out, but this was considered unlikely as novel videos were presented at each session and the expected cue-induced responses re-emerged during the follow-up sessions.
The stress-based intervention reduced cigarette use but not craving and physiological responses during the follow-up sessions. This too differed from studies using cue-based memory updating interventions [27, 29] and may reflect several procedural differences in addition to the features noted above. As a start, we used a single intervention session whereas the previous studies provided two sessions [27, 29]. Second, the minimum duration of abstinence prior to each session was four hours as compared to at least 24 hours in previous work [27, 29]. Third, we tested non-treatment seeking volunteers instead of those either seeking [27] or receiving treatment [27, 29]. Indeed, non-treatment seeking smokers exhibit larger smoking cue-reactivity responses than treatment-seekers [47], potentially accounting for the persisting responses across test sessions. Despite this continued ability of smoking cues to elicit craving, the stress-based intervention affected our primary outcome, cigarette use, which decreased by 26% in the stress group (as compared to 10% in controls) by six weeks. Dissociations between self-reported craving and substance use are frequently reported and are thought to indicate that drug-seeking behaviors are driven in large part by processes outside of conscious awareness [48,49,50]. The present study therefore suggests that the stress-based intervention may be more effective at targeting the preconscious processes. Further studies with longer follow-up periods will be needed to determine whether the behavioral changes persist, increase further, or eventually dissipate.
Interestingly, the control procedure also conferred some benefit. Across groups, we observed decreased nicotine dependence scores, increased motivation to quit smoking, and decreased cigarette use. While this may in part be a byproduct of study participation (e.g., placebo or Hawthorne effect), it may also reflect individual differences in responsiveness to the intervention. Just as the stress task may not have been equally stressful to all participants, for some, the control arithmetic task may have been stressful. These individual differences in stress reactivity may account for the correlations between physiological responding at intervention and changes in cigarette use. Across all participants, greater decreases in cigarette use correlated with greater phase 1 systolic BP responses and greater decreases in systolic BP during phase 2. Systolic BP responses could potentially reflect both the reactivation of craving-related processes and the efficacy of the intervention.
While this study was originally conceived as a memory updating paradigm, other interpretations are plausible. One possible interpretation is that phase 2 alone led to decreased cigarette use. However, although extinction procedures (often in the form of exposure therapy) can produce transient reductions in cigarette use [51, 52], long-term clinical efficacy is lacking [51,52,53,54,55,56]. More importantly, in the present study, all participants were exposed to a 60-minute extinction phase yet only those also exposed to the stressor exhibited significant decreases in cigarette use. It is therefore considered unlikely that extinction alone accounted for the present results.
A more plausible alternative interpretation may be that the stress procedure enhanced extinction. Although no studies (to our knowledge) have investigated behavioral stress induction on extinction (as in the current study), cortisol has been used to induce a stress state. In fear-related studies, elevated stress hormones during extinction learning (either endogenously or through prior cortisol administration) can further reduce fear responses post-extinction and at follow-up [57,58,59,60,61,62]. In the only study to date examining the role of pre-extinction stress on appetitive memories in a clinical population, administration of cortisol before exposure to alcohol cues decreased within-session cravings in those with a severe alcohol use disorder but increased cravings in those with less severe symptoms [63]. These limited results with a short follow-up (<8 days) are challenging to interpret and compare with the current findings. Here, as well as in cue-based memory updating studies [27, 64, 65], beneficial outcomes were evident at later time points but not during the extinction session or shortly after it. In contrast, many enhanced extinction studies report favorable effects during or soon after exposure to cues [57, 59, 66]. These different within-exposure session effects may indicate that different mechanisms can lead to similar outcomes, though with different time-courses.
While it is not possible to determine which mechanism (i.e., memory updating or enhanced extinction) is involved, the present study nonetheless provides, to our knowledge, the first evidence that a single-session stress-based intervention can reduce cigarette use in non-treatment seeking smokers. Future studies may wish to examine neurobiological underpinnings and clarify differences between enhanced extinction and memory updating.
References
Centers for Disease Control and Prevention. Smoking & Tobacco Use. 2020. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/index.htm. Accessed 23 April 2021.
Villanti AC, Bover Manderski MT, Gundersen DA, Steinberg MB, Delnevo CD. Reasons to quit and barriers to quitting smoking in US young adults. Fam Pr. 2016;33:133–9.
Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: A systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4:1–15.
Hughes JR. Smokers’ beliefs about the inability to stop smoking. Addict Behav. 2009;34:1005–9.
Cokkinides VE, Ward E, Jemal A, Thun MJ. Under-use of smoking-cessation treatments: Results from the National Health Interview Survey, 2000. Am J Prev. 2005;28:119–22.
Jiloha R. Pharmacotherapy of smoking cessation. Indian J Psychiatry. 2014;56:87–95.
Piasecki TM. Relapse to smoking. Clin Psychol Rev. 2006;26:196–215.
Teneggi V, Tiffany ST, Squassante L, Milleri S, Ziviani L, Bye A. Smokers deprived of cigarettes for 72 h: Effect of nicotine patches on craving and withdrawal. Psychopharmacology 2002;164:177–87.
Waters AJ, Shiffman S, Sayette MA, Paty JA, Gwaltney CJ, Balabanis MH. Cue-provoked craving and nicotine replacement therapy in smoking cessation. J Consult Clin Psychol. 2004;72:1136–43.
Gross B, Brose L, Schumann A, Sabina U, Christian M, Henry V, et al. Reasons for not using smoking cessation aids. BMC Public Health. 2008;8:1–9.
Rosenthal L, Carroll-Scott A, Earnshaw VA, Naa S, O’Malley SS, Alycia S, et al. Targeting cessation: Understanding barriers and motivations to quitting among urban adult daily tobacco smokers. Addict Behav. 2013;38:1639–42.
Niaura RS, Rohsenow DJ, Binkoff JA, Monti PM, Pedraza M, Abrams DB. Relevance of cue reactivity to understanding alcohol and smoking relapse. J Abnorm Psychol. 1988;97:133–52.
Abrams DB, Monti PM, Carey KB, Pinto RP, Jacobus SI. Reactivity to smoking cues and relapse: Two studies of discriminant validity. Behav Res Ther. 1988;26:225–33.
l’Absi M, Hatsukami D, Davis GL. Attenuated adrenocorticotropic responses to psychological stress are associated with early smoking relapse. Psychopharmacology 2005;181:107–17.
Baker TB, Brandon TH, Chassin L. Motivational influences on cigarette smoking. Annu Rev Psychol. 2004;55:463–91.
Brandon TH. Negative affect as motivation to smoke. Curr Dir Psychol Sci. 1994;3:33–37.
Pomerleau CS, Pomerleau OF. The effects of a psychological stressor on cigarette smoking and subsequent behavioral and physiological responses. Psychophysiology 1987;24:278–85.
Rose JE, Ananda S, Jarvik ME. Cigarette smoking during anxiety-provoking and monotonous tasks. Addict Behav. 1983;8:353–9.
Slopen N, Kontos EZ, Ryff CD, Ayanian JZ, Albert MA, Williams DR. Psychosocial stress and cigarette smoking persistence, cessation, and relapse over 9–10 years: A prospective study of middle-aged adults in the United States. Cancer Causes Control. 2013;24:1849–63.
Eikelboom R, Stewart J. Conditioning of drug-induced physiological responses. Psychol Rev. 1982;89:507–28.
Björkstrand J, Agren T, Åhs F, Andreas F, Elna-Marie L, Olof H, et al. Think twice, it’s all right: Long lasting effects of disrupted reconsolidation on brain and behavior in human long-term fear. Behav Brain Res. 2017;324:125–9.
Brunet A, Orr SP, Tremblay J, Robertson K, Nader K, Pitman RK. Effect of post-retrieval propranolol on psychophysiologic responding during subsequent script-driven traumatic imagery in post-traumatic stress disorder. J Psychiatr Res. 2008;42:503–6.
Schiller D, Monfils M-H, Raio CM, Johnson DC, LeDoux JE, Phelps EA. Preventing the return of fear in humans using reconsolidation update mechanisms. Nature 2010;463:49–53.
Soeter M, Kindt M. An abrupt transformation of phobic behavior after a post-retrieval amnesic agent. Biol Psychiatry. 2015;78:880–6.
Telch MJ, York J, Lancaster CL, Monfils MH. Use of a brief fear memory reactivation procedure for enhancing exposure therapy. Clin Psychol Sci. 2017;5:367–78.
Lee JL, Nader K, Schiller D. An update on memory reconsolidation updating. Trends Cogn Sci. 2017;21:531–45.
Germeroth LJ, Carpenter MJ, Baker NL, Froeliger B, LaRowe SD, Saladin ME. Effect of a brief memory updating intervention on smoking behavior: A randomized clinical trial. JAMA Psychiatry. 2017;74:214–23.
Marsden J, Goetz C, Meynen T, Luke M, Garry S, Brian E, et al. Memory-focused cognitive therapy for cocaine use disorder: Theory, procedures and preliminary evidence from an external pilot randomised controlled trial. EBioMedicine 2018;29:177–89.
Xue Y-X, Luo Y-X, Wu P, Hai-Shui S, Li-Fen X, Chen C, et al. A memory retrieval-extinction procedure to prevent drug craving and relapse. Science 2012;336:241–5.
Childs E, de Wit H. Effects of acute psychosocial stress on cigarette craving and smoking. Nicotine Tob Res. 2010;12:449–53.
Buchmann A, Laucht M, Schmid B, Wiedemann K, Mann K, Zimmermann U. Cigarette craving increases after a psychosocial stress test and is related to cortisol stress response but not to dependence scores in daily smokers. J Psychopharmacol (Oxf). 2008;24:247–55.
Nakajima M, Lemieux AM, Fiecas M, Soujanya C, Hillol S, Nazir S, et al. Using novel mobile sensors to assess stress and smoking lapse. Int J Psychophysiol. 2020;158:411–8.
Zhao L-Y, Shi J, Zhang X-L, David HE, Xiang-Yang Z, Yu L, et al. Stress enhances retrieval of drug-related memories in abstinent heroin addicts. Neuropsychopharmacology 2010;35:720–6.
Fagerström K. Determinants of tobacco use and renaming the FTND to the Fagerström Test for Cigarette Dependence. Nicotine Tob Res. 2011;14:75–78.
Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerström test for nicotine dependence: A revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86:1119–27.
Bentz D, Michael T, Wilhelm FH, Francina RH, Sabrina K, von Rohr IRR, et al. Influence of stress on fear memory processes in an aversive differential conditioning paradigm in humans. Psychoneuroendocrinology. 2013;38:1186–97.
Sheehan D, Lecrubier Y, Sheehan KH, Janavs J, Weiller E, Keskiner A, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry. 1997;12:232–41.
Karelitz JL, Michael VC, Perkins KA. Analysis of agreement between expired-air carbon monoxide monitors. J Smok Cessat. 2017;12:105–12.
Perkins KA, Karelitz JL, Jao NC. Optimal carbon monoxide criteria to confirm 24-hr smoking abstinence. Nicotine Tob. 2013;15:978–82.
Biener L, Abrams DB. The Contemplation Ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychol. 1991;10:360–5.
Etter J-F. A self-administered questionnaire to measure cigarette withdrawal symptoms: The Cigarette Withdrawal Scale. Nicotine Tob Res. 2005;7:47–57.
Heishman SJ, Singleton EG, Pickworth WB. Reliability and validity of a Short Form of the Tobacco Craving Questionnaire. Nicotine Tob Res. 2008;10:643–51.
Cox LS, Tiffany ST, Christen AG. Evaluation of the brief questionnaire of smoking urges (QSU-brief) in laboratory and clinical settings. Nicotine Tob Res. 2001;3:7–16.
Dedovic K, Renwick R, Mahani NK, Engert V, Lupien SJ, Pruessner JC. The Montreal Imaging Stress Task: Using functional imaging to investigate the effects of perceiving and processing psychosocial stress in the human brain. J Psychiatry Neurosci. 2005;30:319–25.
Betts JM, Dowd AN, Forney M, Hetelekides E, Tffany ST. A meta-analysis of cue reactivity in tobacco cigarette smokers. Nicotine Tob Res. 2021;23:249–58.
Saladin ME, Gray KM, Carpenter MJ, LaRowe SD, DeSantis SM, Upadhyaya HP. Gender differences in craving and cue reactivity to smoking and negative affect/stress cues. Am J Addict. 2012;21:210–20.
Sayette MA, Dimoff JD. In search of anticipatory cigarette cravings: The impact of perceived smoking opportunity and motivation to seek treatment. Psychol Addict Behav 2016;30:277–86.
Dagher A, Tannenbaum B, Hayashi T, Pruessner JC, McBride D. An acute psychosocial stress enhances the neural response to smoking cues. Brain Res. 2009;1293:40–48.
Rosenberg H. Clinical and laboratory assessment of the subjective experience of drug craving. Clin Psychol Rev. 2009;29:519–34.
Venugopalan VV, Casey KF, O’Hara C, O’Loughlin J, Benkelfat C, Fellows LK, et al. Acute phenylalanine/tyrosine depletion reduces motivation to smoke cigarettes across stages of addiction. Neuropsychopharmacology 2011;36:2469–76.
Lowe MR, Green L, Kurtz SM, Ashenberg ZS, Fisher EB Jr. Self-initiated, cue extinction, and covert sensitization procedures in smoking cessation. J Behav Med. 1980;3:357–72.
Götestam KG, Melin L. An experimental study of covert extinction on smoking cessation. Addict Behav. 1983;8:27–31.
Conklin CA, Tiffany ST. Applying extinction research and theory to cue‐exposure addiction treatments. Addiction 2002;97:155–67.
Niaura R, Abrams DB, Shadel WG, Rohsenow DJ, Monti PM, Sirota AD. Cue exposure treatment for smoking relapse prevention: A controlled clinical trial. Addiction 1999;94:685–95.
Pericot-Valverde I, Secades-Villa R, Gutiérrez-Maldonado J. A randomized clinical trial of cue exposure treatment through virtual reality for smoking cessation. J Subst Abus Treat. 2019;96:26–32.
Brandon TH, Zelman DC, Baker TB. Effects of maintenance sessions on smoking relapse: Delaying the inevitable? J Consulting Clin Psychol. 1987;55:780–7822.
de Quervain DJF, Bentz D, Michael TT, Bolt OC, Wiederhold BK, Margraf J, et al. Glucocorticoids enhance extinction-based psychotherapy. Proc Nat Acad Sci. 2011;108:6621–5.
Siegmund A, Köester L, Meves AM, Plag J, Stoy M, Ströhle A. Stress hormones during flooding therapy and their relationship to therapy outcome in patients with panic disorder and agoraphobia. J Psychiatr Res. 2011;45:339–46.
Soravia LM, Heinrichs M, Aerni A, Maroni C, Schelling G, Ehlert U, et al. Glucocorticoids reduce phobic fear in humans. Proc Nat Acad Sci. 2006;103:5585–90.
Meir Drexler S, Merz CJ, Wolf OT. Preextinction stress prevents context-related renewal of fear. Behav Ther. 2018;49:1008–19.
Meuret AE, Trueba AF, Abelson JL, Liberzon I, Auchus R, Bhaskara L, et al. High cortisol awakening response and cortisol levels moderate exposure-based psychotherapy success. Psychoneuroendocrinology 2015;51:331–40.
Yehuda R, Bierer LM, Pratchett LC, Lehrner A, Koch EC, Van Manen JA, et al. Cortisol augmentation of a psychological treatment for warfighters with posttraumatic stress disorder: Randomized trial showing improved treatment retention and outcome. Psychoneuroendocrinology 2015;51:589–97.
Soravia LM, Moggi F, de Quervain DJF. Effects of cortisol administration on craving during in vivo exposure in patients with alcohol use disorder. Transl Psychiatry. 2021;11:1–9.
Zandonai T, Benvegnù G, Tommasi F, Ferrandi E, Libener E, Ferraro S, et al. A virtual reality study on postretrieval extinction of smoking memory reconsolidation in smokers. J Subs Abus Treat. 2021;125:108317.
Björkstrand J, Agren T, Åhs F, Frick A, Larsson EM, Hjorth O, et al. Disrupting reconsolidation attenuates long-term fear memory in the human amygdala and facilitates approach behavior. Curr Biol. 2016;26:2690–5.
de Quervain DJF, Margraf J. Glucocorticoids for the treatment of post-traumatic stress disorder and phobias: A novel therapeutic approach. Eur J Pharm. 2008;583:365–71.
Acknowledgements
The authors would like to thank Rhonda Amsel for valuable statistical advice and Elena Pérez Gómez for assembling and editing the smoking and neutral video cues. We are also grateful to the large team of undergraduate students who assisted with screening and administrative tasks.
Funding
This research was funded by a James McGill Professor Research Award to KN and Canadian Institutes of Health Research operating funds to KN and ML (MOP-211696) and JP and KN (PJT-148728). The funders had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
AB, KG and ML had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: AB, KG, KN, ML. Acquisition, analysis, or interpretation of data: All authors. Statistical analysis: AB, KG, ML. Drafting of the manuscript: AB, KG, ML. Critical revision of the article for key intellectual content: All authors. Final approval of the version to be published: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barnabe, A., Gamache, K., de Camargo, J.V.P. et al. A novel stress-based intervention reduces cigarette use in non-treatment seeking smokers. Neuropsychopharmacol. 48, 308–316 (2023). https://doi.org/10.1038/s41386-022-01455-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-022-01455-6
This article is cited by
-
Drug memory reconsolidation: from molecular mechanisms to the clinical context
Translational Psychiatry (2023)