Abstract
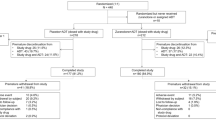
Sub-threshold hypomanic symptoms are common in major depressive disorder. This study evaluated the prevalence, the clinical and sociodemographic correlates, and the overall and differential effects of the presence/absence of sub-threshold hypomanic symptoms at baseline on acute-phase treatment outcomes with bupropion-plus-escitalopram combination, escitalopram monotherapy, and venlafaxine-plus-mirtazapine combination. Combining medications to enhance depression outcomes (CO-MED) trial participants (n = 665) were designated as sub-threshold hypomanic symptoms present (Altman Self-Rating Mania Scale score (ASRM) ≥ 1) or absent (ASRM = 0) and compared on clinical and sociodemographic features and remission rates. Participants with sub-threshold hypomanic symptoms (n = 335/665, 50.4%) were more likely to be black and non-Hispanic, have comorbid medical and psychiatric disorders, experience longer index episodes, and report lower depression severity and psychosocial impairment. Intent-to-treat remission rates were lower overall (absent = 42.7%, present = 34.0%, p = 0.02), with escitalopram monotherapy (absent = 45.8%, present = 31.6%, p = 0.03), and with venlafaxine-XR-plus-mirtazapine combination (absent = 44.4%, present = 30.1%, p = 0.03) but not with bupropion-plus-escitalopram combination (absent = 37.7%, present = 40.0%, p = 0.73). Participants without sub-threshold hypomanic symptoms were more likely to remit than those with such symptoms overall [odds ratio (OR) = 1.49], with escitalopram monotherapy (OR = 1.71), and with venlafaxine-plus-mirtazapine combination (OR = 1.97) but not with bupropion-plus-escitalopram combination (OR = 0.96), even after controlling for baseline depression severity, psychosocial impairment, and number of comorbid psychiatric disorders. Sub-threshold hypomanic symptoms (found in about 50% of patients in this report) were associated with lower remission rates with escitalopram monotherapy and with venlafaxine-plus-mirtazapine combination but not with the bupropion-plus-escitalopram combination.
Similar content being viewed by others
Introduction
While the diagnosis of major depressive disorder (MDD) rests on the presence of at least five of the nine criterion diagnostic symptoms, patients with MDD often report symptoms of anxiety, irritability, mania/hypomania, and psychosis [1, 2]. Specifically, the co-occurrence of agitation, excitability, or flight of ideas along with depressed mood has long been recognized [3]. The National Comorbidity Survey Replication (NCS-R) study, a nationally representative face-to-face household survey, found that over a third of respondents with major depressive disorder endorsed lifetime history of sub-threshold hypomania [4]. Similarly, other studies have reported the occurrence of at least one hypomanic symptom during major depressive episodes (MDEs) in 26–50% of patients with MDD [5, 6] and three or more hypomanic symptoms in 7–23% of patients with MDD [3, 7].
Presence of sub-threshold hypomanic symptoms in patients with MDD, as compared to those without these symptoms, is associated with higher rates of comorbid anxiety and substance use disorders [4, 8], family history of bipolar disorder [4, 6, 9], polypharmacy with drugs of multiple classes [8], hospitalizations [8, 10], and comorbid medical disorders [5], along with earlier age of onset [2, 6], greater severity of suicidal thoughts [9], longer duration of index episode [9], and higher total healthcare costs [8]. Additionally, history of sub-threshold hypomanic symptoms in patients with MDD is associated with poorer lifetime pattern of response to antidepressant medications [10]. Lurasidone, an atypical antipsychotic which is approved by the Food and Drug Administration for treatment of bipolar depression, was more effective than placebo as monotherapy in MDD patients with mixed features [11]. Clinical recognition of sub-threshold hypomanic symptoms in MDD will likely increase with the inclusion of “with mixed features” specifier of MDD in DSM-5 [2]. However, the extent to which the presence of hypomanic symptoms affects acute-phase antidepressant treatment outcome remains unclear.
This report is a secondary data analysis that uses acute-phase data from the Combining Medications to Enhance Depression Outcomes (CO-MED) trial to answer the following questions:
-
1.
What is the prevalence of self-reported hypomanic symptoms in a representative sample of outpatients with chronic or recurrent MDD in whom bipolar disorder was ruled out with the structured diagnostic interview?
-
2.
What baseline clinical and sociodemographic features distinguish those with and without hypomanic symptoms?
-
3.
Do pre-treatment hypomanic symptoms affect acute-phase treatment outcome?
-
4.
Do treatment arms (escitalopram-plus-placebo, bupropion-plus-escitalopram, and venlafaxine-plus-mirtazapine) differ in acute-phase treatment outcome based on pre-treatment hypomanic symptoms?
Material and methods
Study overview and participants
The analytic sample included 665 participants in the CO-MED trial, who were recruited from six primary and nine psychiatric care sites in the United States from March 2008 to September 2009. All participants provided written informed consent prior to completing study procedures. The CO-MED trial was approved by the Institutional Review Boards at UT Southwestern Medical Center at Dallas, the University of Pittsburgh Data Coordinating Center, and each participating regional center and clinical site, and was monitored by an independent Data Safety and Monitoring Board. Eligible participants met criteria for nonpsychotic, chronic (current episode exceeded 2 years) or recurrent depression (with current episode ≥2 months in duration) assessed per the Mini-International Neuropsychiatric Interview (MINI) [12]. The 17-item Hamilton Rating Scale for Depression (HRSD17) [13] was administered during the screening visit to determine eligibility (a score of ≥16 met inclusion criteria) and to assess the severity of depressive symptoms. Participants were excluded if they had a history of psychotic depression, schizophrenia, bipolar (I, II, or NOS), schizoaffective, or any other Axis I psychotic disorder. Study design and detailed inclusion and exclusion criteria have been previously reported by Rush et al. [14].
Treatments
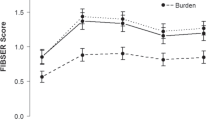
Upon enrollment into the clinical trial, participants were randomly assigned to one of the following three treatment arms in a 1:1:1 ratio: (1) escitalopram-plus-placebo (SSRI monotherapy), (2) sustained-release (SR) bupropion-plus-escitalopram (bupropion–SSRI combination), and (3) extended-release (XR) venlafaxine-plus-mirtazapine (venlafaxine–mirtazapine combination). Details regarding randomization may be found in the primary paper [14]. Study visits for the acute phase were as follows: baseline and weeks 1, 2, 4, 6, 8, 10, and 12; the continuation-phase study visits were weeks 16, 20, 24, and 28, at which time the planned study ended (Clinical Trials Registration, 2008). At each visit within the first 8 weeks, study physicians used measurement-based care (MBC), to guide adjustments to medication dosage [15]. The Quick Inventory of Depressive Symptomatology, Clinician-rated version (QIDS-C16) [16] scale was used to monitor symptom severity and the Frequency, Intensity, and Burden of Side Effects Rating (FIBSER) [17] scale was used to determine medication tolerability as part of MBC [15]. Participants proceeded to the continuation-phase only if they (1) had received an acceptable benefit (defined as QIDS-C16 score of 9 or less by 3 months) or (2) had reached a score of 10–13 on QIDS-C16 and both the study physician and the participant decided to continue treatment due to substantial benefit [14].
Acute-phase treatment outcome
In the CO-MED trial, the primary outcome was symptom remission, which was based on the last two consecutive measurements of Quick Inventory of Depressive Symptomatology, Self-Report version (QIDS-SR16) during the 12-week acute-phase to ensure that one “good” week did not falsely signal remission [14]. Remission was ascribed if at least one of these QIDS-SR16 scores were <6 while the other had to be <8. For participants who exited before week-12, their last two consecutive scores were used to ascribe remission. Participants who had fewer than two post-baseline visits were considered not to have attained remission.
Assessments
The following measures were obtained at baseline and each subsequent study visit (weeks 1, 2, 4, 6, 8, 10, 12, 16, 20, 24, and 28).
The Altman Self-Rating Mania Scale (ASRM): This five item self-rating scale assesses (1) elevated/euphoric mood, (2) increased self-esteem, (3) decreased need for sleep, (4) pressured speech, and (5) psychomotor agitation, over the past 7 days. Each item consists of five possible responses, with scores ranging from 0 to 4, and the total score is obtained by adding the item scores with a scale of 0–20. The scale has a Cronbach’s alpha of 0.79. The correlation coefficients with Clinician-Administered Rating Scale for Mania (CARS-M) and the Young Mania Rating Scale (YMRS) were 0.766 and 0.718 respectively. A total score of 6 or more has high sensitivity and specificity in identifying acute mania [18, 19].
Quick Inventory of Depressive Symptomatology: This 16-item clinician-rated (QIDS-C16) or self-report (QIDS-SR16) scale is used as a measure of overall depression severity with a total score range of 0–27 with higher scores indicating greater severity of the nine criterion depressive symptom domains that define a major depressive episode. Each of the nine domains is rated from 0 to 3. The Pearson moment correlations between QIDS-SR16 and HRSD17 was 0.86 and between QIDS-C16 and HRSD17 was 0.93 in a previous report [16]. The primary outcome of the CO-MED trial was based on QIDS-SR16 while the QIDS-C16 was obtained from 30-item Inventory of Depressive Symptomatology (IDS-C) [20] and was used by clinicians to monitor symptom change [14].
Analysis plan
A series of exploratory analyses were conducted to address questions about the types and presence of hypomanic symptoms in this sample of participants with unipolar major depressive disorder and how they might influence treatment outcome. These retrospective analyses were designed to address questions of clinical relevance but were not posed as hypotheses to be tested. Results should be viewed as hypothesis generating. Therefore, effect sizes reported as number needed to treat and odds ratios are more important than specific p values [21].
What is the prevalence of self-reported hypomanic symptoms in a representative sample of outpatients with chronic or recurrent MDD in whom bipolar disorder was excluded with a structured diagnostic interview? The distribution of hypomanic symptoms at baseline as measured by total ASRM scores were evaluated using frequency plots. Three hundred and thirty-five participants (total ASRM score ≥1) reported the presence of sub-threshold hypomanic symptoms, while no hypomanic symptom was endorsed by 330 participants (total ASRM score of 0).
What baseline clinical and sociodemographic features distinguish those with and without hypomanic symptoms? Descriptive statistics were used to compare baseline clinical and sociodemographic characteristics among CO-MED trial participants with and without sub-threshold hypomanic symptoms at baseline. Based on a literature review, the following baseline clinical and sociodemographic features were compared: comorbid anxiety and substance use disorders [4, 8]; number of comorbid medical disorders [5]; age of onset before 18-years [6]; severity of suicidal ideation at baseline [9]; duration of current episode [7, 9]; employment status [5]; psychosocial impairment [4]; lifetime history of suicide attempt [4]; and depressive symptom severity [4]. In the CO-MED trial, severity of suicidal ideation was measured via Concise Health Risk Tracking (CHRT) scale [22], psychosocial impairment was measured via Work and Social Adjustment Scale [23], number of comorbid medical disorders were measured via Self-Administered Comorbidity Questionnaire (SCQ) [24], and the presence, as well as the number of comorbid psychiatric disorders, were assessed via Psychiatric Diagnostic Screening Questionnaire [25]. Additional variables collected as part of baseline assessments in CO-MED trial and compared included age, gender, ethnicity, monthly income, and years of education. As monthly income, years of education, episode duration, number of comorbid medical disorders, and number of comorbid psychiatric disorders were not normally distributed, they were categorized as listed in Table 1. While categories of QIDS-SR16 were also compared between the two groups to replicate findings of a previous report [4], total scores of QIDS-SR16 were used as a covariate instead of the categories of depression severity.
Do pre-treatment hypomanic symptoms affect acute-phase treatment outcome? To determine whether baseline sub-threshold hypomanic symptoms (absent vs. present) predicted treatment outcomes, the χ2 test was conducted with remission (defined earlier in the acute-phase treatment outcome subsection) as treatment outcome.
Do the treatment arms (escitalopram-plus-placebo, bupropion-plus-escitalopram, and venlafaxine-plus-mirtazapine) differ in acute-phase treatment outcome based on pre-treatment hypomanic symptoms? Since there were no published reports to suggest that specific treatments are more effective for MDD patients with subthreshold hypomanic symptom, a two-step approach was used. An overall test to determine if the presence of subthreshold hypomanic symptoms impacted treatment outcomes was used along with follow-up simple effect tests in each arm that were conditional on the overall test. Given the large number of potential covariates, the simple effects approach allows for the inclusion of the covariates without the need to test for the large number of interactions with treatment groups needing to be tested. Thus, separate analyses for each treatment arm were conducted to determine whether the three treatment arms (SSRI monotherapy, bupropion–escitalopram combination, and venlafaxine–XR–mirtazapine combination) differed in remission rate depending on baseline hypomanic symptoms (absent or present). Finally, logistic regressions were conducted to control for baseline variables that differed between those with sub-threshold hypomanic symptoms and those without. The initial logistic regression model included all variables from Table 1 that showed a difference between the two groups (p < 0.10). In a two-stage process, all the covariates were tested in the initial model regression model but only the significant ones were included in the final model (QIDS-SR16, WSAS, and a number of comorbid conditions on the Psychiatric Diagnostic Screening Questionnaire (PDSQ) at baseline).
Results
What is the prevalence of self-reported hypomanic symptoms in a representative sample of outpatients with chronic or recurrent MDD in whom bipolar disorder was ruled out with the structured diagnostic interview?
Half the sample (335/665) (50.4%) reported at least one hypomanic symptom at baseline. Figure 1 shows the distribution of total ASRM scores with 6.0% (40/665) participants reporting scores ≥6. In participants who reported at least one hypomanic symptom (n = 335), pressured speech was reported most often while psychomotor agitation was reported least often (Fig. 2; also see supplementary table 1 for distribution of responses to individual items).
What baseline clinical and sociodemographic features distinguish those with and without hypomanic symptoms?
Table 1 summarizes the baseline features of the full sample and the subgroups based on the presence of hypomanic symptoms. Among demographic features, black race and non-Hispanic ethnicity were associated with the presence of hypomanic symptoms (Table 1). Among clinical features, the presence of sub-threshold hypomanic symptoms was associated with longer episode duration, a greater number of comorbid medical and psychiatric disorder, lower self-reported but not clinician-rated depression severity, and lower psychosocial function impairment (Table 1). Alcohol use disorder, bulimia, obsessive-compulsive disorder, post-traumatic stress disorder, and social anxiety were reported more frequently on PDSQ by participants with sub-threshold hypomanic symptoms as compared to those without these symptoms.
Do pre-treatment hypomanic symptoms affect acute-phase treatment outcome?
Yes. Overall, remission rates were 1.45 times higher (95% confidence interval [CI] = 1.06, 1.98, χ2 (1) = 5.30, p = 0.02) among participants without sub-threshold hypomanic symptom (42.7%, 141/330) as compared to those with these symptoms present (34.0%, 114/335; see Table 2). In logistic regression analysis with remission as the outcome variable, the participants without sub-threshold hypomanic symptoms continued to have greater likelihood of attaining remission (odds ratio = 1.49, 95% CI = 1.06, 2.10, χ2 (1) = 5.32, p = 0.02) than those with these symptoms present even after controlling for baseline self-reported depression severity, psychosocial function, and number of comorbid psychiatric disorders.
Do treatment arms differ in acute-phase treatment outcome based on pre-treatment hypomanic symptoms?
Yes. With SSRI monotherapy, participants without hypomanic symptoms were 1.82 times [95% CI = 1.06, 3.15, χ2 (1) = 4.74, p = 0.03] more likely to remit (45.8%, 49/107) than those with hypomanic symptoms present (31.6%, 37/117). Similarly, in the venlafaxine–mirtazapine combination arm, participants without hypomanic symptoms were 1.86 times [95% CI = 1.06, 3.24, χ2 (1) = 4.80, p = 0.03] more likely to remit (44.4%, 52/117) than those with hypomanic symptoms present (30.1%, 31/103). However, in bupropion-SSRI treatment arm, there was no difference [χ2 (1) = 0.12, p = 0.73] in remission rate between those with hypomanic symptoms absent (37.7%, 40/106) and present (40.0%, 46/115; see Fig. 3). In logistic regression analyses adjusted for baseline self-reported depression severity, psychosocial function, and number of comorbid psychiatric disorders present, participants without sub-threshold hypomanic symptoms were marginally more likely to attain remission with SSRI monotherapy [OR = 1.71, 95% CI = 0.95, 3.10, χ2 (1) = 3.16, p = 0.076] and with venlafaxine–mirtazapine combination [OR = 1.97, 95% CI = 1.09, 3.58, χ2 (1) = 4.99, p = 0.026] but not with bupropion–SSRI combination [OR = 0.96, 95% CI = 0.52, 1.75, χ2 (1) = 0.02, p = 0.89], than those with such symptoms present.
Discussion
In this large study of treatment-seeking outpatients with chronic or recurrent MDD, half of the participants (50.4%) endorsed at least one symptom of hypomania with decreased need for sleep as the most frequent and psychomotor agitation was the least frequent symptom. Participants with sub-threshold hypomanic symptoms had longer illness duration, higher burden of comorbid disorders and were less likely to remit with antidepressant treatment than those without these symptoms. In these exploratory analyses, the association of sub-threshold hypomanic symptoms with treatment outcome differed among the three treatment arms. Specifically, escitalopram monotherapy and venlafaxine-mirtazapine combinations were less effective in those with sub-threshold hypomanic symptoms than those without these symptoms. But with the bupropion-SSRI combination, remission rates did not differ between those with and without sub-threshold hypomanic symptoms. These associations of baseline sub-threshold hypomanic symptoms with remission continued to be significant even after controlling for baseline covariates.
The proportion of participants with MDD with at least one hypomanic symptom (50.4%)—is comparable to previous studies [6, 26]. Consistent with previous reports, rates of substance use (alcohol) disorder [4, 5], anxiety (social anxiety) disorder [4, 5], and comorbid medical disorder [5] were higher, and duration of index episode was longer [9] in participants with sub-threshold hypomanic symptoms as compared to those without these symptoms. The association of race and ethnicity with the presence of hypomanic symptoms in this report differs from the previous report of McIntyre et al. who did not report any difference in race between MDD patients with and without DSM-5 mixed features specifier [5]. This difference is likely related to the substantially greater proportion of non-white participants in this report (36.1%) as compared to that (10.5%) of McIntyre et al. [5], thus enabling detection of difference among racial groups. Additionally, unlike McIntyre et al., there was no difference in employment status amongst those with or without hypomanic symptoms in this report which may be related to lower rates of employment (41.6%) in McIntyre et al. as compared to 49.8% in this report [5]. The finding of differences in QIDS-SR16 between those with and without hypomanic symptoms differs from that of Angst et al. who did not find any differences in QIDS-SR16 severity thresholds of MDD patients with and without sub-threshold hypomanic symptoms [4].
Previous studies have reported a lifetime pattern of non-response to antidepressant medication in MDD patients with hypomanic symptoms [10], which is consistent with the finding of lower acute-phase remission rates in the CO-MED trial. However, Perlis et al. did not find a significant association between hypomanic/manic symptoms, using six items from the PDSQ [27] with remission outcomes in the Sequenced Treatment Alternatives to Relieve Depression study (STAR*D) study [26]. The difference in findings of Perlis et al. and this report may be related to the tools for assessing symptoms and the number of treatment trials (up to four in STAR*D vs. one in CO-MED). The yes/no questions in PDSQ ask about the last 6 months while the ASRM in this study explicitly asked about varying severity of particular symptom over the prior week. Additionally, the psychometric properties of the PDSQ mania/hypomania questions were poor (test–retest correlation of 0.50) and correlation with other scales of mania was modest (0.51) resulting in the mania subscale being dropped from the final version of PDSQ [27, 28]. In addition, Perlis et al. analyzed their data to determine whether, across several treatment steps, those with features suggesting bipolar spectrum might fare more poorly and be an indicator of treatment-resistant depression. This report evaluated only one treatment step in non-resistant patients with MDD.
This is the first report to demonstrate that the presence of hypomanic symptoms at baseline may help in guiding antidepressant medication selection. Previous reports in well-powered samples, by and large, have not found that pretreatment symptom features, clinical or demographic parameters including baseline depressive symptom severity, chronicity, suicidal ideation, insomnia, melancholic, atypical, or anxious features act as moderators to recommend one treatment over another [29,30,31,32,33,34]. Rather, many of these features, when present, have been indicative of an overall treatment effect that applied across a range of medications [35]. Future prospective clinical trials that assign treatment based on sub-threshold hypomanic symptoms (SSRI monotherapy for those without and bupropion for those with these symptom) are needed to establish the clinical utility. Additional studies are also needed to test whether augmentation with atypical antipsychotic medications such as lurasidone is superior to SSRI monotherapy in MDD patients with sub-threshold hypomanic symptoms [11]. This is especially important, as the presence of mixed features has been associated with poorer response to currently available antidepressant treatments [36, 37].
Based on findings from this report, as well as others, the presence of hypomanic symptoms is common in MDD, and could possibly represent a subtype of depression warranting differential treatment considerations. Symptoms of hypomania appear to have a modest effect on treatment outcome and future efforts to screen for this symptomology in patients presenting with a unipolar diagnosis, prior to treatment initiation, could potentially have clinical value. These efforts will also elucidate whether the effect of sub-threshold hypomanic symptoms on treatment outcome is mediated by other clinical and sociodemographic variables. Whether these hypomanic symptoms wax and wane or are persistent over the course of a treated or untreated MDE is unclear.
This report has several limitations. The analyses were post hoc, thus replication is required. As differential outcomes based on the presence of hypomanic symptoms at baseline was not an a priori identified goal of the CO-MED trial, the analyses in this report may not have been adequately powered to detect these differences. Additionally, ASRM does not assess hypomanic symptoms of flight of ideas or racing thoughts, distractibility, and excessive involvement in activities that have a high potential for painful consequences or risky behaviors [2]. Full-range of mania symptoms could not be assessed and the “mixed features” specifier of DSM-5 was not fully operationalized. By design, the CO-MED trial included a serotonergic antidepressant in each treatment arm and did not include either mood stabilizer or atypical antipsychotic medications, which may have been effective in the presence of sub-threshold hypomanic symptoms.
In conclusion, hypomanic symptoms in MDD are common (occurring in about 50%) of outpatients with non-psychotic MDD and clinically important in informing treatment selection. These symptoms predict poorer acute-phase remission rates with SSRI monotherapy or venlafaxine-mirtazapine combination. The combination of bupropion combined with escitalopram is unaffected by the presence or absence of these hypomanic symptoms.
References
Uher R, Payne JL, Pavlova B, Perlis RH. Major depressive disorder in DSM-5: implications for clinical practice and research of changes from DSM-IV. Depress Anxiety. 2014;31:459–71.
Association AP. Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Publishing; Washington, D.C. 2013.
Koukopoulos A, Sani G. DSM-5 criteria for depression with mixed features: a farewell to mixed depression. Acta Psychiatr Scand. 2014;129:4–16.
Angst J, Cui L, Swendsen J, Rothen S, Cravchik A, Kessler RC, et al. Major depressive disorder with subthreshold bipolarity in the National Comorbidity Survey Replication. Am J Psychiatry. 2010;167:1194–201.
McIntyre RS, Soczynska JK, Cha DS, Woldeyohannes HO, Dale RS, Alsuwaidan MT, et al. The prevalence and illness characteristics of DSM-5-defined “mixed feature specifier” in adults with major depressive disorder and bipolar disorder: results from the International Mood Disorders Collaborative Project. J Affect Disord. 2015;172:259–64.
Sato T, Bottlender R, Schroter A, Moller HJ. Frequency of manic symptoms during a depressive episode and unipolar ‘depressive mixed state’ as bipolar spectrum. Acta Psychiatr Scand. 2003;107:268–74.
Akiskal HS, Benazzi F, Perugi G, Rihmer Z. Agitated “unipolar” depression re-conceptualized as a depressive mixed state: implications for the antidepressant-suicide controversy. J Affect Disord. 2005;85:245–58.
McIntyre RS, Ng-Mak D, Chuang CC, Halpern R, Patel PA, Rajagopalan K, et al. Major depressive disorder with subthreshold hypomanic (mixed) features: a real-world assessment of treatment patterns and economic burden. J Affect Disord. 2017;210:332–7.
Maj M, Pirozzi R, Magliano L, Fiorillo A, Bartoli L. Agitated “unipolar” major depression: prevalence, phenomenology, and outcome. J Clin Psychiatry. 2006;67:712–9.
Smith DJ, Forty L, Russell E, Caesar S, Walters J, Cooper C, et al. Sub-threshold manic symptoms in recurrent major depressive disorder are a marker for poor outcome. Acta Psychiatr Scand. 2009;119:325–9.
Suppes T, Silva R, Cucchiaro J, Mao Y, Targum S, Streicher C, et al. Lurasidone for the treatment of major depressive disorder with mixed features: a randomized, double-blind, placebo-controlled study. Am J Psychiatry. 2016;173:400–7.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33.
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62.
Rush AJ, Trivedi MH, Stewart JW, Nierenberg AA, Fava M, Kurian BT, et al. Combining medications to enhance depression outcomes (CO-MED): acute and long-term outcomes of a single-blind randomized study. Am J Psychiatry. 2011;168:689–701.
Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163:28–40.
Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54:573–83.
Wisniewski SR, Rush AJ, Balasubramani GK, Trivedi MH, Nierenberg AA. Self-rated global measure of the frequency, intensity, and burden of side effects. J Psychiatr Pract. 2006;12:71–9.
Altman E, Hedeker D, Peterson JL, Davis JM. A comparative evaluation of three self-rating scales for acute mania. Biol Psychiatry. 2001;50:468–71.
Altman EG, Hedeker D, Peterson JL, Davis JM. The Altman self-rating mania scale. Biol Psychiatry. 1997;42:948–55.
Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The Inventory of Depressive Symptomatology (IDS): psychometric properties. Psychol Med. 1996;26:477–86.
Kraemer HC, Kupfer DJ. Size of treatment effects and their importance to clinical research and practice. Biol Psychiatry. 2006;59:990–6.
Trivedi MH, Wisniewski SR, Morris DW, Fava M, Gollan JK, Warden D, et al. Concise health risk tracking scale: a brief self-report and clinician rating of suicidal risk. J Clin Psychiatry. 2011;72:757–64.
Mundt JC, Marks IM, Shear MK, Greist JH. The work and social adjustment scale: a simple measure of impairment in functioning. Br J Psychiatry. 2002;180:461–4.
Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49:156–63.
Zimmerman M, Chelminski I. A scale to screen for DSM-IV Axis I disorders in psychiatric out-patients: performance of the Psychiatric Diagnostic Screening Questionnaire. Psychol Med. 2006;36:1601–11.
Perlis RH, Uher R, Ostacher M, et al. Association between bipolar spectrum features and treatment outcomes in outpatients with major depressive disorder. Arch Gen Psychiatry. 2011;68:351–60.
Zimmerman M, Mattia JI. A self-report scale to help make psychiatric diagnoses: the Psychiatric Diagnostic Screening Questionnaire. Arch Gen Psychiatry. 2001b;58:787–94.
Zimmerman M, Mattia JI. The psychiatric diagnostic screening questionnaire: development, reliability and validity. Compr Psychiatry. 2001a;42:175–89.
Sung SC, Haley CL, Wisniewski SR, Fava M, Nierenberg AA, Warden D, et al. The impact of chronic depression on acute and long-term outcomes in a randomized trial comparing selective serotonin reuptake inhibitor monotherapy versus each of 2 different antidepressant medication combinations. J Clin Psychiatry. 2012;73:967–76.
Sung SC, Wisniewski SR, Balasubramani GK, Zisook S, Kurian B, Warden D, et al. Does early-onset chronic or recurrent major depression impact outcomes with antidepressant medications? A CO-MED trial report. Psychol Med. 2013;43:945–60.
Sung SC, Wisniewski SR, Luther JF, Trivedi MH, Rush AJ. Pre-treatment insomnia as a predictor of single and combination antidepressant outcomes: a CO-MED report. J Affect Disord. 2015;174:157–64.
Arnow BA, Blasey C, Williams LM, Palmer DM, Rekshan W, Schatzberg AF, et al. Depression subtypes in predicting antidepressant response: a report from the iSPOT-D trial. Am J Psychiatry. 2015;172:743–50.
Bobo WV, Chen H, Trivedi MH, Stewart JW, Nierenberg AA, Fava M. et al. Randomized comparison of selective serotonin reuptake inhibitor (escitalopram) monotherapy and antidepressant combination pharmacotherapy for major depressive disorder with melancholic features: a CO-MED report. J Affect Disord. 2011;133:467–76.
Friedman ES, Davis LL, Zisook S, Wisniewski SR, Trivedi MH, Fava M. et al. Baseline depression severity as a predictor of single and combination antidepressant treatment outcome: results from the CO-MED trial. Eur Neuropsychopharmacol. 2012;22:183–99.
Rush AJ, Wisniewski SR, Warden D, Luther JF, Davis LL, Fava M. et al. Selecting among second-step antidepressant medication monotherapies: predictive value of clinical, demographic, or first-step treatment features. Arch Gen Psychiatry. 2008;65:870–80.
Perugi G, Medda P, Zanello S, Toni C, Cassano GB. Episode length and mixed features as predictors of ECT nonresponse in patients with medication-resistant major depression. Brain Stimul. 2012;5:18–24.
Rybakowski JK. Bipolarity and inadequate response to antidepressant drugs: clinical and psychopharmacological perspective. J Affect Disord. 2012;136:e13–e19.
Acknowledgements
The CO-MED trial was funded by NIMH (N01 MH-90003) and received medications at no cost from Forest Pharmaceuticals, GlaxoSmithKline, Organon, and Wyeth Pharmaceuticals. This work was also supported in part through the Center for Depression Research and Clinical Care at UT Southwestern, Hersh Foundation, and Jordan Harris Foundation. The authors thank the clinical staff at each clinical site for their assistance with this project; all of the study participants; and Jeremy A. Kee, M.A., for administrative support. The content of this publication does not necessarily reflect the views or policies of the U.S. Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. government. NIMH had no role in the drafting or review of the manuscript or in the collection or analysis of the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Ms. Malchow and Mr. Grannemann have no potential conflicts of interest. Dr. Jha has received contract research support from Acadia Pharmaceuticals and Janssen. Dr. Rush has received consulting fees from Akili, Brain Resource Inc., Compass Inc., Curbstone Consultant LLC, Emmes Corp, Johnson and Johnson (Jannsen), Liva-Nova, Mind Linc., Sunovion, Taj Medical; speaking fees from Liva-Nova; and royalties from Guilford Press and the University of Texas Southwestern Medical Center, Dallas, TX. (for the Inventory of Depressive Symptoms and its derivatives). He is also named co-inventor on two patents: U.S. Patent No. 7,795,033: Methods to Predict the Outcome of Treatment with Antidepressant Medication, Inventors: McMahon FJ, Laje G, Manji H, Rush AJ, Paddock S, Wilson AS and U.S. Patent No. 7,906,283: Methods to Identify Patients at Risk of Developing Adverse Events During Treatment with Antidepressant Medication, Inventors: McMahon FJ, Laje G, Manji H, Rush AJ, Paddock S. Dr. Trivedi, is or has been an advisor/consultant and received fee from: Alkermes, AstraZeneca, Cerecor, Eli Lilly & Company, Lundbeck, Naurex, Otsuka Pharmaceuticals, Pamlab, Pfizer Inc., and Takeda. In addition, he has received grants/research support from National Institute of Mental Health and National Institute on Drug Abuse.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Jha, M.K., Malchow, A.L., Grannemann, B.D. et al. Do baseline sub-threshold hypomanic symptoms affect acute-phase antidepressant outcome in outpatients with major depressive disorder? Preliminary findings from the randomized CO-MED trial. Neuropsychopharmacol 43, 2197–2203 (2018). https://doi.org/10.1038/s41386-018-0180-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-018-0180-z