Abstract
Little is known about B-lymphoblastic leukemia (B-ALL) that lacks expression of terminal deoxynucleotidyl transferase (TdT). To address this, we performed the largest study to date of TdT-negative B-ALL using data from St. Jude Total XV and XVI clinical trials. Compared to TdT-positive B-ALL (n = 896), TdT-negative B-ALL (n = 21) was associated with younger age (median, 1.4 versus 6.8 years, P < 0.001), higher white blood cell count (median, 52.8 versus 9.9 × 109/L, P < 0.001), absence of hyperdiploidy (0 versus 27.8%, P = 0.002), KMT2A rearrangement (100 versus 1.9%, P < 0.001), and inferior 5-year event-free survival (EFS) (76.2 versus 90.3%, P = 0.047). In the context of KMT2A-rearranged B-ALL (n = 38), TdT-negativity was significantly associated with the MLLT1 rearrangement partner (P = 0.026) but was not independently predictive of survival, suggesting that the high-risk features of TdT-negative B-ALL are secondary to underlying KMT2A rearrangements. Finally, we compared the sensitivity of TdT-negativity to neuron-glial antigen 2 (NG.2) expression for the detection of KMT2A rearrangements and found that 63% of KMT2A-rearranged B-ALL cases not identified by NG.2 were TdT-negative. The results of this study expand the spectrum of immunophenotypic features that are specific for high-risk KMT2A rearrangements in pediatric B-ALL and can be readily implemented using existing standard acute leukemia flow cytometry panels.
Similar content being viewed by others
Background
Terminal deoxynucleotidyl transferase (TdT) expression is an immunophenotypic marker of immaturity characteristic of lymphoblasts. With rare exceptions, the expression of TdT by an aberrant leukemic clonal B-cell population supports the diagnosis of B-lymphoblastic leukemia (B-ALL) while effectively ruling-out a mature B-cell neoplasm. However, ~2% of B-ALL cases lack TdT expression [1] and little is known about the clinicopathologic and genetic features of this unusual and potentially diagnostically challenging immunophenotypic subtype. To address this, we performed the largest study to date of TdT-negative B-ALL.
Methods
With approval from the institutional review board of St. Jude Children’s Research Hospital, all cases of B-ALL treated on the St. Jude Total Therapy XV and XVI clinical trials were identified [2, 3]. Cases of B-ALL that were reported as TdT-negative were selected for further review. Review of corresponding bone marrow aspirate or peripheral blood smears was performed for all cases to confirm that the leukemic population was morphologically consistent with lymphoblasts. Original flow cytometry scatter plots were reviewed for each case to evaluate TdT expression using residual T-lymphocytes as a negative internal control with a 10% cutoff used to define TdT negativity [4]. Cases in which the intensity of lymphoblast TdT expression matched that of the isotype control yet exceeded that of residual lymphocytes in >10% of events were regarded as TdT subset positive (Fig. 1). Corresponding clinicopathologic and survival data for cases of TdT-negative B-ALL were subsequently compared to those of TdT-positive B-ALL.
Flow cytometry scatter plots depict three separate cases of B-ALL with different levels of TdT expression. Expression of TdT was measured using T-lymphocytes as a negative internal control and cases were classified as TdT-positive if >10% of B-lymphoblasts expressed TdT at an intensity greater than that of the T-lymphocytes. Blue events represent T-lymphocytes and red events represent leukemic B-lymphoblasts. A Example of B-ALL classified as TdT-negative based on <10% of B-lymphoblasts expressing TdT at an intensity greater than that of the T-lymphocytes. B Example of a case classified as TdT subset positive due to dim TdT expression in >10% of B-lymphoblasts. C Example of TdT-positive B-ALL with uniformly bright TdT expression.
Flow cytometry
Four or eight color flow cytometry was performed on diagnostic peripheral blood and bone marrow aspirate samples using a FACSCalibur or FACSCanto II flow cytometer and analyzed with FACSDiva software (Becton Dickinson, San Jose, CA) as previously described [5, 6]. Anti-TdT antibody (clone HT-6; Agilent Technologies, Santa Clara, CA) was used to evaluate cytoplasmic TdT expression. A minimum of 20,000 cells per tube were counted and the overall sensitivity of the assay for the detection of a leukemic lymphoblast population was 0.05%.
Leukemic B-lymphoblasts were identified by a combination of CD45 versus side‐scatter properties, co-expression of B-lineage markers (CD19, CD22, and cytoplasmic CD79a), and immunophenotypic markers of immaturity (CD34, CD133, and NG.2), absence of cytoplasmic CD3 and cytoplasmic MPO expression, and aberrant immunophenotypic features which distinguished the neoplastic population from hematogones. In cases which lacked expression of all immaturity markers (TdT, CD34, CD133, and NG.2), the diagnosis of B-ALL was supported by the presence of extensive leukemic disease, lymphoblast morphology, absence of surface light chain expression by flow cytometry, and cytogenetic features.
Cytogenetics
Giemsa-banded conventional cytogenetic studies were performed on unstimulated fresh bone marrow aspirate or peripheral blood samples with a minimum of 20 metaphases counted. KMT2A rearrangements were also identified by fluorescence in situ hybridization using a KMT2A (11q23) dual color probe (Abbott Molecular Inc., Des Plaines, IL) with 200 interphase nuclei evaluated for each case and by reverse-transcriptase polymerase chain reaction (RT-PCR).
Evaluation of CNS disease
Assessment of central nervous system (CNS) involvement was performed by cytomorphologic evaluation of Wright-stained cerebrospinal fluid cytospin preparations and classified as follows: CNS 1, no detectable blasts; CNS 2, <5 WBC/μL with blasts; CNS 3, ≥5 WBC/μL with blasts; and traumatic lumbar puncture with blasts, ≥10 RBCs/μL with blasts.
Statistical analysis
Categorical variables were compared using Fisher’s exact test while continuous variables were compared using the Wilcoxon rank sum test. Event-free survival (EFS) and overall survival (OS) probabilities were estimated using the Kaplan–Meier method and compared using the log-rank test. All reported P values are two-sided and not adjusted for multiple comparisons. Statistical analyses were performed with SAS version 9.4.
Results
Immunophenotypic features of TdT-negative B-ALL
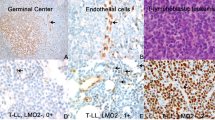
Twenty-one cases of B-ALL originally reported as TdT-negative were identified among the 917 B-ALL cases treated on Total XV and XVI (2.3%), all of which met the morphologic and immunophenotypic inclusion criteria. By flow cytometry, all cases were uniformly positive for CD19, CD22, and cytoplasmic CD79a while negative for cytoplasmic CD3, cytoplasmic MPO, and surface kappa/lambda light chains. The frequency of at least dim or partial expression of other markers was as follows: CD20 (47.6%), CD38 (100%), CD34 (42.9%), CD117 (0%), CD133 (61.9%), CD123 (71.4%), HLA-DR (100%), CD10 (23.8%), CD15 (47.6%), NG.2 (68.8%), CD13 (0%), CD14 (0%), CD33 (33.3%), CD2 (14.2%), CD5 (9.5%), and CD7 (52.3%). Three cases (14.3%) were negative for all immunophenotypic markers of immaturity (TdT, CD34, CD133, and NG.2); in these cases, the diagnosis of B-ALL was supported by the presence of extensive leukemic disease, morphologic features consistent with lymphoblasts, absence of surface light chain expression by flow cytometry, and the presence of KMT2A rearrangements.
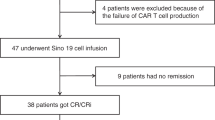
Characteristics and outcomes of TdT-negative B-ALL from Total XV and XVI
The complete clinicopathologic features are summarized in Table 1. Compared to TdT-positive B-ALL, TdT-negative B-ALL was associated with younger age at diagnosis (median, 1.4 versus 6.8 years, P < 0.001), higher white blood cell count (median, 52.8 versus 9.9 × 109/L, P < 0.001), non-hyperdiploidy (DNA index < 1.16) (0 versus 27.8%, P = 0.002), and KMT2A rearrangement (100 versus 1.9%, P < 0.001). KMT2A-rearrangement represented the sole cytogenetic abnormality in 66.7% of TdT-negative cases; in the remaining cases, none of the additional cytogenetic abnormalities were recurrent. TdT-negative B-ALL had significantly lower 5-year EFS compared to TdT-positive B-ALL (76.2 versus 90.3%, P = 0.047; Fig. 2). The difference in 5-year OS between the two groups was not statistically significant (85.7 versus 95.5% for TdT-negative and positive B-ALL, respectively; P = 0.091). There was no significant difference in outcomes between cases which only harbored KMT2A rearrangements and those which had additional cytogenetic abnormalities.
TdT expression in the context of KMT2A-rearranged B-ALL
Among the 917 cases of B-ALL, KMT2A rearrangements were identified in 38 (4.1%), the clinicopathologic features of which are summarized in Table 1. Negative TdT expression was identified in 55.3% of KMT2A-rearranged B-ALL; among the TdT-positive cases, 47.1% were dim positive while 52.9% showed moderate to bright positivity (Fig. 1). Among KMT2A-rearranged B-ALL cases, negative TdT expression was significantly associated with the presence of the MLLT1 rearrangement partner, which was present in 38.1% of TdT-negative cases versus 5.9% of TdT-positive cases (P = 0.026). However, there was no significant association between TdT expression and EFS (75.9% versus 58.8% for TdT-negative and positive KMT2A-rearranged B-ALL, respectively; P = 0.3).
NG.2 and negative TdT expression as immunophenotypic markers of KMT2A rearrangement
NG.2 expression was evaluated in 23 cases of KMT2A-rearranged B-ALL and was positive in 15 cases (65.2%). Among the eight cases of KMT2A-rearranged B-ALL that did not express NG.2, five were TdT negative (62.5%).
Discussion
TdT is a DNA polymerase present in immature pre-B and pre-T cells that is responsible for the insertion of nucleotides to the V(D)J gene segment during immunoglobulin and T cell receptor gene rearrangement. Its expression is limited to the lymphoid compartment with regulation influenced by stage-specific transcription factors. Leukemic lymphoblasts, in general, express high levels of TdT; ALL cell lines were in fact one of the first sources of the purified enzyme [7]. However, ~2% of pediatric B-ALL cases lack TdT expression [1] and little is known about this unusual subtype. Here, in the largest series of TdT-negative B-ALL to date, we demonstrate that these potentially diagnostically-challenging cases represent an immunophenotypic variant of KMT2A-rearranged B-ALL.
Compared to TdT-positive B-ALL, TdT-negative B-ALL was significantly associated with younger age at diagnosis (median, 1.4 versus 6.8 years), higher white blood cell count (median, 52.8 versus 9.9 × 109/L), uniform absence of hyperdiploidy (0 versus 27.8%), and inferior 5-year EFS (76.2 versus 90.3%). Notably, however, when TdT-negative KMT2A-r B-ALL was compared to a cohort of similarly treated TdT-positive KMT2A-r B-ALL cases, TdT expression was not associated with a significant difference in EFS, suggesting that the high-risk features of TdT-negative B-ALL are best explained, at least in part, by the presence of underlying KMT2A rearrangements.
Negative TdT expression is a frequent feature of KMT2A-rearranged B-ALL. Overall, 55.2% of pediatric KMT2A-rearranged B-ALL was found to be TdT-negative and, interestingly, this distinctive immunophenotypic feature was significantly associated with the MLLT1 rearrangement partner. In total, eight out of nine cases (88.9%) of B-ALL cases with KMT2A-MLLT1 were TdT-negative and this accounted for 38.1% of all TdT-negative KMT2A-rearranged B-ALL cases compared to 5.9% of TdT-positive cases (P = 0.026). The single case with KMT2A-MLLT1 that was classified as TdT-positive showed only dim subset positivity, indicating that negative or occasionally dim TdT expression is a defining immunophenotypic feature of this particular KMT2A-rearranged B-ALL subtype. Consistent with the absence of TdT expression found in this study, a report on immunoglobulin gene rearrangements in infantile KMT2A-rearranged B-ALL found that rearrangements were less frequent in KMT2A-rearranged disease compared to childhood B-ALL [8]. Further, the maturity status of the rearrangement was mainly determined by the KMT2A partner with KMT2A-MLLT1 positive patients having significantly less IGK and IGL gene rearrangements compared to KMT2A-MLLT3 [8].
The observation that TdT-negative B-ALL is consistently KMT2A-rearranged aligns with what little data is available in the literature. In a study of 186 children with newly diagnosed B-ALL, only five cases were found to be TdT-negative among which three harbored KMT2A rearrangements [1]. Interestingly, Yasmeen et al described four cases of KMT2A-wildtype B-ALL which were reported as TdT-negative by flow cytometry but TdT-positive by immunohistochemistry [9]. Given that these cases were TdT-positive by immunohistochemistry, it is possible that the application of the flow cytometric criteria for TdT expression used in our study would have led to the classification of at least some of these cases as TdT dim-positive. Alternatively, this discrepancy may reflect subtle differences in gating strategies or in the overall sensitivity of the assays for the detection of low-level TdT expression. As bone marrow biopsies for B-ALL diagnosed by peripheral blood flow cytometry are not routinely performed at our institution, confirmatory TdT immunohistochemistry was not possible in this study.
The data presented in this study expand the spectrum of immunophenotypic features that are specific for KMT2A rearrangement in B-ALL and can be reliably used to predict the presence of these high-risk rearrangements at the time of initial flow cytometric diagnosis. Currently, expression of NG.2 represents the most well-established standalone immunophenotypic marker specific for KMT2A-rearrangement in B-ALL [6, 10]. However, anti-NG.2 antibody is not a standard component of most diagnostic flow cytometry panels currently utilized in the clinical setting. Further, even in this series where NG.2 expression was evaluated in a significant subset of cases, it yielded a false negative result in 34.8%. Notably, however, among the KMT2A-rearranged B-ALL cases that were NG.2-negative, 62.5% were TdT-negative, demonstrating that even in a setting where NG.2 expression is routinely evaluated, negative TdT expression represents a complementary immunophenotypic parameter for predicting KMT2A rearrangement.
In summary, the results of this study demonstrate that negative TdT expression in pediatric B-ALL is a specific immunophenotypic marker for KMT2A rearrangement and that this association likely underlies the poor clinical outcomes documented in these cases. As TdT expression is already routinely evaluated by most standard acute leukemia diagnostic flow cytometry panels, recognition of negative TdT expression at the time of initial flow cytometric diagnosis can be used to anticipate the likelihood of KMT2A rearrangement and ensure that appropriate confirmatory genetic testing is performed.
References
Liu L, McGavran L, Lovell MA, Wei Q, Jamieson BA, Williams SA, et al. Nonpositive terminal deoxynucleotidyl transferase in pediatric precursor B-lymphoblastic leukemia. Am J Clin Pathol. 2004;6:810.
Pui CH, Campana D, Pei D, Bowman WP, Sandlund JT, Kaste SC, et al. Treating childhood acute lymphoblastic leukemia without cranial irradiation. N Engl J Med. 2009;26:2730–41.
Jeha S, Pei D, Choi J, Cheng C, Sandlund JT, Coustan-Smith E, et al. Improved CNS control of childhood acute lymphoblastic leukemia without cranial irradiation: St Jude total therapy study 16. J Clin Oncol. 2019;35:3377–91.
Bene MC, Castoldi G, Knapp W, Ludwig WD, Matutes E, Orfao A, et al. Proposals for the immunological classification of acute leukemias. European Group for the immunological characterization of leukemias (EGIL). Leukemia. 1995;10:1783–6.
Cheng J, Klairmont MM, Choi JK. Peripheral blood flow cytometry for the diagnosis of pediatric acute leukemia: highly reliable with rare exceptions. Pediatr Blood Cancer. 2019;1:e27453.
Behm FG, Smith FO, Raimondi SC, Pui CH, Bernstein ID. Human homologue of the rat chondroitin sulfate proteoglycan, NG2, detected by monoclonal antibody 7.1, identifies childhood acute lymphoblastic leukemias with t(4;11)(q21;q23) or t(11;19)(q23;p13) and MLL gene rearrangements. Blood. 1996;87:1134–9.
Deibel MR Jr., Coleman MS. Biochemical properties of purified human terminal deoxynucleotidyltransferase. J Biol Chem. 1980;9:4206–12.
Jansen MW, Corral L, van der Velden VH, Panzer-Grümayer R, Schrappe M, Schrauder A, et al. Immunobiological diversity in infant acute lymphoblastic leukemia is related to the occurrence and type of MLL gene rearrangement. Leukemia. 2007;4:633–41.
Yasmeen S, Rajkumar A, Grossman H, Szallasi A. Terminal deoxynucleotidyl transferase (TdT)-negative lymphoblastic leukemia in pediatric patients: incidence and clinical significance. Pediatr Dev Pathol. 2017;6:463–8.
Prieto C, López-Millán B, Roca-Ho H, Stam RW, Romero-Moya D, Rodríguez-Baena FJ, et al. NG2 antigen is involved in leukemia invasiveness and central nervous system infiltration in MLL-rearranged infant B-ALL. Leukemia. 2018;3:633–44.
Acknowledgements
We thank the patients who participated in Total XV and XVI and Christopher Clark from the St. Jude flow cytometry laboratory.
Author information
Authors and Affiliations
Contributions
Study conception: M.M.K. and J.K.C.; Study design: M.M.K., J.K.C., H.I., and C.-H.P.; provision of study material: C.-H.P., S.J., J.K.C., H.I., and T.A.G.; data collection and assembly: Y.Z., J.K.C., M.M.K., and Y.L.; data analysis and interpretation: MMK, JKC, YZ, CC, CHP, HI; manuscript writing: MMK; manuscript editing and final approval: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Klairmont, M.M., Zhou, Y., Cheng, C. et al. Clinicopathologic and prognostic features of TdT-negative pediatric B-lymphoblastic leukemia. Mod Pathol 34, 2050–2054 (2021). https://doi.org/10.1038/s41379-021-00853-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-021-00853-3