Abstract
Long-acting injectable contraceptives have been associated with mucosal immune changes and increased HIV acquisition, but studies have often been hampered by the inaccuracy of self-reported data, unknown timing of injection, and interactions with mucosal transmission co-factors. We used mass spectrometry to quantify the plasma concentrations of injectable contraceptives in women from the CAPRISA004 study (n = 664), with parallel quantification of 48 cytokines and >500 host proteins in cervicovaginal lavage. Higher DMPA levels were associated with reduced CVL concentrations of GCSF, MCSF, IL-16, CTACK, LIF, IL-1α, and SCGF-β in adjusted linear mixed models. Dose-dependent relationships between DMPA concentration and genital cytokines were frequently observed. Unsupervised clustering of host proteins by DMPA concentration suggest that women with low DMPA had increases in proteins associated with mucosal fluid function, growth factors, and keratinization. Although DMPA was not broadly pro-inflammatory, DMPA was associated with increased IP-10 in HSV-2 seropositive and older women. DMPA–cytokine associations frequently differed by vaginal microbiome; in non-Lactobacillus-dominant women, DMPA was associated with elevated IL-8, MCP-1, and IP-10 concentrations. These data confirm a direct, concentration-dependant effect of DMPA on functionally important immune factors within the vaginal compartment. The biological effects of DMPA may vary depending on age, HSV-2 status, and vaginal microbiome composition.
Similar content being viewed by others
Introduction
Over 140 million women worldwide use hormonal contraceptives (HCs) and depo-medroxyprogesterone acetate (DMPA) is one of the most common injectable progestins used in sub-Saharan African countries (including South Africa), a region with high HIV prevalence.1,2,3,4 Improved contraceptive choices have provided women control over their reproductive health, decreased unintended pregnancies, reduced risk of maternal and infant mortality, and improved opportunities to advance their education status.5 However, epidemiological studies have suggested that HC use, particularly DMPA, increases HIV acquisition risk.4 Meta-analyses have shown a positive association between DMPA use and HIV infection (~40%–50% increase in risk), although results varied considerably across studies, and debate continues about how biological mechanisms and epidemiologic data might explain HIV–contraceptive associations.1,6,7 As it is young women in southern Africa who prefer DMPA, and are at the highest risk for HIV infection,4 it is important to ascertain whether any increases in HIV risk are due to behavioral and/or biological effects.
Intended to resolve epidemiological controversies around DMPA and HIV, residual confounding in particular, the recent results of a large randomized open-label trial, Evidence for Contraceptive Options and HIV Outcomes (ECHO), reported no significant difference in HIV incidence between intramuscularly delivered DMPA (DMPA-IM) and two other methods of contraception: copper intrauterine device (IUD) and a levonorgestrel (LNG) implant.8 However, the study was limited by lack of a true control group, as most studies that report increased HIV risk among DMPA users is compared with non-injectable HC users or with those using combined oral method.9,10,11,12 Another limitation of ECHO is that the study was only powered to detect 50% increase in HIV risk. Also, it is worth noting that an HIV incidence of 4.2 per 100 women (95% confidence interval: 3.5–4.9) is higher than anticipated, particularly in a clinical trial context. Finally, a statistical trend was observed when comparing HIV incidence between DMPA-IM and LNG-implant group (hazard ratio (HR) = 1.23, p = 0.097 in intent-to-treat analysis); this was stronger in analyses that accounted for contraceptive switching and potential confounders. These concerns temper the interpretation that DMPA is completely safe with respect to HIV acquisition risk.
Studies in non-human primates have demonstrated the effect of contraceptives on simian immunodeficiency virus (SIV) acquisition, yielding more consistent results compared with analogous studies on humans. Studies of rhesus and pigtail macaques demonstrated increased risk of HIV acquisition during the luteal phase of the menstrual cycle, which is progesterone dominated.13,14,15 Furthermore, intramuscular treatment of macaques with 30 mg of DMPA has been observed to substantially reduce vaginal epithelium thickness, a mechanism that has been associated with increased SIV or SHIV acquisition in DMPA-treated macaques.13,16,17,18,19,20 However, even though animal studies provide important proof of concept, it is worth noting the differences in reproductive biology between macaques and humans, and the relatively higher doses of DMPA often used in non-human primate experiments. To address this, Radzio et al.13 demonstrated increases in Cmax of 6.6- and 5-fold AUC0-12wk values after treating macaques with 30 and 3 mg of DMPA, respectively; this yielded Cmax and AUC0-12wk values closer to the ranges observed in humans receiving 150 mg of DMPA.13
Contradicting data regarding intramuscular injection of women with 150 mg of DMPA and vaginal epithelium thinning have been reported.20,21,22,23 A study by Miller et al.22 reported a reduction in the mean number of epithelium cell layers and decreased epithelial thickness in vaginal biopsies of DMPA users. Zalenskaya et al.24 conducted a whole-genome expression profiling of the ectocervical mucosa of DMPA users and reported DMPA use to result in downregulation of genes encoding cell junction proteins desmosomal cadherins desmoglein 1 (DSG1) and desmocollin 2, which are involved in epithelial integrity and differentiation. These latter results agree with those of Quispe et al.,25 who reported enhanced genital mucosal permeability and reduced DSG1α in progestin-treated mice. However, a number of studies have demonstrated that DMPA does not significantly alter the female genital tract epithelium thickness, number of cell layers, and/or the number of Langerhans cells.20,26,27 Therefore, the difference in DMPA dose given could explain the difference in the observed vaginal epithelium thinning between macaques and humans.
In humans, HC use has been associated with changes in genital cytokines and chemokine levels, and antiviral factors in cervicovaginal lavages (CVLs).28,29 Progestins have been positively associated with pro-inflammatory cytokines and HIV risk, likely by activating mucosal HIV target cells.3,26 In contrast, some studies have demonstrated DMPA to be immunosuppressive, resulting in downregulation of both the innate and adaptive immunity, leading to reduced host abilities to fight off invading pathogens.30 Specifically, DMPA has been shown to suppress the production of interleukin (IL)-2, IL-4, IL-6, IL-12, granulocyte colony-stimulating factor (G-CSF), interferon (IFN)-γ, tumor necrosis factor (TNF)-α, and macrophage inflammatory protein (MIP)-1α.31,32,33,34 In addition to reduced pro-inflammatory cytokines, DMPA has been associated with elevated anti-inflammatory IL-1RA in women <25 years of age.28
Therefore, despite a large number of published studies on the topic, to date the exact biological mechanisms that might potentially link DMPA use and increased HIV risk remain unclear. In addition, it has been challenging to accurately quantify the potential biological and behavioral variables that might contribute to DMPA’s associations with HIV acquisition. To better define the mucosal impact of DMPA, we hypothesized that any HIV-associated biological effects of DMPA should be most evident shortly after DMPA injection, in a dose-dependent manner. To address this, we developed a Multiple Reaction Monitoring (MRM) assay utilizing high-performance liquid chromatography (HPLC) in combination with liquid chromatography-tandem triple quadruple mass spectrometry (LC-MS/MS) (HPLC-LC-MS/MS) to measure DMPA, norethisterone enanthate (NET-EN), and progesterone concentrations in plasma samples. We applied this assay to longitudinal samples obtained from South African women enrolled in clinical studies at Centre for the AIDS Programme of Research in South Africa (CAPRISA) to understand the relationship between plasma hormone contraception drug levels and the concentrations of cytokines in the female genital tract.
Results
Study participants
We analyzed plasma specimens from 664 CAPRISA004 participants who had matching CVL cytokine data.35 Of these, 45 women were sampled at more than one pre-infection visit, while an additional 5 women were sampled longitudinally with a minimum of 6 longitudinal samples following acute HIV infection (CAPRISA002). Contraceptive use was part of the inclusion criteria for CAPRISA004; self-reported contraception choices included DMPA (n = 448/664; 67%), NET-EN (n = 112/664; 17%), and non-injectables including combined oral contraceptives, IUD, hysterectomy, and tubal ligation (n = 104/664; 16%; Table 1). Although there was no age difference between participants who self-reported DMPA and NET-EN use (median 22 years, interquartile range (IQR): 20–25 for both groups), women not reporting an injectable contraceptive tended to be older (median 26 years, IQR: 22–31, p < 0.001, Kruskal–Wallis test). Baseline herpes simplex virus (HSV)-2 status was similar between contraceptive groups. HSV-2 was seroprevalent in 50.4% (n = 226) from the DMPA group, 50.5% (n = 56/111) from the NET_EN group, and 56.3% (n = 58/103) from women using other forms of contraception (p = 0.55). A majority of women who reported using DMPA came from the rural vs. urban study site (81.7% vs. 18.3%, respectively; p < 0.001). Condom use differed between groups, with women reporting to “always” use condoms accounting for 23.7%, 41.1%, and 28.8% of the DMPA, NET-EN, and other contraception users, respectively (p = 0.01). There was no significant differences in the number of sex acts reported per month or reporting of genital symptoms by women from the three contraceptive groups.
Kinetics of MPA decay
We used MRM analysis to construct standard curves for each analyte using charcoal plasma specimens with known concentrations ranging from 10 to 10,000 pg/ml for MPA (the form of DMPA measured by mass spectrometry), 1000 to 30,000 pg/ml for NET-EN, and 10 to 20,000 pg/ml for endogenous progesterone (Supplementary Fig. 1). These standards were included in each run to determine the concentration of MPA, NET-EN, and progesterone in plasma samples using HPLC-LC-MS/MS (Supplementary Fig. 2). We estimated the months post DMPA injection (based on self-report) for each of the five women with longitudinal MPA levels measured in CAPRISA002. Peak MPA concentrations were defined as peak serum MPA levels of at least 963 pg/ml that were measured between 2 and 14 days after DMPA injection.36 In our study, peaks were ~3 days after the self-reported day of first DMPA injection, ranging from ~900 to 2400 pg/ml, whereas 30 days after injection the concentrations ranged from 300 to 860 pg/ml (Fig. 1). By 2–3 months post DMPA injection, the median plasma MPA concentration were 170 pg/ml (IQR: 150–190 pg/ml; Fig. 1). Thus, there is some degree of variability in DMPA concentration, which may result from the biological variation in pharmacokinetic decay of DMPA in the blood, accuracy of self-reported injection date, and/or low sample size of the study. Irrespectively, the range of concentrations measured carries the notable advantage of directly measuring relative plasma DMPA levels to correlate to immunological variables. We used these data to create four MPA groups to model cytokine levels, with MPA levels defined as undetectable (0–9 pg/ml), low (≥ 9 and < 300 pg/ml), medium (≥300 and <800 pg/ml), and high (≥ 800 pg/ml) concentrations (Table 2).
Accuracy of self-reported contraceptive use
We observed a strong concordance between self-reported injectable contraceptive use and the detection of the reported injectable contraceptive in the plasma (Table 2). MPA was detected in 97.8% of those who self-reported DMPA use, compared with 17% in participants who self-reported using NET-EN. Upon further inspection, high proportion of the NET-EN-reporting individuals with detectable MPA had low MPA (95%) or medium (5%) MPA concentrations. A minority (8.8%) of participants who reported that they were not using injectable contraceptives had detectable MPA, but in most cases (90%) these were defined as “low” MPA levels. These data suggest that self-report correlates strongly with detection of the injectable contraceptive, in line with a recent report.37
Furthermore, although ~19.8% (89/448) of DMPA users had detectable plasma levels of endogenous progesterone, high concentrations of progesterone (≥238 pg/ml) were detected in only 0.9% (4/448) of DMPA-reporting participants. Similarly, of the 89 women with detectable progesterone, 40.4% (36/89) had detectable low and medium MPA levels, whereas only 5.6% (5/89) had high levels of detectable MPA. None of the women with high plasma MPA had high plasma progesterone levels.
Associations between plasma MPA concentrations and genital cytokines
Cytokines were measured in CVL fluid in all participants35 and correlated to injectable concentration category using linear mixed models. Mutually exclusive study groups were created where only MPA and not NET-EN was detected (and vice versa). In this way, NET-EN-detectable women were excluded from MPA analyses. In unadjusted analyses, 15 cytokines were significantly associated with detectable MPA concentrations. The strongest cytokine associations with MPA were with reduced growth factors (GF): stromal-derived factor (SDF)-1α, stem cell GF (SCGF)-β, Macrophage colony-stimulating factor (MCSF), leukemia inhibitory factor (LIF), and Granulocyte-colony stimulating factor (GCSF) concentrations were all reduced with higher levels of MPA (GCSF and MCSF reduced in all three MPA concentrations). IL-15 was reduced at both medium and low MPA (Fig. 2a and Supplementary Table 1). Several associations were observed for chemokines, with IL-16 and cutaneous T-cell attracting chemokine (CTACK) significantly reduced at high MPA concentrations and regulated upon activation normal T-cell expressed and presumably secreted (RANTES) significantly elevated at low MPA concentrations. At medium MPA concentrations, pro-inflammatory cytokine macrophage migration inhibitory factor (MIF), MIP-1β, IL-18, and IL-8 were significantly elevated, whereas IL-1α was reduced at high MPA concentrations.
a An unadjusted model conducted using 426 samples of n = 390 women with detectable MPA, compared with 98 samples of n = 91 women without detectable contraceptive. b Model adjusting for HSV-2, age, study arm, study site, number of sex acts per month, condom use, and microbial grouping using 356 samples from n = 344 women with MG data and have detectable MPA compared with 90 samples of n = 86 women without detectable contraceptive. Stars denotes the degree of significance: *p < 0.05, **p < 0.01, ***p < 0.001.
Similar results were observed in multivariable analyses adjusting for HSV-2, study arm, study site, age, number of sex acts per month, condom use, and vaginal microbiota grouping, the latter coded as Lactobacillus (LD) vs. non-LD dominant (non-LD; Fig. 2b and Supplementary Table 1).38 These variables were selected as being potentially related to DMPA usage and/or drivers of genital cytokine levels. As vaginal microbiome data were only available for 443 women, we conducted an additional multivariable analysis without including microbial grouping (Supplemental Fig. 3 and Supplementary Table 1); this did not have any substantial impact on the main estimates, with MCSF and GCSF still significantly reduced in all MPA concentrations in a dose-dependent manner. In multivariable analyses, IL-1RA was significantly elevated in medium MPA levels, whereas IL-12p70 and vascular endothelial GF (VEGF) were significantly reduced for high MPA concentration; these were statistical trends in unadjusted models.
MPA and genital cytokine associations were modified by HSV-2, age, and vaginal microbiome grouping
Inconsistent mucosal associations with DMPA could be driven by effect modification, as suggested by several epidemiological studies that have stratified by HSV-2, age, and vaginal microbiome/STI.3,39,40 We used stratification and interaction analyses to determine whether cytokine-DMPA associations were consistent between several potentially modifying factors (Fig. 3). Although the interaction analyses assess whether a third factor impacts a given DMPA–cytokine association, stratification is a useful visualization tool to understand the directions of these differential effects. In HSV-2 seropositive women, detectable MPA trended toward elevated growth regulated (GRO)-α and basic fibroblast GF (FGF), and reduced MCSF; in HSV-2 seronegative women, detectable DMPA trended toward elevated IL-1Rα (interaction p < 0.05; Fig. 3a). Detectable DMPA trended toward increased IL-1RA and monokine induced by γ-IFN (MIG), whereas MCSF was decreased in older women (interaction p < 0.05 for all; Fig. 3b).
Interaction analsysis showing the impact of detectable MPA vs. non-detectable MPA on cervical cytokines stratified by (a) baseline HSV-2, (b) age, and (c) microbial grouping (MG). Pro-inflammatory cytokines (red), chemokines (green), growth factors (purple), adaptive factors (blue), and anti-inflammatory cytokines (gray). Stars denotes the degree of significance: *p < 0.05, **p < 0.01, ***p < 0.001. The P-value of the interaction analysis is represented using boxes: p < 0.05 (red box), p > 0.05, and ≤0.1 (green box), and p > 0.1 and ≤ 0.2 (blue box). For baseline HSV-2 and age, interaction and stratification analysis were conducted using 426 samples of n = 390 women with detectable MPA, compared with 98 samples of n = 91 women without detectable contraceptive, whereas for MG 356 samples of n = 344 women with MG data and have detectable MPA compared with 90 samples of n = 86 women without detectable contraceptive.
Significant interactions were observed between DMPA and microbial grouping for five cytokines: MIG, induced protein-10 (IP-10), IL-6, SGCF-β, and GCSF (interaction p < 0.05). DMPA was associated with increased or decreased concentrations of these cytokines, depending on microbial grouping. In contrast, in LD women, DMPA was associated with significantly reduced GFs (GCSF and MCSF; p < 0.05) and the pro-inflammatory cytokine TNF-α (p < 0.05), whereas the anti-inflammatory cytokine IL-1RA was significantly elevated (p < 0.05; Fig. 3c). In non-LD women, detectable DMPA was associated with increased PDGF-ββ and RANTES, and trended towards elevated pro-inflammatory cytokines, GFs, and chemokines (IP-10, MIG, GRO-α, monocyte chemotactic protein (MCP)-1, RANTES, IL-16, IL-7, platelet-derived GF (PDGF)-ββ, SCGF-β, and IL-8; interaction p < 0.2).
Given the dose dependence of several MPA–cytokine associations, we carried out additional sensitivity analyses with combined low/undetectable MPA specimens and compared these with specimens with medium and high MPA concentrations, which led to minor variation in some of the analysis outcomes (Supplementary Fig. 4). In participants who were HSV-2 seropositive at baseline, high/medium DMPA was associated with reduced genital concentrations of IL-2 and elevated IP-10 concentrations compared with participants with low/undetectable MPA concentrations (p < 0.05). In HSV-2 seronegative women, medium/high MPA was associated with elevated TNF-related apoptosis inducing ligand (TRAIL) (p < 0.05; Supplementary Fig. 4a). Significant HSV-2-DMPA interactions were observed for IP-10 (p = 0.015), TRAIL (p = 0.026), and MIG (p = 0.051). Stratified by age (Supplementary Fig. 4b), we observed that in older women (≥23 years old, i.e., the median age), medium/high MPA was associated with elevated concentrations of MIF, β-nerve GF (β-NGF), IL-18, IP-10, IL-8, IL-1RA, hepatocyte GF (HGF), and MIG, and significantly reduced concentrations of VEGF (p < 0.05). In younger women (≤22 years old), MPA was associated with reduced IL-13 concentrations (p < 0.05). Significant interactions were observed between age and DMPA for MIG, VEGF, IL-13, HGF, and IL-1Rα (p < 0.05), whereas nonsignificant trends were observed for IL-12P70 (p = 0.053) and CTACK (p = 0.054). Stratifying by vaginal microbial groups, medium/high MPA was associated with reduced CVL concentrations of IL-15 in non-LD women and with reduced GCSF and MCP-1 in LD women (p < 0.05; Supplementary Fig. 4c). Together, these data provide several examples of DMPA–cytokine associations that are modified by an external variable, highlighting the complexity of understanding the biological effects of this compound in humans.
Association between detectable DMPA and concentrations of host proteins in CVL that are important for mucosal fluid function
To explore in more depth the biological interactions between DMPA levels and female genital tract immunology, we next examined the potential impact of DMPA concentration on host protein expression using a shotgun proteomic approach, as described elsewhere.41 Hierarchical clustering was carried out to compare additional host proteins present in CVL, as measured by mass spectrometry, which were associated with DMPA use (Fig. 4). A total of 576 host proteins were detected in CVL from all women after quality assurance; of these, 71/576 (12%) significantly correlated with MPA levels, after adjusting for multiple hypothesis testing. As GCSF and MCSF were the CVL cytokines with the strongest MPA associations, we incorporated these into host protein analyses to investigate their associated pathways. Many proteins associated with MPA levels were also associated with GCSF and/or MCSF (Fig. 4a). A heatmap of these data suggest that two major protein clusters (PrC) were observed; PrC1 was a LD-dominated, low-GF, high-MPA branch, which was characterized by significantly elevated epidermal barrier factors such as CASP14, ANXA1, SPRR3, and IVL (p = 0.00296, false discovery rate = 0.3; Fig. 4b). In contrast, PrC2 was characterized by low MPA concentration, high GF, and both microbial groupings. Factors in PrC2 included those important for mucosal fluid function including mucins (MUC16, MUC5B, and PIGR, which binds mucosal antibodies to aid in aggregation), keratinization factors, and structural components (TGM, SPRR2F, TMPRSS11d, and CILP), GFs (HDGF and CILP), protein processing factors (CPB), and integrin binding factors (CD177). The two main PrCs could be further divided into four sub-branches; in doing this, it became evident that sub-branches 1B and 2A contained a higher frequency of women with undetectable MPA (p < 0.00001) and higher concentrations of both MCSF (p = 0.00003) and a similar trend for GCSF (p = 0.05, Fig. 4c). These data suggest that additional biological pathways related to mucosal integrity can be differentiated by a combination of plasma MPA concentrations and genital GF expression.
Protein clusters with MPA/growth factor levels showing (a) the number of proteins which were associated with MPA levels. b Hierarchical cluster analysis of proteins associated with MPA levels formed four sub-branches based on protein expression patterns. c Quartile figures were used to show the frequency of women associated with MPA, MCSF, and GCSF levels.
Discussion
Despite some controversy surrounding the interpretation of the ECHO trial,8 the high number of HIV infections in all study groups underscores the urgent need to understand biological mechanisms by which contraceptives impact the genital immune milieu in women. Changes in cytokine concentrations in the lower reproductive tract have been previously associated with the risk of HIV acquisition42,43 and could provide a mechanistic link between DMPA and relative risk. We hypothesized that if a direct relationship exists between DMPA and genital cytokines, this association would be dose dependent and strongest shortly after injection, when contraceptive concentrations were highest. To answer this, we established an affordable, sensitive technique to quantify HCs and progesterone in plasma samples collected from South African women of whom we also compiled a large mucosal cytokine dataset.35 In addition to studying dose dependency, this approach also helps to control for the uncertainty of self-reported DMPA use common to many studies. Several measures of internal validity are evident within our assay, including that our results are in line with literature that describes DMPA inhibiting ovulation, typically keeping serum progesterone levels below 0.40 ng/ml in DMPA users.44
Our results do not suggest that DMPA is broadly inflammatory. Indeed, we found that the strongest associations between DMPA and genital cytokines were the reduction in M-CSF and G-CSF. Previous studies have associated DMPA with immunosuppression of the genital tract, which could be consistent with a reduction in G-CSF,22,45,46 which is associated with the recruitment of neutrophils to counteract infection.47,48,49 However, this may not be a direct effect, as increased levels of neutrophils factors in the genital tract have been associated with increased HIV acquisition risk in several studies.50 Alternatively, downregulation of these GFs could be associated with impairment of the mucosal barrier, as G-CSF is known to directly promote epithelial barrier repair.51 Also, G-CSF treatment has been shown to promote impairment and wound healing after burn trauma.52,53,54 Likewise, M-CSF is associated with the polarization of M2 macrophages, which help to limit excessive inflammation and promote wound repair.55 Topical application of M-CSF has been reported to promote wound healing.56 Therefore, one could hypothesize that reduction in these two cytokines could be detrimental in women who suffer abrasions during sex or other forms of mucosal injury, thus potentially increasing HIV risk. Another explanation for HIV risk could lie in the moderate elevation of pro-inflammatory cytokines including IL-8, MIP-1β, MIF, and IL-18, particularly in sub-groups of participants with other sources of genital inflammation.
Although contradictory data on the association between DMPA and HIV have been attributed to studies relying on self-report, we observed a strong association between self-reported injectable use and detection of contraceptive compounds in plasma. Self-reported DMPA use was highly accurate; 98% (472/482) of those with “detectable” MPA self-reported DMPA use, whereas MPA was detected, mostly at very low levels, only in 16.7% participants who reported NET-EN use and in 9.4% of those who reported no-HC use. However, it is also of interest that DMPA levels varied greatly within the small number of individuals where we had longitudinal measurements available, even close to the reported timing of DMPA injection. Therefore, given that we observed a dose-dependent effect of DMPA on several cytokines, it is clear that empirical detection of DMPA in plasma is a useful tool to increase the specificity of any future studies examining the biological impact of DMPA in the female genital tract.
Several studies suggest that the association between DMPA use and HIV risk may be subject to sub-group effects, whereby different women respond to DMPA differently; these include groups defined by HSV-2 (seroprevalence), age, and bacterial vaginosis.3,39,40 We addressed whether similarly the host immune associations of DMPA might differ when stratified by these variables. In HSV-2 seropositive women, DMPA trended toward reduced IL-5, IL-12p70, M-CSF, VEGF and elevated IP-10, MCP-1, basic-FGF, and GRO-α, whereas in HSV-2-negative women, DMPA trended toward elevated levels of the anti-inflammatory cytokine IL-1RA. IL-12 production has been associated with immune activation.57 As we highlighted earlier, elevated IP-10 has been associated with increased risk of HIV infection; therefore, the reduction in IL-5, IL-12p70, M-CSF, VEGF, and elevation of IFN-γ IP-10 in HSV-2-positive samples with detectable MPA could result in an increased risk of HIV acquisition in DMPA users who are HSV-2+. We observed pro-inflammatory cytokines and chemokines, which have been previously associated with increased HIV risk being elevated in women with non-LD vaginal microbiota; these women appeared to have more genital inflammation due to observed elevation of four of the cytokines, IL-8, IL-7, IP-10, and IL-6, which have been previously reported to be pro-inflammatory and to be associated with increased HIV risk.43 Also, women with non-LD vaginal microbiota had significantly elevated RANTES concentrations in CVL. Fichorova et al.58 reported a positive association between cervical RANTES and risk of HIV seroconversion. This could mean that a combined DMPA-vaginal microbiota phenotype is immunologically distinct from DMPA in another context, highlighting the importance of understanding these effects in large, well powered human cohorts.
A healthy vagina is dominated by LD species, whereas bacterial vaginosis (BV) is characterized by alterations in genital microbiota including the presence of Gardnerella vaginalis and other anerobes.59,60,61 BV has been associated with an increased risk of HIV acquisition, with potential mechanisms including epithelial barrier disruption and increased pro-inflammatory cytokines.38,41,62 As previous studies have shown that BV induces pro-inflammatory cytokines, our finding of elevated chemokines (including IL-8, MCP-1, and IP-10) in MPA-detectable non-LD women suggests that MPA may exacerbate genital inflammation in women with molecular-BV,63 which could in turn predispose them to increased risk of HIV infection.
Some studies have reported that HCs such as DMPA are pro-inflammatory.28,64 We found that CVL concentrations of IL-8, MIP-1β, MIF, and IL-18 were positively associated with detection of medium plasma concentrations of MPA, in unadjusted analysis. This could be important, given that genital MIP-1β and IL-8 have been associated with increased risk for SIV43,65 and HIV infection in CAPRISA004.43,66 We have previously reported that mucosa-biased gradients (plasma:CVL) of IL-8, MIP-1β, and IP-10 were associated with the increased risk of acquiring HIV infection.42 However, in multivariable analysis, only one pro-inflammatory cytokine (MIF) and one anti-inflammatory cytokine (IL-1RA) were significantly elevated. It appears, however, that elevated pro-inflammatory cytokines in CVLs from women with detectable MPA to be attributed by potential mediators such as HSV-2 (seropositivity) and non-LD microbiota. In agreement with previous studies,67,68 detectable MPA in our analysis was primarily associated with reduction in many pro-inflammatory cytokines. It will be advisable for future studies, including secondary studies arising from ECHO trial, to also consider variables such as HSV-2 serostatus and BV in particular, which could possibly bias or alter DMPA’s association with inflammation. It is difficult to rule these effects out in ECHO, e.g., the HR for DMPA vs. LNG was 1.36 compared with 1.08 in HSV-2+ vs. HSV-2− women (both not significant). Furthermore, development of model systems that could incorporate analyses of sub-group effects may clarify the underlying biology of this injectable contraceptive. Future studies can assess the implication of upregulated cervical IP-10 in HSV-2 seropositive women. Therefore, in the sub-analysis of the ECHO samples, it would be interesting to determine whether DMPA was inflammatory in different sub-groups of women at risk of HIV infection. More broadly, it would be interesting for future studies that study the effect of DMPA on TB to measure G-CSF and M-CSF on lung biopsies and correlate the cytokine levels with TB outcome.
Previously, DMPA use was associated with protein signatures of epithelial wounding and decreased amount of proteins important for epithelial repair.24,69 This is consistent with the reduction of GCSF and MCSF, given the role of these cytokines in promoting epithelial barrier repair. However, in our host proteomic analysis, we found that women with LD microbiota, low GF expression, and high MPA levels clustered together, reiterating the conclusion that MPA’s mucosal impact may be context dependent. In this cluster, there was evidence for elevated concentrations of factors important for mucosal fluid function (including MUC16 and MUC5B), growth, protein processing, and integrin binding related to maintenance of the epidermal barrier. MUC16, a member of the mucin family glycoproteins, lines the endocervix, endometrium, and fallopian tubes of the female reproductive tract, providing a physical barrier against pathogens such as HIV. Similarly, MUC5B (isolated from saliva) has been shown to inhibit HIV-1 activity in vitro.70,71 The observed changes in mucins is in line with previous observations that DMPA prevents pregnancy, in part, through thickening cervical mucus which prevent fertilization.72
Our study has some limitations. The data are based on a secondary analysis of the CAPRISA004 microbicide trial, a cohort that was not designed to study the effect of HC on the genital mucosa. Therefore, we did not have a large control group, with only 98 samples without detectable HCs. Also, the first day of DMPA injection kinetics analysis was self-reported and we only had five women with clear peaks that we could use for our kinetics analyses. We also did not conduct any cellular work to confirm how exactly MPA use affected immune cells in the genital tract. We also did not measure estrogen concentrations to determine whether participants with low detectable MPA levels had high estrogen levels, as has been reported previously.73,74 Although we did not correct for multiple comparisons in the cytokine analyses, we conclude that most cytokines did not show any association and the strongest associations with GFs pass stringent multiple test corrections.
Nevertheless, the strengths of our study included that we were able to use sensitive tools to accurately detect hormones in plasma samples. Our sample size was relatively large, allowing for stratification for important potential confounders, and also our ability to stratify hormones levels into low, medium, and high levels that could be related directly to the decay kinetics that occur in vivo.
In conclusion, our study showed DMPA to be associated with a broadly immunosuppressive profile in adjusted analyses, with reduced expression of GFs (particularly GCSF and MCSF). Stratified and interaction analyses demonstrated that detectable MPA was associated with elevated genital pro-inflammatory cytokines in HSV-2 seropositive and/or non-LD women. This could mean that DMPA alone is not broadly pro-inflammatory, but has different effects in different sub-groups of women. Host proteome analyses suggested an association between low DMPA concentrations, high GF expression, and factors important for mucosal fluid function (such as mucins). In contrast, LD women with higher MPA but lower GF concentrations were associated with elevated epithelial barrier factors. These data have important implications for understanding the biological effects of injectable HCs in women at high risk of HIV infection. These data may also have implications for other diseases that feature immunosuppression, such as TB and cancer; since DMPA appears to immunosuppressive itself, its use could exacerbate these conditions—although more evidence will need to be generated in this regard.
Materials and methods
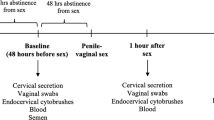
Study design
This is a cross-sectional study, with a subset of participants sampled longitudinally, to assess dose-dependent effects of MPA on the cervical microenvironment of the female reproductive tract of CAPRISA004 participants. The CAPRISA004 was a randomized placebo-controlled double-blinded study that assessed the safety and efficacy of tenofovir 1% gel trial in preventing HIV infection. It was conducted between May 2007 and March 2010 in KwaZulu-Natal, South Africa, by CAPRISA from two sites in KwaZulu-Natal: Vulindlela (rural) and eThekwini (urban).75 CAPRISA002 is a prospective cohort study enrolling participants with acute HIV infection, with frequent sampling within the first year of HIV diagnosis.76 Samples were not collected in women who tested positive for pregnancy in monthly urine screening.77 All participants provided informed, written consent for study participation and specimen storage, and the study was approved by the Biomedical Research Ethics Committee at the University of KwaZulu-Natal (BE028/17).
Sample preparation
Specimens were selected to match those for which matching mucosal cytokine data were available, with most participants sampled once but a small subset sampled at multiple time points to measure inflammation over time. Methods for hormone quantification were modified from Augustine et al.78 Acid citrate dextrose plasma samples, which were previously stored at −80 °C were used. Cryovials were thawed on ice and transferred into Eppendorf tubes. Each sample was spiked with 10 µl of 103 nM progesterone-D9 (internal standard) and then 20 µl of 90% methanol was added and incubated on ice for 1 h. Ethyl acetate-hexane (80:20) was then added for hormone extraction. The mixture was vortexed at room temperature thoroughly to mix the sample and centrifuged at 300 × g for 5 min. After centrifugation, the organic phase was collected into a separate Eppendorf tube and washed with 0.1 M ammonium formate (pH 9.0). The top layer from the wash-step was transferred into a glass vial and dried under a stream of nitrogen gas. Dried samples were reconstituted in H2O: formic acid: MeOH (49:1:50) and briefly vortexed to concentrate the sample in the base of the glass vial. Samples were then transferred into micro-inserts in auto sampler glass vials and ran in HPLC-LC/MS/MS.
Mass spectrometry analysis
HPLC in combination with LC-MS/MS was used for MRM analysis of MPA, progesterone, and NET-EN. The Agilent Technologies 1200 Series was used for HPLC. MPA, PROG, and NET-EN were separated using a Phenomenex C-18 (50 × 2.10 mm) analytical column. Formic acid (0.1%) in HPLC water was used as mobile phase A, whereas mobile phase B consisted of 0.1% formic acid in HPLC acetonitrile. The gradient with a total run time of 23 min per sample was used and a flow rate of 200 µL/min was held constant. The column oven was maintained at −4 °C with a sample injection of 20 µl. Analytes were detected using ABSciEx Q-TRAP 5500 mass spectrometer with an electrospray ionization in a positive ion mode and MRM to measure the precursor-to-product ion transition. Analyst Software (version 1.6) was used for analyzing MRM data obtained from HPLC-LC-MS/MS.
The peak area of standards and patient plasma was used to determine the concentration of the hormones in each samples. Lower limit of detection (LLOD) for MPA was 0.1 ng/ml (100 pg/ml) with calculated signal-to-noise (S/N) ratio of 3.53 and the lower limit of quantification (LOQ) was 50 pg/ml. The LLOD for NET-EN was 75 pg/ml and LOQ was 250 pg/ml, whereas LLOD for progesterone was 10 pg/ml and LOQ was 50 pg/ml. All samples were run in duplicate.
Cytokine measurement in CVL samples
Quantification of 48 cytokines (Bio-Plex Pro Human Cytokine Group I 27-Plex Panel and Group II 21-Plex Panel; Bio-Rad Laboratories, Inc.; Hercules, CA, USA) was carried out using undiluted CVL samples using Luminex multiplexing technology.35 The cytokine panel included the following pro-inflammatory, hematopoietic, regulatory, adaptive, and/or growth-related cytokines: IL-1β, IL-1Rα, IL-2, IL-4, IL-5, IL-6, IL-7, IL-8, IL-9, IL-10, IL-12p70, IL-12p40, IL-16, IL-18, IL-1α, IL-2Rα, IL-3, IL-13, IL-15, IL-17, basic-FGF, CTACK, eotaxin, G-CSF, granulocyte macrophage colony-stimulating factor, GRO-α, HGF, IFN-γ, IFN-α2, IFN IP-10, LIF, MCP-1, MCP-3, M-CSF, MIG, MIF, MIP-1α, MIP-1β, NGF-β, PDGF-ββ, RANTES, stem cell factor, SCGF-β, SDF-1α, TNF-α, TNF-β, TRAIL, and VEGF. All cytokines were measured using Bio-Plex Pro Human Cytokine kits and a Bio-Plex MagPix Array Reader (Bio-Rad Laboratories). Data were collected using Bio-Plex Manager software version 6 and a 5-PL regression formula was used to calculate sample concentrations from the standard curves.
Statistical analyses
We tested for an association between baseline self-reported contraceptive type and different covariates by using Kruskal–Wallis test for continuous variables and χ2-test/Fisher’s exact test for categorical variables. Cytokine levels below the LLOD of the assay were reported as half the lowest concentrations measured for each cytokine. To minimize the effect of inter-plate variability, CVL samples from the same participant were analyzed on the same plate. We used multivariable linear mixed model to assess the effect of MPA concentrations, modeled as an ordinal variable based on cut-offs established in longitudinal analyses. Separate models were used for each log10 cytokine concentration as the outcome. In these models, variance components covariance structure was used, with a random intercept. Models were adjusted for the following covariates: age, study arm, study site, number of sex acts, condom use, vaginal microbiome group, HSV-2 serology, and detection of progesterone in the plasma. Microbiome data were generated from CVL supernatants using shotgun MS approaches, as described in ref. 41 Women were classified as either LD or non-LD, based on abundance of microbial proteins that were quantified. We used stratification and interaction analyses to assess how HSV-2 serostatus, age, and vaginal microbial group modified DMPA–cytokine associations. The selection of these variables was based a priori on literature surrounding DMPA and effect modification. GraphPad Prism version 7.03, SAS version 9.4, and SPSS version 25 were used for statistical analyses.
Proteomics analyses
Metaproteome data analysis was carried out as performed previously elsewhere.38 Mascot (v2.4, Matrix Science, Boston, MA) was used to compare peptides with a curated database that included the many vaginally relevant bacterial genera: LD, Gardnerella, Pseudomonas, Mobiluncus, Ruminococcus, Prevotella, Ruegeria, Bifidobacterium, Megasphaera, Pedobacter, Streptococcus, Escherichia, Atopobium, Dialister, Fusobacterium, Peptoniphilus, Peptostreptococcus, Porphyromonas, Shuttleworthia, and Sneathia (UniProt SwissProtKB/TrEMBL, 2015). Women with >50% of all bacterial proteins falling under the LD genus were categorized as LD; the remainder were considered to be nnon-LD. Hierarchical cluster analyses of proteins significantly associated with MPA and G-CSF/M-CSF were used to define major host protein clusters. Correlations were run using groups defined by no detectable MPA, low MPA, medium MPA, and high MPA, and also by concentrations of the two cytokines (M-CSF and G-CSF). Enrichment of variables in major or sub-branches was determined determined using χ2- or Fisher’s exact tests.
References
Morrison, C. S. et al. Hormonal contraception and the risk of HIV acquisition: an individual participant data meta-analysis. PLoS Med. 12, e1001778 (2015).
Noguchi, L. M. et al. Risk of HIV-1 acquisition among women who use diff erent types of injectable progestin contraception in South Africa: a prospective cohort study. Lancet HIV 2, e279–e287 (2015).
Smith-McCune, K. K. et al. Effects of depot-medroxyprogesterone acetate on the immune microenvironment of the human cervix and endometrium: implications for HIV susceptibility. Mucosal Immunol. 10, 1270–1278 (2017).
Hapgood, J. P., Kaushic, C. & Hel, Z. Hormonal contraception and HIV-1 acquisition: biological mechanisms. Endocr. Rev. 39, 36–78 (2018).
Huijbregts, R. P., Michel, K. G. & Hel, Z. Effect of progestins on immunity: medroxyprogesterone but not norethisterone or levonorgestrel suppresses the function of T cells and pDCs. Contraception 90, 123–129 (2014).
Ralph, L. J., Gollub, E. L. & Jones, H. E. Hormonal contraceptive use and women's risk of HIV acquisition: priorities emerging from recent data. Curr. Opin. Obstet. Gynecol. 27, 487–95. (2015).
Ralph, L. J. et al. Hormonal contraceptive use and women's risk of HIV acquisition: a meta-analysis of observational studies. Lancet Infect. Dis. 15, 181–189 (2015).
Evidence for Contraceptive Options and HIV Outcomes (ECHO) Trial Consortium. HIV incidence among women using intramuscular depot medroxyprogesterone acetate, a copper intrauterine device, or a levonorgestrel implant for contraception: a randomised, multicentre, open-label trial. Lancet 394, 303–313 (2019).
Kiddugavu, M. et al. Hormonal contraceptive use and HIV-1 infection in a population-based cohort in Rakai, Uganda. Aids 17, 233–240 (2003).
Morrison, C. S. et al. Hormonal contraception and the risk of HIV acquisition among women in South Africa. Aids 26, 497–504 (2012).
Crook, A. M. et al. Injectable and oral contraceptives and risk of HIV acquisition in women: an analysis of data from the MDP301 trial. Hum. Reprod. (Oxf., Engl.) 29, 1810–1817 (2014).
Heffron, R. et al. Use of hormonal contraceptives and risk of HIV-1 transmission: a prospective cohort study. Lancet Infect. Dis. 12, 19–26 (2012).
Radzio, J. et al. Physiologic doses of depot-medroxyprogesterone acetate do not increase acute plasma simian HIV viremia or mucosal virus shedding in pigtail macaques. AIDS 28, 1431–1439 (2014).
Sodora, D. L. et al. Vaginal transmission of SIV: assessing infectivity and hormonal influences in macaques inoculated with cell-free and cell-associated viral stocks. AIDS Res Hum. Retroviruses 14(Suppl 1), S119–S123 (1998).
Vishwanathan, S. A. et al. High susceptibility to repeated, low-dose, vaginal SHIV exposure late in the luteal phase of the menstrual cycle of pigtail macaques. J. Acquir. Immune Defic. Syndr. 57, 261–264 (2011).
Sanders-Beer, B. et al. Depo-Provera(®) does not alter disease progression in SIVmac-infected female Chinese rhesus macaques. AIDS Res. Hum. Retroviruses 26, 433–443 (2010).
Hild-Petito, S. et al. Effects of two progestin-only contraceptives, Depo-Provera and Norplant-II, on the vaginal epithelium of rhesus monkeys. AIDS Res. Hum. Retroviruses 14(Suppl 1), S125–S130 (1998).
Trunova, N. et al. Progestin-based contraceptive suppresses cellular immune responses in SHIV-infected rhesus macaques. Virology 352, 169–177 (2006).
Veazey, R. S. et al. Prevention of virus transmission to macaque monkeys by a vaginally applied monoclonal antibody to HIV-1 gp120. Nat. Med. 9, 343–346 (2003).
Mauck, C. K. et al. The effect of one injection of Depo-Provera on the human vaginal epithelium and cervical ectopy. Contraception 60, 15–24 (1999).
Achilles, S. L. & Hillier, S. L. The complexity of contraceptives: understanding their impact on genital immune cells and vaginal microbiota. AIDS (London, England) 27, (S5–S15 (2013).
Miller, L. et al. Depomedroxyprogesterone-induced hypoestrogenism and changes in vaginal flora and epithelium. Obstet. Gynecol. 96, 431–439 (2000).
Ildgruben, A. K., Sjoberg, I. M. & Hammarstrom, M. L. Influence of hormonal contraceptives on the immune cells and thickness of human vaginal epithelium. Obstet. Gynecol. 102, 571–582 (2003).
Zalenskaya, I. A. et al. Use of contraceptive depot medroxyprogesterone acetate is associated with impaired cervicovaginal mucosal integrity. J. Clin. Investig. 128, 4622–4638 (2018).
Quispe Calla, N. E. et al. Medroxyprogesterone acetate and levonorgestrel increase genital mucosal permeability and enhance susceptibility to genital herpes simplex virus type 2 infection. Mucosal Immunol. 9, 1571–1583 (2016).
Chandra, N. et al. Depot medroxyprogesterone acetate increases immune cell numbers and activation markers in human vaginal mucosal tissues. AIDS Res. Hum. Retroviruses 29, 592–601 (2013).
Bahamondes, L. et al. The effect upon the human vaginal histology of the long-term use of the injectable contraceptive Depo-Provera. Contraception 62, 23–27 (2000).
Morrison, C. et al. Cervical inflammation and immunity associated with hormonal contraception, pregnancy, and HIV-1 seroconversion. J. Acquir. Immune Defic. Syndr. 66, 109–117 (2014).
Fleming, D. C. et al. Hormonal contraception can suppress natural antimicrobial gene transcription in human endometrium. Fertil. Steril. 79, 856–863 (2003).
Huijbregts, R. P. et al. Hormonal contraception and HIV-1 infection: medroxyprogesterone acetate suppresses innate and adaptive immune mechanisms. Endocrinology 154, 1282–1295 (2013).
Kleynhans, L. et al. The contraceptive depot medroxyprogesterone acetate impairs mycobacterial control and inhibits cytokine secretion in mice infected with Mycobacterium tuberculosis. Infect. Immun. 81, 1234–1244 (2013).
Francis, S. C. et al. Immune activation in the female genital tract: expression profiles of soluble proteins in women at high risk for HIV infection. PLoS ONE 11, e0143109–e0143109 (2016).
Keller, M. J. et al. PRO 2000 elicits a decline in genital tract immune mediators without compromising intrinsic antimicrobial activity. AIDS 21, 467–476 (2007).
Fichorova, R. N. Guiding the vaginal microbicide trials with biomarkers of inflammation. J. Acquir. Immune Defic. Syndr. 37(Suppl 3), S184–S193 (2004).
McKinnon, L. R. et al. Genital inflammation undermines the effectiveness of tenofovir gel in preventing HIV acquisition in women. Nat. Med. 24, 491–496 (2018).
Halpern, V. et al. Pharmacokinetics of subcutaneous depot medroxyprogesterone acetate injected in the upper arm. Contraception 89, 31–35 (2014).
Pyra, M. et al. Concordance of self-reported hormonal contraceptive use and presence of exogenous hormones in serum among African women. Contraception 97, 357–362 (2018).
Klatt, N. R. et al. Vaginal bacteria modify HIV tenofovir microbicide efficacy in African women. Science 356, 938–945 (2017).
Roxby, A. C. et al. Changes in vaginal microbiota and immune mediators in HIV-1-seronegative Kenyan women initiating depot medroxyprogesterone acetate. J. Acquir. Immune Defic. Syndr. 71, 359–366 (2016).
Polis, C. B. et al. Assessing the effect of hormonal contraception on HIV acquisition in observational data: challenges and recommended analytic approaches. AIDS (Lond., Engl.) 27(Suppl 1), S35–S43 (2013).
Zevin, A. S. et al. Microbiome composition and function drives wound-healing impairment in the female genital tract. PLoS Pathog. 12, e1005889 (2016).
Liebenberg, L. J. et al. Genital-systemic chemokine gradients and the risk of HIV acquisition in women. J. Acquir. Immune Defic. Syndr. 74, 318–325 (2017).
Masson, L. et al. Genital inflammation and the risk of HIV acquisition in women. Clin. Infect. Dis. 61, 260–269 (2015).
Mishell, D. R. Jr Pharmacokinetics of depot medroxyprogesterone acetate contraception. J. Reprod. Med. 41(5 Suppl), 381–390 (1996).
Kleynhans, L. et al. Medroxyprogesterone acetate alters Mycobacterium bovis BCG-induced cytokine production in peripheral blood mononuclear cells of contraceptive users. PLoS ONE 6, e24639 (2011).
Michel, K. G. et al. Effect of hormonal contraception on the function of plasmacytoid dendritic cells and distribution of immune cell populations in the female reproductive tract. J. Acquir. Immune Defic. Syndr. 68, 511–518 (2015).
Bendall, L. J. & Bradstock, K. F. G-CSF: from granulopoietic stimulant to bone marrow stem cell mobilizing agent. Cytokine Growth Factor Rev. 25, 355–367 (2014).
Xu, S. et al. Granulocyte colony-stimulating factor (G-CSF) induces the production of cytokines in vivo. Br. J. Haematol. 108, 848–853 (2000).
Keiser, P. et al. Granulocyte colony-stimulating factor use is associated with decreased bacteremia and increased survival in neutropenic HIV-infected patients. Am. J. Med. 104, 48–55 (1998).
Hensley-McBain, T. & Klatt, N. R. The dual role of neutrophils in HIV infection. Curr. HIV/AIDS Rep. 15, 1–10 (2018).
Paris, A. J. et al. Neutrophils promote alveolar epithelial regeneration by enhancing type II pneumocyte proliferation in a model of acid-induced acute lung injury. Am. J. Physiol. Lung Cell Mol. Physiol. 311, L1062–l1075 (2016).
Eroglu, E. et al. Effects of granulocyte-colony stimulating factor on wound healing in a mouse model of burn trauma. Tohoku J. Exp. Med. 204, 11–16 (2004).
Huang, H. et al. Granulocyte-colony stimulating factor (G-CSF) accelerates wound healing in hemorrhagic shock rats by enhancing angiogenesis and attenuating apoptosis. Med. Sci. Monit. 23, 2644–2653 (2017).
Shen, G.-Y. et al. Local injection of granulocyte-colony stimulating factor accelerates wound healing in a rat excisional wound model. Tissue Eng. Regenerative Med. 13, 297–303 (2016).
Keane, T. J. et al. Restoring mucosal barrier function and modifying macrophage phenotype with an extracellular matrix hydrogel: potential therapy for ulcerative colitis. J. Crohns Colitis 11, 360–368 (2017).
Li, Y., Jalili, R. B. & Ghahary, A. Accelerating skin wound healing by M-CSF through generating SSEA-1 and -3 stem cells in the injured sites. Sci. Rep. 6, 28979–28979 (2016).
Byrnes, A. A. et al. Immune activation and IL-12 production during acute/early HIV infection in the absence and presence of highly active, antiretroviral therapy. J. Leukoc. Biol. 84, 1447–1453 (2008).
Fichorova, R. N. et al. The contribution of cervicovaginal infections to the immunomodulatory effects of hormonal contraception. MBio 6, e00221–15 (2015).
Spear, G. T., St John, E. & Zariffard, M. R. Bacterial vaginosis and human immunodeficiency virus infection. AIDS Res. Ther. 4, 25–25 (2007).
Antonio, M. A., Hawes, S. E. & Hillier, S. L. The identification of vaginal Lactobacillus species and the demographic and microbiologic characteristics of women colonized by these species. J. Infect. Dis. 180, 1950–1956 (1999).
Fredricks, D. N., Fiedler, T. L. & Marrazzo, J. M. Molecular identification of bacteria associated with bacterial vaginosis. N. Engl. J. Med. 353, 1899–1911 (2005).
Anahtar, M. N. et al. Cervicovaginal bacteria are a major modulator of host inflammatory responses in the female genital tract. Immunity 42, 965–976 (2015).
McKinnon, L. R. et al. The evolving facets of bacterial vaginosis: implications for HIV transmission. AIDS Res. Hum. Retroviruses 35, 219–228 (2019).
Deese, J. et al. Injectable progestin-only contraception is associated with increased levels of pro-inflammatory cytokines in the female genital tract. Am. J. Reprod. Immunol. 74, 357–367 (2015).
Li, Q. et al. Glycerol monolaurate prevents mucosal SIV transmission. Nature 458, 1034–1038 (2009).
Passmore, J. A., Jaspan, H. B. & Masson, L. Genital inflammation, immune activation and risk of sexual HIV acquisition. Curr. Opin. HIV AIDS 11, 156–162 (2016).
Ngcapu, S. et al. Lower concentrations of chemotactic cytokines and soluble innate factors in the lower female genital tract associated with the use of injectable hormonal contraceptive. J. Reprod. Immunol. 110, 14–21 (2015).
Govender, Y. et al. The injectable-only contraceptive medroxyprogesterone acetate, unlike norethisterone acetate and progesterone, regulates inflammatory genes in endocervical cells via the glucocorticoid receptor. PLoS ONE 9, e96497 (2014).
Birse, K. D. et al. Genital injury signatures and microbiome alterations associated with depot medroxyprogesterone acetate usage and intravaginal drying practices. J. Infect. Dis. 215, 590–598 (2017).
Gunn, B. et al. Enhanced binding of antibodies generated during chronic HIV infection to mucus component MUC16. Mucosal Immunol. 9, 1549–1558 (2016).
Habte, H. H. et al. Anti-HIV-1 activity of salivary MUC5B and MUC7 mucins from HIV patients with different CD4 counts. Virol. J. 7, 269–269 (2010).
Butler, K. et al. A depot medroxyprogesterone acetate dose that models human use and its effect on vaginal SHIV acquisition risk. J. Acquir. Immune Defic. Syndr. 72, 363–371 (2016).
Cundy, T. et al. A randomized controlled trial of estrogen replacement therapy in long-term users of depot medroxyprogesterone acetate. J. Clin. Endocrinol. Metab. 88, 78–81 (2003).
Torgrimson, B. N. et al. Depot-medroxyprogesterone acetate and endothelial function before and after acute oral, vaginal, and transdermal estradiol treatment. Hypertension (Dallas, Tex.: 1979) 57, 819–824 (2011).
Abdool Karim, Q. et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science 329, 1168–1174 (2010).
Mlisana, K. et al. Rapid disease progression in HIV-1 subtype C-infected South African women. Clin. Infect. Dis. 59, 1322–1331 (2014).
Matthews, L. T. et al. Women with pregnancies had lower adherence to 1% tenofovir vaginal gel as HIV preexposure prophylaxis in CAPRISA 004, a phase IIB randomized-controlled trial. PLoS ONE 8, e56400 (2013).
Augustine, M. S. Medroxyprogesterone acetate and progesterone measurement in human serum: assessments of contraceptive efficacy. J. Anal. Bioanal. Tech. s5. 2014.
Acknowledgements
We thank all of the CAPRISA002 and 004 study participants, and the clinical and laboratory staff who worked on these studies. This project was funded by the Canadian Institutes of Health Research CIHR) (A.D.B., L.R.M. TMI 138658). R.P.M. was previously funded by the South African National Research Foundation (NRF) PhD Scholarship and University of KwaZulu-Natal College of Health Science (CHS) for PhD running expenses. L.J.L. is funded by a South African National Research Foundation (NRF) Research Career Advancement Fellowship award. L.R.M. and A.D.B are supported by a CIHR New Investigator Awards. The CAPRISA004 tenofovir gel trial was funded principally by the US Agency for International Development, grants through FHI360, and CONRAD for product manufacturing, with support from the South African Department of Science and Technology (DST).
Author information
Authors and Affiliations
Contributions
Designed the study: R.P.M., S.N., A.D.B., J.A.P., and L.R.M. Performed the experiments: R.P.M., L.J.L., L.N.-R., A.M., M.P., K.B., J.H.A., and K.G. Analyzed the data: R.M., L.J.L., L.N.-R., N.M., M.P., K.B., J.H.A., and L.R.M. Wrote the paper: R.M. L.R.M. wrote the first draft and all authors contributed to editing and finalizing. Supervised clinical and/or experimental aspects of the study: A.L., N.J.G., N.S., A.D.B., S.S.A.K., Q.A.K., J.A.P., and L.R.M.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Molatlhegi, R.P., Liebenberg, L.J., Leslie, A. et al. Plasma concentration of injectable contraceptive correlates with reduced cervicovaginal growth factor expression in South African women. Mucosal Immunol 13, 449–459 (2020). https://doi.org/10.1038/s41385-019-0249-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41385-019-0249-y