Abstract
The brain regions responsible for hallucinations remain unclear. We studied 89 brain lesions causing hallucinations using a recently validated technique termed lesion network mapping. We found that hallucinations occurred following lesions to a variety of different brain regions, but these lesion locations fell within a single functionally connected brain network. This network was defined by connectivity to the cerebellar vermis, inferior cerebellum (bilateral lobule X), and the right superior temporal sulcus. Within this single hallucination network, additional connections with the lesion location dictated the sensory modality of the hallucination: lesions causing visual hallucinations were connected to the lateral geniculate nucleus in the thalamus while lesions causing auditory hallucinations were connected to the dentate nucleus in the cerebellum. Our results suggest that lesions causing hallucinations localize to a single common brain network, but additional connections within this network dictate the sensory modality, lending insight into the causal neuroanatomical substrate of hallucinations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
American Psychological Association. APA dictionary of psychology. Washington, DC: American Psychological Association. 2018. https://dictionary.apa.org/hallucination.
Aleman A. Hallucinations: the science of idiosyncratic perception. 1st ed. Washington, DC: American Psychological Association; 2008.
Laroi F. The phenomenological diversity of hallucinations: some theoretical and clinical implications. Psychol Belg. 2006;46:163–83.
Clark ML, Waters F, Vatskalis TM, Jablensky A. On the interconnectedness and prognostic value of visual and auditory hallucinations in first-episode psychosis. Eur Psychiatry. 2017;41:122–8.
Barone P, Antonini A, Colosimo C, Marconi R, Morgante L, Avarello TP, et al. The PRIAMO study: a multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson’s disease. Mov Disord. 2009;24:1641–9.
Schrag A, Hovris A, Morley D, Quinn N, Jahanshahi M. Caregiver-burden in parkinson’s disease is closely associated with psychiatric symptoms, falls, and disability. Parkinsonism Relat Disord. 2006;12:35–41.
Zmigrod L, Garrison JR, Carr J, Simons JS. The neural mechanisms of hallucinations: a quantitative meta-analysis of neuroimaging studies. Neurosci Biobehav Rev. 2016;69:113–23.
Asaad G, Shapiro B. Hallucinations: theoretical and clinical overview. Am J Psychiatry. 1986;143:1088–97.
David AS. The cognitive neuropsychiatry of auditory verbal hallucinations: an overview. Cogn Neuropsychiatry. 2004;9:107–23.
Allen P, Laroi F, McGuire PK, Aleman A. The hallucinating brain: a review of structural and functional neuroimaging studies of hallucinations. Neurosci Biobehav Rev. 2008;32:175–91.
Jardri R, Thomas P, Delmaire C, Delion P, Pins D. The neurodynamic organization of modality-dependent hallucinations. Cereb Cortex. 2013;23:1108–17.
Rolland B, Amad A, Poulet E, Bordet R, Vignaud A, Bation R, et al. Resting-state functional connectivity of the nucleus accumbens in auditory and visual hallucinations in schizophrenia. Schizophr Bull. 2015;41:291–9.
Garrison JR, Fernyhough C, McCarthy-Jones S, Haggard M, Simons JS. Paracingulate sulcus morphology is associated with hallucinations in the human brain. Nat Commun. 2015;6:8956.
Jardri R, Pouchet A, Pins D, Thomas P. Cortical activations during auditory verbal hallucinations in schizophrenia: a coordinate-based meta-analysis. Am J Psychiatry. 2011;168:73–81.
Braun CM, Dumont M, Duval J, Hamel-Hebert I, Godbout L. Brain modules of hallucination: an analysis of multiple patients with brain lesions. J Psychiatry Neurosci. 2003;28:432–49.
Fox MD. Mapping symptoms to brain networks with the human connectome. N Engl J Med. 2018;379:2237–45.
Karnath HO, Sperber C, Rorden C. Mapping human brain lesions and their functional consequences. Neuroimage. 2018;165:180–9.
Adolphs R. Human lesion studies in the 21st century. Neuron. 2016;90:1151–3.
Morenas-Rodriguez E, Camps-Renom P, Perez-Cordon A, Horta-Barba A, Simon-Talero M, Cortes-Vicente E, et al. Visual hallucinations in patients with acute stroke: a prospective exploratory study. Eur J Neurol. 2017;24:734–40.
Boes AD, Prasad S, Liu H, Liu Q, Pascual-Leone A, Caviness VS Jr., et al. Network localization of neurological symptoms from focal brain lesions. Brain. 2015;138(Pt 10):3061–75.
Carrera E, Tononi G. Diaschisis: past, present, future. Brain. 2014;137(Pt 9):2408–22.
Fox MD, Buckner RL, Liu H, Chakravarty MM, Lozano AM, Pascual-Leone A. Resting-state networks link invasive and noninvasive brain stimulation across diverse psychiatric and neurological diseases. Proc Natl Acad Sci USA. 2014;111:E4367–75.
Horn A, Reich M, Vorwerk J, Li N, Wenzel G, Fang Q, et al. Connectivity predicts deep brain stimulation outcome in Parkinson disease. Ann Neurol. 2017;82:67–78.
Weigand A, Horn A, Caballero R, Cooke D, Stern AP, Taylor SF, et al. Prospective nMagnetic stimulation sites. Biol Psychiatry. 2018;84:28–37.
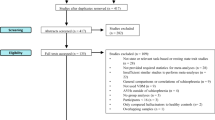
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9.
Darby RR, Laganiere S, Pascual-Leone A, Prasad S, Fox MD. Finding the imposter: brain connectivity of lesions causing delusional misidentifications. Brain. 2016;140:497–507.
Corp DT, Joutsa J, Darby RR, Delnooz CCS, van de Warrenburg BPC, Cooke D, et al. Network localization of cervical dystonia based on causal brain lesions. Brain. 2019;142:1660–74.
Darby RR, Horn A, Cushman F, Fox MD. Lesion network localization of criminal behavior. Proc Natl Acad Sci USA. 2018;115:601–6.
Darby RR, Joutsa J, Burke MJ, Fox MD. Lesion network localization of free will. Proc Natl Acad Sci USA. 2018;115:10792–7.
Joutsa J, Horn A, Hsu J, Fox MD. Localizing parkinsonism based on focal brain lesions. Brain. 2018;141:2445–56.
Joutsa J, Shih LC, Horn A, Reich MM, Wu O, Rost NS, et al. Identifying therapeutic targets from spontaneous beneficial brain lesions. Ann Neurol. 2018;84:153–7.
Wu O, Cloonan L, Mocking SJ, Bouts MJ, Copen WA, Cougo-Pinto PT, et al. Role of acute lesion topography in initial ischemic stroke severity and long-term functional outcomes. Stroke. 2015;46:2438–44.
Powers AR, Mathys C, Corlett P. Pavlovian conditioning–induced hallucinations result from overweighting of perceptual priors. Science. 2017;357:596–600.
Ffytche DH. The hodology of hallucinations. Cortex. 2008;44:1067–83.
Ramnani N. The primate cortico-cerebellar system: anatomy and function. Nat Rev Neurosci. 2006;7:511–22.
Andreasen NC, Pierson R. The role of the cerebellum in schizophrenia. Biol Psychiatry. 2008;64:81–8.
Schmahmann JD. Disorders of the cerebellum: ataxia, dysmetria of thought, and the cerebellar cognitive affective syndrome. J Neuropsychiatry Clin Neurosci. 2004;16:367–78.
Okugawa G, Sedvall GC, Agartz I. Smaller cerebellar vermis but not hemisphere volumes in patients with chronic schizophrenia. Am J Psychiatry. 2003;160:1614–7.
Park HS, KIm BS, Kim YK, Yang YS, Cho SS, Kim SY, et al. Different cerebral metabolic features in dementia with Lewy bodies with/without visual hallucination. J Nucl Med. 2008;49(supplement 1):36P–P.
Pagonabarraga J, Soriano-Mas C, Llebaria G, Lopez-Sola M, Pujol J, Kulisevsky J. Neural correlates of minor hallucinations in non-demented patients with Parkinson’s disease. Parkinsonism Relat Disord. 2014;20:290–6.
McAuley T, Brahmbhatt S, Barch DM. Performance on an episodic encoding task yields further insight into functional brain development. Neuroimage. 2007;34:815–26.
Mesulam MM. From sensation to cognition. Brain. 1998;121(Pt 6):1013–52.
Jones E, Powell T. An anatomical study of converging sensory pathways within the cerebral cortex of the monkey. Brain. 1970;93:793–820.
Beauchamp MS, Lee KE, Argall BD, Martin A. Integration of auditory and visual information about objects in superior temporal sulcus. Neuron. 2004;41:809–23.
Santhouse AM, Howard RJ, ffytche DH. Visual hallucinatory syndromes and the anatomy of the visual brain. Brain. 2000;123:2055–64.
Friston KJ. Hallucinations and perceptual inference. Behav Brain Sci. 2005;28:764–6.
Rajesh PNR, Dana HB. Predictive coding in the visual cortex: a functional interpretation of some extra-classical receptive-field effects. Nat Neurosci. 1999;2:79.
Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, et al. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. 2007;27:2349–56.
Palaniyappan L, Mallikarjun P, Joseph V, White TP, Liddle PF. Reality distortion is related to the structure of the salience network in schizophrenia. Psychol Med. 2011;41:1701–8.
White TP, Joseph V, Francis ST, Liddle PF. Aberrant salience network (bilateral insula and anterior cingulate cortex) connectivity during information processing in schizophrenia. Schizophr Res. 2010;123:105–15.
Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15:483–506.
Jones EG. The Thalamus. New York: Plenum Press; 1985.
Manford M, Andermann F. Complex visual hallucinations. Clin neurobiological insights Brain. 1998;121(Pt 10):1819.
Geddes MR, Tie Y, Gabrieli JD, McGinnis SM, Golby AJ, Whitfield-Gabrieli S. Altered functional connectivity in lesional peduncular hallucinosis with REM sleep behavior disorder. Cortex. 2016;74:96–106.
Weil RS, Hsu JK, Darby RR, Soussand L, Fox MD. Neuroimaging in Parkinson’s disease dementia: connecting the dots. Brain Commun. 2019;1. https://doi.org/10.1093/braincomms/fcz006. [Epub ahead of print].
Leiner HC, Leiner AL, Dow RS. Cognitive and language functions of the human cerebellum. Trends Neurosci. 1993;16:444–7.
Kotz SA, Schwartze M. Cortical speech processing unplugged: a timely subcortico-cortical framework. Trends Cogn Sci. 2010;14:392–9.
Thürling M, Küper M, Stefanescu R, Maderwald S, Gizewski E, Ladd ME, et al. Activation of the dentate nucleus in a verb generation task: a 7 T MRI study. Neuroimage. 2011;57:1184–91.
Curcic-Blake B, Ford JM, Hubl D, Orlov ND, Sommer IE, Waters F, et al. Interaction of language, auditory and memory brain networks in auditory verbal hallucinations. Prog Neurobiol. 2017;148:1–20.
Cheng DT, Meintjes EM, Stanton ME, Desmond JE, Pienaar M, Dodge NC, et al. Functional MRI of cerebellar activity during eyeblink classical conditioning in children and adults. Hum Brain Mapp. 2014;35:1390–403.
Ffytche DH, Howard RJ, Brammer MJ, David A, Woodruff P, Williams S. The anatomy of conscious vision: an fMRI study of visual hallucinations. Nat Neurosci. 1998;1:738–42.
Zhang S, Xu M, Kamigaki T, Hoang Do JP, Chang WC, Jenvay S, et al. Selective attention. Long-range and local circuits for top-down modulation of visual cortex processing. Science. 2014;345:660–5.
Hirsch JA, Wang X, Sommer FT, Martinez LM. How inhibitory circuits in the thalamus serve vision. Annu Rev Neurosci. 2015;38:309–29.
Carcea I, Froemke RC. Cortical plasticity, excitatory-inhibitory balance, and sensory perception. Prog Brain Res. 2013;207:65–90.
Jardri R, Hugdahl K, Hughes M, Brunelin J, Waters F, Alderson-Day B, et al. Are hallucinations due to an imbalance between excitatory and inhibitory influences on the brain? Schizophr Bull. 2016;42:1124–34.
Lee I, Nielsen K, Nawaz U, Hall MH, Ongur D, Keshavan M, et al. Diverse pathophysiological processes converge on network disruption in mania. J Affect Disord. 2019;244:115–23.
Waters F, Fernyhough C. Hallucinations: a systematic review of points of similarity and difference across diagnostic classes. Schizophr Bull. 2017;43:32–43.
Padmanabhan JL, Cooke D, Joutsa J, Siddiqi SH, Ferguson M, Darby RR, et al. A human depression circuit derived from focal brain lesions. Biol Psychiatry. 2019. https://doi.org/10.1016/j.biopsych.2019.07.023.
Orlov ND, Giampietro V, O’Daly O, Lam SL, Barker GJ, Rubia K, et al. Real-time fMRI neurofeedback to down-regulate superior temporal gyrus activity in patients with schizophrenia and auditory hallucinations: a proof-of-concept study. Transl Psychiatry. 2018;8:46.
Slotema CW, Blom JD, van Lutterveld R, Hoek HW, Sommer IE. Review of the efficacy of transcranial magnetic stimulation for auditory verbal hallucinations. Biol Psychiatry. 2014;76:101–10.
Merabet LB, Kobayashi M, Barton J, Pascual-Leone A. Suppression of complex visual hallucinatory experiences by occipital transcranial magnetic stimulation: a case report. Neurocase. 2003;9:436–40.
Bürgel U, Amunts K, Hoemke L, Mohlberg H, Gilsbach JM, Zilles K. White matter fiber tracts of the human brain: three-dimensional mapping at microscopic resolution, topography and intersubject variability. Neuroimage. 2006;29:1092–105.
Diedrichsen J, Maderwald S, Küper M, Thürling M, Rabe K, Gizewski E, et al. Imaging the deep cerebellar nuclei: a probabilistic atlas and normalization procedure. Neuroimage. 2011;54:1786–94.
Acknowledgements
DT was supported by a DuPont-Warren Fellowship Award from Harvard Medical School. JJ was supported by funding from the Academy of Finland #295580, the Finnish Medical Foundation, and a grant from the Orion Research Foundation. JMF was supported by RETICS INVICTUS PLUS (RD06/0019/0010) and FEDER. MDF was supported by the National Institute of Mental Health (R01MH113929), Nancy Lurie Marks Foundation, and Mathers Foundation. None of the institutions mentioned above have a role in the design and conduct of the study, in the collection, management, analysis, and interpretation of the data, in the preparation, review, or approval of the manuscript, nor in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
NYK, JH, and MDF conceived and designed the work; NYK, JJ, OW, NR, EMR, and JMF acquired the data; NYK, JH, JJ, LS, APL, and MDF analyzed and interpreted data; NYK, DT, and MDF drafted the work; PRC, APL, and MDF revised the manuscript critically for important intellectual content; all authors approved the final version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. NYK and MDF had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kim, N.Y., Hsu, J., Talmasov, D. et al. Lesions causing hallucinations localize to one common brain network. Mol Psychiatry 26, 1299–1309 (2021). https://doi.org/10.1038/s41380-019-0565-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-019-0565-3
This article is cited by
-
Cerebellar Transcranial Magnetic Stimulation in Psychiatric Disorders: A Systematic Review
Current Behavioral Neuroscience Reports (2024)
-
Using causal methods to map symptoms to brain circuits in neurodevelopment disorders: moving from identifying correlates to developing treatments
Journal of Neurodevelopmental Disorders (2022)
-
Multimodal and multidomain lesion network mapping enhances prediction of sensorimotor behavior in stroke patients
Scientific Reports (2022)
-
Causal mapping of human brain function
Nature Reviews Neuroscience (2022)
-
A depression network caused by brain tumours
Brain Structure and Function (2022)