Abstract
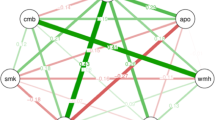
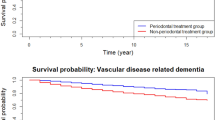
Co-infection between Helicobacter pylori (Hp) and groups of periodontal pathogens may alter the onset of Alzheimer’s disease (AD) and all-cause dementia. We examined the interactive associations among Hp sero-positivity, periodontal disease (Pd), and infections with incident AD and all-cause dementia, among older adults (≥65 years at baseline). Up to 1431 participants from phase 1 of the National Health and Nutrition Survey III (1988–1991) had complete data till January 1st, 2014 on Hp sero-positivity with a mean follow-up of 10–11 years for AD and all-cause dementia incidence. Exposures consisted of 19 periodontal pathogens, constructed factors and clusters, and two Pd markers- probing depth and clinical attachment loss (CAL). Cox proportional hazards models were performed. Around 55% of the selected sample was Hp+. We found that Prevotella intermedia, Campylobacter Rectus, Factor 2 (Pi/Prevotella nigrescens/Prevotella melaninogenica), and the Orange-Red cluster interacted synergistically with Hp sero-positivity, particularly with respect to AD incidence. The presence of higher levels of Actinomyces Naeslundii (An) enhanced the effect of being Hp+ on both AD and all-cause dementia incidence. In contrast, Fusobacterim nucleatum (Fn), and Factor 1 (which included Fn), exhibited an antagonistic interaction with Hp in relation to all-cause dementia. Both probing depth and CAL had direct associations with all-cause dementia among Hp+ individuals, despite nonsignificant interaction. Selected periodontal pathogen titers, factors, and clusters interacted mostly synergistically, with Hp sero-positivity, to alter the risk of AD and all-cause dementia. Ultimately, a randomized controlled trial is needed, examining effects of co-eradication of Hp and select periodontal pathogens on neurodegenerative disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Alzheimer’s Association. 2019 Alzheimer’s disease facts and figures. Alzheimer's Dement. 2019;15:321–87.
Lindeboom J, Weinstein H. Neuropsychology of cognitive ageing, minimal cognitive impairment, Alzheimer’s disease, and vascular cognitive impairment. Eur J Pharm. 2004;490:83–86.
Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011;10:819–28.
Kamer AR, Dasanayake AP, Craig RG, Glodzik-Sobanska L, Bry M, de Leon MJ. Alzheimer’s disease and peripheral infections: the possible contribution from periodontal infections, model and hypothesis. J Alzheimer's Dis. 2008;13:437–49.
Noble JM, Borrell LN, Papapanou PN, Elkind MS, Scarmeas N, Wright CB. Periodontitis is associated with cognitive impairment among older adults: analysis of NHANES-III. J Neurol Neurosurg Psychiatry. 2009;80:1206–11.
Noble JM, Scarmeas N, Celenti RS, Elkind MS, Wright CB, Schupf N, et al. Serum IgG antibody levels to periodontal microbiota are associated with incident Alzheimer disease. PLoS One. 2014;9:e114959.
Sparks Stein P, Steffen MJ, Smith C, Jicha G, Ebersole JL, Abner E, et al. Serum antibodies to periodontal pathogens are a risk factor for Alzheimer’s disease. Alzheimer's Dement. 2012;8:196–203.
Beydoun MA, Beydoun HA, Elbejjani M, Dore GA, Zonderman AB. Helicobacter pylori seropositivity and its association with incident all-cause and Alzheimer’s disease dementia in large national surveys. Alzheimer's Dement. 2018;14:1148–58.
Beydoun MA, Beydoun HA, Shroff MR, Kitner-Triolo MH, Zonderman AB. Helicobacter pylori seropositivity and cognitive performance among US adults: evidence from a large national survey. Psychosom Med. 2013;75:486–96.
Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366:1809–20.
Bielanski W. Epidemiological study on Helicobacter pylori infection and extragastroduodenal disorders in Polish population. J Physiol Pharm. 1999;50:723–33.
Rezvani F, Sayadnasiri M, Rezaei O. The study of memory and executive dysfunction in patients infected with Helicobacter pylori. Neurol Res. 2017;39:953–8.
Doulberis M, Kotronis G, Thomann R, Polyzos SA, Boziki M, Gialamprinou D, et al. Review: impact of Helicobacter pylori on Alzheimer’s disease: what do we know so far? Helicobacter 2018;23. https://doi.org/10.1111/hel.12454.
Kountouras J, Boziki M, Zavos C, Gavalas E, Giartza-Taxidou E, Venizelos I, et al. A potential impact of chronic Helicobacter pylori infection on Alzheimer’s disease pathobiology and course. Neurobiol Aging. 2012;33:e3–4.
Roubaud-Baudron C, Krolak-Salmon P, Quadrio I, Megraud F, Salles N. Impact of chronic Helicobacter pylori infection on Alzheimer’s disease: preliminary results. Neurobiol Aging. 2012;33:1009 e1011–1009.
Al Asqah M, Al Hamoudi N, Anil S, Al Jebreen A, Al-Hamoudi WK. Is the presence of Helicobacter pylori in dental plaque of patients with chronic periodontitis a risk factor for gastric infection? Can J Gastroenterol. 2009;23:177–9.
Nalliah RP, Virun V, Dhaliwal G, Kaur H, Kote A. Fifteen-year gap between oral health of blacks and whites in the USA. J Investig Clin Dent. 2019;10:e12415.
Zajacova A, Dowd JB, Aiello AE. Socioeconomic and race/ethnic patterns in persistent infection burden among U.S. adults. J Gerontol A Biol Sci Med Sci. 2009;64:272–9.
Chen Z, Cai J, Chen YM, Wei J, Li HB, Lu Y, et al. A meta-analysis of the association between the presence of Helicobacter pylori and periodontal diseases. Medicine. 2019;98:e15922.
Demmer RT, Papapanou PN. Epidemiologic patterns of chronic and aggressive periodontitis. Periodontology 2000. 2010;53:28–44.
Beydoun MA, Beydoun HA, Hossain S, El-Hajj, ZW, Weiss J, Zonderman AB. Clinical and Bacterial Markers of Periodontitis and Their Association with Incident All-Cause and Alzheimer's Disease Dementia in a Large National Survey. J Alzheimers Dis. 2020. https://doi.org/10.3233/JAD-200064. [Epub ahead of print].
Center for Disease Control and Prevention (CDC). The Third National Health and Nutrition Examination Survey (NHANES III 1988–94) Reference Manuals and Reports (CD-ROM). Bethesda, MD: Centers for Disease Control and Prevention; 1996.
NHANES and CMS linked data overview. 2012. https://www.cdc.gov/nchs/tutorials/NHANES-CMS/Orientation/Overview/index.htm. Accessed 2012.
Choi YH, McKeown RE, Mayer-Davis EJ, Liese AD, Song KB, Merchant AT. Association between periodontitis and impaired fasting glucose and diabetes. Diabetes Care. 2011;34:381–6.
Plan and operation of the third National Health and Nutrition Examination Survey,1988–1994. Series 1: Programs and No. 32 Collection Procedures. 2009. http://www.cdc.gov/nchs/data/series/sr_01/sr01_032.pdf. Accessed 2009.
Choi YH, McKeown RE, Mayer-Davis EJ, Liese AD, Song KB, Merchant AT. Serum C-reactive protein and immunoglobulin G antibodies to periodontal pathogens may be effect modifiers of periodontitis and hyperglycemia. J Periodontol. 2014;85:1172–81.
Papapanou PN, Neiderud AM, Sandros J, Dahlen G. Checkerboard assessments of serum antibodies to oral microbiota as surrogate markers of clinical periodontal status. J Clin Periodontol. 2001;28:103–6.
Shrestha D, Choi YH, Zhang J, Hazlett LJ, Merchant AT. Relationship between serologic markers of periodontal bacteria and metabolic syndrome and its components. J Periodontol. 2015;86:418–30.
Helicobacter pylori IgG antibodies in serum by enzyme immunoassay. National Health and Nutrition Examination laboratory protocol. 2008. http://www.cdc.gov/nchs/data/nhanes/nhanes_99_00/lab11_met_helicobacter_pylori.pdf. Accessed 2008.
STATA. Statistics/data analysis: Release 16.0. College Station, Texas: Stata Corporation; 2019.
Lee KJ, Carlin JB. Multiple imputation for missing data: fully conditional specification versus multivariate normal imputation. Am J Epidemiol. 2010;171:624–32.
Hochberg Y, Tamhane AC. Multiple comparison procedures. New York: Wiley; 1987.
Selvin S. Statistical analysis of epidemiologic data. 3rd ed. New York: Oxford University Press; 2004.
Lee YT, Lee HC, Hu CJ, Huang LK, Chao SP, Lin CP, et al. Periodontitis as a modifiable risk factor for dementia: a nationwide population-based cohort study. J Am Geriatr Soc. 2017;65:301–5.
Maldonado A, Laugisch O, Burgin W, Sculean A, Eick S. Clinical periodontal variables in patients with and without dementia-a systematic review and meta-analysis. Clin Oral Investig. 2018;22:2463–74. https://doi.org/10.1007/s00784-018-2523-x.
Kamer AR, Craig RG, Dasanayake AP, Brys M, Glodzik-Sobanska L, de Leon MJ. Inflammation and Alzheimer’s disease: possible role of periodontal diseases. Alzheimer’s Dement: J Alzheimer’s Assoc. 2008;4:242–50.
Burucoa C, Axon A. Epidemiology of Helicobacter pylori infection. Helicobacter. 2017;22 Suppl 1. https://doi.org/10.1111/hel.12454.
Grad YH, Lipsitch M, Aiello AE. Secular trends in Helicobacter pylori seroprevalence in adults in the United States: evidence for sustained race/ethnic disparities. Am J Epidemiol. 2012;175:54–9.
Dye BA, Kruszon-Moran D, McQuillan G. The relationship between periodontal disease attributes and Helicobacter pylori infection among adults in the United States. Am J Public Health. 2002;92:1809–15.
Ishihara K, Miura T, Ebihara Y, Hirayama T, Kamiya S, Okuda K. Shared antigenicity between Helicobacter pylori and periodontopathic Campylobacter rectus strains. FEMS Microbiol Lett. 2001;197:23–27.
Tanabe S, Hinode D, Yokoyama M, Fukui M, Nakamura R, Yoshioka M, et al. Helicobacter pylori and Campylobacter rectus share a common antigen. Oral Microbiol Immunol. 2003;18:79–87.
Yamanaka T, Furukawa T, Matsumoto-Mashimo C, Yamane K, Sugimori C, Nambu T, et al. Gene expression profile and pathogenicity of biofilm-forming Prevotella intermedia strain 17. BMC Microbiol. 2009;9:11.
Doke M, Fukamachi H, Morisaki H, Arimoto T, Kataoka H, Kuwata H. Nucleases from Prevotella intermedia can degrade neutrophil extracellular traps. Mol Oral Microbiol. 2017;32:288–300.
Matsui A, Jin J-O, Johnston CD, Yamazaki H, Houri-Haddad Y, Rittling SR. Pathogenic bacterial species associated with endodontic infection evade innate immune control by disabling neutrophils. Infect Immun. 2014;82:4068–79.
Hu Z, Zhang Y, Li Z, Yu Y, Kang W, Han Y, et al. Effect of Helicobacter pylori infection on chronic periodontitis by the change of microecology and inflammation. Oncotarget. 2016;7:66700–12.
Sarkonen N, Könönen E, Summanen P, Kanervo A, Takala A, Jousimies-Somer H. Oral colonization with Actinomyces species in infants by two years of age. J Dent Res. 2000;79:864–7.
Kim SR, Jung LY, Oh I-J, Kim Y-C, Shin K-C, Lee MK, et al. Pulmonary actinomycosis during the first decade of 21st century: cases of 94 patients. BMC Infect Dis. 2013;13:216–216.
Shen S, Samaranayake L, Yip H-K. Coaggregation profiles of the microflora from root surface caries lesions. Arch Oral Biol. 2005;50:23–32.
Tang G, Yip H-K, Samaranayake LP, Chan K-Y, Luo G, Fang HH. Direct detection of cell surface interactive forces of sessile, fimbriated and non-fimbriated Actinomyces spp. using atomic force microscopy. Arch Oral Biol. 2004;49:727–38.
Andersen RN, Ganeshkumar N, Kolenbrander PE. Helicobacter pylori adheres selectively to Fusobacterium spp. Oral Microbiol Immunol. 1998;13:51–4.
Gharbia S, Shah H, Lawson P, Haapasalo M. The distribution and frequency of Fusobacterium nucleatum subspecies in the human oral cavity. Oral Microbiol Immunol. 1990;5:324–7.
Casarin R, Barbagallo A, Meulman T, Santos V, Sallum E, Nociti F, et al. Subgingival biodiversity in subjects with uncontrolled type‐2 diabetes and chronic periodontitis. J Periodontal Res. 2013;48:30–6.
Wang X, Buhimschi CS, Temoin S, Bhandari V, Han YW, Buhimschi IA. Comparative microbial analysis of paired amniotic fluid and cord blood from pregnancies complicated by preterm birth and early-onset neonatal sepsis. PloS One. 2013;8:e56131–e56131.
Rubinstein MR, Wang X, Liu W, Hao Y, Cai G, Han YW. Fusobacterium nucleatum promotes colorectal carcinogenesis by modulating E-cadherin/β-catenin signaling via its FadA adhesin. Cell Host Microbe. 2013;14:195–206.
Xu M, Yamada M, Li M, Liu H, Chen SG, Han YW. FadA from Fusobacterium nucleatum utilizes both secreted and nonsecreted forms for functional oligomerization for attachment and invasion of host cells. J Biol Chem. 2007;282:25000–9.
Manson McGuire A, Cochrane K, Griggs AD, Haas BJ, Abeel T, Zeng Q, et al. Evolution of invasion in a diverse set of Fusobacterium species. mBio. 2014;5:e01864.
Ishida N, Ishihara Y, Ishida K, Tada H, Funaki-Kato Y, Hagiwara M, et al. Periodontitis induced by bacterial infection exacerbates features of Alzheimer’s disease in transgenic mice. NPJ Aging Mech Dis. 2017;3:15.
Dominy SS, Lynch C, Ermini F, Benedyk M, Marczyk A, Konradi A, et al. Porphyromonas gingivalis in Alzheimer’s disease brains: evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv. 2019;5:eaau3333.
Liu Y, Wu Z, Nakanishi Y, Ni J, Hayashi Y, Takayama F, et al. Infection of microglia with Porphyromonas gingivalis promotes cell migration and an inflammatory response through the gingipain-mediated activation of protease-activated receptor-2 in mice. Sci Rep. 2017;7:11759.
Ilievski V, Zuchowska PK, Green SJ, Toth PT, Ragozzino ME, Le K, et al. Chronic oral application of a periodontal pathogen results in brain inflammation, neurodegeneration and amyloid beta production in wild type mice. PLoS One. 2018;13:e0204941.
Yonezawa H, Osaki T, Hanawa T, Kurata S, Zaman C, Woo TD, et al. Destructive effects of butyrate on the cell envelope of Helicobacter pylori. J Med Microbiol. 2012;61:582–9.
Sekiya M, Shimoyama Y, Ishikawa T, Sasaki M, Futai M, Nakanishi-Matsui M. Porphyromonas gingivalis is highly sensitive to inhibitors of a proton-pumping ATPase. Biochem Biophys Res Commun. 2018;498:837–41.
Roubaud-Baudron C, Krolak-Salmon P, Quadrio I, Megraud F, Salles N. Impact of chronic Helicobacter pylori infection on Alzheimer’s disease: preliminary results. Neurobiol Aging. 2012;33:1009.e11-9. https://doi.org/10.1016/j.neurobiolaging.2011.10.021.
D’Elios MM, Amedei A, Benagiano M, Azzurri A, Del Prete G. Helicobacter pylori, T cells and cytokines: the “dangerous liaisons”. FEMS Immunol Med Microbiol. 2005;44:113–9.
Harris SA, Harris EA. Herpes simplex virus type 1 and other pathogens are key causative factors in sporadic Alzheimer’s disease. J Alzheimer's Dis. 2015;48:319–53.
Acknowledgements
The authors would like to thank Mr. Negasi Beyene (CDC/NCHS/RDC) and Mr. Ray Kuntz (AHRQ) for their help with access to the restricted data at the RDC and facilitating data analysis at the AHRQ headquarters, Rockville, MD. We would also like to thank Ms. Megan Williams and Ms. Nicolle Mode (NIA/NIH/IRP) for internally reviewing our manuscript.
Funding
This study was entirely supported by the National Institute on Aging, Intramural Research Program (NIA/NIH/IRP).
Author information
Authors and Affiliations
Contributions
MAB: Study concept, plan of analysis, data management, statistical analysis, literature search, write-up of the manuscript, revision of the manuscript. HAB: Plan of analysis, literature search and review, write-up of parts of the manuscript, revision of the manuscript. JW: Assistance with statistical analysis, write-up of parts of the manuscript, revision of the manuscript. SH: Plan of analysis, literature search and review, write-up of parts of the manuscript, revision of the manuscript. ZE-H: Literature search and review, write-up of parts of the manuscript, revision of the manuscript. ABZ: Study concept, plan of analysis, write-up of parts of the manuscript, revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Disclosure
The views expressed in this article are those of the author(s) and do not reflect the official policy of the Department of the Army/Navy/Air Force, Department of Defense, or the U.S. Government.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Beydoun, M.A., Beydoun, H.A., Weiss, J. et al. Helicobacter pylori, periodontal pathogens, and their interactive association with incident all-cause and Alzheimer’s disease dementia in a large national survey. Mol Psychiatry 26, 6038–6053 (2021). https://doi.org/10.1038/s41380-020-0736-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-020-0736-2
This article is cited by
-
The association between periodontal diseases and helicobacter pylori: an updated meta-analysis of observational studies
BMC Oral Health (2023)
-
Advances in Molecular Psychiatry – March 2023: mitochondrial function, stress, neuroinflammation – bipolar disorder, psychosis, and Alzheimer’s disease
Molecular Psychiatry (2023)
-
Nutrition in Alzheimer’s disease: a review of an underappreciated pathophysiological mechanism
Science China Life Sciences (2023)
-
Dementia, infections and vaccines: 30 years of controversy
Aging Clinical and Experimental Research (2023)
-
Gut- and oral-dysbiosis differentially impact spinal- and bulbar-onset ALS, predicting ALS severity and potentially determining the location of disease onset
BMC Neurology (2022)