Abstract
The clinical and pathologic diagnosis of hypersensitivity pneumonitis has been confounded by conflicting definitions, with two recent guidelines suggesting that hypersensitivity pneumonitis simply be diagnosed as nonfibrotic or fibrotic. Nonfibrotic hypersensitivity pneumonitis is usually characterized by a bronchiolocentric chronic interstitial inflammatory infiltrate, frequently but by no means always with associated granulomas or giant cells. Fibrotic hypersensitivity pneumonitis may take the form of interstitial fibrosis confined to the peribronchiolar regions, or fibrotic nonspecific interstitial pneumonia, or a process similar to and sometimes indistinguishable from usual interstitial pneumonia/idiopathic interstitial fibrosis, but the exact pathologic features that favor a diagnosis of fibrotic hypersensitivity pneumonitis are disputed. Granulomas/giant cells are much less frequent in fibrotic compared to nonfibrotic hypersensitivity pneumonitis. Extensive peribronchiolar metaplasia, particularly peribronchiolar metaplasia affecting more than half the bronchioles, supports a diagnosis of fibrotic hypersensitivity pneumonitis over usual interstitial pneumonia, as does the presence of predominantly peribronchiolar disease with relative subpleural sparing. Clinical and CT features are crucial to the diagnosis of hypersensitivity pneumonitis: sparing of the lung bases, centrilobular nodules, air-trapping, or the triple density sign with fibrosis favor a diagnosis of fibrotic hypersensitivity pneumonitis. At this point there are no molecular tests that reliably separate fibrotic hypersensitivity pneumonitis from other forms of interstitial lung disease. Currently the separation of fibrotic hypersensitivity pneumonitis from usual interstitial pneumonia is crucial to treatment (immunosuppressives for the former, anti-fibrotics for the latter) but this approach is changing and all progressive fibrosing interstitial pneumonias will probably be treated with antifibrotics in the future.
Similar content being viewed by others
Introduction
Hypersensitivity pneumonitis (HP) has been a recognized form of interstitial lung disease (ILD) for many years. The diagnostic features of nonfibrotic HP (in the past referred to as subacute HP—see the section “Definition, Classification, and Causes of Hypersensitivity Pneumonitis,” below, for traditional and new HP classifications) have been generally well defined, but there has been poor agreement on the clinical, radiologic, and pathologic features and even nomenclature of fibrotic forms of HP, as well as the separation of fibrotic forms of HP from other ILD. In the past this separation was not crucial and fibrotic ILD tended to all be treated with immunosuppressive agents, typically steroids. But the recognition that immunosuppressive agents are contraindicated in usual interstitial pneumonia/idiopathic pulmonary fibrosis (UIP/IPF; in this paper the term UIP/IPF will be used to indicate idiopathic pulmonary fibrosis, and a UIP-like pattern to indicate other disease that can mimic UIP/IPF pathologically), and the introduction of antifibrotic therapies for UIP/IPF has mandated accurate separation of UIP/IPF from fibrotic forms of HP and other fibrosing ILDs (see section “Prognosis and Treatment”, below) [1, 2].
The magnitude of the problem is well illustrated by two studies. Walsh et al. [3] circulated 70 ILD cases to seven experienced multidisciplinary discussion (MDD) groups. For UIP/IPF and connective tissue disease-associated ILD (CTD-ILD) agreement was good across groups (weighted kappas 0.71 and 0.73, respectively), but for fibrotic HP agreement was poor (weighted kappa 0.29). Morell et al. [4] reviewed 46 cases that met the criteria for UIP/IPF according to the American Thoracic Society (ATS) 2011 diagnostic guidelines [1]; by adding more detailed exposure histories, evaluation of specific serum immunoglobulins, and/or inhalation challenge, they reclassified 20 (43%) as fibrotic HP.
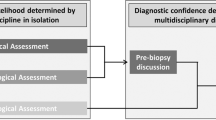
This problem applies at the level of pathology as well, with disagreements in the literature about which features do or don’t allow a diagnosis of fibrotic forms of HP, particularly features that separate fibrotic HP from UIP/IPF [5,6,7,8]. This review will cover new concepts and ongoing controversies in the diagnosis of HP with an emphasis on pathology, comment on the just-released American Thoracic Society (ATS) HP guidelines [9] and American College of Chest Physicians (ACCP) HP guidelines [10], and provide information for the pathologist on how to approach a diagnosis of HP, particularly the fibrotic forms. However, it is important to bear in mind that accurate pathologic diagnoses of HP, like any form of ILD, cannot be done in a vacuum; rather, diagnosis requires clinical and radiologic information, either in the formal setting of a multidisciplinary discussion (MDD) in which clinicians, radiologists, and pathologists all take part, or at least informally from record review/curbside consultation.
Definition, classification, and causes of hypersensitivity pneumonitis
The 2020 ATS hypersensitivity pneumonitis diagnostic guidelines [9] define HP as “an inflammatory and/or fibrotic disease affecting the lung parenchyma and small airways. It typically results from an immune-mediated reaction provoked by an overt or occult inhaled antigen in susceptible individuals.” While this definition is simple, in practice HP can be a difficult diagnosis, and how to approach the diagnosis (at a largely clinical level) is the thrust of the guidelines.
The classification of HP has a long and somewhat contentious history. Traditionally, HP was separated into acute, subacute, and chronic forms (Table 1). Under this scheme, acute HP presents as an acute self-limited febrile illness, believed to be caused by high level exposure to the sensitizing agent, whereas subacute HP is an interstitial lung disease that develops insidiously over weeks to months and is thought to reflect lower level ongoing exposure. The major problem with this scheme is the term “chronic HP,” which some authors have used for disease present over some arbitrary time period (four months, six months, and one year have all been described in the literature), while other authors have reserved “chronic HP” for disease in which there is radiologic or pathologic evidence of fibrosis (reviewed in 11).
The problem with using a time definition for chronic HP is that one ends up with a mixture of cases with and without interstitial fibrosis, and this scenario confounds making estimates of prognosis and determining treatment, because it is clear that the presence of fibrosis has an adverse prognostic effect in HP (see section “Prognosis and Treatment”, below). For this reason, the new ATS and ACCP guidelines [9, 10] recommend simply separating HP into “nonfibrotic” and “fibrotic” forms, and that is the convention followed here.
More than 50 different occupations/exposures associated with HP have been described [9, 11], etiologically related to contaminating microorganisms, animal proteins, and, less frequently, inorganic chemicals, but many of these only apply to very restricted groups of workers. In North American the common causes of HP are farming, bird/avian antigen exposures (including feather-containing bedding/clothing), household mold, micro-organism contaminated humidifiers/ventilation systems, and hot tubs/showers/saunas contaminated with atypical mycobacteria (“hot tub lung”). In Japan, where summers are hot and humid, so-called “summer-type” HP, caused by a variety of yeasts and bacteria that thrive in houses in these conditions, is common. In India, also a hot and humid climate, HP is the most frequent form of ILD and is typically related to microorganisms contaminating air coolers [12].
Identification and avoidance of the sensitizing antigen is an important part of the diagnosis and treatment of HP, but a case where the offending agent cannot be found after a thorough history, serologic investigation, and even inhalation challenge testing, becomes a major problem. This scenario occurs in a minority of nonfibrotic (subacute) HP cases, but in up to 60% of patients with fibrotic HP [9], and is one of the factors that can make the diagnosis of fibrotic forms of HP difficult. These are the cases that often come to biopsy and determination of whether a fibrotic ILD is fibrotic HP or another disease in this situation is sometimes extremely difficult.
Clinical features of HP
In large series, patients with nonfibrotic HP tend to have a relatively acute onset and more often an identifiable antigen compared to patients with fibrotic HP. Apart from a history or evidence of antigen exposure, the clinical findings of HP are fairly nonspecific and include shortness of breath, cough, and mid-expiratory squeaks. Constitutional symptoms (chills, low grade fever, malaise) are sometimes present. Pulmonary function tests typically show some degree of restriction and a decreased diffusing capacity.
Bronchoalveolar lavage cell counts can be extremely helpful in establishing a diagnosis of HP, particularly nonfibrotic HP, where a lavage lymphocyte count of >20% is thought to support the diagnosis. For fibrotic HP a lymphocyte count of 20% is suggestive of HP (sensitivity 69%, specificity 61%) and a count of 40% has a specificity of 93% (sensitivity 43%) for separating fibrotic HP from UIP/IPF [9]. However, other conditions such as sarcoid can also have relatively high lavage lymphocyte counts. A further confounding factor is that many cases of fibrotic HP do not have an elevated lymphocyte count [9]. As well, the specificity of lavage lymphocyte counts has been challenged on the grounds that the test is not standardized and different laboratories report different percentages [13].
The role of serologic testing to identify specific IgGs is also controversial, in part again because there are no standardized tests, various laboratories test for different antigens using different methods, and for many potential antigens no routinely accessible tests are available, although some specialized laboratories have generated their own antibodies [11]. It has also been observed that the presence of circulating antibodies does not always correlate with the exposure that is actually causing disease. Conversely, patients may have circulating antibodies and no disease; this is well documented for individuals who keep pet birds or breed birds [14]. The ATS and ACCP guidelines recommended serologic testing, but with very low confidence in the estimated effects.
Inhalation challenge testing is even more specialized. Munoz et al. [15] reported inhalation challenge testing in 123 patients and found a sensitivity/specificity of 73/84%, using acute pulmonary function decline as a positive result. They pointed out that a negative inhalation challenge test does not rule out HP.
Radiologic features of HP
Nonfibrotic HP typically shows a picture of ground glass opacities that may be diffuse or only present as centrilobular nodules, and evidence of air-trapping (Fig. 1A) [9, 10]. Fibrotic HP combines features of fibrosis (reticulation, traction bronchiectasis/bronchiolectasis, honeycombing) with evidence of bronchiolar obstruction (“bronchiolitis”) in the form of centrilobular nodules or mosaic attenuation or overt air-trapping on expiratory images. Ground glass opacities are common and sometimes images show a so-called “headcheese” or “triple density” pattern with areas of increased attenuation (ground glass), normal attenuation, and decreased attenuation (air-trapping) [9, 10, 16] (Fig. 1B). Ground glass opacities and air-trapping on expiratory images are particularly useful features for separating fibrotic HP from UIP/IPF. In fibrotic HP the fibrosing process may spare the most dependent lung bases or be more severe in the upper than lower lobes, findings that are distinctly against a diagnosis of UIP/IPF. However, some cases of fibrotic HP are radiologically indistinguishable from UIP/IPF.
A High resolution CT scan showing multiple centrilobular ground glass nodules and hyperlucent area representing air trapping (arrow). B High resolution CT scan showing the triple density pattern: hyperlucent areas representing air-trapping, normal lung, and ground glass opacities. There is also mild reticulation. C Low power view showing mild bronchiolocentric chronic interstitial inflammation and interstitial granulomas. This is the usual pattern of nonfibrotic HP. D Marked chronic inflammation of bronchiolar wall with granulomas representing so-called “bronchiolitis” in nonfibrotic HP. The process focally extends into the interstitium. Narrowing of the bronchiolar lumen by inflammation in the wall is the cause of air-trapping on CT imaging. E Higher power view of Fig. 3 showing details of the granuloma; one is interstitial but a second granuloma is in an airspace. Although granulomas in HP are often said to be poorly defined, in fact in many cases they are quite well defined, as here, but always lack the concentric fibrosis seen in many sarcoid granulomas.
Pathologic features of HP
Nonfibrotic HP
Most cases of nonfibrotic HP show a distinctly bronchiolocentric pattern of chronic interstitial inflammation, which fades off to normal parenchyma away from the bronchioles (Table 2, Fig. 1C and for further illustrations see [17]). The interstitial infiltrate is typically lymphocytes and may be accompanied by a few plasma cells; however, a preponderance of plasma cells is against a diagnosis of nonfibrotic HP and suggests underlying connective tissue disease (CTD-ILD). Lymphoid aggregates usually are few to nonexistent in nonfibrotic HP, and lymphoid aggregates with germinal centers are distinctly uncommon; the presence of numerous lymphoid aggregates/germinal centers again suggests underlying connective tissue disease [18].
The interstitial infiltrate can produce significant expansion of the walls of bronchioles (Fig. 1D), a process some authors refer to as “bronchiolitis.” In functional terms this idea is correct because it is the thickened bronchiolar walls/narrowed bronchiolar lumens that produce the characteristic finding of air-trapping on imaging. However, if on biopsy the infiltrate is present only in the walls of bronchioles without any inflammation in the immediately surrounding alveolar walls, the process in question is probably a true bronchiolitis and not HP.
Granulomas or individual giant cells are present in the majority of nonfibrotic HP cases. In general these structures are present in the peribronchiolar interstitium (Fig. 1E), but can sometimes be found in airspaces near bronchioles as well [19] (Fig. 1E). The granulomas/giant cells may contain cholesterol clefts or Schaumann bodies. Sometimes only naked Schaumann bodies are present; these structures are the tombstones of granulomas and provide equivalent diagnostic information. Schaumann bodies can be found in any persisting granuloma; they are rare to nonexistent in granulomatous infections, and in my experience are much more common in HP than in sarcoid.
Although the granulomas of HP (fibrotic or nonfibrotic) are often described as poorly defined, in fact the granulomas of HP are often quite well defined (Figs. 1E, 2A), but what they always lack is the pattern of fine concentric rings of fibrosis that is characteristic of sarcoid.
A A case of nonfibrotic HP with a cellular nonspecific interstitial pneumonia (NSIP) pattern in a patient with farm exposure. Inset shows a granuloma. B Fibrotic HP. Fibrotic HP with purely bronchiolocentric fibrosis. Patient exposed to metal-working fluids. C Fibrotic HP. Higher power of Fig. 2B showing giant cells with cholesterol clefts (arrows). D Fibrotic HP. Patient with pet bird exposure. Note the peribronchiolar fibrosis in the upper part of the field and the subpleural fibrosis in the lower part.
In general there are no differences in the underlying pathologic findings in cases with or without granulomas/giant cells, but there is a (poorly documented) belief that the presence of granulomas/giant cells in either nonfibrotic or fibrotic HP is a marker of ongoing antigen exposure and mandates a careful workup for the offending agent.
Occasionally the inflammatory process in nonfibrotic HP is more diffuse and is identical to cellular nonspecific interstitial pneumonia (NSIP) (Fig. 2A).
Fibrotic HP
As opposed to nonfibrotic HP, where the morphologic diagnosis is straightforward in the majority of cases, fibrotic HP is the problem child of ILD at a pathologic as well as a clinical and radiologic level. This situation arises in part from the protean pathologic findings that can be seen in fibrotic HP, in part from disagreements about the features that do or don’t define fibrotic HP, and in part from the ability of fibrotic HP to mimic other forms of fibrotic ILD and vice versa, especially UIP/IPF. A further complication is that biopsy of clinically and radiologically evident UIP/IPF cases is now not recommended [1], so that the cases that are biopsied are atypical/indeterminate, and an increasing proportion of biopsies in the setting of a fibrosing interstitial pneumonia are cases of fibrotic HP. The distinction of fibrotic HP from UIP/IPF is not just an academic exercise, because at present treatment for these conditions differs considerably (see “Prognosis and Treatment”, below).
Interstitial fibrosis in fibrotic HP may take several different forms (Tables 3, 4): bronchiolocentric (Figs. 2B, C); bronchiolocentric with subpleural fibrosis (Figs. 2D, 3A); fibrotic NSIP (Figs. 3B, C), and variably UIP-like (Fig. 3D). Granulomas/giant cells are similar to those in nonfibrotic HP (Fig. 4A), but unlike nonfibrotic HP they may be found anywhere in the parenchyma and not just in a peribronchiolar location. Granulomas/giant cells are very helpful when present; however, they are found in only a minority of fibrotic HP cases. As is true of nonfibrotic HP, Schaumann bodies are sometimes present and are substitutes for granulomas (Fig. 3A). Granulomas/giant cells may occasionally also be a feature of connective tissue disease-associated ILD [18], but are not part of UIP/IPF.
A Several Schaumann bodies with a giant cell in the same field as Fig. 2D. Schaumann bodies are, effectively, tombstones of granulomas and provide the same diagnostic information. B Patient with household mold exposure. In this case the pattern is that of fibrotic nonspecific interstitial pneumonia (NSIP). C Higher power view of figure 11 showing granulomas (arrows) which indicate that this is really fibrotic HP and not NSIP. D Patient with hot tub exposure. In this lobe the biopsy is a perfect mimic of usual interstitial pneumonia/idiopathic pulmonary fibrosis.
A Same case as Fig. 3D. In this lobe is prominent peribronchiolar fibrosis with minimal subpleural fibrosis, a pattern that is against a diagnosis of usual interstitial pneumonia/idiopathic pulmonary fibrosis (UIP/IPF). A granuloma is shown in the inset. B Low power view of the biopsy shows minimal subpleural fibrosis with fine bridging fibrosis and peribronchiolar fibrosis. C Same case as Fig. 4B. High power view of another area showing prominent peribronchiolar metaplasia. Peribronchiolar metaplasia was present around more than 50% of bronchioles, a finding that supports a diagnosis of fibrotic HP. No source of exposure could be determined. D An example of fibrotic HP in which the underlying pattern of fibrosis is that of UIP, but there is peribronchiolar metaplasia around every airway in the field (arrows), a finding that favors fibrotic HP.
Peribronchiolar metaplasia refers to fine interstitial fibrosis with overlying metaplastic bronchiolar epithelium that spreads in the peribronchiolar interstitium (Figs. 4B–D). We have shown [20] that peribronchiolar metaplasia affecting more than half of bronchioles is a generally reliable marker of fibrotic HP (Fig. 5A), and that this high fraction of bronchioles with peribronchiolar metaplasia is not seen in UIP/IPF or connective tissue disease-associated ILD [18, 20]. However, occasional foci of peribronchiolar metaplasia can be found in any fibrosing interstitial pneumonia and even in otherwise normal lung, so determination of the proportion of affected bronchioles is required to use this feature for the diagnosis of fibrotic HP.
A Relationship between percent confidence in a diagnosis of fibrotic hypersensitivity pneumonitis (HP) vs usual interstitial pneumonia/idiopathic pulmonary fibrosis (UIP/IPF) and fraction of bronchioles showing peribronchiolar metaplasia. A 50% or greater fraction of bronchioles with peribronchiolar metaplasia was only seen in cases with a 60% or greater probability of fibrotic HP as determined at a special multidisciplinary discussion (see ref [20]). Note that peribronchiolar fibrosis was present in small numbers in both the fibrotic HP cases (right side of graph) and the UIP/IPF cases (left side of graph); finding only a few foci of peribronchiolar metaplasia is not helpful diagnostically. B A case that is difficult to classify. The basic pattern is that of UIP/IPF, but large blocks of fibrosis extend around bronchioles. This pattern can be seen in both UIP/IPF and fibrotic HP. C Connective tissue disease-associated interstitial lung disease (ILD). There is peribronchiolar fibrosis with almost no subpleural fibrosis. This pattern is strongly against a diagnosis of UIP/IPF but can be seen with both fibrotic HP and connective tissue disease-associated ILD. Here the numerous lymphoid aggregates (arrows), including aggregates with germinal centers (inset) strong favor a diagnosis of connective tissue disease-associated ILD. D Sarcoid. An example of sarcoid with extensive linear scarring somewhat mimicking the peribronchiolar fibrosis of fibrotic HP. However, there are numerous well defined granulomas, some with concentric fibrosis (not visible at this magnification); fibrotic HP cases do not show these features.
The interstitial inflammatory infiltrate of fibrotic HP can be sparse as in UIP/IPF or moderately cellular, and when present is composed predominantly of lymphocytes with a variable number of plasma cells and sometimes a few eosinophils. An interstitial infiltrate that is predominantly plasma cells (plasma cell: lymphocyte ratio >1:1 measured away from lymphoid aggregates) is against a diagnosis of fibrotic HP and favors CTD-ILD [18], as does the presence of numerous lymphoid aggregates or lymphoid aggregates with germinal centers; the latter feature is distinctly against a diagnosis of fibrotic HP [18].
Fibroblast foci are frequent in fibrotic HP, either in a pattern similar to that in UIP/IPF or associated with isolated peribronchiolar fibrosis. It has been suggested that fibroblast foci associated with peribronchiolar fibrosis favor a diagnosis of fibrotic HP over UIP/IPF [21] but we could not find a distinction in a careful morphometric study of cases assigned to one diagnosis or the other at MDD [20]. What we did find was that UIP/IPF cases had statistically greater numbers of fibroblast foci/cm2 of biopsy area compared to fibrotic HP cases, but there was too much overlap in individual case values to use this measure for diagnosis.
Foci of typical nonfibrotic HP in the form of a bronchiolocentric interstitial inflammatory infiltrate with giant cells or granulomas may be found in fibrotic HP biopsies, and can be a very useful hint to the correct diagnosis in cases that otherwise resemble UIP/IPF. However, this feature is absent in most cases of fibrotic HP.
Controversial findings in fibrotic HP
Bronchiolocentric fibrosis is present in many cases of fibrotic HP and indeed is listed as a potential defining feature in the ATS and ACCP guidelines [9, 10]. However, there are differences in how different authors use this term and it also remains unclear how much, if any, bronchiolocentric fibrosis is allowed for a diagnosis of UIP/IPF. For example, Hashisako et al. [7] circulated a set of ILD images from 20 ILD cases to 11 pathologists; there was an almost even split between those who would accept peribronchiolar fibrosis as part of UIP/IPF and those who viewed peribronchiolar fibrosis as a marker of a non-UIP/IPF diagnosis.
More recently Tanizawa et al. [8] examined the presence or absence of peribronchiolar fibrosis in a series of 252 VATS biopsies that had a UIP/IPF-like pattern on biopsy. Of these 215 were considered to represent UIP/IPF after MDD and the other 37 other diagnosis including fibrotic HP. Moderate to marked amounts of peribronchiolar fibrosis were seen in 1/3 of the UIP/IPF cases and roughly 2/3 of the non-IPF cases, producing an odds ratio for a non-IPF diagnosis of 3.71. Thus this study indicates that, although peribronchiolar fibrosis can be seen in UIP/IPF, the presence of peribronchiolar fibrosis favors a non-UIP/IPF diagnosis. The illustrations from this paper suggest that the authors were evaluating peribronchiolar fibrosis that was contiguous with subpleural fibrosis, ie, coarse bridging fibrosis, see below (and similar to Fig. 5B) rather than isolated peribronchiolar fibrosis.
My own belief is that isolated peribronchiolar fibrosis (Figs. 4A, B) suggests a non-UIP/IPF diagnosis, and particularly fibrotic HP, but whether even one such focus moves a case from UIP/IPF or multiple foci are needed is not known. This issue needs further examination.
Bridging fibrosis is another controversial issue. The term refers to fibrotic bridges from the peribronchiolar region to interlobular septa or the subpleural area (Fig. 4B). UIP/IPF starts in the periphery of the lobule (subpleural and/or next to interlobular septa), but as disease advances the lobule tends to be overrun, so that it is common to find coarse bands of bridging fibrosis (for example, Fig. 2C in ref [5]). The controversy is whether fine bands of bridging fibrosis in lobules that are not overrun (such as Fig. 4B) represent fibrotic HP or are also part of UIP/IPF.
The ATS and ACCP guidelines list organizing pneumonia (BOOP, COP) as a feature of nonfibrotic and fibrotic HP. In my experience organizing pneumonia is extremely uncommon in HP, and if substantial amounts are present in fibrotic HP, the process is more likely to be a manifestation of an acute exacerbation rather than an intrinsic part of the disease.
Even ignoring these areas of controversy, there are cases of fibrotic HP that are indistinguishable from UIP/IPF or, less commonly, from fibrotic NSIP.
Role of transbronchial forceps biopsy and cryobiopsy in the diagnosis of HP
Conventional transbronchial forceps biopsy is occasionally useful in the diagnosis of nonfibrotic HP if there is a combination of interstitial chronic inflammation and giant cells/granulomas. The latter must be present because interstitial inflammation by itself is completely nonspecific in a transbronchial biopsy. The diagnosis of HP in this situation always requires compatible clinical and radiologic findings.
Transbronchial cryobiopsy offers the theoretic advantages of potentially much larger pieces of tissue and an absence of collapse artifact, since the lung is frozen in its in situ configuration by the biopsy [22]. However, cryobiopsy for the diagnosis of ILD is extremely controversial, with the only two studies that, thus far, have examined cryobiopsy and VATS biopsy in the same patients coming to diametrically opposite conclusions about whether the diagnosis from cryobiopsy correlates with the diagnosis from VATS biopsy [23, 24].
A further problem with cryobiopsy, considering how hard it is being pushed in some quarters, is an astonishing lack of published pathologic criteria. A very recent followup analysis from the COLDICE study (24, one of the investigations looking at cryobiopsy vs VATS biopsy in the same patients) suggested that patchy fibrosis and fibroblast foci could be used to define UIP/IPF in cryobiopsies [25]; the problem is that patchy fibrosis and fibroblast foci are also features of fibrotic HP and some cases of connective tissue disease-ILD as well, and I do not believe that these features will separate fibrotic HP from UIP/IPF in cryobiopsies.
There appear to be no published data on the features claimed to support a diagnosis of fibrotic HP in cryobiopsies, even though that diagnosis has been made in some of the published studies [23, 24]. To address this in part, we [26] performed an in silico study by creating multiple 20 mm2 “cryobiopies” from the slides of 15 VATS biopsy cases that had been classified as 60% or greater probability of fibrotic HP at a special MDD. Somewhat surprisingly, the sensitivity of these “cryobiopsies” for giant cells/granulomas was poor; even with 8 “cryobiopsies,” (160 mm2 total area) giant cells/granulomas were found in only 50% of the cases in which they were visible in the VATS biopsies. The ability to detect peribronchiolar metaplasia was considerably better; with 4 “cryobiopsies” (80 mm2 total tissue area) the sensitivity/specificity for finding peribronchiolar metaplasia in ≥50% of bronchioles was 86/75%. Addition of giant cells/granulomas increased these numbers to 100/80%. What these data also imply is that cryobiopsies will require sampling of both a minimal number of sites and a minimal tissue area to be useful in this context.
Until there are published data and agreement on the features that allow specific identification of fibrotic HP, pathologists should be very cautious in rendering diagnoses using cryobiopsies.
Pathologic diagnosis using the American Thoracic Society and American College of chest physicians hypersensitivity pneumonitis practice guidelines
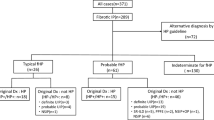
The ATS and ACCP practice guidelines [9, 10] try to standardize criteria for the diagnosis of HP at a clinical, radiologic, and pathologic level. The ATS guidelines use the categories of HP, Probable HP, and Indeterminate for HP, while the ACCP guidelines use Typical HP, Compatible with HP, Indeterminate for HP, and Alternative Diagnosis.
The pathologic criteria for the HP/definite HP category for both nonfibrotic and fibrotic HP largely match what has been set forth in this manuscript (Tables 2 and 3), but with minor differences between this paper and the guidelines and between the two sets of guidelines themselves. In both guidelines the distinction between HP/definite HP and probable HP/compatible with HP (nonfibrotic or fibrotic) is defined by the presence or absence of granulomas/giant cells (presence = definite, absence = probable/compatible), with other features the same in both categories. The reader is referred to those publications for details.
The pathology categories are set up purposely to match the radiologic categories in the same guidelines, and for radiologists the categories seem to work reasonably well. For pathologists this type of categorization is often awkward; indeed the similarly organized ATS IPF pathology guidelines [2] have been the subject of considerable criticism because they are largely unworkable (reviewed in [27, 28]). For HP, the definite HP and probable HP categories are usable, although one would have to pick one or the other or the criteria set out in this paper. The Indeterminate for HP category is functionally useless since it amounts to no more than stating that the features observed in a biopsy are those of an interstitial lung disease but not specific enough to support a diagnosis of HP nor to suggest an alternative diagnosis.
In my view the main application of both guidelines for pathologists is in highly structured multidisciplinary ILD discussions, or as part of research protocols. For everyday practice, the guidelines impose an unrealistic rigidity on diagnoses. I think it is much more useful to either make a definitive diagnosis of HP if the features are clear, or to provide a differential diagnosis such as “fibrosing interstitial pneumonia, favor fibrotic HP over UIP/IPF” than to try to squeeze cases into the guideline categories, which by definition do not allow a differential diagnosis. This approach has broader clinically applicability, since clinicians often want to know the pathologist’s view of the likely possibilities for a given biopsy, rather than just the single category diagnoses that the guidelines allow.
Differential diagnosis of nonfibrotic HP
The major differential diagnoses of nonfibrotic HP are sarcoid, microaspiration, and primary bronchiolitis. The distinction from sarcoid is generally straightforward: in sarcoid granulomas are numerous and are the predominant feature, and there is no interstitial inflammation. Sarcoid granulomas show a lymphangitic distribution (along the bronchovascular bundles, interlobular septa, and pleura) and often have fine rims of concentric fibrosis (for illustrations see ref. [29]).
Microaspiration can produce a granulomatous bronchiolitis. Hints to the correct diagnosis are the presence of foreign material in the bronchiolar walls or lumens that is often digested PAS or polarization positive, and foreign body type giant cells. In general microaspiration does not produce the characteristic peribronchiolar interstitial inflammation of nonfibrotic HP but some cases do show this feature; however, foreign material in the airspaces distal to or around the bronchioles is not a feature of HP.
Primary bronchiolitis has a wide variety of causes (reviewed in [30]), of which infection is probably the most common. The presence of neutrophils is suggestive of an infectious bronchiolitis, as is the combination of neutrophils in the bronchiolar lumen and chronic inflammatory cells in the bronchiolar wall. Infectious bronchiolitis is usually confined to the bronchioles and does not spread in the peribronchiolar interstitium.
Differential diagnosis of fibrotic HP
The differential diagnosis of fibrotic HP depends on the pattern of fibrosis. For pure peribronchiolar fibrosis, a major differential is microaspiration, and this distinction can be difficult if foreign material is not found because both fibrotic HP and microaspirtion can have associated granulomas. One helpful hint is that microaspiration does not produce the pattern of peribronchiolar fibrosis plus separate subpleural fibrosis that is common in fibrotic HP, nor, in my experience does microaspiration produce peribronchiolar metaplasia.
CTD-ILD can also produce a pattern of pure peribronchiolar fibrosis (Fig. 5C). The presence of numerous lymphoid aggregates, especially aggregates with germinal centers, and/or a plasma cell to lymphocyte ratio >1:1 (measured away from lymphoid aggregates) all suggest underlying CTD [18] or so-called interstitial pneumonia with autoimmune features (IPAF) [31].
A fibrotic NSIP pattern is most often a manifestation of underlying connective tissue disease or IPAF [31], and is a relatively uncommon pattern in fibrotic HP. Again, the finding of an interstitial plasma cell:lymphocyte ratio >1:1, numerous lymphoid aggregates, or lymphoid aggregates with germinal centers favors a diagnosis of connective tissue disease-associated NSIP, whereas the presence of granulomas or giant cells favors fibrotic HP. However, granulomas/giant cells are occasionally present in connective tissue disease-associated ILD [18].
Sarcoid usually scars by forming nodules, but sometimes scars in a more linear fashion (Fig. 5D). As opposed to fibrotic HP, in general even scarred sarcoid will demonstrate numerous sharply defined granulomas, and these may be overrun by hyalinization, something that is not a feature of fibrotic HP. As well, in sarcoid there is usually no interstitial inflammatory infiltrate.
The major problem is the separation of fibrotic HP with a UIP-like pattern from UIP/IPF, connective tissue disease-associated ILD with a UIP-like pattern, and, rarely, sarcoid. Differentiating features are shown in Table 4. UIP-like fibrotic HP is often very paucicellular, but if interstitial cellularity is present, the predominant cell (away from lymphoid aggregates) should be lymphocytes. The same findings mentioned above in regard to plasma cells, lymphoid aggregates, and germinal centers apply to the diagnosis of CTD-ILD with a UIP-like pattern [18]. Granulomas/giant cells favor fibrotic HP but occasionally are found in CTD-ILD. Peribronchiolar metaplasia affecting ≥ 50% of bronchioles strongly supports a diagnosis of fibrotic HP [20]. The issue of how much peribronchiolar fibrosis is permissible in UIP/IPF has been discussed above (and see Fig. 5B).
Molecular testing in the diagnosis of HP
Compared to the extensive detailed genetic analysis of neoplasms, there is relatively little in the literature on the genomics of ILD. These published reports have either looked at single nucleotide polymorphisms (SNPs) or gene expression patterns.
The MUC5B minor allele (rs35705950 G to T) was initially described in patients with UIP/IPF and has the functional effect of increased MUC5B production [32]. Non-Hispanic Caucasian heterozygous carriers of the minor allele have about a 6 fold risk of developing UIP/IPF and homozygous carriers about a 20 fold risk compared to individuals with no copies. While the MUC5B allele explains about 30% of the risk of developing UIP/IPF, it cannot be used for diagnosis, both because about 10% of the Non-Hispanic Caucasian population carries the minor allele, so that it may show up with any disease, and, particularly important for this discussion, it is also found with increased frequency in patients with fibrotic HP, patients with rheumatoid arthritis-associated UIP, and patients with asbestosis [32,33,34,35] (Fig. 6). These observations have lead to the conclusion that excess MUC5B is itself fibrogenic, although the mechanisms behind this effect are unclear.
Note the overlaps, particularly the finding of the MUC5B rs35705950 minor allele in usual interstitial pneumonia/idiopathic pulmonary fibrosis, fibrotic hypersensitivity pneumonitis, some cases of connective tissue disease-associated interstitial lung disease, and asbestosis. This allele appears to confer a risk of developing a fibrosing interstitial pneumonia but is not disease specific.
A wide variety of other SNPs are found with increased frequency in UIP/IPF, particularly SNPs in genes related to telomere maintenance (TERT, TERC); some SNPs in these genes lead to shortened telomeres at the ends of chromosomes [32]. However, the same lack of disease specificity applies to TERT and TERC as applies to MUC5B: these SNPs appear to predispose to the development of progressive fibrosing lung diseases but do not discriminate among them. Of interest, short telomeres don’t predispose to COPD [36].
Analysis of RNA expression patterns (RNAseq) has been promulgated as a means of identifying ILD, most commonly UIP/IPF. This approach offers a number of theoretical advantages, including, in some hands, the claimed ability to make specific diagnoses on conventional transbronchial forceps biopsies or transbronchial cryobiopsies [37,38,39]. The problem is that the classifiers have largely been set up by comparing UIP/IPF cases to other forms of ILD that are generally not fibrotic, with very few or no fibrotic HP cases included in the training sets, and the recent report by Kheir et al. [38] showed that their molecular classifier did not discriminate well between UIP/IPF and fibrotic HP; indeed, the paper by Richeldi et al. [39] indicates that this particular classifier will not separate UIP/IPF from fibrotic HP, some cases of CTD-ILD, and asbestosis.
The only paper that has specifically addressed gene expression patterns in fibrotic HP is that of Furosawa et al. [40]. Not surprisingly, they found a major overlap in expression patterns between UIP/IPF and fibrotic HP, presumably reflecting underlying fibrosis, but there were also differences: fibrotic HP cases showed increased expression of genes related to immune responsiveness and chemokine-mediated signaling, and in theory a UIP/IPF vs fibrotic HP expression pattern could be developed from these data.
All of these issues may be sorted out over time, but at the minute there does not appear to be a genetic test for separating UIP/IPF from fibrotic HP. However, given forthcoming changes in treatment of fibrosing interstitial pneumonias, this issue may become moot (see section “Treatment and Prognosis”).
Treatment and prognosis
The prognosis of HP definitely depends on the presence or absence of fibrosis, and less certainly on the ability to identify the offending antigen. Patients with radiologic [41, 42] or pathologic [43, 44] fibrosis have a consistently worse prognosis than those with no evidence of fibrosis; indeed nonfibrotic HP appears to be a disease that responds well to treatment.
In fibrotic HP the exact relationship between the pattern of pathologic fibrosis and prognosis is not clear. The few published reports on patients with fibrotic HP and a UIP-like pattern on biopsy generally reported an outcome similar to UIP/IPF (reviewed in 5). We [43] found that UIP-like and NSIP-like fibrosis were associated with equally poor outcomes, with a median survival of less than four years from the time of biopsy, whereas patients with only isolated peribronchiolar fibrosis fared better, while Wang et al. [44] reported that all 3 patterns were associated with a poor prognosis.
There is a widespread belief among ILD physicians that removal from antigen exposure improves the outcome in HP [45], but with little actual data on the question. However, Fernandez Perez et al. [41] did find that identification of the offending antigen was associated with better survival in both nonfibrotic and fibrotic HP. Sema et al. [46] reported that in patients with bird-induced fibrotic HP who had notionally ceased exposure, those with higher levels of residual household avian proteins fared worse than those with lower levels.
The major problem with removing the patient from antigen exposure is that, for probably the majority of fibrotic HP cases, the offending agent cannot be determined as noted above; [9, 10] nonetheless, it is important to include fibrotic HP in the differential diagnosis of biopsies that morphologically resemble UIP/IPF or fibrotic NSIP so that the clinician can search for potential exposures.
At this time the recommended treatment of both nonfibrotic and fibrotic HP is an immunosuppressive agent. For nonfibrotic HP this is typically a steroid, whereas for fibrotic HP mycophenolate or azathioprine is usually employed [47] (Table 5). The recommended treatment for UIP/IPF is an antifibrotic agent (pirfenidone, nintedanib) and steroids are contraindicated because they lead to worse outcomes [2], so the diagnostic distinction between fibrotic HP and UIP/IPF is crucial.
This scenario often puts the pathologist in a difficult position, since, as indicated above, separating fibrotic HP from UIP/IPF on biopsy can be exceedingly difficult. However, treatment recommendations in this area are rapidly changing because of very recent clinical trials that have demonstrated the value of the antifibrotic agents pirfenidone and nintedanib in any form of progressive fibrosing interstitial pneumonia [48, 49]. Once the use of antifibrotic agents in fibrotic HP becomes the accepted standard of treatment, the distinction between fibrotic HP and UIP/IPF will become less crucial.
Data availability statement
There are no data beyond the original published articles cited in the paper.
References
Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, et al. ATS/ERS/JRS/ALAT Committee on idiopathic pulmonary fibrosis. an official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824.
Raghu G, Remy-Jardin M, Myers JL, Richeldi L, Ryerson CJ, Lederer DJ, et al. American Thoracic Society, European Respiratory Society, Japanese Respiratory Society, and Latin American Thoracic Society. Diagnosis of idiopathic pulmonary fibrosis. an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198:e44–68.
Walsh SL, Wells AU, Desai SR, Poletti V, Piciucchi S, Dubini, et al. Multicentre evaluation of multidisciplinary team meeting agreement on diagnosis in diffuse parenchymal lung disease: a case-cohort study. Lancet Respir Med. 2016;4:557–65.
Morell F, Villar A, Montero MÁ, Muñoz X, Colby TV, Pipvath S, et al. Chronic hypersensitivity pneumonitis in patients diagnosed with idiopathic pulmonary fibrosis: a prospective case-cohort study. Lancet Respir Med. 2013;1:685–94.
Churg A, Bilawich A, Wright JL. Pathology of chronic hypersensitivity pneumonitis what is it? What are the diagnostic criteria? Why do we care? Arch Pathol Lab Med. 2018;142:109–19.
Churg A. Centrilobular fibrosis in fibrotic (chronic) hypersensitivity pneumonitis, usual interstitial pneumonia, and connective tissue disease-associated interstitial lung disease. Arch Pathol Lab Med. 2020;144:1509–1516.
Hashisako M, Tanaka T, Terasaki Y, Uekusa T, Achcar RD, Aswad BI, et al. Interobserver agreement of usual interstitial pneumonia diagnosis correlated with patient outcome. Arch Pathol Lab Med. 2016;140:1375–1382.
Tanizawa K, Ley B, Vittinghoff E, Elicker BM, Henry TS, Wolters PJ, et al. Significance of bronchiolocentric fibrosis in patients with histopathological usual interstitial pneumonia. Histopathology .2019;74:1088–97.
Raghu G, Remy-Jardin M, Ryerson CJ, Myers JL, Kreuter M, Vasakova M. Diagnosis of hypersensitivity pneumonitis in adults. an official ATS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2020;202:e36–69.
Fernández Pérez ER, Travis WD, Lynch DA, Brown KK, Johannson KA, Selman M, et al. Diagnosis and evaluation of hypersensitivity pneumonitis: CHEST Guideline and expert panel report. Chest, Apr 13:S0012-369200686-3. https://doi.org/10.1016/j.chest.2021.03.066. Online ahead of print. PMID: 33861992.
Morell F, Villar A, Ojanguren I, Muñoz X, Cruz MJ. Hypersensitivity pneumonitis: challenges in diagnosis and management, avoiding surgical lung biopsy. Semin Respir Crit Care Med. 2017;37:395–405.
Singh S, Collins BF, Sharma BB, Joshi JM, Talwar D, Katiyar S, et al. Interstitial lung disease in India. Results of a prospective registry. Am J Respir Crit Care Med. 2017;195:801–13.
Ryerson CJ. Making sense of bronchoalveolar lavage lymphocytosis in fibrotic interstitial lung disease. Ann Am Thor Soc. 2020;17:1382–3.
Morell F, Roger À, Reyes L, Cruz MJ, Murio C, Muñoz X. Bird fancier’s lung: a series of 86 patients. Med (Baltim). 2008;87:110–30.
Muñoz X, Sánchez-Ortiz M, Torres F, Villar A, Morell F, Cruz MJ. Diagnostic yield of specific inhalation challenge in hypersensitivity pneumonitis. Eur Respir J. 2014;44:1658–1565.
Silva CI, Müller NL, Lynch DA, Curran-Everett D, Brown KK, Lee KS, et al. Chronic hypersensitivity pneumonitis: differentiation from idiopathic pulmonary fibrosis and nonspecific interstitial pneumonia by using thin-section CT. Radiology .2008;246:288–297.
Hypersensitivity pneumonitis. In, Churg A, Muller NL: Atlas of interstitial lung disease pathology, 2nd ed. New York: Wolters Kluwer; 2020. p. 115–35.
Churg A, Wright JL, Ryerson CJ. Pathologic separation of chronic hypersensitivity pneumonitis from fibrotic connective tissue disease-associated interstitial lung disease. Am J Surg Pathol. 2017;41:1403–9.
Castonguay MC, Ryu JH, Yi ES, Tazelaar HD. Granulomas and giant cells in hypersensitivity pneumonitis. Hum Pathol. 2015;46:607–13.
Wright JL, Churg A, Hague CJ, Wong A, Ryerson CJ. Pathologic separation of idiopathic pulmonary fibrosis from fibrotic hypersensitivity pneumonitis. Mod Pathol. 2020;33:616–25.
Takemura T, Akashi T, Kamiya H, Ikushima S, Ando T, Oritsu M, et al. Pathological differentiation of chronic hypersensitivity pneumonitis from idiopathic pulmonary fibrosis/usual interstitial pneumonia. Histopathology .2012;61:1026–35.
Cavazza A, Colby TV, Dubini A, Tomassetti S, Ravaglia C, Poletti V, et al. Transbronchial cryobiopsy in the diagnosis of diffuse lung disease. Surg Pathol Clin. 2020;13:197–208.
Troy LK, Grainge C, Corte TJ, Williamson JP, Vallely MP, Cooper WA, et al. Cryobiopsy versus Open Lung biopsy in the Diagnosis of Interstitial lung disease alliance (COLDICE) Investigators. Diagnostic accuracy of transbronchial lung cryobiopsy for interstitial lung disease diagnosis (COLDICE): a prospective, comparative study. Lancet. Respir Med. 2020;8:171–81.
Romagnoli M, Colby TV, Berthet JP, Gamez AS, Mallet JP, Serre I, et al. Poor concordance between sequential transbronchial lung cryobiopsy and surgical lung biopsy in the diagnosis of diffuse interstitial lung diseases. Am J Respir Crit Care Med. 2019;199:1249–56.
Cooper WA, Mahar A, Myers JL, Grainge C, Corte TJ, Williamson JP, et al. Cryobiopsy for identification of usual interstitial pneumonia and other interstitial lung disease features: further lessons from COLDICE, a prospective multi-center study. Am J Respir Crit Care Med. 2020 Dec 7. https://doi.org/10.1164/rccm.202009-3688OC. Epub ahead of print. PMID: 33285079.
Churg A, Wright JL. Morphologic features of fibrotic hypersensitivity pneumonitis in transbronchial cryobiopsies versus video-assisted thoracoscopic biopsies: an in silico study. Arch Pathol Lab Med. 2021;145:448–52.
Smith ML, Hariri LP, Mino-Kenudson M, Dacic S, Attanoos R, Borczuk A, et al. Histopathologic assessment of suspected idiopathic pulmonary fibrosis: where we are and where we need to go. Arch Pathol Lab Med. 2020;144:1477–89.
Hariri LP, Smith ML, Mino-Kenudson M, Allen TC, Attanoos R, Borczuk A, et al. Pulmonary pathology society perspective on the 2018 American thoracic society, european respiratory society, japanese respiratory society, and latin american thoracic society idiopathic pulmonary fibrosis clinical practice guidelines. Ann Am Thorac Soc. 2020;17:550–4.
Sarcoid. In, Churg A, Muller NL: Atlas of Interstitial Lung Disease Pathology, 2nd ed. New York: Wolters Kluwer; 2020. p. 136–51.
Bronchiolitis. In, Churg A, Muller NL: Atlas of Interstitial Lung Disease Pathology, 2nd ed. New York: Wolters Kluwer; 2020. p. 223–37.
Graney BA, Fischer A. Interstitial pneumonia with autoimmune features. Ann Am Thorac Soc. 2019;16:525–33.
Adegunsoye A, Vij R, Noth I. Integrating genomics into management of fibrotic interstitial lung disease. Chest .2019;155:1026–40.
Ley B, Newton CA, Arnould I, Elicker BM, Henry TS, Vittinghof E, et al. The MUC5B promoter polymorphism and telomere length in patients with chronic hypersensitivity pneumonitis: an observational cohort-control study. Lancet Respir Med. 2017;5:639–47.
Juge PA, Lee JS, Ebstein E, Furukawa H, Dobrinskikh E, Gazal S, et al. MUC5B promoter variant and rheumatoid arthritis with interstitial lung disease. N. Engl J Med. 2017;379:2209–19.
MGJP Platenburg, Wiertz IA, van der Vis JJ, Crestani B, Borie R, Dieude P, et al. The MUC5B promoter risk allele for idiopathic pulmonary fibrosis predisposes to asbestosis. Eur Respir J. 2020;55:1902361.
Duckworth A, Gibbons MA, Allen RJ, Almond H, Beaumont RN, Wood AR, et al. Telomere length and risk of idiopathic pulmonary fibrosis and chronic obstructive pulmonary disease: a mendelian randomisation study. Lancet Respir Med. 2021;9:285–94.
Raghu G, Flaherty KR, Lederer DJ, Lynch DA, Colby TV, Myers JL, et al. Use of a molecular classifier to identify usual interstitial pneumonia in conventional transbronchial lung biopsy samples: a prospective validation study. Lancet Respir Med. 2019;7:487–96.
Kheir F, Alkhatib A, Berry GJ, Daroca P, Diethelm L, Rampolla R. Using bronchoscopic lung cryobiopsy and a genomic classifier in the multidisciplinary diagnosis of diffuse interstitial lung diseases. Chest .2020;158:2015–25.
Richeldi L, Scholand MB, Lynch DA, Colby TV, Myers JL, Groshong SD, et al. Utility of a molecular classifier as a complement to high- resolution computed tomography to identify usual interstitial pneumonia. Am J Respir Crit Care Med. 2021;203:211–20.
Furusawa H, Cardwell JH, Okamoto T, Walts AD, Konigsberg IR, Kurche JS, et al. Chronic hypersensitivity pneumonitis, an interstitial lung disease with distinct molecular signatures. Am J Respir Crit Care Med. 2020;202:1430–44.
Fernández Pérez ER, Swigris JJ, Forssén AV, Tourin O, Solomon JJ, Huie TJ. et al. Identifying inciting antigen is associated improved survival patients chronic hypersensitivity pneumonitis. Chest. 2013;144:1644–51.
Salisbury ML, Gu T, Murray S, Gross BH, Chughtai A, Sayyouh M, et al. Hypersensitivity pneumonitis: radiologic phenotypes are associated with distinct survival time and pulmonary function trajectory. Chest .2019;155:699–711.
Churg A, Sin DD, Everett D, Brown K, Cool C. Pathologic patterns and survival in chronic hypersensitivity pneumonitis. Am J Surg Pathol. 2009;33:1765–70.
Wang P, Jones KD, Urisman A, Elicker BM, Urbania T, Johannson KA, et al. Pathologic findings and prognosis in a large prospective cohort of chronic hypersensitivity pneumonitis. Chest .2017;152:502–9.
Vasakova M, Morell F, Walsh S, Leslie K, Raghu G. Hypersensitivity pneumonitis: perspectives in diagnosis and management. Am J Respir Crit Care Med. 2017;196:680–9.
Sema M, Miyazaki Y, Tsutsui T, Tomita M, Eishi Y, Inase N. Environmental levels of avian antigen are relevant to the progression of chronic hypersensitivity pneumonitis during antigen avoidance. Immun Inflamm Dis. 2018;6:154–62.
Morisset J, Johannson KA, Vittinghoff E, Aravena C, Elicker BM, Jones KD, et al. Use of mycophenolate mofetil or azathioprine for the management of chronic hypersensitivity pneumonitis. Chest .2017;151:619–25.
Flaherty KR, Wells AU, Cottin V, Devaraj A, Walsh SLF, Inoue Y, et al. INBUILD trial investigators. nintedanib in progressive fibrosing interstitial lung diseases. N. Engl J Med. 2019;381:1718–27.
Maher TM, Corte TJ, Fischer A, Kreuter M, Lederer DJ, Molina-Molina M, et al. Pirfenidone in patients with unclassifiable progressive fibrosing interstitial lung disease: a double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Respir Med. 2020;8:147–57.
Author information
Authors and Affiliations
Contributions
Study design, writing of manuscript: AC.
Corresponding author
Ethics declarations
Funding statement
No specific funding was used for this paper.
Ethics approval and consent to participate
This project was approved by the University of British Columbia Research Ethics Board.
Competing interests
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Churg, A. Hypersensitivity pneumonitis: new concepts and classifications. Mod Pathol 35 (Suppl 1), 15–27 (2022). https://doi.org/10.1038/s41379-021-00866-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-021-00866-y
This article is cited by
-
Usual interstitial pneumonia: a clinically significant pattern, but not the final word
Modern Pathology (2022)