Abstract
Introduction
Meta-analyses implicate immune dysfunction in depression confirming increased levels of circulating immune proteins (e.g., cytokines) in depression cases compared to controls. White blood cells (WBC) both produce and are influenced by cytokines, and play key roles in orchestrating innate and adaptive immune responses, but their role in depression remains unclear. Therefore, a systematic review of studies of various WBC subsets in depression is required for a greater understanding of the nature of immune dysfunction in this illness.
Methods
We searched PubMed and PsycINFO databases (inception to 5th April 2022) and conducted a systematic review and meta-analysis of identified studies comparing absolute count and/or relative percentage of flow cytometry-derived WBC subsets between depression cases and controls. Selected studies were quality assessed. Random-effect meta-analysis was performed.
Results
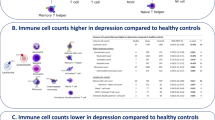
Thirty-three studies were included and 27 studies (n = 2277) were meta-analysed. We report an increase in mean absolute counts of WBC (seven studies; standardised mean difference [SMD] = 1.07; 95% CI, 0.61–1.53; P < 0.01; I2 = 64%), granulocytes (two studies; SMD = 2.07; 95% CI, 1.45–2.68; P < 0.01; I2 = 0%), neutrophils (four studies; SMD = 0.91; 95% CI, 0.23–1.58; P < 0.01; I2 = 82%), monocytes (seven studies; SMD = 0.60; 95% CI, 0.19–1.01; P < 0.01; I2 = 66%), CD4+ helper T cells (11 studies; SMD = 0.30; 95% CI, 0.15–0.45; P < 0.01; I2 = 0%), natural killer cells (11 studies; SMD = 1.23; 95% CI, 0.38–2.08; P < 0.01; I2 = 95%), B cells (10 studies; SMD = 0.30; 95% CI, 0.03–0.57; P = 0.03; I2 = 56%), and activated T cells (eight studies; SMD = 0.45; 95% CI, 0.24–0.66; P < 0.01; I2 = 0%) in depression, compared to controls. Fewer studies reported relative percentage, indicating increased neutrophils and decreased total lymphocytes, Th1, and Th2 cells in depression.
Conclusions
Depression is characterised by widespread alterations in circulating myeloid and lymphoid cells, consistent with dysfunction in both innate and adaptive immunity. Immune cells could be useful biomarkers for illness subtyping and patient stratification in future immunotherapy trials of depression, along with cytokines, other biomarkers, and clinical measures.
Similar content being viewed by others
Introduction
Several lines of evidence implicate immune dysfunction in the pathogenesis of depression. Meta-analyses of case-control studies confirm elevated levels of proinflammatory cytokines, such as interleukin-6 (IL-6), and acute-phase proteins, like C-reactive protein (CRP) in blood and cerebrospinal fluid (CSF) of individuals with depression compared to controls [1,2,3,4,5]. Approximately one quarter of depressed patients show evidence of low-grade inflammation (defined as CRP > 3 mg/L) [6]. Higher IL-6 level in childhood is associated with increased depression risk subsequently in adulthood, in a dose-dependent manner [7]. Mendelian randomization (MR) studies that use genetic variants to address the issues of reverse causation and residual confounding suggest that IL-6 and other immune proteins may play a causal role in depression [8,9,10,11], though null findings have also been reported [12, 13]. Meta-analyses of randomised controlled trials (RCTs) have reported an antidepressant effect of anti-inflammatory drugs [14,15,16], further supporting a role of inflammation in depression.
While the majority of immune biomarker research to date has focused on cytokines and other immune proteins, emerging literature has begun to explore cellular immune markers in the context of depression. These studies are important for a greater understanding of the nature of immune dysfunction in depression, because circulating immune cells: (i) play a critical role in orchestrating immune response; (ii) both produce and are induced by cytokines and other immune proteins; and (iii) are established therapeutic targets in various diseases. Depression has been reported to be associated with leukocytosis, monocytosis, increased neutrophil-to-lymphocyte ratio, and increased CD4+/CD8+ T cell ratio [17,18,19]. An inflammation-related subgroup of depression, defined using peripheral immune cell counts, was reported to be characterised by increased neutrophil, CD4+ helper T cell, and intermediate monocyte counts, higher IL-6 and CRP levels, and increased illness severity [20].
While existing studies indicate alterations in circulating immune cells in depression and potential usefulness of cellular immune markers for dissecting illness heterogeneity, to our knowledge there are currently no systematic reviews and meta-analyses of peripheral blood cellular immunophenotype in depression. A comprehensive summary of this literature is required for a greater understanding of the role immune dysfunction plays in depression. Such work may help clarify the nature and extent of immune dysfunction, identify potential cellular source of cytokine alterations, provide potential immunological treatment targets, and inform the identification of inflammation-related depression subgroups for patient stratification in future immunotherapy trials.
We report a systematic review and meta-analysis of the peripheral blood cellular immunophenotype in depression. Our aim is to provide a comprehensive summary and assessment of the existing literature regarding alterations in various circulating white blood cell (WBC) subsets in depression, compared to controls, derived from flow cytometry, a state-of-the-art immunophenotyping technology.
Methods
Search strategy and study selection
This study was conducted in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [21]. The PRISMA checklist is presented in Supplementary Table 1. Systematic search of the PubMed and PsycINFO databases was carried out to identify all published studies of peripheral blood cellular immunophenotype in depression from database inception to 5th April 2022. Search terms incorporated key indexing terms and wildcards to maximise return and included: (depression OR depressive disorder OR major depressive disorder) AND (leukocyte count OR flow cytometry OR mass cytometry OR immunophenotype OR immunophenotyping OR peripheral blood mononuclear cell). The full search strategy is presented (Supplementary Materials). Our search was restricted to English language articles and human participants. The electronic search was complemented by hand-searching meta-analyses and review articles. All titles and abstracts were examined and relevant studies were retrieved. EMF and JTP applied the inclusion and exclusion criteria independently (detailed below) and selected the final studies for this review. Any differences were resolved by further discussion and consensus involving GMK.
Included studies were: (i) original articles; (ii) written in English; (iii) based on human subjects; (iv) cohort or case-control in design; (v) compared immune phenotype between current depression cases and controls; (vi) defined depression using clinical diagnosis, diagnostic interview using the International Classification of Diseases or the Diagnostic and Statistical Manual of Mental Disorders criteria, or using a validated depression scale score cut-off; (vii) defined controls as individuals with no lifetime history of psychiatric illness; (viii) used flow cytometry, mass cytometry, or related techniques to assess detailed peripheral white blood cell phenotype. Studies that did not primarily examine or report cellular phenotype; focused on specific groups alone (e.g., specific disease group [such as individuals with human immunodeficiency virus infection], elderly, adolescents); or other studies comprised of participants with comorbid medical illness likely to compromise interpretation of immunological data were excluded. As a result, only studies reporting the cellular phenotype of non-immunocompromised adult individuals were included.
Data extraction and quality assessment
Data extraction was performed by EMF and JTP. The main outcome measure was absolute cell count and/or relative percentage in depressed cases and controls. The following data were also extracted for each included study: (i) authors; (ii) year of publication; (iii) country of origin; (iv) study design and setting; (v) sampling method and sample size; (vi) participant age and sex; (vii) case definition; (viii) control definition; (ix) immunophenotyping method; (x) cell types; (xi) covariates. In the case of missing data or uncertainty, authors of respective studies were contacted to provide further information.
The methodological quality of each study was assessed using an adapted version of the Newcastle-Ottawa Scale (NOS) for case-control studies [22]. One NOS scoring item (non-response rate) was deemed irrelevant for the current investigation and so, the maximum possible NOS score here was eight. EMF and JTP performed quality assessment independently. Any differences were resolved by further discussion and consensus involving GMK.
Data synthesis and meta-analysis
Separate meta-analyses were conducted for studies reporting absolute counts and relative percentage of immune cells in depressed cases, compared to controls. However, relative percentages are considered to be a more holistic representation of the immune landscape at the time of sampling, given that relative counts are affected by changes in the parent cell type. Therefore, we focused on results for total cell counts as primary, in line with standard practice in immunology. Studies were grouped according to flow cytometry markers assessed (Supplementary Table 2). Units were harmonised across studies (Supplementary Table 3). When units were not reported, authors were contacted for this information. If no response was obtained, units were deduced based on available information and following expert opinion (REM, LT, GMK). Study results were pooled using the inverse variance method, meaning that studies with larger sample sizes were given greater weight. The standard mean difference (SMD), 95% confidence intervals (CI), and pooled prevalence of each cell type were calculated using quantitative random-effect meta-analysis and visualised using forest plots. Random-effect meta-analysis was chosen, as opposed to fixed effect, due to the evident heterogeneity between studies in setting, sampling method, and assessments. The I2 statistic was used to assess heterogeneity between studies, which describes the percentage of variability in effect estimates that is due to heterogeneity [23]. Publication bias was assessed by visual inspection of funnel plots and Egger’s test for funnel plot asymmetry. Sensitivity analyses were conducted excluding any extreme outlier(s) from primary analyses based on the report of extreme effect size (as compared to other studies included in that particular meta-analysis) and impact on heterogeneity in meta-analysis. Meta-analysis was conducted on all cell types with sufficient data (i.e., reported in ≥2 studies) using Review Manager version 5.4 [24] and R version 4.0.3 using the meta-package [25, 26].
Results
The literature search yielded 1153 potentially relevant studies. After removing duplicates, 934 studies remained. Following title and abstract screening, 98 studies were identified, of which 33 met the inclusion criteria and were included in the review [20, 27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58]. Based on data availability, meta-analysis was conducted on 27 studies (see Fig. 1 for PRISMA diagram of study selection). Table 1 presents the characteristics of included studies.
Meta-analysis of total WBC
Meta-analysis of seven studies comprising 163 depression cases and 105 controls showed an increase in mean total WBC count in cases compared to controls (SMD = 1.07; 95% CI, 0.61–1.53; P < 0.01; I2 = 64%; Supplementary Fig. 1).
Meta-analysis of myeloid cells
Mean absolute counts of granulocytes, neutrophils, and monocytes were found to be higher in depression cases compared to controls (detailed below). Relative percentage of neutrophils was also higher in cases compared to controls.
Granulocytes
Meta-analysis of two studies totalling 34 cases and 32 controls showed higher mean total granulocyte count in depression (SMD = 2.07; 95% CI, 1.45–2.68; P < 0.01; I2 = 0%; Supplementary Fig. 2).
Neutrophils
Meta-analysis of four studies with 282 cases and 117 controls showed an increase in mean total neutrophil count in depression (SMD = 0.91; 95% CI, 0.23–1.58; P < 0.01; I2 = 82%; Fig. 2A). Similarly, separate meta-analysis of three studies showed higher relative percentage of neutrophils in depression compared to controls (SMD = 1.90; 95% CI, 0.02–3.78; P = 0.05; I2 = 93%; Supplementary Fig. 3). Results were similar after removing outliers and heterogeneity reduced to 0% (Supplementary Fig. 4).
Monocytes (CD14+)
Meta-analysis of seven studies with 191 cases and 141 controls showed higher mean absolute monocyte counts in depression (SMD = 0.60; 95% CI, 0.19–1.01; P < 0.01; I2 = 66%; Fig. 2B). However, separate meta-analysis of six studies with 250 cases and 300 controls that reported relative percentage of monocytes showed no difference between groups (SMD = 0.26; 95% CI, −0.08–0.60; P = 0.13; I2 = 65%; Supplementary Fig. 5).
Meta-analysis of lymphoid cells
Mean absolute CD4+ helper T cell, natural killer (NK) cell, B cell, and activated T cell counts were found to be higher in depression cases compared to controls (detailed below). Relative percentage of lymphocytes, Th1, and Th2 were shown to be decreased in cases compared to controls.
Total lymphocytes
Meta-analysis of 10 studies comprising 263 cases and 205 controls showed no difference in mean absolute total lymphocyte count between cases and controls (SMD = −0.18; 95% CI, −0.65–0.30; P = 0.47; I2 = 83%; Supplementary Fig. 6). Results were similar after removing outliers and heterogeneity reduced to 58% (Supplementary Fig. 7). However, separate meta-analysis of six studies that reported relative percentage of total lymphocytes showed a decrease in depression cases compared to controls (SMD = −0.41; 95% CI, −0.80–−0.02; P = 0.04; I2 = 67%; Supplementary Fig. 8).
T (CD3+), helper T (CD4+), and cytotoxic T (CD8+) cells
Meta-analysis of 11 studies totalling 465 cases and 307 controls showed higher CD4+ helper T cell count in depression (SMD = 0.30; 95% CI, 0.15–0.45; P < 0.01; I2 = 0%; Fig. 3). However, total CD3+ and CD8+ T cell count did not differ between groups (Fig. 3). Results were similar when outliers for CD3+ and CD8+ T cells were excluded from meta-analysis and heterogeneity in meta-analysis decreased for both cell types (Supplementary Fig. 9).
Separate meta-analyses of relative percentages of CD3+ T cells, CD4+ helper T cells, and CD8+ cytotoxic T cells, including outliers, showed no differences between depressed cases and controls (Supplementary Fig. 10). Results were similar when the single extreme CD8+ T cell outlier was excluded from meta-analysis and heterogeneity in meta-analysis decreased (Supplementary Fig. 11).
Helper T cell subsets: Th1, Th2, and Th17 cells
No studies reported absolute cells counts for Th1, Th2, or Th17 cells, but relative percentage data for Th1 (four studies), Th2 (three studies), and Th17 (four studies) cells was available. Relative percentage of Th1 (SMD = −0.31; 95% CI, −0.49–−0.14; P < 0.01; I2 = 0%) and Th2 (SMD = −0.36; 95% CI, −0.55–−0.17; P < 0.01; I2 = 0%) cells were found to be lower in depression compared to controls (Supplementary Fig. 12). There was no difference in Th17 cells (Supplementary Fig. 12).
T Regulatory cells
Meta-analysis of four studies with 233 cases and 316 controls showed no difference in relative percentage of T regulatory cells between groups (SMD = −0.13; 95% CI, −0.30–0.04; P = 0.14; I2 = 3%; Supplementary Fig. 13).
NK cells (CD16+/CD56+)
Meta-analysis of 11 studies comprising 291 cases and 277 controls showed higher mean absolute NK cell count (SMD = 1.23; 95% CI, 0.38–2.08; P < 0.01; I2 = 95%; Fig. 4A) in cases compared to controls. Results were similar when the single extreme outlier was excluded from meta-analysis and heterogeneity reduced to 95% (Supplementary Fig. 14). However, meta-analysis of eight studies of relative percentage of NK cells showed no difference between groups (SMD = 0.50; 95% CI, −0.23–1.24; P = 0.18; I2 = 95%; Supplementary Fig. 15). Results were similar when the single extreme outlier was excluded from meta-analysis and heterogeneity in meta-analysis decreased (Supplementary Fig. 16).
B cells (CD19+)
Meta-analysis of 11 studies of mean absolute B cell count with 468 cases and 305 controls showed no difference between groups (SMD = −0.24; 95% CI, −0.88–0.41; P = 0.48; I2 = 93%; Supplementary Fig. 17). However, after excluding the single extreme outlier, meta-analysis of 10 studies with 435 cases and 272 controls showed higher mean absolute B cell count in depression, and heterogeneity in meta-analysis decreased (SMD = 0.30; 95% CI, 0.03–0.57; P = 0.03; I2 = 56%; Fig. 4B).
Meta-analysis of seven studies reporting relative percentage of B cells found no difference between groups (SMD = −0.22; 95% CI, −0.74–0.30; P = 0.420 I2 = 91%; Supplementary Fig. 18). Results were similar when the single extreme outlier was excluded from meta-analysis and heterogeneity dropped to 35% (Supplementary Fig. 19).
Activated T cells: CD25+ and CD3+HLADR+
Meta-analysis of eight studies totalling 233 cases and 169 controls showed higher mean absolute cell counts of activated T cells (CD25+ and CD3+HLADR+) in depressed cases compared to controls (SMD = 0.45; 95% CI, 0.24–0.66; P < 0.01; I2 = 0%; Fig. 5). In particular, SMD for mean absolute cell counts of CD25+ in depression was 0.41 (95% CI, 0.08–0.74; P = 0.02; I2 = 0%; Fig. 5) and SMD for mean absolute CD3+HLADR+ cells in depression was 0.50 (95% CI, 0.19–0.81; P < 0.01; I2 = 21%; Fig. 5). However, meta-analysis of seven studies with 371 cases and 160 controls found no difference between groups in relative percentage of activated T cells (SMD = 0.30; 95% CI, −0.26–0.85; P = 0.29; I2 = 85%; Supplementary Fig. 20).
CD4+/CD8+ ratio
Meta-analysis of seven studies with 130 cases and 133 controls showed no difference in mean absolute CD4+/CD8+ ratio count between groups (SMD = 0.42; 95% CI, −0.41–1.25; P = 0.32; I2 = 89%; Supplementary Fig. 21). Results were similar when outliers were excluded from meta-analysis and heterogeneity reduced to 21% (Supplementary Fig. 22).
Naïve T cells (CD45RA+)
Meta-analysis of two studies with 50 cases and 57 controls showed no difference in mean absolute naïve T cell counts between groups (SMD = 0.29; 95% CI, −0.10–0.67; P = 0.14; I2 = 0%; Supplementary Fig. 23). Moreover, meta-analysis of three studies with 36 cases and 41 controls found no difference between groups in relative percentage of naïve T cells (SMD = −0.04; 95% CI, −0.86–0.78; P = 0.93; I2 = 68%; Supplementary Fig. 24).
Memory T cells (CD45RO+/CD45RA−)
Meta-analysis of five studies with 242 cases and 159 controls found no difference between groups in relative percentage of memory T cells (SMD = −0.13; 95% CI, −0.80–0.54; P = 0.70; I2 = 87%; Supplementary Fig. 25).
Assessment of bias
All 33 studies included in this systematic review had an NOS score of ≥4 out of a maximum of eight, indicating reasonable study quality and relatively low risk of bias (Table 1; Supplementary Table 4). However, two studies scored four stars indicating possible risk of bias and 24 of the 33 studies included were deemed at risk of bias regarding selection of controls, comparability, and/or method of ascertainment for cases and controls.
Publication bias was assessed using Egger’s test (Supplementary Table 5) for all meta-analyses, except for five WBC subsets due to the small number of studies included. There was evidence of publication bias for two subsets, namely studies of mean absolute counts of total lymphocytes (p = 0.02) and relative percentage of cytotoxic T cells (p = 0.02).
Discussion
Our systematic review and meta-analysis suggests that depression is associated with alterations in several myeloid and lymphoid cells, including increased mean absolute counts of total WBC, granulocytes, neutrophils, monocytes, CD4+ helper T cells, NK cells, CD19+ B cells, and CD25+ and CD3+HLADR+ activated T cells. Individuals with depression also displayed increased relative percentage of neutrophils, but decreased relative percentage of lymphocytes, Th1, and Th2 cells, although relatively fewer studies assessed relative percentage of cells. To the best of our knowledge, this is the first systematic review and meta-analysis to consider the peripheral blood cellular immunophenotype of depression, and our findings highlight the potential role of both innate and adaptive immune dysfunction in the aetiology of the illness.
Our results suggest that peripheral blood immune cell counts could be useful biomarkers for the identification of inflammation-related depression subgroups, and for immunological treatment development by informing patient stratification in future clinical trials. We report evidence of leukocytosis, monocytosis, and neutrophilia in depression, which is consistent with previous research implicating innate immune dysfunction in the pathogenesis of this illness [59,60,61]. In particular, previous studies have reported increased leukocytes and myeloid cells, particularly neutrophils and monocytes, in depression [17, 19, 62]. Furthermore, we provide a novel finding of increased absolute granulocyte counts in depressed cases, further implicating myeloid cells in depression aetiology.
Though myeloid cells are strongly implicated in the data presented, it is clear that lymphoid cells also play an important role. It is known that CD4+ helper T cells facilitate cytokine production [63]. We show results for cells that are consistent with cytokine signature and reveal potential cellular sources of cytokine alterations implicated in depression. In addition, we present evidence of elevated NK cell, B cell, and activated T cell absolute counts in depression. Taken together, our results not only provide further evidence of immune dysregulation in depression, but also implicate both the innate and adaptive immune responses in the pathogenesis of the disease.
These findings could be useful for several reasons. First, while the evidence of cytokine abnormalities is well established in depression, immune cell alterations in this illness are relatively less understood. Identifying cellular immunophenotypes in depression may help elucidate a cellular source(s) of these known cytokine alterations. Moreover, cell phenotyping in addition to protein data may prove useful for illness subtyping. This would be particularly beneficial for patient stratification in future immunotherapy RCTs. Our investigation also highlights the need for future investigations to determine the direction of association between immune cell alterations identified and depression. If deemed causal, immune cells may represent suitable treatment targets for major depressive disorder.
We report that depression is associated with a decrease in relative percentage of total lymphocytes, Th1, and Th2 cells and an increase in relative percentage of neutrophils. However, several cell types displaying a large effect in meta-analyses of mean absolute cell counts showed no effect in meta-analyses of changes in relative cell percentage. One possible explanation could be that relative percentages are a holistic representation of the immune landscape at the time of sampling. Unlike total cell count, change in relative percentage of one cell type can be influenced by changes in another cell type(s). For example, our finding of a decrease in the relative percentage of lymphocytes, Th1, and Th2 cells may indicate an absolute decrease in the number of these cells in depressed cases compared to controls, or an absolute increase in the number of a different cell type(s). Therefore, in line with standard practice in immunology we focus on results for mean absolute cell count as primary.
Although our investigation revealed a number of cellular differences between depressed cases and controls, there are also several null findings of interest. Firstly, CD4+/CD8+ ratio has been reported to be higher in depressed patients [19]. Though our research found a possible trending increase in absolute numbers of this ratio, the confidence intervals overlapped the null. Moreover, no associations were identified for absolute numbers of total lymphocytes, CD3+ cells, CD8+ cells, T regulatory cells, or naïve T cells. Aside from the possibility of there being no actual differences between groups on these cell types, these lack of associations may also be due to the low number of studies that focused on these cell subsets, the immunophenotyping methods used in these studies, and sample characteristics. Basophils and eosinophils were also of interest to the current investigation, however, only one eligible study reported these cell counts. Therefore, future immunophenotyping research should focus on exploring more detailed levels of the cellular hierarchy in patients with depression.
Strengths of this work include the systematic literature search of two databases which identified 1,286 cases and 991 control participants. All studies were assessed using the validated Newcastle-Ottawa Scale (NOS) for case-control studies and publication bias was evaluated by visual inspection of funnel plots and Egger’s test. While the majority of studies originated from Europe and North America, countries outside these regions were also represented in our final selection. Rigorous inclusion criteria was applied to ensure depressed cases were defined using a validated scale, controls had no lifetime history of psychiatric illness, and immunophenotyping was conducted using an established method.
Limitations of this work include the quality of studies included. Case-control studies are prone to selection bias, as reflected by the NOS scores for many of the included studies. While most of these studies recruited controls from the community, psychiatric assessment was often unblinded and not all studies reported method of control recruitment. Second, meta-analyses of certain cell types, namely granulocytes and naïve T cells, were based on data from only two studies. Although meta-analysis can be carried out using data from a minimum of two studies, standard random-effects meta-analysis methods have been reported to perform poorly when applied to few studies [64,65,66]. Therefore, while we report a large effect for mean absolute counts of granulocytes and no effect for mean absolute naïve T cell count, these results should be considered in the context of limited data currently available. Overall, compared with studies of circulating immune proteins [1,2,3,4,5], there are fewer studies of immune cell counts in depression at present. Further studies are required, as our results suggest that such studies can provide valuable insights into the nature of immune dysfunction in depression. Moreover, although we conducted a thorough and up-to-date literature search, publication bias, especially from selective non-reporting of null findings, is always a possibility for meta-analysis. We assessed evidence of publication bias using visual inspection of funnel plots and Egger’s test. All but two studies showed no evidence of publication bias. Egger’s test was found to be significant for mean absolute total lymphocyte counts and relative percentages of cytotoxic T cells, indicating possible publication bias in these subsets. Most included studies controlled for confounding (particularly age and sex), but this was not the case for all studies. Therefore, more robust confounding adjustment, for example ethnicity, socio-economic status, medications, physical illness, and/or body mass index, is required in future studies. Considerable heterogeneity between studies can be observed in select analyses, however, after the removal of outliers, I2 statistic dropped and results remained similar for most analyses. However, it is worth noting that heterogeneity remained high for select cell types (i.e., WBC, neutrophils, monocytes, NK cells). Additionally, this review and respective protocol was not registered prior to analysis. Lastly, by design it is difficult to infer causality from case-control studies, and so future research is needed to examine whether observed associations are likely to be causal. Genetic approaches, such as MR analysis, could be particularly useful for this purpose. Results for many cell types were mixed, possibly due to phenotyping method used and sample characteristics, and so there is a need for the standardisation of immunophenotyping methods in studies of depression.
In summary, depression is associated with altered peripheral blood myeloid and lymphoid cell counts, particularly WBC, granulocytes, neutrophils, monocytes, CD4+ helper T cells, NK cells, and activated T cells, and with altered cell relative percentages of neutrophils, lymphocytes, Th1, and Th2 cells. These findings are consistent with a potential role of both innate and adaptive immune dysfunction in the aetiology of depression. Immune cells could be useful biomarkers for illness sub-typing and the identification of inflammation-related depression subgroups for patient stratification in future immunotherapy trials. Further research is required to establish whether and how altered immune cells may causally influence the risk of depression, in consort with changes in cytokines and other immune protein levels/activity.
References
Chamberlain SR, Cavanagh J, Boer P, de, Mondelli V, Jones DNC, Drevets WC, et al. Treatment-resistant depression and peripheral C-reactive protein. Br J Psychiatry. 2019;214:11–9.
Haapakoski R, Mathieu J, Ebmeier KP, Alenius H, Kivimäki M. Cumulative meta-analysis of interleukins 6 and 1β, tumour necrosis factor α and C-reactive protein in patients with major depressive disorder. Brain Behav Immun. 2015;49:206–15.
Köhler CA, Freitas TH, Maes M, de Andrade NQ, Liu CS, Fernandes BS, et al. Peripheral cytokine and chemokine alterations in depression: a meta-analysis of 82 studies. Acta Psychiatr Scand. 2017;135:373–87.
Wang AK, Miller BJ. Meta-analysis of cerebrospinal fluid cytokine and tryptophan catabolite alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder, and depression. Schizophr Bull. 2018;44:75–83.
Goldsmith DR, Rapaport MH, Miller BJ. A meta-analysis of blood cytokine network alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder and depression. Mol Psychiatry. 2016;21:1696–709.
Osimo EF, Baxter LJ, Lewis G, Jones PB, Khandaker GM. Prevalence of low-grade inflammation in depression: a systematic review and meta-analysis of CRP levels. Psychol Med. 2019;49:1958–70.
Khandaker GM, Pearson RM, Zammit S, Lewis G, Jones PB. Association of serum interleukin 6 and C-reactive protein in childhood with depression and psychosis in young adult life: a population-based longitudinal study. JAMA Psychiatry. 2014;71:1121–8.
Khandaker GM, Zammit S, Burgess S, Lewis G, Jones PB. Association between a functional interleukin 6 receptor genetic variant and risk of depression and psychosis in a population-based birth cohort. Brain Behav Immun. 2018;69:264–72.
Ye Z, Kappelmann N, Moser S, Davey Smith G, Burgess S, Jones PB, et al. Role of inflammation in depression and anxiety: tests for disorder specificity, linearity and potential causality of association in the UK Biobank. EClinicalMedicine. 2021;38:100992.
Lamers F, Milaneschi Y, Smit JH, Schoevers RA, Wittenberg G, Penninx BWJH. Longitudinal association between depression and inflammatory markers: results from the Netherlands Study of Depression and Anxiety. Biol Psychiatry. 2019;85:829–37.
Khandaker GM, Zuber V, Rees JMB, Carvalho L, Mason AM, Foley CN, et al. Shared mechanisms between coronary heart disease and depression: findings from a large UK general population-based cohort. Mol Psychiatry. 2020;25:1477–86.
Wium-Andersen MK, Orsted DD, Nordestgaard BG. Elevated C-reactive protein, depression, somatic diseases, and all-cause mortality: a mendelian randomization study. Biol Psychiatry. 2014;76:249–57.
Kappelmann N, Arloth J, Georgakis MK, Czamara D, Rost N, Ligthart S, et al. Dissecting the association between inflammation, metabolic dysregulation, and specific depressive symptoms: a genetic correlation and 2-sample mendelian randomization study. JAMA Psychiatry. 2021;78:161–70.
Kappelmann N, Lewis G, Dantzer R, Jones PB, Khandaker GM. Antidepressant activity of anti-cytokine treatment: a systematic review and meta-analysis of clinical trials of chronic inflammatory conditions. Mol Psychiatry. 2018;23:335–43.
Wittenberg GM, Stylianou A, Zhang Y, Sun Y, Gupta A, Jagannatha PS, et al. Effects of immunomodulatory drugs on depressive symptoms: A mega-analysis of randomized, placebo-controlled clinical trials in inflammatory disorders [no. 6]. Mol Psychiatry. 2020;25:1275–85.
Köhler O, Benros ME, Nordentoft M, Farkouh ME, Iyengar RL, Mors O, et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2014;71:1381–91.
Maes M, Van der Planken M, Stevens WJ, Peeters D, DeClerck LS, Bridts CH, et al. Leukocytosis, monocytosis and neutrophilia: hallmarks of severe depression. J Psychiatr Res. 1992;26:125–34.
Mazza MG, Lucchi S, Tringali AGM, Rossetti A, Botti ER, Clerici M. Neutrophil/lymphocyte ratio and platelet/lymphocyte ratio in mood disorders: A meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2018;84:229–36.
Zorrilla EP, Luborsky L, McKay JR, Rosenthal R, Houldin A, Tax A, et al. The relationship of depression and stressors to immunological assays: a meta-analytic review. Brain Behav Immun. 2001;15:199–226.
Lynall M-E, Turner L, Bhatti J, Cavanagh J, de Boer P, Mondelli V, et al. Peripheral blood cell–stratified subgroups of inflamed depression. Biol Psychiatry. 2020;88:185–96.
Moher D, Liberati A, Tetzlaff J, Altman D, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009;6:e1000097.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
The Cochrane Collaboration. Review Manager (RevMan) Version 5.4. 2020.
R Core Team. R: A Language Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2022. https://www.r-project.org/.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22:153–60.
Atanackovic D, Kröger H, Serke S, Deter H-C. Immune parameters in patients with anxiety or depression during psychotherapy. J Affect Disord. 2004;81:201–9.
Başterzi AD, Yazici K, Buturak V, Çimen B, Yazici A, Eskandari G, et al. Effects of venlafaxine and fluoxetine on lymphocyte subsets in patients with major depressive disorder: a flow cytometric analysis. Prog Neuro-Psychopharmacol Biol Psychiatry. 2010;34:70–5.
Becking K, Haarman BCM, Grosse L, Nolen WA, Claes S, Arolt V, et al. The circulating levels of CD4+ t helper cells are higher in bipolar disorder as compared to major depressive disorder. J Neuroimmunol. 2018;319:28–36.
Euteneuer F, Schwarz MJ, Schmidmaier R, Hennings A, Riemer S, Stapf TM, et al. Blunted exercise-induced mobilization of monocytes in somatization syndromes and major depression. J Affect Disord. 2014;166:156–64.
Ghosh R, Kumar PK, Mitra P, Purohit P, Nebhinani N, Sharma P. Circulating T helper 17 and IFN-γ positive Th17 cells in Major Depressive Disorder. Behavioural Brain Res. 2020;394:112811.
Grosse L, Carvalho LA, Birkenhager TK, Hoogendijk WJ, Kushner SA, Drexhage HA, et al. Circulating cytotoxic T cells and natural killer cells as potential predictors for antidepressant response in melancholic depression. Restoration of T regulatory cell populations after antidepressant therapy. Psychopharmacology. 2016a;233:1679–88.
Grosse L, Hoogenboezem T, Ambrée O, Bellingrath S, Jörgens S, de Wit HJ, et al. Deficiencies of the T and natural killer cell system in major depressive disorder. Brain, Behav, Immun. 2016b;54:38–44.
Hasselmann H, Gamradt S, Taenzer A, Nowacki J, Zain R, Patas K, et al. Pro-inflammatory monocyte phenotype and cell-specific steroid signaling alterations in unmedicated patients with major depressive disorder. Front Immunol. 2018;9:2693.
Hernandez ME, Martinez-Fong D, Perez-Tapia M, Estrada-Garcia I, Estrada-Parra S, Pavón L. Evaluation of the effect of selective serotonin-reuptake inhibitors on lymphocyte subsets in patients with a major depressive disorder. Eur Neuropsychopharmacol. 2010;20:88–95.
Hosseini RF, Azad FJ, Talaee A, Miri S, Hosseini FF, Esmaeili H, et al. Assessment of the immune system activity in Iranian patients with major depression disorder (MDD). Iran J Immunol. 2007;4:38–43.
Kanba S, Manki H, Shintani F, Ohno Y, Yagi G, Asai M. Aberrant interleukin-2 receptor-mediated blastoformation of peripheral blood lymphocytes in a severe major depressive episode. Psychol Med. 1998;28:481–4.
Landmann R, Schaub B, Link S, Wacker HR. Unaltered monocyte function in patients with major depression before and after three months of antidepressive therapy. Biol Psychiatry. 1997;41:675–81.
Maes M, Stevens WJ, DeClerck LS, Bridts CH, Peeters D, Schotte C, et al. A significantly increased number and percentage of B cells in depressed subjects: results of flow cytometric measurements. J Affect Disord. 1992;24:127–34.
Maes M, Stevens W, Declerck L, Bridts C, Peeters D, Schotte C, et al. Significantly increased expression of T-cell activation markers (interleukin-2 and HLA-DR) in depression: further evidence for an inflammatory process during that illnessING THAT ILLNESS. Prog Neuropsychopharmacol Biol Psychiatry. 1993b;17:241–55.
Maes M, Lambrechts J, Bosmans E, Jacobs J, Suy E, Vandervorst C, et al. Evidence for a systemic immune activation during depression: results of leukocyte enumeration by flow cytometry in conjunction with monoclonal antibody staining. Psychol Med. 1992b;22:45–53.
Maes M, Stevens W, DeClerck L, Bridts C, Peeters D, Schotte C, et al. Immune disorders in depression: higher T helper/T suppressor-cytotoxic cell ratio. Acta Psychiatr Scand. 1992c;86:423–31.
Maes M, Lambrechts J, Suy E, Vandervorst C, Bosnians E. Absolute number and percentage of circulating natural killer, non-MHC-restricted T cytotoxic, and phagocytic cells in unipolar depression. Neuropsychobiology. 1994a;29:157–63.
Maes M, Meltzer HY, Stevens W, Calabrese J, Cosyns P. Natural killer cell activity in major depression: relation to circulating natural killer cells, cellular indices of the immune response, and depressive phenomenology. Prog Neuro-Psychopharmacol Biol Psychiatry. 1994b;18:717–30.
Maes M, Scharpé S, Meltzer HY, Cosyns P. Relationships between increased haptoglobin plasma levels and activation of cell-mediated immunity in depression. Biol Psychiatry. 1993a;34:690–701.
Nowak W, Grendas LN, Sanmarco LM, Estecho IG, Arena ÁR, Eberhardt N, et al. Pro-inflammatory monocyte profile in patients with major depressive disorder and suicide behaviour and how ketamine induces anti-inflammatory M2 macrophages by NMDAR and mTOR. EBioMedicine. 2019;50:290–305.
Patas K, Willing A, Demiralay C, Engler JB, Lupu A, Ramien C, et al. T cell phenotype and T cell receptor repertoire in patients with major depressive disorder. Front Immunol. 2018;9:291.
Pavón L, Sandoval-López G, Eugenia Hernández M, Loría F, Estrada I, Pérez M, et al. Th2 cytokine response in Major Depressive Disorder patients before treatment. J Neuroimmunol. 2006;172:156–65.
Ravindran AV, Griffiths J, Merali Z, Anisman H. Circulating lymphocyte subsets in obsessive compulsive disorder, major depression and normal controls. J Affect Disord. 1999;52:1–10.
Ravindran AV, Griffiths J, Merali Z, Anisman H. Variations of lymphocyte subsets associated with stress in depressive populations. Psychoneuroendocrinology. 1996;21:659–71.
Ravindran AV, Griffiths J, Merali Z, Anisman H. Circulating lymphocyte subsets in major depression and dysthymia with typical or atypical features. Psychosom Med. 1998;60:283–9.
Robertson MJ, Schacterle RS, Mackin GA, Wilson SN, Bloomingdale KL, Ritz J, et al. Lymphocyte subset differences in patients with chronic fatigue syndrome, multiple sclerosis and major depression. Clin Exp Immunol. 2005;141:326–32.
Rothermundt M, Arolt V, Fenker J, Gutbrodt H, Peters M, Kirchner H. Different immune patterns in melancholic and non-melancholic major depression. Eur Arch Psychiatry Clin Neurosci. 2001;251:90–7.
Schiweck C, Valles-Colomer M, Arolt V, Müller N, Raes J, Wijkhuijs A, et al. Depression and suicidality: a link to premature T helper cell aging and increased Th17 cells. Brain, Behav, Immun. 2020;87:603–9.
Schlatter J, Ortuño F, Cervera-Enguix S. Lymphocyte subsets and lymphokine production in patients with melancholic versus nonmelancholic depression. Psychiatry Res. 2004;128:259–65.
Seidel A, Arolt V, Hunstiger M, Rink L, Behnisch A, Kirchner H. Major depressive disorder is associated with elevated monocyte counts. Acta Psychiatr Scand. 1996;94:198–204.
Suzuki H, Savitz J, Kent Teague T, Gandhapudi SK, Tan C, Misaki M, et al. Altered populations of natural killer cells, cytotoxic T lymphocytes, and regulatory T cells in major depressive disorder: association with sleep disturbance. Brain Behav Immun. 2017;66:193–200.
Syed SA, Beurel E, Loewenstein DA, Lowell JA, Craighead WE, Dunlop BW, et al. Defective inflammatory pathways in never-treated depressed patients are associated with poor treatment response. Neuron. 2018;99:914–92.e3.
Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9:46–56.
Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65:732–41.
Leday GGR, Vértes PE, Richardson S, Greene JR, Regan T, Khan S, et al. Replicable and coupled changes in innate and adaptive immune gene expression in two case-control studies of blood microarrays in major depressive disorder. Biol Psychiatry. 2018;83:70–80.
Surtees P, Wainwright N, Day N, Luben R, Brayne C, Khaw K-T. Association of depression with peripheral leukocyte counts in EPIC-Norfolk-role of sex and cigarette smoking. J Psychosom Res. 2003;54:303–6.
Cohen SB, Maurer KJ, Egan CE, Oghumu S, Satoskar AR, Denkers EY. CXCR3-dependent CD4+ T cells are required to activate inflammatory monocytes for defense against intestinal infection. PLOS Pathog. 2013;9:e1003706.
Seide SE, Röver C, Friede T. Likelihood-based random-effects meta-analysis with few studies: empirical and simulation studies. BMC Med Res Methodol. 2019;19:16.
Röver C, Knapp G, Friede T. Hartung-Knapp-Sidik-Jonkman approach and its modification for random-effects meta-analysis with few studies. BMC Med Res Methodol. 2015;15:99.
Friede T, Röver C, Wandel S, Neuenschwander B. Meta-analysis of few small studies in orphan diseases. Res Synth Methods. 2017;8:79–91.
Acknowledgements
We would like to thank Dr Mary-Ellen Lynall (University of Cambridge) for providing additional information regarding their study for our systematic review and meta-analysis.
Funding
This research was funded in whole, or in part, by the Wellcome Trust (Grant number 201486/B/16/Z). For the purpose of open access, the authors have applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission. EMF is supported by a Medical Research Council Integrative Epidemiology Unit PhD Studentship (MC_UU_00011/1). JTP acknowledges funding from the Versus Arthritis Award (Grant No. 22453). REM is supported by the Medical Research Council Integrative Epidemiology Unit (MC_UU_00011/1). LT acknowledges funding support from NIHR Cambridge BioResource. GMK is supported by the Wellcome Trust (Grant No. 201486/Z/16/Z), the Medical Research Council (Grant No. MC_PC_17213, Grant No. MR/S037675/1, and Grant No. MR/W014416/1), The MQ: Transforming Mental Health (Grant No. MQDS17/40), and the BMA Foundation (J. Moulton Grant 2019). The funders had no role in the design or conduct of this study.
Author information
Authors and Affiliations
Contributions
GMK conceived the study and provided overall supervision for the project, which was led by EMF. EMF and JTP performed the literature search, study selection, data extraction, and quality assessment. EMF was responsible for all statistical analyses and wrote the first draft of the manuscript. REM and LT were responsible for providing and sharing expertise on all immunological aspects of the study. All authors critically reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
EMF, JTP, REM, and GMK have no conflicts of interest to report. LT is an employee of bit.bio. LT declares no other affiliations with or involvement in any organisation or entity with any financial or non-financial interest in the subject matter or materials disclosed in this manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Foley, É.M., Parkinson, J.T., Mitchell, R.E. et al. Peripheral blood cellular immunophenotype in depression: a systematic review and meta-analysis. Mol Psychiatry 28, 1004–1019 (2023). https://doi.org/10.1038/s41380-022-01919-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-022-01919-7