Abstract
There is a need to increase the armamentarium of pharmacotherapies for alcohol use disorder (AUD). Recent research suggests that mineralocorticoid receptor (MR) antagonism via spironolactone may represent a novel pharmacological treatment for AUD. We conducted a pharmacoepidemiologic retrospective cohort study (June 1, 2014 to May 31, 2018) to examine whether spironolactone dispensation (≥90 continuous days), for any indication, is associated with changes in weekly alcohol use about 6 months later. We compared 523 spironolactone-treated adults and 2305 untreated adults, matched on high-dimensional propensity scores created from a set of predefined (sociodemographic and health characteristics, diagnoses, and service utilization) and empirical electronic health record-derived covariates. The sample was 57% female and 27% non-White with a mean age of 59.2 years (SD = 19.3). Treated patients reduced their weekly alcohol use by 3.50 drinks (95% CI = −4.22, −2.79), while untreated patients reduced by 2.74 drinks (95% CI = −3.22, −2.26), yielding a significant difference of 0.76 fewer drinks (95% CI = −1.43, −0.11). Among those who drank >7 drinks/week at baseline, treated patients, compared to untreated patients, reported a greater reduction in weekly alcohol use by 4.18 drinks (95% CI = −5.38, −2.97), while there was no significant difference among those who drank less. There was a significant dose-response relationship between spironolactone dosage and change in drinks/week. Pending additional evidence on its safety and efficacy in individuals with AUD, spironolactone (and MR blockade, at large) may hold promise as a pharmacotherapy for AUD.
Similar content being viewed by others
Introduction
The past-year and lifetime prevalence of alcohol use disorder (AUD) was 13.9% and 29.1% in 2012–2013 in the U.S. [1]. Excessive alcohol use was associated with $249 billion in costs in 2010 and with 255 deaths per day between 2011 and 2015 in the U.S. [2]. AUD treatment, especially pharmacotherapy, is highly underutilized. For example, among individuals aged 12 or older from the National Survey on Drug Use and Health in 2019, only 1.9% of those who needed treatment for AUD and 19.8% of those who received AUD treatment, received pharmacotherapy for AUD [3].
Currently, there are only three medications approved by the U.S. Food and Drug Administration for AUD treatment: acamprosate, disulfiram, and naltrexone (oral and intramuscular). A recent review found that naltrexone can reduce the risk of binge-drinking, and that acamprosate and disulfiram can maintain abstinence, yet effect sizes across meta-analyses were small [4]. Another recent review found that the use of naltrexone and acamprosate to control alcohol consumption had only low to moderate efficacy [5]. Therefore, there is a need to investigate novel targets to increase the armamentarium of pharmacotherapies for AUD [6].
Prior research suggests that neuroendocrine pathways play critical roles in the development and maintenance of AUD. For example, the hormone aldosterone, which regulates electrolyte and fluid homeostasis through binding to mineralocorticoid receptors (MRs), has been shown to modulate stress-related behaviors and alcohol use across studies of animals and humans. Specifically, in AUD patients, blood aldosterone levels increase during early alcohol withdrawal and normalize during recovery [7], and have been found to be positively correlated with anxiety, craving, and drinking levels [8, 9]. Consistent with these findings in humans, a study of nonhuman primates found that aldosterone levels significantly increased after sub-chronic alcohol self-administration and that MR gene (Nr3c2) expression in the central nucleus of the amygdala (CeA) was negatively correlated with average alcohol intake [9]. In addition, low Nr3c2 expression levels in the CeA were associated with greater anxiety and compulsive drinking in alcohol-dependent, but not in nondependent, rats [9]. Furthermore, recent rodent studies found that intraperitoneal injection of the MR antagonist spironolactone, as well as CeA injection of the MR antagonist eplerenone, significantly reduced alcohol self-administration [10, 11]. These cross-species findings provide evidence that high functional activity in the aldosterone/MR pathway may contribute to excessive drinking and that pharmacological blockade of the MR may serve as a novel approach for AUD pharmacotherapy.
Spironolactone is widely used in primary care and specialty settings to treat various health conditions (e.g., essential hypertension, heart failure, primary hypoaldosteronism, hypokalemia, and nephrotic syndrome). Notwithstanding spironolactone’s frequent and serious side effects (e.g., hyperkalemia, gynecomastia, and hypotension), the drug has an overall acceptable safety and tolerability profile, especially with proper dose management and close monitoring [12,13,14,15,16,17], which are factors that can facilitate repurposing of this drug and potentially other MR antagonists (e.g., eplerenone) for AUD treatment, pending efficacy studies. The objective of this study was to examine whether spironolactone dispensation for any indication is associated with changes in self-reported weekly alcohol use, using electronic health record (EHR)-based data from Kaiser Permanente Northern California (KPNC), a large integrated health care system, where spironolactone is commonly prescribed and over 90% of outpatient prescriptions are filled at in-house pharmacies.
Patients and methods
Setting
KPNC serves 4.3 million members, about one-third of the population in Northern California. The membership is diverse and reflects the U.S. population with access to care [18]. Membership includes enrollees from Medicaid, Medicare, employer-based plans, and health insurance exchanges. The KPNC Institutional Review Board reviewed the study and granted a waiver of informed consent to examine EHR data.
In June 2013, KPNC implemented systematic alcohol screening in adult primary care and has maintained an average 80% screening rate [19]. As part of the screening, patients are asked three questions embedded in the EHR about their alcohol use, including a modified version of the evidence-based National Institute on Alcohol Abuse and Alcoholism (NIAAA) single-item screening question [20] (tailored to the patient’s age and sex) to determine whether patients had any heavy drinking days: (1) “How many times in the past 3 months have you had 5 or more drinks containing alcohol in a day?” (for men aged 18–65 years), or “4 or more drinks” (for women of any age and men aged 66 or older); and two questions for calculating the average number of alcoholic drinks consumed per week: (2) “On average, how many days per week do you have an alcoholic drink?”; and (3) “On a typical drinking day, how many drinks do you have?”
Study sample and exposure
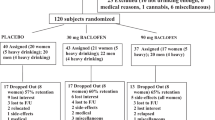
We identified patients who received (treated) or did not receive (untreated) spironolactone dispensed from outpatient KPNC pharmacies. The treated group consisted of 38,466 patients who filled spironolactone prescriptions for any indication between June 1, 2014 and May 31, 2018; the index date was the first dispensation of spironolactone during the inception period. For the untreated group, we identified 5,003,201 patients with at least one outpatient visit during the inception period, and randomly selected one visit as the index date. Treated patients who filled spironolactone prescriptions that supplied <90 continuous days of treatment over a 6-month period post-index (n = 7857), and untreated patients who received spironolactone anytime between June 1, 2014 and May 31, 2019 (n = 46,959) were excluded (Fig. 1). We also sequentially excluded patients if they received spironolactone in the 120 days before the index date (treated = 5782; untreated = 181), had noncontinuous KPNC membership or drug coverage in the year before the index date (allowing 30 day gaps) (treated = 6228; untreated = 1,646,274), did not complete an alcohol screening in the year before the index date (treated = 4810; untreated = 1,440,980), or did not report any alcohol use at the baseline screening (treated = 10,617; untreated = 1,298,726).
Outcome measure and follow-up
The outcome measure was change in alcoholic drinks consumed per week (drinks/week), a discrete measure calculated by subtracting the number of drinks/week reported at the follow-up alcohol screening from the number reported at the baseline screening. We identified the baseline alcohol screening as any in the year before the index date; if the patient had multiple, then the screening closest to the index date was chosen (Supplementary Fig. 1). To emulate a 6-month clinical trial, we identified follow-up alcohol screenings between 120 and 240 days post-index date; if a patient had more than one screening during this period, the one closest to 180 days was chosen. Patients in both groups were sequentially excluded if they were lost to follow-up [treated = 2610 (130 died, 157 disenrolled, and 2323 without a screening); untreated = 510,413 (3720 died, 52,018 disenrolled, and 454,675 without a screening)], or received alcohol treatment during follow-up (i.e., had any visits to specialty addiction medicine or filled a prescription of acamprosate, disulfiram, or naltrexone) (treated = 35; untreated = 1061) (Fig. 1). Thus, there were 527 eligible treated patients and 58,607 eligible untreated patients.
Spironolactone daily dosage
For treated patients, we extracted all outpatient spironolactone prescription fills post-index through follow-up. We constructed a dataset of daily use with one record per patient per day to indicate whether spironolactone was used and the total daily dosage in mg [21]. We assumed that patients took spironolactone according to the days’ supply indicated by the provider on the prescription. If a patient filled a prescription with 7 or more days remaining on a prior fill, then we assumed that the new fill was used concurrently, otherwise it was treated as a fill in stock. Patients could have up to 3 fills in stock, which were assumed to be used consecutively with no gaps. Episodes of spironolactone use (defined as the period from the dispensation date until a gap in days’ supply of more than 30 days) were then generated from the daily use dataset. Mean spironolactone daily dosage was calculated across the duration of the episode, and only the first episode was used if there was more than one during follow-up.
High-dimensional propensity score model and matching
Among the sample of treated (n = 527) and untreated patients (n = 58,607), we generated high-dimensional propensity scores (HDPS) using the Pharmacoepidemiology Toolbox macro to adjust for the conditional probability of exposure (i.e., outpatient spironolactone dispensation to supply at least 90 continuous days of treatment for any indication), given a set of predefined and empirical covariates derived from EHR-based data [22]. In comparison to hypothesis-driven approaches, the HDPS algorithm performs just as well in controlling for confounding and is highly efficient [23]. Briefly, the algorithm takes p data elements, identifies n candidate empirical covariates based on prevalence, and prioritizes the top k covariates based on a selected metric (e.g., Bross formula [24], or association with exposure). We extracted the following 5 data elements (p) from the EHR and included all data in the year before the index date (as early as June 1, 2013 and as late as May 31, 2017): all International Classification of Diseases (ICD) diagnosis codes from outpatient encounters, all ICD diagnosis codes from inpatient hospitalizations, all procedure codes, all generic names of outpatient prescriptions filled at KPNC pharmacies (excluding spironolactone), and all outpatient departments visited. Since KPNC began using ICD-10 diagnosis codes in October 2015, all ICD-9 diagnosis codes were converted to their best ICD-10 equivalent. We identified 300 empirical covariates (n) and prioritized the top 100 covariates (k) based on their association with spironolactone dispensation. HDPS (i.e., the predicted probability of exposure) were estimated using a logistic regression model that included the top 100 empirical covariates and the following predefined covariates: age at index date; sex; race/ethnicity; year of index date; month of index date; smoking status (current or never/former); body mass index [underweight (<18.5), normal weight (18.5–24.9), overweight (25.0–29.9), or obese (≥30.0)] [25]; household income based on geocoded 2017 U.S. Census data [low (≤$74,883), middle ($74,884–$108,988), or high (≥$108,989), based on tertiles of the overall distribution]; number of outpatient, inpatient, and emergency department visits in the year prior to the index date; whether patients had an AUD diagnosis in the year before the index date; and whether patients had a diagnosis indicated for spironolactone treatment in the year before the index date (heart failure, hypertension, hyperaldosteronism, hypokalemia, liver cirrhosis, and nephrotic syndrome) [12].
Using the logit of the HDPS, treated patients were matched to up to 5 untreated patients, using a greedy nearest neighbor algorithm without replacement and within a caliper distance of 0.2 of the standard deviation of the logit of the HDPS [26, 27].
Statistical analysis
We calculated standardized mean differences (SMDs) to examine balance of patient characteristics and health service utilization between treated and untreated patients in the sample, before and after HDPS matching. Characteristics with absolute SMDs < 0.1 were considered to be sufficiently balanced [28].
We estimated the average change in drinks/week associated with spironolactone dispensation (difference-in-difference) using ordinary least squares regression. We also evaluated whether baseline alcohol use (≤7 drinks/week or >7 drinks/week [29]) moderated the association between spironolactone dispensation and alcohol use by including an interaction term with exposure group in the regression model. Models were fit to obtain unadjusted estimates and then were adjusted for patient characteristics that remained imbalanced after matching based on SMD > 0.1 (i.e., sex, heart failure, and hypokalemia), a method that has been shown to successfully remove residual confounding bias [30]. To characterize effect sizes, we calculated Cohen’s d based on the difference-in-difference estimates, where d = 0.2 was considered small, d = 0.5 was moderate, and d = 0.8 was large [31].
To evaluate potential residual differences in the matched groups on illness severity, we calculated the Charlson comorbidity index, a measure that estimates 1-year mortality risk based on a weighted score of 17 medical conditions [32]. We found that the treated group had a higher mean score (mean = 2.45, SD = 2.64) than the untreated group (mean = 2.23, SD = 1.22), with a SMD of −0.136. Thus, as a sensitivity analysis, we added the Charlson index as a covariate in the regression models.
Among the treated sample, we estimated the average dose-response relationship of spironolactone dosage on the change in drinks/week, using ordinary least squares regression, adjusting for all baseline patient characteristics and health service utilization covariates. As a sensitivity analysis, we excluded patients with standardized residuals ≥5, representing extreme values for change in drinks/week.
All statistical analyses were conducted using SAS software, Version 9.4 of the SAS System for Unix (SAS Institute Inc., Cary, NC).
Results
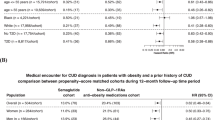
Prior to HDPS-matching, the treated (n = 527) and untreated (n = 58,607) groups differed significantly on most baseline characteristics and past-year utilization (Table 1). A total of 523 treated patients were HDPS-matched to 2305 untreated patients (Table 1): 410 (78%) matched to five, 15 (3%) matched to four, 39 (7%) matched to three, 19 (4%) matched to two, and 40 (8%) matched to one. Unmatched treated patients (n = 4) had higher HDPS (mean = 0.93, SD = 0.12) than those who were matched (n = 523, mean = 0.13, SD = 0.20).
Overall, the aggregate HDPS-matched sample (n = 2828) was 57% female and 27% non-White with a mean age of 59.2 years (SD = 19.3) (data not shown). Distributions of most baseline characteristics were balanced between the treated and untreated groups after HDPS-matching, except for sex (54% versus 59% female), heart failure (33% versus 28%), and hypokalemia (9% versus 7%) (Table 1). There were no differences in baseline weekly alcohol use between the matched groups. The average number of days between the baseline and follow-up screenings was 395.3 days (SD = 99.8).
Spironolactone was prescribed for a variety of health conditions. Among the 523 matched treated patients, 351 (67%) had one diagnosis associated with their index prescription, 77 (15%) had more than one, and 95 (18%) had none. Specifically, 297 (57%) patients were prescribed spironolactone for cardiovascular conditions (e.g., hypertension, heart failure, cardiomyopathy), 101 (19%) for acne or other skin conditions, 31 (6%) for cirrhosis or liver disease, 24 (5%) for ascites, 23 (4%) for edema, 11 (2%) for chronic kidney disease, and 66 (13%) for other conditions (e.g., polycystic ovarian syndrome, hypokalemia, hyperaldosteronism). The average duration of treatment (from index date to the end of the treatment episode) was 144.5 days (SD = 45.3). There were 250 patients (48%) who were still taking spironolactone at the time of their follow-up alcohol screening, and the remaining 273 patients had a mean of 69.1 days (SD = 38.0) between the end of their treatment episode and follow-up screening.
Changes in alcohol use
Weekly alcohol use decreased from baseline to follow-up in both the spironolactone-treated and untreated groups; however, spironolactone-treated patients had a significantly greater reduction in their drinking, compared to untreated patients. Unadjusted and adjusted estimates of the change in drinks/week (the latter acquired from the model adjusting for sex, heart failure, and hypokalemia) were similar (Table 2), thus only adjusted estimates are discussed. On average, spironolactone-treated patients reduced alcohol use by 3.50 drinks/week (95% CI = −4.22, −2.79), while untreated patients reduced alcohol use by 2.74 drinks/week (95% CI = −3.22, −2.26), signifying a difference-in-difference of −0.76 drinks/week (95% CI = −1.43, −0.11) and a Cohen’s d of 0.2.
Baseline alcohol use moderated the association between spironolactone dispensation and change in alcohol use. Among those who reported >7 drinks/week at baseline, treated patients (mean difference = −10.82; 95% CI = −11.96, −9.68) reported a greater reduction in weekly drinking than untreated patients (mean difference = −6.64; 95% CI = −7.23, −6.05), yielding a difference-in-difference of −4.18 drinks (95% CI = −5.38, −2.97) and a Cohen’s d of 0.6. However, among patients who reported ≤7 drinks/week at baseline, there was no significant difference-in-difference of weekly drinking, comparing treated (mean difference = −0.52; 95% CI = −1.24, 0.19) and untreated groups (mean difference = −0.65; 95% CI = −1.12, −0.17).
In sensitivity analyses, we additionally adjusted for the Charlson comorbidity index in the regression models (Supplementary Table 1). The difference-in-difference estimates did not meaningfully differ from those presented in Table 2 (i.e., <10% change).
Dose-response relationship
Among spironolactone-treated patients (n = 523), there was a significant dose-response relationship between spironolactone dosage and change in weekly alcohol use. After adjusting for all baseline characteristics, each additional 10 mg of spironolactone dispensed was associated with a reduction of 0.89 drinks/week (95% CI = −1.46, −0.31) (Fig. 2). We next conducted a sensitivity analysis excluding 3 extreme outliers with standardized residuals >5 for the change in alcohol use, and found a weaker, yet significant, dose-response relationship; each additional 10 mg of spironolactone prescribed was associated with a reduction of 0.40 drinks/week (95% CI = −0.77, −0.03).
Discussion
In this pharmacoepidemiologic study, we found a small, yet significant association between spironolactone dispensation and reduction in self-reported weekly alcohol use among patients with a range of drinking behaviors. The results were more robust among those with higher baseline alcohol use. Specifically, among patients who reported drinking more than 7 drinks/week at baseline (a conservative threshold indicating the potential for alcohol-related harm in both men and women [29]), we found a moderate association between spironolactone dispensation and reduction in weekly alcohol use, suggesting these results may be meaningful from a clinical standpoint. This could be because those who drank ≤7 drinks/week at baseline had a lower baseline drinking level from which they could reduce, or spironolactone was more effective among patients with heavier drinking. Moreover, we found a significant dose-response relationship between spironolactone dosage and change in alcohol use, suggesting a potential causal relationship. While randomized controlled trials are needed to confirm these results, the present pharmacoepidemiologic findings are consistent with recent preclinical work [10, 11] and provide the first preliminary human evidence, to our knowledge, that MR antagonism via spironolactone (and possibly more selective MR antagonists such as eplerenone) could be further studied as a potential novel pharmacotherapy for AUD. Given the potential for spironolactone dose-related side effects [17], results of this study should be interpreted in the context of the risk-benefit ratio and therapeutic index as related to the use of spironolactone in patients with AUD.
In addition to psychosocial and behavioral interventions, medications play a key role in AUD treatment [33]. Considering the unmet need for more efficacious pharmacological options and the complexity of de novo medication development, drug repurposing can facilitate and accelerate this process [34]. Spironolactone is an old drug that is relatively safe, affordable, well-known to clinicians, and widely used to treat several medical conditions in clinical practice, including the hemodynamic complications related to decompensated liver disease. Notably, some patients with AUD develop liver disease, which complicates the management of pharmacotherapy for AUD from a safety standpoint [35]. Furthermore, evidence from a rodent study suggests lack of alcohol-spironolactone interactions, as co-administration of spironolactone and alcohol did not alter alcohol-induced motor impairment [36]. These considerations provide preliminary support in favor of repurposing MR antagonists for AUD treatment; however, much more research is needed to understand their efficacy and safety in this context.
In this study, spironolactone was prescribed mainly in primary care settings. Pending confirmation of efficacy and safety in prospective randomized controlled trials, this aspect suggests the potential feasibility of large-scale implementation of spironolactone treatment for AUD in primary care, a health care setting that is well-positioned to monitor alcohol use through systematic screening and to manage pharmacotherapy. Primary care engagement has also been shown to be an important component of continuing care for AUD and the recovery process [37, 38].
Patients in both the spironolactone-treated and untreated groups reduced alcohol consumption meaningfully from baseline to follow-up, which could be because they received brief advice to limit their drinking by their provider or due to the high prevalence of medical conditions (i.e., hypertension, heart failure) in this matched cohort. Health concerns are among the main reasons why individuals decrease or quit drinking [39], which may explain why both groups reduced the number of drinks consumed per week about in half. Our sensitivity analysis showed that any residual confounding bias due to illness severity was minimal, therefore, the differential reduction in drinking observed is likely not due to health status differences between groups.
Strengths and limitations
By leveraging EHR-based data collected as part of clinical care in an integrated health care system, we examined associations between spironolactone dispensation and changes in alcohol use among a large and diverse sample. Retrospective analysis of EHR data has been used as one of the main approaches to inform drug repurposing endeavors [40]. While the availability of clinical and therapeutic data drawn from population-based EHR data offer great opportunities for pharmacoepidemiologic research, ascertainment of exposure and outcome in such type of studies has some level of uncertainty [41]. For example, data on spironolactone dispensation was acquired retrospectively from past pharmacy fills; therefore, direct assessment of compliance was not feasible. Social desirability bias and recall bias represent other potential limitations of self-reported alcohol use data. For example, prior research has found that self-reported volume of alcohol only accounted for 40% of total sales volume of alcohol [42]. The healthcare system in this study conducted an implementation trial to determine the best workflow for alcohol screening that would minimize stigma and optimize patient comfort in disclosing alcohol use [19], so while underreporting is possible, more in-depth qualitative data is needed to understand the extent of these potential biases on study findings. Additionally, about half of the treated group in this study had follow-up alcohol screenings after completion of their spironolactone fills. While the duration of this gap was unlikely to affect the representativeness of the follow-up screening in measuring alcohol use at time of exposure, a future study with a large enough sample should consider examining whether effect sizes differ by duration and timing of use at follow-up. We did not have data on adverse side effects (e.g., dizziness, headache, lightheadedness, fainting) or other forms of alcohol treatment (e.g., 12-Step, Alcoholics Anonymous), so we could not adjust for these factors in our analyses; however, patients who received specialty addiction treatment were excluded from the study.
Although we cannot infer causality with our observational study design, we utilized methods that appropriately adjusted for potential bias and confounding. Similar to a prior study that examined the effects of gabapentin on alcohol consumption in veterans with and without AUD, we used propensity score matching to assemble an untreated group with similar characteristics as the treated group [43]. In addition to predefined covariates, we generated empirical covariates from the EHR (e.g., all generic names of outpatient prescriptions and all departments visited in the prior year) to calculate HDPS. While treatment groups differed significantly on nearly all predefined variables before matching (as expected given the clinical indications for which spironolactone is prescribed), balance was achieved on nearly all variables after HDPS matching, except a few, which were added as covariates in the models. Additionally, we examined spironolactone dispensation among patients who did not previously fill a prescription in the prior 4 months, which is important for assuring temporality of the association between spironolactone dispensation and change in alcohol consumption. The presence of a meaningful dose-response relationship adds support, albeit preliminary, for a potential causal relationship between spironolactone dispensation and change in alcohol use. Since there was a low proportion of patients with a daily dosage greater than 200 mg/day, extrapolation of the dose-response relationship for high dosages is not possible. From a mechanistic standpoint, it is important to note that spironolactone binds to other receptors and is thus not selective for the MR; however, a recent rodent study has demonstrated that the MR-selective antagonist eplerenone led to similar reductions in alcohol use as spironolactone [11].
Unlike a prior gabapentin study in veterans [43], we were unable to examine whether AUD moderated the association between spironolactone dispensation and change in alcohol use due to the small number of patients with AUD in our study (n = 64); however, we found that higher baseline alcohol use was a significant moderator. A future prospective randomized controlled study should examine both abstinence and reduction in alcohol use as outcomes in assessing the efficacy of spironolactone in treating AUD [44].
Conclusion
Findings suggest that MR antagonism via spironolactone or possibly other compounds blocking MR could be further studied as a potential pharmacotherapeutic option for AUD treatment. While future preclinical studies should examine the underlying mechanisms of action, randomized controlled trials in humans are needed to evaluate the safety and efficacy of MR antagonists for AUD treatment.
References
Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–66.
Esser MB, Sherk A, Liu Y, Naimi TS, Stockwell T, Stahre M, et al. Morbidity and Mortality Weekly Report: Deaths and years of potential life lost from excessive alcohol use—United States, 2011–2015. U.S. Department of Health and Human Services, Center for Disease Control and Prevention. 2020;69:1428–33. https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6939a6-H.pdf. Accessed 7 Oct 2020.
Substance Abuse and Mental Health Services Administration. Section 5: Substance Use Disorder and Treatment Tables. Results from the 2019 National Survey on Drug Use and Health: Detailed Tables. 2020. https://www.samhsa.gov/data/sites/default/files/reports/rpt29394/NSDUHDetailedTabs2019/NSDUHDetTabsSect5pe2019.htm. Accessed 28 Oct 2020.
Kranzler HR, Soyka M. Diagnosis and pharmacotherapy of alcohol use disorder: a review. JAMA. 2018;320:815–24.
Palpacuer C, Duprez R, Huneau A, Locher C, Boussageon R, Laviolle B, et al. Pharmacologically controlled drinking in the treatment of alcohol dependence or alcohol use disorders: a systematic review with direct and network meta-analyses on nalmefene, naltrexone, acamprosate, baclofen and topiramate. Addiction. 2018;113:220–37.
Farokhnia M, Browning BD, Leggio L. Prospects for pharmacotherapies to treat alcohol use disorder: an update on recent human studies. Curr Opin Psychiatry. 2019;32:255–65.
Kovács GL. The role of atrial natriuretic peptide in alcohol withdrawal: a peripheral indicator and central modulator? Eur J Pharmacol. 2000;405:103–12.
Leggio L, Ferrulli A, Cardone S, Miceli A, Kenna GA, Gasbarrini G, et al. Renin and aldosterone but not the natriuretic peptide correlate with obsessive craving in medium-term abstinent alcohol-dependent patients: a longitudinal study. Alcohol. 2008;42:375–81.
Aoun EG, Jimenez VA, Vendruscolo LF, Walter NAR, Barbier E, Ferrulli A, et al. A relationship between the aldosterone-mineralocorticoid receptor pathway and alcohol drinking: preliminary translational findings across rats, monkeys and humans. Mol Psychiatry. 2018;23:1466–73.
Makhijani VH, Van Voorhies K, Besheer J. The mineralocorticoid receptor antagonist spironolactone reduces alcohol self-administration in female and male rats. Pharm Biochem Behav. 2018;175:10–8.
Makhijani VH, Irukulapati P, Van Voorhies K, Fortino B, Besheer J. Central amygdala mineralocorticoid receptors modulate alcohol self-administration. Neuropharmacology. 2020;181:108337.
U.S. Food and Drug Administration. Aldactone, spironolactone tablets, USP. 2008. https://www.accessdata.fda.gov/drugsatfda_docs/label/2008/012151s062lbl.pdf. Accessed 11 Aug 2020.
Shaw JC, White LE. Long-term safety of spironolactone in acne: results of an 8-year followup study. J Cutan Med Surg. 2002;6:541–5.
Wang C, Xiong B, Huang J. Efficacy and safety of spironolactone in patients with resistant hypertension: a meta-analysis of randomised controlled trials. Heart Lung Circ. 2016;25:1021–30.
Xiang Y, Shi W, Li Z, Yang Y, Wang SY, Xiang R, et al. Efficacy and safety of spironolactone in the heart failure with mid-range ejection fraction and heart failure with preserved ejection fraction: A meta-analysis of randomized clinical trials. Medicine. 2019;98:e14967.
Buckallew AR, Tellor KB, Watson R, Miller W, Mbachu G, Whitlock C, et al. Evaluation of the safety and tolerability of spironolactone in patients with heart failure and chronic kidney disease. Eur J Clin Pharmacol. 2021. 15 Jan 2021. https://doi.org/10.1007/s00228-020-03069-7.
Lainscak M, Pelliccia F, Rosano G, Vitale C, Schiariti M, Greco C, et al. Safety profile of mineralocorticoid receptor antagonists: spironolactone and eplerenone. Int J Cardiol. 2015;200:25–29.
Gordon NP. Similarity of the adult Kaiser Permanente membership in Northern California to the insured and general population in Northern California: statistics from the 2011 California Health Interview Survey. 2015. https://divisionofresearch.kaiserpermanente.org/projects/memberhealthsurvey/SiteCollectionDocuments/chis_non_kp_2011.pdf. Accessed 15 Mar 2019.
Mertens JR, Chi FW, Weisner CM, Satre DD, Ross TB, Allen S, et al. Physician versus non-physician delivery of alcohol screening, brief intervention and referral to treatment in adult primary care: the ADVISe cluster randomized controlled implementation trial. Addict Sci Clin Pract. 2015;10:26.
National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: a clinician’s guide. 2005. https://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf. Accessed 13 Mar 2018.
Ray GT, Bahorik AL, VanVeldhuisen PC, Weisner CM, Rubinstein AL, Campbell CI. Prescription opioid registry protocol in an integrated health system. Am J Manag Care. 2017;23:e146–55.
Schneeweiss S, Rassen JA, Glynn RJ, Avorn J, Mogun H, Brookhart MA. High-dimensional propensity score adjustment in studies of treatment effects using health care claims data. Epidemiology. 2009;20:512–22.
Guertin JR, Rahme E, Dormuth CR, LeLorier J. Head to head comparison of the propensity score and the high-dimensional propensity score matching methods. BMC Med Res Methodol. 2016;16:22.
Bross ID. Spurious effects from an extraneous variable. J Chronic Dis. 1966;19:637–47.
Centers for Disease Control and Prevention. About Adult BMI. Healthy Weight. 2019. https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. Accessed 29 Apr 2019.
Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10:150–61.
Austin PC. A comparison of 12 algorithms for matching on the propensity score. Stat Med. 2014;33:1057–69.
Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38:1228–34.
Sherk A, Thomas G, Churchill S, Stockwell T. Does drinking within low-risk guidelines prevent harm? Implications for high-income countries using the International Model of Alcohol Harms and Policies. J Stud Alcohol Drugs. 2020;81:352–61.
Nguyen T-L, Collins GS, Spence J, Daurès J-P, Devereaux PJ, Landais P, et al. Double-adjustment in propensity score matching analysis: choosing a threshold for considering residual imbalance. BMC Med Res Methodol. 2017;17:78.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1988.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9.
Witkiewitz K, Litten RZ, Leggio L. Advances in the science and treatment of alcohol use disorder. Sci Adv. 2019;5:eaax4043.
Litten RZ, Falk DE, Ryan ML, Fertig JB. Discovery, development, and adoption of medications to treat alcohol use disorder: goals for the phases of medications development. Alcohol Clin Exp Res. 2016;40:1368–79.
Leggio L, Lee MR. Treatment of alcohol use disorder in patients with alcoholic liver disease. Am J Med. 2017;130:124–34.
Grupp LA, Elias J, Perlanski E, Stewart RB. Modification of ethanol-induced motor impairment by diet, diuretic, mineralocorticoid, or prostaglandin synthetase inhibitor. Psychopharmacology. 1985;87:20–4.
Joudrey PJ, Kladney M, Cunningham CO, Bachhuber MA. Primary care engagement is associated with increased pharmacotherapy prescribing for alcohol use disorder (AUD). Addict Sci Clin Pract. 2019;14:19.
Chi FW, Parthasarathy S, Mertens JR, Weisner CM. Continuing care and long-term substance use outcomes in managed care: early evidence for a primary care-based model. Psychiatr Serv. 2011;62:1194–200.
Rosansky JA, Rosenberg H. A systematic review of reasons for abstinence from alcohol reported by lifelong abstainers, current abstainers and former problem-drinkers. Drug Alcohol Rev. 2020;39:960–74.
Pushpakom S, Iorio F, Eyers PA, Escott KJ, Hopper S, Wells A, et al. Drug repurposing: progress, challenges and recommendations. Nat Rev Drug Discov. 2019;18:41–58.
Moore N, Blin P, Droz C. Pharmacoepidemiology. Handb Exp Pharmacol. 2019;260:433–51.
Høyer G, Nilssen O, Brenn T, Schirmer H. The Svalbard study 1988–89: a unique setting for validation of self-reported alcohol consumption. Addiction. 1995;90:539–44.
Rentsch CT, Fiellin DA, Bryant KJ, Justice AC, Tate JP. Association between gabapentin receipt for any indication and Alcohol Use Disorders Identification Test-Consumption scores among clinical subpopulations with and without alcohol use disorder. Alcohol Clin Exp Res. 2019;43:522–30.
Falk D, Wang XQ, Liu L, Fertig J, Mattson M, Ryan M, et al. Percentage of subjects with no heavy drinking days: evaluation as an efficacy endpoint for alcohol clinical trials. Alcohol Clin Exp Res. 2010;34:2022–34.
Acknowledgements
The authors gratefully acknowledge Dr. Raye Litten from the National Institute on Alcohol Abuse and Alcoholism for providing invaluable feedback during the initial development of this project.
Funding
This study was supported by grants from the National Institute on Alcohol Abuse and Alcoholism (NIAAA): HHSN275201800625P (CW) and R01AA025902 (SS). MF and LL are supported by the National Institute on Drug Abuse (NIDA) and NIAAA intramural research funding ZIA-DA000635 and ZIA-AA000218 (LL). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
VAP had full access to the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. VAP, MF, AHK, LL, CW, and FWC conceptualized and designed the work. VAP conducted the statistical analyses. All authors contributed to acquisition, analysis, or interpretation of data. VAP, MF, and LL drafted the original manuscript. All authors critically revised the manuscript for important intellectual content. CW, MF, and LL obtained funding for the work and provided administrative, technical, and material support. FWC, CW, and LL supervised the work. All authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Palzes, V.A., Farokhnia, M., Kline-Simon, A.H. et al. Effectiveness of spironolactone dispensation in reducing weekly alcohol use: a retrospective high-dimensional propensity score-matched cohort study. Neuropsychopharmacol. 46, 2140–2147 (2021). https://doi.org/10.1038/s41386-021-01117-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-021-01117-z