Abstract
In managing patients with solid tumors, the value of detecting the status of tumor DNA mismatch repair function is widely recognized. Mismatch repair protein immunohistochemistry and molecular microsatellite instability testing constitute the two major test modalities currently in use, yet each is associated with caveats and limitations that can be consequential. Most notably, the traditional approach of defining mismatch repair protein immunohistochemistry abnormality by complete loss of staining in all tumor cells is evolving. Partial or clonal loss is becoming recognized as a manifestation of gene abnormality; in some cases, such clonal loss is associated with germline pathogenic variants. The current criteria and cutoff values for defining microsatellite instability-high are developed primarily according to colorectal tumors. Non-colorectal cases, and occasionally even colorectal tumors, that are mismatch repair-deficient by immunohistochemistry but not microsatellite instability-high by current standards are being recognized. Emerging data suggest that these immunohistochemistry abnormal / non-microsatellite instability-high cases warrant further genetic workup for Lynch syndrome detection. Whether these tumors respond to immunotherapy is a question still to be addressed. It is imperative that pathologists as well as clinicians and investigators be aware of such intricacies regarding routine immunohistochemistry and microsatellite instability testing and the results they generate. This review summarizes our current understanding of the advantages and limitations of these tests and offer our view on what constitutes the most optimal strategy in test selection and how best to utilize case context to enhance the interpretation of the test results.
Similar content being viewed by others
Introduction
In human cells, the process of DNA mismatch repair (MMR) deficiency starts when a major MMR gene (MLH1, MSH2, MSH6, or PMS2) is inactivated via germline and/or somatic mutations or epigenetic silencing. This is followed by loss of the MMR protein which then leads to loss of MMR function and subsequent accumulation of non-repaired mismatch mistakes (base-base mismatches and insertion-deletion [indel] errors) in the repetitive DNA sequences known as microsatellites. When such altered or “unstable” microsatellites involve the coding or other functionally important sequences of cancer-associated genes, tumor initiation or accelerated progression ensues1,2,3,4,5. These mutations, particularly the indels, can also cause exonic sequence frameshifting and generate unique neopeptides, that in turn elicit robust T cell infiltration in the tumor, bringing about a heightened tumor immune microenvironment6,7.
There are two major categories of tissue-based testing currently in use for the detection of the status of MMR8,9,10,11,12,13,14. One is MMR immunohistochemistry (IHC) which detects the MMR proteins in the cells (in this review, MMRd and MMRp specifically refer to MMR protein deficient or proficient as detected by IHC). The other is microsatellite instability (MSI) testing which detects the unstable microsatellites (in this review, MSI-H, MSI-L, MSI-I, and MSS refer to microsatellite instability-high, low, indeterminate, and microsatellite stable, respectively, as detected by MSI testing). Various PCR- and next-generation sequencing (NGS)-based MSI testing platforms have been developed; the classic assay that was standardized early on is the PCR-MSI1 utilizing a National Cancer Institute (NCI)-endorsed panel of five microsatellite markers.
MMR IHC and MSI testing are garnering growing attention owing to the significant implications of the test results (MMR loss signifying increased risk of Lynch syndrome [LS] and likelihood of responding to immunotherapy) on the one hand, and the persistence of certain limitations to the testing methodologies on the other. As technologies evolve, various test-related questions remain open, such as “is one test sufficient”, “if both are needed, what would the best strategy be to incorporate them into routine clinical practice”, and “how best to deal with discrepant results from the two types of tests”.
This review provides an updated summary of our current understanding of the advantages and limitations of these two tests and offers our view on what constitutes best strategies in selecting tests and interpreting results. Special emphasis is placed on (1) the changing IHC definition of MMRd, and (2) the potential clinical implication of cases with “MMRd/non-MSI-H”.
MMR immunohistochemistry
MMR IHC has been in use for more than two decades15. For the vast majority of the cases, the test is easy and yields straightforward results. Most tumors show the presence of nuclear staining for all four proteins, indicative of MMRp. The MMRd cases typically manifest loss of MLH1 and PMS2 (associated with MLH1 inactivation), loss of MSH2 and MSH6 (associated with MSH2 inactivation), loss of MSH6 alone (associated with MSH6 inactivation), or loss of PMS2 alone (associated with PMS2 inactivation). In these MMRd cases, the loss of staining is frequently uniform throughout the tumor.
Advantages
A number of salient features of MMR IHC are generally accepted as advantageous. They include:
-
Wide availability in routine diagnostic laboratories.
-
Fast turn-around time.
-
Relatively low cost.
-
Feasibility in samples with <20% tumor content.
-
Amenability to IHC external quality assurance measures. Proficiency tests and recommended protocols offered by organizations such as the College of American Pathologists (CAP) and Nordic immunohistochemical Quality Control (NordiQC) serve to promote test quality across laboratories.
-
Direct visualization of the stained cells and correlation with morphology.
-
Identification of the specific defective protein, thus allowing inference of the affected gene; in certain situations, this also helps the determination of the pathogenicity of MMR gene variants of uncertain significance.
-
Detection of cases that have MMR deficiency but are not MSI-H.
-
Ability to suggest the possibility of Constitutional MMR Deficiency (CMMRD) when properly processed stains fail to show unequivocal nuclear staining in both the neoplastic and non-neoplastic cells, especially in pediatric patients or young adults; these cases can be missed by MSI testing.
A further added value of routine use of MMR IHC is the continued accumulation of IHC data that can facilitate the profiling of various atypical staining patterns, leading to continued refinement of the definition of MMRd and consequently the detection of cases that would have been missed otherwise. For example, IHC MMR clonal loss (with part of the tumor still having retained MMR) has gradually been recognized as a likely form of MMRd that can be associated with germline defect when occurring in certain case scenarios (see below).
Caveats and limitations
MMR IHC is subject to all the caveats and limitations inherent to the IHC technique in general as well as those that are more specific to the testing of the MMR proteins specifically15,16,17,18,19,20,21,22.
-
Pre-analytic (e.g., tissue ischemia, fixation, decalcification, age of the blocks) and analytic factors (e.g., tissue or staining artifacts like tissue tearing or folding, fixation gradients, edge effects, DAB trapping, antibody specificity, etc.) can affect IHC performance. Thus, stringent IHC quality assurance and control procedures are paramount, and lab participation in proficiency testing (as offered by CAP and other organizations such as NordiQC) is necessary.
-
Poor fixation in particular can result in reduced staining intensity to various degrees and could lead to an erroneous interpretation of MMR protein loss.
-
The type of fixative warrants attention. In general, MMR IHC does not work well with non-formalin-based fixatives.
-
The performance of various antibody clones and associated detection systems may vary (commonly used MMR antibody clones are listed in Supplementary Table 1).
-
MLH1 IHC alone can miss some MLH1 deficient cases, possibly related to MLH1 missense or in-frame indel variants (that can produce a functionally inactive but antigenically intact mutant protein causing false normal staining on IHC) or technical issues (including poor sensitivity of the MLH1 IHC antibody)15,16,17,18,19. Adding PMS2 IHC increases the sensitivity in detecting these cases23.
-
While a two-antibody approach (PMS2 + MSH6), first proposed in 200920, detects almost all MMRd cases that are detectable by the full four-antibody panel, it can still miss cases. Thus, the most optimal approach calls for the use of all four MMR antibodies.
-
IHC staining patterns and staining intensity can have both inter- and intra-tumor variability15,21,22, making concrete scoring recommendations or guidelines difficult and causing interpretation inconsistency among observers.
-
The current IHC protocols, mostly optimized according to colorectal samples (which is highly proliferative and therefore has high expression of MMR proteins), may not be optimal for non-colorectal tissues that are less proliferative and possess lower expression of MMR proteins.
-
IHC staining, particularly the staining for MSH6, can be significantly reduced or abolished altogether in carcinomas that have been subjected to chemo-radiation therapy via as-yet undefined mechanisms but typically not related to germline or somatic MMR gene alteration or MSI-H, making post-treatment specimens unreliable for interpretation24,25.
-
IHC can miss cases in which the MMR deficiency is due to inactivation of genes other than the four tested.
Additional comments on pattern and intensity of MMR IHC and the changing definition of MMRd
It has long been recognized that MMR IHC staining can be “heterogeneous”. Focal and weak staining, as well as punctate nuclear staining, frequently associated with MLH1, could potentially be related to the presence of a mutant protein or the lack of specificity of the MLH1 antibody (which is developed against a full length protein), and can be remedied by adding PMS2 to the IHC panel15,23,26 (Table 1, Fig. 1).
In case 1 (A, B), a right colon adenocarcinoma, the staining for MLH1 (A) appears variable with most tumor cells having a staining intensity weaker than the internal control or no staining, whereas the staining for PMS2 (B) is lost. In this scenario, the loss of PMS2 serves as a surrogate marker for MLH1 abnormality. This patient was indeed found to carry a deleterious germline MLH1 mutation. In case 2 (C, D), another colonic adenocarcinoma, the variable staining of MLH1 (C) is accompanied by normal staining of PMS2 (D) as well as normal staining of MSH2 and MSH6 (not shown). The normal PMS2 staining suggests that the variable MLH1 staining is likely due to technical or other clinically inconsequential etiologies. This tumor was microsatellite stable.
Another source of “heterogeneity” is poor tissue fixation or poor performance of the staining procedure in regions of the tumor or parts of the section, and this can be remedied by vigilance in detecting the presence or absence of acceptable internal positive control (staining in lymphocytes, stromal cells, and normal epithelium in the vicinity of the tumor). Internal positive controls are mandatory for interpretation of results. Regions of poor tumor cell staining without acceptable internal positive control should be regarded as not interpretable.
Edge effect may also give rise to observed “heterogeneity”. This typically affects biopsy samples and the MSH6 stain27, with some nuclei staining towards the periphery while the remaining tumor shows loss of staining. Often these tumors have a true MSH6 protein abnormality.
An as-yet under-recognized issue related to staining heterogeneity pertains to regional loss of tumor cell staining in a properly stained section with consistent internal positive control18,19. In this review, we regard distinct regional loss of staining as “clonal loss”. The extent of the “clone” with loss of staining could range from minimal to almost the entire tumor (on individual sections, it could be 1% to 100%).
Traditionally, the definition of MMRd is “no staining in the tumor anywhere” (i.e., “all absent = abnormal”), and as such, tumors with clonal loss have been regarded as MMRp because parts of the tumor still have retained staining with an intensity stronger than the surrounding stroma. This is in fact still the definition currently recommended by the College of American Pathologists28. It is indicated that any positive reaction in the nuclei of tumor cells is considered as intact expression (normal), and it is common for intact staining to be somewhat patchy. The VENTANA MMR RxDx Panel (Roche Diagnostics, Rotkreuz, Switzerland) that was recently approved by the U.S. Food and Drug Administration (FDA) as a companion diagnostic to identify MMRd solid tumor patients eligible for anti-PD1 immunotherapy took this approach as well29,30. Its scoring algorithm indicates “focal weak equivocal nuclear staining in the viable tumor cells in the presence of internal positive controls should be given a Clinical Status of Loss. On the other hand, focal strong unequivocal nuclear staining in the viable tumor cells in the presence of internal positive controls should be given a Clinical Status of Intact.”
However, emerging literature18,19,31,32,33,34 and personal experience have indicated that in some cases with focal staining, the area of staining loss represents distinct clonal loss (Figs. 2 and 3), and such clonal loss is frequently associated with MMR gene alterations as can be seen in the following scenarios:
-
Clonal MLH1 promoter methylation. This results in clonal loss of MLH1 and PMS2 on IHC.
-
Clonal somatic mutation in one or more MMR genes in a tumor that is already MMRd/MSI-H. Most major MMR genes harbor coding microsatellites. Thus, in MLH1 and/or PMS2 deficient tumors, secondary mutation in the MSH6 coding microsatellites can lead to the emergence of a tumor clone that has loss of MSH6, resulting in an IHC phenotype of concurrent loss of MLH1/PMS2 and MSH6 in this clone24. Sometimes, such secondary clones can overtake the entire tumor. In MSH6 deficient cancers, secondary mutation could occur in the coding microsatellites of MSH3 in a clonal fashion leading to clonal loss of MSH3; as MSH3 is the major alternative partner for MSH2, its loss (in the absence of MSH6) could lead to MSH2 proteolytic degradation and a phenotype of concurrent clonal MSH2 loss and complete MSH6 loss (in some situations, the MSH6 loss can also be “heterogenous” due to edge artifact or other reasons).
-
POLE-mutated tumors. The ultra-mutating phenotype may secondarily involve MMR genes.
-
De novo clonal somatic mutation in an MMR gene is speculated to occur as well. These cases do not have other MMR gene deficiency.
-
Germline MMR pathogenic variants. It has been suggested in the literature and we have also observed in our practice that LS cases with defined germline MMR pathogenic variants can manifest clonal loss (rather than complete loss) of the corresponding MMR protein. This is presumably a reflection of the varied carcinogenesis pathways in LS-associated tumors. The frequency of this phenomenon is still to be determined. Our experience suggests that it is more likely to involve MSH6 or PMS2.
The MSH6 immunohistochemical stain (A) shows regions with unequivocal positive labeling and juxtaposed regions with distinct staining loss. In the regions with MSH6 loss, the staining for MSH2 (B) is reduced in intensity. The reduced MSH2 staining intensity does not appear to be related to secondary loss of MSH3 as the MSH3 staining (C) is diffuse and strong. The staining for MLH1 (not shown) and PMS2 (D) is retained throughout the tumor.
In patient 1 (A–C), the clonal loss involves both MSH2 (A) and MSH6 (B), while the staining for MLH1 (not shown) and PMS2 (C) is normal. Genetic testing in this patient has not been performed. In patient 2 (D–F), the clonal loss involves both MLH1 (D) and PMS2 (E), while the staining for MSH2 (not shown) and MSH6 (F) is normal. This patient was negative for germline pathogenic mutation, the clonal MLH1/PMS2 loss is likely due to clonal MLH1 promoter methylation.
These observations have thus led investigators to propose that clonal loss also be regarded as “MMR IHC abnormal”. According to this proposal, only when nuclear staining is uniformly present in all tumor cells can we regard the stain as normal. In other words, “all present = normal” (Table 2). It has been emphasized19,35 that normal MMR IHC staining should consist of staining throughout the tumor that is clearly stronger in intensity than that of the internal control (ideally carried out on well-fixed biopsy tissue); any deviation from this potentially constitutes an abnormal pattern. This is indeed what the British Association of Gynaecological Pathologists (BAGP) recommends for endometrial carcinomas; in this recommendation, a 10% cutoff is suggested for the lower limit of the tumor proportion with loss of staining for the tumor to be categorized as MMRd18,19,36.
This approach of “all present = normal” will undoubtedly capture certain MMRd cases that could have been missed by the “all absent = abnormal” approach. Caution is needed, however, to avoid over-interpretation of MMRd when applying this approach to routine practice. One pitfall, for example, is the phenomenon of intra-tumor gland staining heterogeneity that is known to occur, particularly with MSH6 staining. The pattern of staining loss in such intra-tumor gland heterogeneity is typically indistinct, with cells losing staining intimately juxtaposed to cells with retained staining. However, the number of tumor cells without staining (or with only weak staining) may still amount to 10% or more of the tumor and would therefore fulfill the 10% cutoff. Yet these cases have not been documented to be associated with gene abnormality thus far. Some examples are illustrated in Fig. 4.
In case 1 (A, B), the region without staining is likely due to poor tissue fixation (or other technical issues) as indicated by the lack of staining not only in tumor cells but also in internal control cells. In this case, the phenomenon affected all four proteins (shown here are MSH6 in A and PMS2 in B). This tumor was microsatellite stable. In case 2 (C MLH1), scattered individual glands or stretches of cells within individual glands show lack of staining, resulting in an indistinct pattern of staining heterogeneity. It is unclear what biological implications this phenomenon carries. This particular tumor was microsatellite stable and there was no evidence of germline mutation. In case 3 (D, E), the MSH6 staining (D) appears heterogeneous, with some tumor cells showing loss of staining while other tumor cells have retained staining with good intensity, but the MSH2 staining is lost (E). The etiology of the heterogenous MSH6 staining is unclear, but the phenomenon underscores the importance of using the four-antibody panel (as opposed to the two-antibody panel) in tumor testing.
Our own experience suggests that true clonal MMR protein loss on IHC reflective of gene alteration has a distinct pattern; the MMRd regions are typically sharply demarcated from the MMRp regions (Figs. 2 and 3); the relative proportions or percentages of the two regions can vary widely across sections or cases.
The clinical implication of such genuine clonal MMRd is two-fold. From the perspective of detecting LS, it is the distinct clonal loss that cannot be explained by secondary somatic alteration (e.g., focal MLH1 methylation, or MSH6 mutation in tumors that are already MLH1/PMS2 deficient) that will warrant further genetic workup. From the perspective of predicting response to immunotherapy, the meaning of clonal loss remains to be defined. A noteworthy phenomenon is that the metastasis from these rare tumors with clonal loss of MMR could be either MMRd or MMRp (MSS), as has been documented in the literature33. When the metastasis is MMRp/MSS, it may not respond to immunotherapy.
Summary
The easy availability of MMR IHC, along with its other advantages, has allowed its widespread use among clinical laboratories. However, to ensure test accuracy, pathologists need to be aware of its various caveats and limitations. Vigilance towards the existence of varied staining patterns is of particular importance. Additionally, the definition of what constitutes abnormal protein expression is still evolving. The traditional definition considers MMRd as complete loss of staining in the tumor (all absent = abnormal), whereas more recent observations have indicated the association of clonal (i.e., partial) loss of staining with gene abnormality in some cases and suggest that only when staining is present throughout the tumor can the tumor be regarded as MMR normal (all present = normal).
Table 1 summarizes our approach in dealing with the various atypical staining patterns. With regard to the interpretation of clonal loss, while awaiting more definitive guidelines, we suggest that its presence be documented in the pathology report; a comment can be used to indicate that “this pattern is likely sporadic in nature (particularly when involving both MLH1 and PMS2) but could also be due to Lynch or related syndromes”. Caution is needed in distinguishing true clonal loss from clinically inconsequential staining variability that is typically caused by technical issues such as poor fixation. True clonal loss should have a distinct pattern, with the regions of staining loss sharply demarcated from the adjacent regions with retained staining; the presence of a consistent reliable internal positive control is mandatory.
MSI testing
MSI is defined as “a change of any length due to either insertion or deletion of repeating units, in a microsatellite within a tumor when compared to normal tissue”1. It is a molecular phenotype of MMR loss and characterizes a hypermutable state of cells. It is the hypermutability, as well as the nature of the mutations (frequently frameshift), that renders tumors with this phenotype rich in neoantigens leading to the development of a hyper-intense immune microenvironment37. The immune checkpoint inhibitors—pembrolizumab, nivolumab, and ipilimumab, all approved by the Food and Drug Administration in the treatment of MMRd or MSI-H metastatic colorectal cancer (CRC) or in patients with MMRd or MSI-H CRC who have previously received chemotherapy—achieve their therapeutic efficacy by blocking tumor specific checkpoints and enabling T cells to exert their cytotoxic effect. Detection of MSI-H status (as well as MMRd) is thus paramount in selecting patients for this treatment.
The classic MSI detection method is a PCR-MSI test using an NCI-endorsed marker panel consisting of two [A/T]n mononucleotide repeats (BAT-26 and BAT-25) and three [GT/CA]n dinucleotide repeats (D5S346, D2S123, and D17S250) commonly referred to as the Bethesda Panel1. Recent years have seen the emergence of various modified and improved MSI testing platforms with more sensitive marker amplification38,39,40,41,42 (multiplex instead of simplex, fluorescent primers instead of radio-labeled primers) and more effective read-out strategies43,44 (capillary electrophoresis or other methods such as denaturing high performance liquid chromatography and high resolution melting analysis instead of gel electrophoresis). The marker panels have also been improved45,46, incorporating more mononucleotide markers at the growing appreciation that such markers are quasi-monomorphic (nearly all individuals have the same number of repeats at these loci) and sensitive in detecting MSI47. Some examples of such improved MSI platforms are the Pentaplex MSI-PCR (Fig. 5), MSI-PCR incorporating long mononucleotide repeats48, HSP110 (T17) PCR49, and the IdyllaTM MSI Assay (Table 3, Supplementary Table 2). The Idylla assay is fully-automated with fast turnaround time and no need for matched normal tissue50,51. At the current time, the pentaplex PCR-based methods are the standard test for detecting MSI, and are recommended by major organizations such as the European Society for Medical Oncology (ESMO) as the preferred MSI testing modality in the context of immunotherapy52,53.
Top panel: tumor tissue; bottom panel: matched normal tissue. The shifted alleles are indicated by arrows. Green: electropherogram showing the peaks of 2’,7’-dimethoxy-4,5-dichloro-6-carboxyfluorescein (JOE)-labeled loci, NR-21, BAT-25, and MONO-27. Blue: electropherogram showing peaks of the fluorescein-labeled loci, BAT-26 and Penta D. Black: electropherogram showing the peaks of tetramethyl rhodamine (TMR)-labeled loci, NR-24 and Penta C.
NGS-based MSI-detection is another testing modality that has emerged in recent years and infer the status of tumor microsatellites from tumor or tumor/normal genome sequencing data. By utilizing computational software tools, these methodologies allow automatic detection of somatic microsatellite changes. MSIsensor, for example, is a program first proposed by Niu et al.54 that assesses the number and length of homopolymers/microsatellites within the targeted regions of tumor-normal sample pairs. Other programs that similarly perform tumor-normal comparisons of repeat length distribution of microsatellites include MSIseq55, MOSAIC56, MANTIS57 (5), a model by Cortes-Ciriano et al.58, MSIsensor-ct59, and MiMSI60. As paired tumor-normal sequencing may not be feasible for a lot of academic institutions and commercial labs, researchers have developed MSI prediction tools that do not rely on paired tumor-normal data, such as mSINGS61, MIRMMR62, MSI-pred63, MSI-ColonCore64, MIAmS65, a model by Pang et al.66 and MSIsensor-pro67. A detailed summary of these NGS-based MSI detection methods is presented in Table 4.
These programs can then be incorporated into the clinical NGS platforms and, at some institutions, serve as an alternative test modality for MSI in solid tumors. MSK MSIsensor for example applies the MSIsensor program54 to all available genomic microsatellites covered by MSK-IMPACT (a custom targeted sequencing platform in clinical use at Memorial Sloan Kettering Cancer Center) within tumor samples against the matched normal DNA. The result is a continuous rather than categorical MSI score assignment for the tumor sample. Loci are considered unstable if k-mer distributions are significantly different between the tumor and matched normal using a standard multiple testing correction of χ2 p-values. The percentage fraction of unstable sites is reported as the MSIsensor score and based on validation data, the assay uses a MSIsensor score threshold of 10 or greater to define MSI-H68.
Advantages
A common advantage of all MSI testing modalities is their ability to detect the functional status of the MMR system. They inform whether the system is dysfunctional and are not limited to protein expression. Cases in which the MMR deficiency is due to inactivation of genes other than the four major ones tested by MMR IHC can be picked up by these modalities.
For PCR-based MSI testing, a few salient features are generally accepted as advantageous. They include:
-
Fast turnaround time. Some newer platforms now have a turnaround time comparable to MMR IHC.
-
Decreasing cost. The cost of some platforms is now comparable to MMR IHC.
-
Ability to detect MSI-H and separate that from MSI-L and MSS.
-
Amenability to external proficiency testing.
-
In general high reproducibility.
For NGS-based MSI detection programs, commonly accepted advantages include:
-
Multi-functionality. It allows simultaneous detection of tumor mutation burden (TMB), and additional gene alterations that may be clinically actionable. The detection of somatic alterations in the MMR genes and/or in BRAF can inform LS diagnostics in certain scenarios.
-
“Quantification” of the degree of MSI. The MSIsensor via MSK-IMPACT16, for example, calculates a numeric score (>10 = MSI-H, 3–10 = MSI-I, < 3 = MSS). Although not backed by direct data, some cases in the MSI-I category may overlap with MSI-L by PCR methods. This carries implications in clinical application (see below).
-
Amenability to enlarged microsatellite panels including microsatellites other than mononucleotide repeats that may help discover novel DNA repair mechanism failures beyond the current understanding of MMR loss.
-
As NGS-based mutational testing has become a standard clinical practice for cancer patient management, especially for late-stage cancers where standard therapeutic approaches are not available, determining MSI status using the methods in Table 4 does not increase the wet-lab cost and MSI detection can be easily implemented in the routine bioinformatics pipeline. Therefore, detection and reporting MSI status by NGS testing can provide guidance on immunotherapy and identify potential LS patients.
Caveats and limitations
Both the PCR-based and the NGS-based MSI detection methods have issues that warrant attention.
-
One size may not fit all. Currently, all tumor types are subject to the same marker panel and cutoff values for any given MSI testing platform, typically calibrated according to CRC samples. This may not be the most optimal because differences exist in the degree of MSI between CRC and other tumor types. This may have resulted in the low sensitivity in detecting MSI in non-colorectal neoplasms by some or all MSI testing platforms.
-
Related to the above, the specific MSI profiles may also differ across tumor types. Endometrial cancers, for example, harbor smaller size deletions or insertions in microsatellite regions than CRC69. This results in a smaller number of additional peaks on post-PCR fragment length analysis, or subtle alternations on the integrative genomics viewer. These minimal shifts, therefore, call for extra vigilance in the interpretation of these results12.
-
MSI detection assays in general require a minimum of 20% tumor content; non-colorectal samples may require even higher tumor cellularity12.
-
Some assays require matched normal DNA.
-
MSI detection assays do not have tissue correlation. In cases with clonal MMR loss, the MSI results may be equivocal depending on the relative proportion of the MMRd and MMRp components captured in the sample being tested.
-
MSI detection cannot imply the defective MMR gene.
-
The multitude of assay platforms, while serving to foster continued improvement of test accuracy, can cause difficulties in standardization and cross-sectional comparison.
-
All tests require well-established molecular facility and expertise, including sophisticated bioinformatics protocols in the case of NGS-based assays. The NGS platform also has a slow turnaround time.
Summary
MSI testing allows the detection of the functionality of the MMR system, and can identify functional deficiencies beyond the presence or absence of the four major MMR proteins. However, limitations exist. As MSI-H/MMRd has become a tissue-agnostic indication for immunotherapy, MSI testing is expanding increasingly beyond its traditional use in CRC. In this context, one current issue that particularly deserves attention is the presence of MSI heterogeneity across tumor types. This heterogeneity can manifest in the degree and/or the specific profiles of MSI. Many of the existing test platforms are developed and validated primarily for CRC. Simple adoption of these tests to other tumor types may result in under-detection of certain unique forms of MMR abnormality in unique tumor types.
Should it be MMR IHC, MSI testing, or both?
Comparisons of MMR IHC vs. MSI testing
In detecting MMR loss in solid tumors, be it for LS screening or immunotherapy eligibility, a persistent question is what constitutes the best testing strategy.
Numerous studies in the literature have compared the concordance between MMR IHC and MSI testing, but many of these studies have limitations. Common issues are inconsistent test methodologies, small case numbers including a lack of large population-based cases with known germline or other molecular data for the evaluation of true test specificity, and significantly, over-representation of CRC (often enriched for typical LS tumors or MLH1-methylated cases) in analyses that aim to address MSI pan-cancer. Nonetheless, the available data do suggest a high sensitivity and specificity for both test modalities in detecting MMR loss (the sensitivity in predicting LS is estimated at 94% and 85% for MMR IHC and PCR-MSI, respectively, with the specificity at >90% for both)15,70,71,72, and a high concordance rate between the two tests, at about 95%73. At the same time, discordances occur, and each of the two test modalities will miss a small but not insignificant number of cases (estimated to be 5–10%)16,36,73.
Two major discordant patterns are (1) MMRp/MSI-H, and (2) MMRd/non-MSI-H.
MMRp/MSI-H is commonly a result of “false normal IHC” due to misinterpretation or biological factors such as germline and/or somatic mutations in MMR genes that lead to loss of MMR function but do not affect the antigenicity of the protein, or MMR loss caused by genes other than the four tested by IHC.
MMRd/non-MSI-H could also be related to technical or interpretational issues, i.e., false IHC or MSI test results. However, a biological etiology also exists74,75,76,77.
It has long been recognized that certain non-colorectal/non-endometrial LS-associated tumors (typically less proliferative tumors) may be MMRd—losing the syndrome-defining MMR protein on IHC, but not always exhibiting detectable MSI-H76. A recent analysis of 15,045 tumor samples encompassing >50 tumor types77 showed that about 30% of the non-colorectal and non-endometrial LS-associated tumors do not have MSI-H (by the MSK-IMPACT MSIsensor program68), instead they have “MSI-I” (MSK-IMPACT MSIsensor score in the range of 3–10). In fact, in this study, up to 29% of the LS-associated endometrial cancers also had only MSI-I. In contrast, of all the LS-associated CRCs tested, 96% were MSI-H and only 4% were MSI-I. By IHC, all of the tested MSI-I LS-associated tumors, including non-canonical tumors, exhibited loss of MMR protein, indicating that these tumors are indeed MMRd. These MMRd/non-MSI-H tumors have two important clinical implications.
First, for the purpose of LS detection, tumors found to exhibit MSI-I may warrant further IHC testing irrespective of tumor type, and if IHC shows MMRd, the patient should undergo LS germline testing despite the non-MSI-H result.
Second, for the purpose of predicting response to immunotherapy with checkpoint inhibitors, the implication of MSI-I (or MSI-L) is still to be defined. Literature data exist78 that the lower degree of MSI in MSI-I tumors (typically accompanied by a lower TMB) may not be sufficient to render the tumor responsive to anti-PD1 treatment, even though the tumor is MMRd by IHC; only fully developed MSI-H (with accompanying high TMB) may confer tumor sensitivity to such treatment. Currently, the regulatory approvals for use of anti-PD1 therapy in advanced solid tumors apply to tumors that are either MSI-H or MMRd53; the inclusion of these MMRd/non-MSI-H tumors could therefore account for the lack of response in some patients. This calls for further investigation and clarification.
Recommendations
At present, the National Comprehensive Cancer Network (NCCN) recommends screening for MMR status either by IHC or by MSI-PCR79,80, whereas the ESMO consensus recommendation (in the context of immunotherapy)52 calls for MMR IHC to be the first-line test and molecular testing be performed when IHC is doubtful.
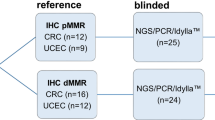
Given the intricacies related to MMR IHC versus MSI testing and the clinical implications of the different patterns of results, we regard both test modalities as essential, and think both should be maintained in the clinical and molecular diagnostic laboratories (hospital-based or reference laboratories). When dealing with patients who are at high risk for LS, both tests may be necessary (i.e., if one test shows normal results, the other should also be performed). In most other scenarios, the two tests can be used sequentially as recommended by ESMO (Fig. 6). MMR IHC has sufficient advantages to be used as the first-line method, and MSI testing can follow if the IHC is inconclusive or if the IHC is normal but there is clinical or pathological concern (e.g., positive family history concerning for Lynch syndrome, or tumor morphology suggestive of MMRd/MSI-H). However, the decision about first-line test also hinges on local resources and expertise. In places where MSI testing is well-established, MSI should yield similar efficacy as IHC as the front-line test. Additionally, at institutions where validated NGS platforms are in use, NGS-based MSI testing could be the primary modality for cases where there is no clinical urgency for MMR results at the time of diagnosis (e.g., not needed to inform the immediate next-step treatment); this is particularly applicable to tumor types with low frequency of MMR abnormality and are therefore not otherwise routinely tested for MMR.
Concluding remarks
The important clinical value of detecting the status of MMR in solid tumors is widely recognized. The current IHC and MSI testing methodologies have served to accurately detect this status in the vast majority of the cases. However, much remains to be improved. It is imperative that pathologists, and clinicians and investigators alike, keep abreast of the most up-to-date understanding of these tests and the caveats and limitations they bear. A recent report of an almost 10% false positive MMRd or MSI-H rate by local laboratories in metastatic colorectal cancer patients enrolled in immunotherapy trials81 serves to further enforce this need. In these trials, the false results were associated with therapy failure.
Towards achieving the most accurate MMR IHC interpretation, some key points worthy of attention are as follows:
-
A reliable internal positive control is mandatory for result interpretation.
-
Consistent weak staining in the tumor cells, at an intensity lower than that of the surrounding stroma, should prompt additional testing (MSI or genetic testing). This is particularly true with MSH2, MSH6, and PMS2 IHC (Table 1).
-
The old concept of “all absent = abnormal” is being challenged. Partial or clonal loss (especially when occurring in a distinct pattern) often also reflects gene abnormality.
-
While awaiting standard guidelines, we suggest documentation of distinct clonal loss in routine pathology reports.
MSI testing, PCR- or NGS-based, is being continuously refined. Established methods have predominantly focused on and been optimized for CRC; constructing MSI markers or sequence panels that are tumor type-specific is challenging but warranted.
The best strategy in the utilization of MMR IHC vs. MSI testing will depend, in large part, on local resources and expertise. In general, the two test modalities should be regarded as complementary.
Particular attention is warranted towards the tumor variant that harbors MMRd but not MSI-H by current methodologies. These cases should be followed up with further workup to assess the possibility of LS if clinically indicated. Whether and how these MMRd/non-MSI-H tumors respond to immunotherapy remains to be clarified.
References
Boland CR, Thibodeau SN, Hamilton SR, Sidransky D, Eshleman JR, Burt RW et al. A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res 58, 5248–5257 (1998).
Markowitz S, Wang J, Myeroff L, Parsons R, Sun L, Lutterbaugh J et al. Inactivation of the type II TGF-beta receptor in colon cancer cells with microsatellite instability. Science 268, 1336–1338 (1995).
Abe T, Ouyang H, Migita T, Kato Y, Kimura M, Shiiba K et al. The somatic mutation frequency of the transforming growth factor beta receptor type II gene varies widely among different cancers with microsatellite instability. Eur J Surg Oncol 22, 474–477 (1996).
Srinivasan P, Bandlamudi C, Jonsson P, Kemel Y, Chavan SS, Richards AL et al. The context-specific role of germline pathogenicity in tumorigenesis. Nat Genet 53, 1577–1585 (2021).
Umar A, Boland CR, Terdiman JP, Syngal S, de la Chapelle A, Ruschoff J et al. Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst 96, 261–268 (2004).
Saeterdal I, Gjertsen MK, Straten P, Eriksen JA & Gaudernack G. A TGF betaRII frameshift-mutation-derived CTL epitope recognised by HLA-A2-restricted CD8+ T cells. Cancer Immunol Immunother 50, 469–476 (2001).
Jardim DL, Goodman A, de Melo Gagliato D & Kurzrock R. The challenges of tumor mutational burden as an immunotherapy biomarker. Cancer Cell 39, 154–173 (2021).
Bruegl AS, Ring KL, Daniels M, Fellman BM, Urbauer DL & Broaddus RR. Clinical challenges associated with universal screening for Lynch syndrome-associated endometrial cancer. Cancer Prev Res (Phila) 10, 108–115 (2017).
Dedeurwaerdere F, Claes KB, Van Dorpe J, Rottiers I, Van der Meulen J, Breyne J et al. Comparison of microsatellite instability detection by immunohistochemistry and molecular techniques in colorectal and endometrial cancer. Sci Rep 11, 12880 (2021).
Bartley AN, Luthra R, Saraiya DS, Urbauer DL & Broaddus RR. Identification of cancer patients with Lynch syndrome: clinically significant discordances and problems in tissue-based mismatch repair testing. Cancer Prev Res (Phila) 5, 320–327 (2012).
Leenen CH, van Lier MG, van Doorn HC, van Leerdam ME, Kooi SG, de Waard J et al. Prospective evaluation of molecular screening for Lynch syndrome in patients with endometrial cancer ≤ 70 years. Gynecol Oncol 125, 414–420 (2012).
Siemanowski J, Schomig-Markiefka B, Buhl T, Haak A, Siebolts U, Dietmaier W et al. Managing difficulties of microsatellite instability testing in endometrial cancer-limitations and advantages of four different PCR-based approaches. Cancers (Basel) 13, 1268 (2021).
Velasco A, Tokat F, Bonde J, Trim N, Bauer E, Meeney A et al. Multi-center real-world comparison of the fully automated Idylla microsatellite instability assay with routine molecular methods and immunohistochemistry on formalin-fixed paraffin-embedded tissue of colorectal cancer. Virchows Arch 478, 851–863 (2021).
Yamamoto H & Imai K. An updated review of microsatellite instability in the era of next-generation sequencing and precision medicine. Semin Oncol 46, 261–270 (2019).
Shia J. Immunohistochemistry versus microsatellite instability testing for screening colorectal cancer patients at risk for hereditary nonpolyposis colorectal cancer syndrome. Part I. The utility of immunohistochemistry. J Mol Diagn 10, 293–300 (2008).
Hechtman JF, Rana S, Middha S, Stadler ZK, Latham A, Benayed R et al. Retained mismatch repair protein expression occurs in approximately 6% of microsatellite instability-high cancers and is associated with missense mutations in mismatch repair genes. Mod Pathol 33, 871–879 (2020).
Shia J. The diversity of tumours with microsatellite instability: molecular mechanisms and impact upon microsatellite instability testing and mismatch repair protein immunohistochemistry. Histopathology 78, 485–497 (2021).
Singh N, Wong R, Tchrakian N, Allen S, Clarke B, Gilks CB. Interpretation and reporting terminology for mismatch repair protein immunohistochemistry in endometrial cancer, [Internet]. The British Association of Gynaecological Pathologists, 2020. Available from https://www.thebagp.org/resources/
Singh N, Wong R, Tchrakian N, Allen SG, Clarke B & Gilks CB. Interpretation of mismatch repair protein expression using obsolete criteria results in discrepancies with microsatellite instability and mutational testing results. Comment on Hechtman et al. Mod Pathol 2020; 33:871–879. Mod Pathol 34, 1031–1032 (2021).
Shia J, Tang LH, Vakiani E, Guillem JG, Stadler ZK, Soslow RA et al. Immunohistochemistry as first-line screening for detecting colorectal cancer patients at risk for hereditary nonpolyposis colorectal cancer syndrome: a 2-antibody panel may be as predictive as a 4-antibody panel. Am J Surg Pathol 33, 1639–1645 (2009).
Dong L, Zou S, Jin X, Lu H, Zhang Y, Guo L et al. Cytoplasmic MSH2 related to genomic deletions in the MSH2/EPCAM genes in colorectal cancer patients with suspected Lynch syndrome. Front Oncol 11, 627460 (2021).
Sekine S, Ogawa R, Saito S, Ushiama M, Shida D, Nakajima T et al. Cytoplasmic MSH2 immunoreactivity in a patient with Lynch syndrome with an EPCAM-MSH2 fusion. Histopathology 70, 664–669 (2017).
de Jong AE, van Puijenbroek M, Hendriks Y, Tops C, Wijnen J, Ausems MG et al. Microsatellite instability, immunohistochemistry, and additional PMS2 staining in suspected hereditary nonpolyposis colorectal cancer. Clin. Cancer Res 10, 972–980 (2004).
Shia J, Zhang L, Shike M, Guo M, Stadler Z, Xiong X et al. Secondary mutation in a coding mononucleotide tract in MSH6 causes loss of immunoexpression of MSH6 in colorectal carcinomas with MLH1/PMS2 deficiency. Mod Pathol 26, 131–138 (2013).
Bao F, Panarelli NC, Rennert H, Sherr DL & Yantiss RK. Neoadjuvant therapy induces loss of MSH6 expression in colorectal carcinoma. Am J Surg Pathol 34, 1798–1804 (2010).
Chen W, Hampel H, Pearlman R, Jones D, Zhao W, Alsomali M et al. Unexpected expression of mismatch repair protein is more commonly seen with pathogenic missense than with other mutations in Lynch syndrome. Hum Pathol 103, 34–41 (2020).
Shia J, Stadler Z, Weiser MR, Rentz M, Gonen M, Tang LH et al. Immunohistochemical staining for DNA mismatch repair proteins in intestinal tract carcinoma: how reliable are biopsy samples? Am J Surg Pathol 35, 447–454 (2011).
Longacre TA, Broaddus R, Chuang LT, Cohen MB, Jarboe EA, Mutter GL et al. Template for reporting results of biomarker testing of specimens from patients with carcinoma of the endometrium. Arch Pathol Lab Med 141, 1508–1512 (2017).
Roche receives FDA approval for first companion diagnostic to identify dMMR solid tumour patients eligible for anti-PD-1 immunotherapy, [Internet]. Roche, 2021, [cited 7 May 2022]. Available from https://www.roche.com/media/releases/med-cor-2021-08-18
VENTANA MMR RxDx Panel – P210001, [Internet]. Food and Drug Administration, 2011, [cited 7 May 2022]. Available from https://www.fda.gov/medical-devices/recently-approved-devices/ventana-mmr-rxdx-panel-p210001
McCarthy AJ, Capo-Chichi JM, Spence T, Grenier S, Stockley T, Kamel-Reid S et al. Heterogenous loss of mismatch repair (MMR) protein expression: a challenge for immunohistochemical interpretation and microsatellite instability (MSI) evaluation. J Pathol Clin Res 5, 115–129 (2019).
Joost P, Veurink N, Holck S, Klarskov L, Bojesen A, Harbo M et al. Heterogenous mismatch-repair status in colorectal cancer. Diagn Pathol 9, 126 (2014).
Tachon G, Frouin E, Karayan-Tapon L, Auriault ML, Godet J, Moulin V et al. Heterogeneity of mismatch repair defect in colorectal cancer and its implications in clinical practice. Eur J Cancer 95, 112–116 (2018).
Sari A, Pollett A, Eiriksson LR, Lumsden-Johanson B, Van de Laar E, Kazerouni H et al. Interobserver agreement for mismatch repair protein immunohistochemistry in endometrial and nonserous, nonmucinous ovarian carcinomas. Am J Surg Pathol 43, 591–600 (2019).
Casey L & Singh N. POLE, MMR, and MSI testing in endometrial cancer: proceedings of the ISGyP Companion Society Session at the USCAP 2020 Annual Meeting. Int J Gynecol Pathol 40, 5–16 (2021).
Stelloo E, Jansen AML, Osse EM, Nout RA, Creutzberg CL, Ruano D et al. Practical guidance for mismatch repair-deficiency testing in endometrial cancer. Ann Oncol 28, 96–102 (2017).
Bai Z, Zhou Y, Ye Z, Xiong J, Lan H & Wang F. Tumor-infiltrating lymphocytes in colorectal cancer: the fundamental indication and application on immunotherapy. Front Immunol 12, 808964 (2021).
How-Kit A, Daunay A, Buhard O, Meiller C, Sahbatou M, Collura A et al. Major improvement in the detection of microsatellite instability in colorectal cancer using HSP110 T17 E-ice-COLD-PCR. Hum Mutat 39, 441–453 (2018).
Ladas I, Yu F, Leong KW, Fitarelli-Kiehl M, Song C, Ashtaputre R et al. Enhanced detection of microsatellite instability using pre-PCR elimination of wild-type DNA homo-polymers in tissue and liquid biopsies. Nucleic Acids Res 46, e74 (2018).
Baudrin LG, Duval A, Daunay A, Buhard O, Bui H, Deleuze JF et al. Improved microsatellite instability detection and identification by nuclease-assisted microsatellite instability enrichment using HSP110 T17. Clin Chem 64, 1252–1253 (2018).
Gilson P, Levy J, Rouyer M, Demange J, Husson M, Bonnet C et al. Evaluation of 3 molecular-based assays for microsatellite instability detection in formalin-fixed tissues of patients with endometrial and colorectal cancers. Sci Rep 10, 16386 (2020).
Silveira AB, Bidard FC, Kasperek A, Melaabi S, Tanguy ML, Rodrigues M et al. High-accuracy determination of microsatellite instability compatible with liquid biopsies. Clin Chem 66, 606–613 (2020).
Pan KF, Liu W, Lu YY, Zhang L, Li ZP, Lu WL et al. High throughput detection of microsatellite instability by denaturing high-performance liquid chromatography. Hum Mutat 22, 388–394 (2003).
Janavicius R, Matiukaite D, Jakubauskas A & Griskevicius L. Microsatellite instability detection by high-resolution melting analysis. Clin Chem 56, 1750–1757 (2010).
Bacher JW, Sievers CK, Albrecht DM, Grimes IC, Weiss JM, Matkowskyj KA et al. Improved detection of microsatellite instability in early colorectal lesions. PLoS One 10, e0132727 (2015).
Wu S, Liu X, Wang J, Zhou W, Guan M, Liu Y et al. DNA mismatch repair deficiency detection in colorectal cancer by a new microsatellite instability analysis system. Interdiscip Sci 12, 145–154 (2020).
Pecriaux A, Favre L, Calderaro J, Charpy C, Derman J & Pujals A. Detection of microsatellite instability in a panel of solid tumours with the Idylla MSI Test using extracted DNA. J Clin Pathol 74, 36–42 (2021).
Lin JH, Chen S, Pallavajjala A, Guedes LB, Lotan TL, Bacher JW et al. Validation of long mononucleotide repeat markers for detection of microsatellite instability. J Mol Diagn 24, 144–157 (2022).
Buhard O, Lagrange A, Guilloux A, Colas C, Chouchene M, Wanherdrick K et al. HSP110 T17 simplifies and improves the microsatellite instability testing in patients with colorectal cancer. J Med Genet 53, 377–384 (2016).
Gilson P, Merlin JL & Harle A. Detection of microsatellite instability: state of the art and future applications in circulating tumour DNA (ctDNA). Cancers (Basel) 13, 1491 (2021).
Zwaenepoel K, Holmgaard Duelund J, De Winne K, Maes V, Weyn C, Lambin S et al. Clinical performance of the Idylla MSI test for a rapid assessment of the DNA microsatellite status in human colorectal cancer. J Mol Diagn 22, 386–395 (2020).
Luchini C, Bibeau F, Ligtenberg MJL, Singh N, Nottegar A, Bosse T et al. ESMO recommendations on microsatellite instability testing for immunotherapy in cancer, and its relationship with PD-1/PD-L1 expression and tumour mutational burden: a systematic review-based approach. Ann Oncol 30, 1232–1243 (2019).
Yoshino T, Pentheroudakis G, Mishima S, Overman MJ, Yeh KH, Baba E et al. JSCO-ESMO-ASCO-JSMO-TOS: international expert consensus recommendations for tumour-agnostic treatments in patients with solid tumours with microsatellite instability or NTRK fusions. Ann Oncol 31, 861–872 (2020).
Niu B, Ye K, Zhang Q, Lu C, Xie M, McLellan MD et al. MSIsensor: microsatellite instability detection using paired tumor-normal sequence data. Bioinformatics 30, 1015–1016 (2014).
Huang MN, McPherson JR, Cutcutache I, Teh BT, Tan P & Rozen SG. MSIseq: software for assessing microsatellite instability from catalogs of somatic mutations. Sci Rep 5, 13321 (2015).
Hause RJ, Pritchard CC, Shendure J & Salipante SJ. Classification and characterization of microsatellite instability across 18 cancer types. Nat Med 22, 1342–1350 (2016).
Kautto EA, Bonneville R, Miya J, Yu L, Krook MA, Reeser JW et al. Performance evaluation for rapid detection of pan-cancer microsatellite instability with MANTIS. Oncotarget 8, 7452–7463 (2017).
Cortes-Ciriano I, Lee S, Park WY, Kim TM & Park PJ. A molecular portrait of microsatellite instability across multiple cancers. Nat Commun 8, 15180 (2017).
Han X, Zhang S, Zhou DC, Wang D, He X, Yuan D et al. MSIsensor-ct: microsatellite instability detection using cfDNA sequencing data. Brief Bioinform 22, bbaa402 (2021).
Ziegler J, Hechtman JF, Ptashkin R, Jayakumaran G, Middha S, Chavan SS et al. MiMSI - a deep multiple instance learning framework improves microsatellite instability detection from tumor next-generation sequencing. bioRxiv (2022). https://doi.org/10.1101/2020.09.16.299925
Salipante SJ, Scroggins SM, Hampel HL, Turner EH & Pritchard CC. Microsatellite instability detection by next generation sequencing. Clin Chem 60, 1192–1199 (2014).
Foltz SM, Liang WW, Xie M & Ding L. MIRMMR: binary classification of microsatellite instability using methylation and mutations. Bioinformatics 33, 3799–3801 (2017).
Wang C & Liang C. MSIpred: a python package for tumor microsatellite instability classification from tumor mutation annotation data using a support vector machine. Sci Rep 8, 17546 (2018).
Zhu L, Huang Y, Fang X, Liu C, Deng W, Zhong C et al. A novel and reliable method to detect microsatellite instability in colorectal cancer by next-generation sequencing. J Mol Diagn 20, 225–231 (2018).
Escudie F, Van Goethem C, Grand D, Vendrell J, Vigier A, Brousset P et al. MIAmS: microsatellite instability detection on NGS amplicons data. Bioinformatics 36, 1915–1916 (2019).
Pang J, Gindin T, Mansukhani M, Fernandes H & Hsiao S. Microsatellite instability detection using a large next-generation sequencing cancer panel across diverse tumour types. J Clin Pathol 73, 83–89 (2020).
Jia P, Yang X, Guo L, Liu B, Lin J, Liang H et al. MSIsensor-pro: fast, accurate, and matched-normal-sample-free detection of microsatellite instability. Genomics Proteomics Bioinformatics 18, 65–71 (2020).
Middha S, Zhang L, Nafa K, Jayakumaran G, Wong D, Kim HR et al. Reliable pan-cancer microsatellite instability assessment by using targeted next-generation sequencing data. JCO Precis Oncol 1, PO.17.00084 (2017).
Kuismanen SA, Moisio AL, Schweizer P, Truninger K, Salovaara R, Arola J et al. Endometrial and colorectal tumors from patients with hereditary nonpolyposis colon cancer display different patterns of microsatellite instability. Am J Pathol 160, 1953–1958 (2002).
Xicola RM, Llor X, Pons E, Castells A, Alenda C, Pinol V et al. Performance of different microsatellite marker panels for detection of mismatch repair-deficient colorectal tumors. J Natl Cancer Inst 99, 244–252 (2007).
Palomaki GE, McClain MR, Melillo S, Hampel HL & Thibodeau SN. EGAPP supplementary evidence review: DNA testing strategies aimed at reducing morbidity and mortality from Lynch syndrome. Genet Med 11, 42–65 (2009).
Baudrin LG, Deleuze JF & How-Kit A. Molecular and computational methods for the detection of microsatellite instability in cancer. Front Oncol 8, 621 (2018).
Evrard C, Tachon G, Randrian V, Karayan-Tapon L & Tougeron D. Microsatellite instability: diagnosis, heterogeneity, discordance, and clinical impact in colorectal cancer. Cancers (Basel) 11, 1567 (2019).
Schwartz CJ, da Silva EM, Marra A, Gazzo AM, Selenica P, Rai VK et al. Morphological and genomic characteristics of breast cancers occurring in individuals with Lynch Syndrome. Clin Cancer Res 28, 404–413 (2022).
Vyas M, Firat C, Hechtman JF, Weiser MR, Yaeger R, Vanderbilt C et al. Discordant DNA mismatch repair protein status between synchronous or metachronous gastrointestinal carcinomas: frequency, patterns, and molecular etiologies. Fam Cancer 20, 201–213 (2021).
Karamurzin Y, Zeng Z, Stadler ZK, Zhang L, Ouansafi I, Al-Ahmadie HA et al. Unusual DNA mismatch repair-deficient tumors in Lynch syndrome: a report of new cases and review of the literature. Hum Pathol 43, 1677–1687 (2012).
Latham A, Srinivasan P, Kemel Y, Shia J, Bandlamudi C, Mandelker D et al. Microsatellite instability is associated with the presence of Lynch syndrome pan-cancer. J Clin Oncol 37, 286–295 (2019).
Mandal R, Samstein RM, Lee KW, Havel JJ, Wang H, Krishna C et al. Genetic diversity of tumors with mismatch repair deficiency influences anti-PD-1 immunotherapy response. Science 364, 485–491 (2019).
Provenzale D, Gupta S, Ahnen DJ, Bray T, Cannon JA, Cooper G et al. Genetic/familial high-risk assessment: colorectal version 1.2016, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 14, 1010–1030 (2016).
Ryan N, Wall J, Crosbie EJ, Arends M, Bosse T, Arif S et al. Lynch syndrome screening in gynaecological cancers: results of an international survey with recommendations for uniform reporting terminology for mismatch repair immunohistochemistry results. Histopathology 75, 813–824 (2019).
Cohen R, Hain E, Buhard O, Guilloux A, Bardier A, Kaci R et al. Association of primary resistance to immune checkpoint inhibitors in metastatic colorectal cancer with misdiagnosis of microsatellite instability or mismatch repair deficiency status. JAMA Oncol 5, 551–555 (2019).
Acknowledgements
We thank Dr. Cyriac Kandoth (Director, Clinical Bioinformatics, Molecular Diagnostics at UCLA) for his expert guidance on the NGS-based MSI detection methods.
Author information
Authors and Affiliations
Contributions
JS conceived the review manuscript. All authors participated in reviewing the literature and drafting the manuscript. JS and CW revised the final manuscript which was approved by all authors.
Corresponding author
Ethics declarations
Competing interests
JS discloses the following relationship: Consultant, Paige.AI, Inc. LZ discloses the following relationship: Family members hold leadership positions and ownership interests in Decipher Medicine. CW: None. EV: None.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wang, C., Zhang, L., Vakiani, E. et al. Detecting mismatch repair deficiency in solid neoplasms: immunohistochemistry, microsatellite instability, or both?. Mod Pathol 35, 1515–1528 (2022). https://doi.org/10.1038/s41379-022-01109-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-022-01109-4
This article is cited by
-
Comparison of standard mismatch repair deficiency and microsatellite instability tests in a large cancer series
Journal of Translational Medicine (2024)
-
Impact of formalin fixation on mismatch repair protein evaluation by immunohistochemistry
Virchows Archiv (2023)
-
Evaluating mismatch repair deficiency in colorectal cancer biopsy specimens
Histochemistry and Cell Biology (2023)
-
Testung auf Mismatch-Reparatur-Defizienz und Mikrosatelliteninstabilität
Die Pathologie (2023)
-
Testing for deficient mismatch repair and microsatellite instability
Die Pathologie (2023)