Abstract
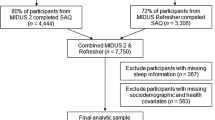
Prior research suggests that sleep disturbances are associated with increased risk of suicide. However, sleep disturbances are associated with a wide range of psychiatric disorders, and it is unknown whether this association is independent of psychopathology. In a large nationally representative prospective survey, the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), we used structural equation modeling to examine the shared and specific effects of three sleep complaints (i.e., trouble falling asleep, early morning awakening, and hypersomnia) on the 3-year occurrence of attempting suicide. Because psychiatric disorders increase the risk of suicide attempt almost exclusively through a general psychopathology factor representing their shared effect, covariates included that factor, prior history of suicide attempt, and a wide range of sociodemographic and clinical characteristics. The 3-year prevalence rate of suicide attempt was 0.6% (n = 241). Compared with participants who did not attempt suicide between the two waves, those who did reported significantly more frequently having trouble falling asleep (44.6% vs. 16.6%), early morning awakening (38.9% vs. 12.7%), and hypersomnia (35.0% vs. 10.7%). Following adjustments, effects of sleep complaints on this risk were significant and exerted almost exclusively through a general sleep complaints factor representing the shared effect across all sleep complaints. There were no residual associations of any individual sleep complaint with attempting suicide above that association. Sleep complaints are associated with an increased risk of attempting suicide independently of psychopathology, and should be included in suicide risk assessments as these symptoms may provide targets for reducing the risks of suicidal behaviors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The original data set for the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) is available from the National Institute on Alcohol Abuse and Alcoholism (http://www.niaaa.nih.gov).
References
World Health Organization. Global health estimates 2013: deaths by cause, age and sex, estimates for 2000–2012. Geneva: World Health Organization; 2014.
WHO|Suicide data. World Health Organization. https://www.who.int/mental_health/prevention/suicide/suicideprevent/en/. Accessed 16 Jan 2017.
Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159:909–16.
Krakow B, Ribeiro JD, Ulibarri VA, Krakow J, Joiner TE. Sleep disturbances and suicidal ideation in sleep medical center patients. J Affect Disord. 2011;131:422–7.
Bernert RA, Joiner TE, Cukrowicz KC, Schmidt NB, Krakow B. Suicidality and sleep disturbances. Sleep. 2005;28:1135–41.
Fawcett J, Scheftner WA, Fogg L, Clark DC, Young MA, Hedeker D, et al. Time-related predictors of suicide in major affective disorder. Am J Psychiatry. 1990;147:1189–94.
Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73:e1160–67.
Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatry Rep. 2015;17:554.
Sateia MJ. Update on sleep and psychiatric disorders. Chest. 2009;135:1370–9.
Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, et al. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. 2016;142:969–90.
Geoffroy PA, Hoertel N, Etain B, Bellivier F, Delorme R, Limosin F, et al. Insomnia and hypersomnia in major depressive episode: prevalence, sociodemographic characteristics and psychiatric comorbidity in a population-based study. J Affect Disord. 2018;226:132–41.
Courtet P, Gottesman II, Jollant F, Gould TD. The neuroscience of suicidal behaviors: what can we expect from endophenotype strategies?. Transl Psychiatry. 2011;1:e7.
Pascal de Raykeer R, Hoertel N, Blanco C, Olfson M, Wall M, Seigneurie A-S, et al. Effects of psychiatric disorders on suicide attempt: similarities and differences between older and younger adults in a national cohort study. J Clin Psychiatry. 2018;79;pii: 17m11911; https://doi.org/10.4088/JCP.17m11911.
Hoertel N, Franco S, Wall MM, Oquendo MA, Kerridge BT, Limosin F, et al. Mental disorders and risk of suicide attempt: a national prospective study. Mol Psychiatry. 2015;20:718–26.
Hoertel N, Blanco C, Olfson M, Oquendo MA, Wall MM, Franco S, et al. A comprehensive model of predictors of suicide attempt in depressed individuals and effect of treatment-seeking behavior: results from a national 3-year prospective study. J Clin Psychiatry. 2018;79:17m11704. https://doi.org/10.4088/JCP.17m11704.
Liu T-Z, Xu C, Rota M, Cai H, Zhang C, Shi M-J, et al. Sleep duration and risk of all-cause mortality: a flexible, non-linear, meta-regression of 40 prospective cohort studies. Sleep Med Rev. 2017;32:28–36.
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92.
Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14:1051–66.
Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39:37–44.
Chatterji S, Saunders JB, Vrasti R, Grant BF, Hasin D, Mager D. Reliability of the alcohol and drug modules of the Alcohol Use Disorder and Associated Disabilities Interview Schedule-Alcohol/Drug-Revised (AUDADIS-ADR): an international comparison. Drug Alcohol Depend. 1997;47:171–85.
Canino G, Bravo M, Ramírez R, Febo VE, Rubio-Stipec M, Fernández RL, et al. The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability and concordance with clinical diagnoses in a Hispanic population. J Stud Alcohol. 1999;60:790–9.
Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16.
Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend. 1997;44:133–41.
Koffel E, Watson D. The two-factor structure of sleep complaints and its relation to depression and anxiety. J Abnorm Psychol. 2009;118:183–94.
Hoertel N, Faiz H, Airagnes G, Blanco C, Pascal De Raykeer R, Franco S, et al. A comprehensive model of predictors of suicide attempt in heavy drinkers: results from a national 3-year longitudinal study. Drug Alcohol Depend. 2018;186:44–52.
Blanco C, Wall MM, Hoertel N, Krueger RF, Liu S-M, Grant BF, et al. Psychiatric disorders and risk for multiple adverse outcomes: a national prospective study. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0459-4. Accessed 26 Jul 2019.
Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model: Multidiscip J. 1999;6:1–55.
Britton PC, McKinney JM, Bishop TM, Pigeon WR, Hirsch JK. Insomnia and risk for suicidal behavior: a test of a mechanistic transdiagnostic model in veterans. J Affect Disord. 2019;245:412–8.
Titus CE, Speed KJ, Cartwright PM, Drapeau CW, Heo Y, Nadorff MR. What role do nightmares play in suicide? A brief exploration. Curr Opin Psychol. 2018;22:59–62.
Liu X. Sleep and adolescent suicidal behavior. Sleep. 2004;27:1351–8.
Cassé-Perrot C, Lanteaume L, Deguil J, Bordet R, Auffret A, Otten L, et al. Neurobehavioral and cognitive changes induced by sleep deprivation in healthy volunteers. CNS Neurol Disord Drug Targets. 2016;15:777–801.
Geoffroy PA, Tebeka S, Blanco C, Dubertret C, Le Strat Y. Shorter and longer durations of sleep are associated with an increased twelve-month prevalence of psychiatric and substance use disorders: findings from a nationally representative survey of US adults (NESARC-III). J Psychiatr Res. 2020;124:34–41.
Killgore WDS. Effects of sleep deprivation on cognition. Prog Brain Res. 2010;185:105–29.
Oldershaw A, Grima E, Jollant F, Richards C, Simic M, Taylor L, et al. Decision making and problem solving in adolescents who deliberately self-harm. Psychol Med. 2009;39:95–104.
Jollant F, Bellivier F, Leboyer M, Astruc B, Torres S, Verdier R, et al. Impaired decision making in suicide attempters. Am J Psychiatry. 2005;162:304–10.
Porras-Segovia A, Pérez-Rodríguez MM, López-Esteban P, Courtet P, Barrigón MML, López-Castromán J, et al. Contribution of sleep deprivation to suicidal behaviour: a systematic review. Sleep Med Rev. 2019;44:37–47.
Gevers W, Deliens G, Hoffmann S, Notebaert W, Peigneux P. Sleep deprivation selectively disrupts top-down adaptation to cognitive conflict in the Stroop test. J Sleep Res. 2015;24:666–72.
Lamis DA, Innamorati M, Erbuto D, Berardelli I, Montebovi F, Serafini G, et al. Nightmares and suicide risk in psychiatric patients: the roles of hopelessness and male depressive symptoms. Psychiatry Res. 2018;264:20–5.
Liu X, Liu Z-Z, Wang Z-Y, Yang Y, Liu B-P, Jia C-X. Daytime sleepiness predicts future suicidal behavior: a longitudinal study of adolescents. Sleep. 2019;42. https://doi.org/10.1093/sleep/zsy225.
McMahon K, Hoertel N, Olfson M, Wall M, Wang S, Blanco C. Childhood maltreatment and impulsivity as predictors of interpersonal violence, self-injury and suicide attempts: a national study. Psychiatry Res. 2018;269:386–93.
Ludwig B, Dwivedi Y. The concept of violent suicide, its underlying trait and neurobiology: a critical perspective. Eur Neuropsychopharmacol. 2018;28:243–51.
Fanelli G, Serretti A. The influence of the serotonin transporter gene 5-HTTLPR polymorphism on suicidal behaviors: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;88:375–87.
Deuschle M, Schredl M, Schilling C, Wüst S, Frank J, Witt SH, et al. Association between a serotonin transporter length polymorphism and primary insomnia. Sleep. 2010;33:343–7.
Palagini L, Bastien CH, Marazziti D, Ellis JG, Riemann D. The key role of insomnia and sleep loss in the dysregulation of multiple systems involved in mood disorders: a proposed model. J Sleep Res. 2019;28:e12841.https://doi.org/10.1111/jsr.12841.
Brundin L, Bryleva EY, Thirtamara Rajamani K. Role of inflammation in suicide: from mechanisms to treatment. Neuropsychopharmacology. 2017;42:271–83.
Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. 2016;80:40–52.
Irwin MR, Opp MR. Sleep health: reciprocal regulation of sleep and innate immunity. Neuropsychopharmacology. 2017;42:129–55.
Vgontzas AN, Zoumakis M, Papanicolaou DA, Bixler EO, Prolo P, Lin H-M, et al. Chronic insomnia is associated with a shift of interleukin-6 and tumor necrosis factor secretion from nighttime to daytime. Metab Clin Exp. 2002;51:887–92.
Lindqvist D, Janelidze S, Hagell P, Erhardt S, Samuelsson M, Minthon L, et al. Interleukin-6 is elevated in the cerebrospinal fluid of suicide attempters and related to symptom severity. Biol Psychiatry. 2009;66:287–92.
Wang Q, Roy B, Turecki G, Shelton RC, Dwivedi Y. Role of complex epigenetic switching in tumor necrosis factor-α upregulation in the prefrontal cortex of suicide subjects. Am J Psychiatry. 2018;175:262–74.
Meerlo P, Sgoifo A, Suchecki D. Restricted and disrupted sleep: effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Med Rev. 2008;12:197–210.
Tsujino N, Yamanaka A, Ichiki K, Muraki Y, Kilduff TS, Yagami K, et al. Cholecystokinin activates orexin/hypocretin neurons through the cholecystokinin A receptor. J Neurosci. 2005;25:7459–69.
Jahangard L, Solgy R, Salehi I, Taheri SK, Holsboer-Trachsler E, Haghighi M, et al. Cholecystokinin (CCK) level is higher among first time suicide attempters than healthy controls, but is not associated with higher depression scores. Psychiatry Res. 2018;266:40–6.
Littlewood DL, Kyle SD, Carter L-A, Peters S, Pratt D, Gooding P. Short sleep duration and poor sleep quality predict next-day suicidal ideation: an ecological momentary assessment study. Psychol Med. 2019;49:403–11.
Bernert RA, Hom MA, Iwata NG, Joiner TE. Objectively assessed sleep variability as an acute warning sign of suicidal ideation in a longitudinal evaluation of young adults at high suicide risk. J Clin Psychiatry. 2017;78:e678–87.
Agargun MY, Cartwright R. REM sleep, dream variables and suicidality in depressed patients. Psychiatry Res. 2003;119:33–9.
Ballard ED, Vande Voort JL, Bernert RA, Luckenbaugh DA, Richards EM, Niciu MJ, et al. Nocturnal wakefulness is associated with next-day suicidal ideation in major depressive disorder and bipolar disorder. J Clin Psychiatry. 2016;77:825–31.
Boudebesse C, Geoffroy PA, Bellivier F, Henry C, Folkard S, Leboyer M, et al. Correlations between objective and subjective sleep and circadian markers in remitted patients with bipolar disorder. Chronobiol Int. 2014;31:698–704.
Geoffroy PA, Boudebesse C, Bellivier F, Lajnef M, Henry C, Leboyer M, et al. Sleep in remitted bipolar disorder: a naturalistic case-control study using actigraphy. J Affect Disord. 2014;158:1–7.
Kaplan KA, Gruber J, Eidelman P, Talbot LS, Harvey AG. Hypersomnia in inter-episode bipolar disorder: does it have prognostic significance? J Affect Disord. 2011;132:438–44.
Lichstein KL, Durrence HH, Taylor DJ, Bush AJ, Riedel BW. Quantitative criteria for insomnia. Behav Res Ther. 2003;41:427–45.
Arfken CL, Joseph A, Sandhu GR, Roehrs T, Douglass AB, Boutros NN. The status of sleep abnormalities as a diagnostic test for major depressive disorder. J Affect Disord. 2014;156:36–45.
Geoffroy PA, Scott J, Boudebesse C, Lajnef M, Henry C, Leboyer M, et al. Sleep in patients with remitted bipolar disorders: a meta-analysis of actigraphy studies. Acta Psychiatr Scand. 2015;131:89–99.
Lopez J, Hoffmann R, Armitage R. Reduced sleep spindle activity in early-onset and elevated risk for depression. J Am Acad Child Adolesc Psychiatry. 2010;49:934–43.
Pillai V, Kalmbach DA, Ciesla JA. A meta-analysis of electroencephalographic sleep in depression: evidence for genetic biomarkers. Biol Psychiatry. 2011;70:912–9.
Le Strat Y, Hoertel N. Correlation is no causation: gymnasium proliferation and the risk of obesity. Addiction. 2011;106:1871–2.
Acknowledgements
The sponsors had no additional role in the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MAO receives royalties for the commercial use of the C-SSRS, owns shares in Mantra Inc., and her family owns stock in Bristol Myers Squibb. FL has received speaker and consulting fees from AstraZeneca, Janssen, Lundbeck, Otsuka Pharmaceuticals, Roche and Servier outside the submitted work. Other authors report no conflicts of interest.
Disclaimer
The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or the US government.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Geoffroy, P.A., Oquendo, M.A., Courtet, P. et al. Sleep complaints are associated with increased suicide risk independently of psychiatric disorders: results from a national 3-year prospective study. Mol Psychiatry 26, 2126–2136 (2021). https://doi.org/10.1038/s41380-020-0735-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-020-0735-3
This article is cited by
-
Sleep and circadian rhythms in adolescents with attempted suicide
Scientific Reports (2024)
-
Evaluation and management of insomnia in the clinical practice in Italy: a 2023 update from the Insomnia Expert Consensus Group
Journal of Neurology (2024)
-
Abnormal alterations of regional spontaneous neuronal activity and functional connectivity in insomnia patients with difficulty falling asleep: a resting-state fMRI study
BMC Neurology (2023)
-
Insomnia During the Perinatal Period and its Association with Maternal and Infant Psychopathology: A Systematic Review and Meta-Analysis
Current Psychiatry Reports (2023)
-
Self-reported sleep and exercise patterns in patients admitted with suicidal attempts: a cross-sectional comparative study
BMC Psychiatry (2022)