Abstract
Allograft survival of deceased donor kidneys with suboptimal histology (DRTx/suboptimal histology: >10% glomerulosclerosis, >10% tubulointerstitial scarring, or >mild vascular sclerosis) is inferior to both DRTx with optimal histology (DRTx/optimal histology) and living donor kidneys irrespective of histologic changes (LRTx). In this report, we explored the reasons behind this guarded outcome with a special focus on the role of alloimmunity. We initially assessed gene expression in 39 time-zero allograft biopsies using the Nanostring 770 genes PanCancer Immune Profiling Panel. Subsequently, we studied 696 consecutive adult kidney allograft recipients that were grouped according to allograft type and histology at time-zero biopsy [DRTx/suboptimal histology (n = 194), DRTx/optimal histology (n = 166), and LRTx (n = 336)]. Part-1: Several immune pathways were upregulated in time-zero biopsies from DRTx/suboptimal histology (n = 11) compared to LRTx (n = 17) but not to DRTx/optimal histology (n = 11). Part-2: Amongst the three groups of recipients, DRTx/suboptimal histology had the highest incidence of acute rejection episodes, most of which occurred during the first year after transplantation (early rejection). This increase was mainly attributed to T cell mediated rejection, while the incidence of antibody-mediated rejection was similar amongst the three groups. Importantly, early acute T cell mediated rejection was a strong independent predictor for allograft failure in DRTx/suboptimal histology (adjusted HR: 2.13, P = 0.005) but not in DRTx/optimal histology nor in LRTx. Our data highlight an increased baseline immunogenicity in DRTx/suboptimal histology compared to LRTx but not to DRTx/optimal histology. However, our results suggest that donor chronic histologic changes in DRTx may help transfer such increased baseline immunogenicity into clinically relevant acute rejection episodes that have detrimental effects on allograft survival. These findings may provide a rationale for enhanced immunosuppression in recipients of DRTx with baseline chronic histologic changes to minimize subsequent acute rejection and to prolong allograft survival.
Similar content being viewed by others
Introduction
Despite being the most commonly transplanted solid organs with more than 23,000 kidney transplanted nationally in 2019 [https://unos.org/data/transplant-trends/], there remains inadequate supply of donor kidneys and an unacceptably high discard rate of potentially transplantable kidneys [1,2,3]. The most common reason reported for kidney discard is significant chronic changes on donor biopsy at the time of organ recovery [4]. To overcome these problems, clinicians must expand their criteria for allograft acceptance from deceased donors (DRTx) to include older donors, procurement biopsies with significant histologic chronic changes, and prolonged ischemia time [5]. Such an approach is challenging and not universally accepted because this may lead to reduced long-term allograft survival, which is already worse in patients receiving DRTx compared to those who receive allografts from living donors (LRTx) [6, 7]. In a recent study, we assessed the impact of donor’s chronic histologic changes on allograft survival using formalin-fixed paraffin-embedded (FFPE) time-zero biopsies [8]. We have shown that DRTx with chronic histologic changes defined by one or more of: >10% glomerulosclerosis, >10% tubulointerstitial scarring, or more than mild vascular sclerosis (also referred to as “suboptimal histology) were associated with inferior long-term allograft survival compared to DRTx with “optimal histology” or to LRTx, where chronic histologic changes were not associated with allograft survival [8]. The explanations for such differences are not completely clear. However, since alloimmune injuries remain the main obstacle to long-term allograft survival [9], we hypothesized that acute rejection is a major contributing factor in DRTx with suboptimal histology.
To address this issue, we first conducted a pilot comparison of gene expression in 39 time-zero kidney allograft biopsies (11 DRTx/suboptimal histology, 11 DRTx/optimal histology, and 17 LRTx) as indicators of baseline immune-related pathways. This was followed by retrospective analysis of a large cohort of 696 adult kidney allograft recipients, where we focused on the association of allograft source and histology with subsequent acute rejection and allograft survival.
Material and methods
This two-part retrospective single center study was performed under the approved guidance of the institutional review board at Columbia University Irving Medical Center (CUIMC).
Part-1: Gene expression analysis
Using Nanostring platform (Seattle, WA), we performed a pilot exploration of gene expression profile in a 39 FFPE kidney allograft time-zero biopsies. These intraoperative biopsies were performed ~1 h after allograft reperfusion (11 DRTx/suboptimal histology, 11 DRTx/optimal histology, and 17 LRTx) following completion of the ureteroneocystostomy. Briefly, biopsies were sectioned (each 10 μm ×10). Total RNA was isolated from sectioned material using miRNeasy FFPE Kit (Qiagen, Valencia, CA) according to the manufacturer’s instructions and quantified by NanoDrop (Thermo Scientific, Wilmington, DE), Bioanalyzer 2100 (Agilent, Santa Clara, CA), and Qubit RNA BR (Thermo Fisher Scientific, Waltham, MA). 100 ng of isolated RNA was then hybridized to the 770 genes PanCancer Immune Profiling Panel (NanoString Technologies) for 20 h at 65 °C according to the manufacturer’s instructions. After hybridization, the sample cartridge was transferred to the Digital Analyzer where Digital counting was used to determine gene expression using the maximum 555 fields of view.
For data analysis, we utilized the nSolver Analysis Software (version 4.0), including the nCounter Advanced Analysis (version 2.0), which uses the geNorm algorithm to normalize the data. Differential Expression (DE) module was used to identify the specific targets which exhibit significantly increased or decreased expression where false discovery rate was calculated by moderately conservative estimates of the Benjamini-Yekutieli (B.Y.) method. Pathway scores were assessed in 20 different immunology-associated pathways using the nCounter Advanced Analysis Software. In each sample, individual pathway scores were calculated by summarizing several gene measurements from a particular pathway into a single score based on the first principal component of each gene set’s data [10,11,12]. Pathway scores were compared using Mann–Whitney. Since 20 pathways have been studied, a Bonferroni corrected significance cutoff of 0.0025 was utilized.
Part-2: Clinical-pathologic assessment
All time-zero kidney allograft biopsies, obtained ~1 h after reperfusion, from adult patients (≥18 years old) who underwent kidney transplantation at CUIMC between 1/2006 and 12/2009 were identified retrospectively. To reduce bias, ABO-incompatible grafts and time-zero biopsies containing <7 glomeruli were excluded. The final cohort comprised 696 patients with time-zero biopsies (360 DRTx, 336 LRTx). For all LRTx, donor and recipient operations were performed concomitantly, not sequentially, resulting in minimal ischemic time.
Circulating donor-specific antibodies (DSA) were assessed using Luminex single-antigen bead assay (One Lambda Inc, Canoga Park, CA). DSA was considered positive if one or more of the HLA antibodies directed against donor antigens had an MFI higher than 1000.
Per CUIMC protocol, the vast majority of patients are maintained on tacrolimus and mycophenolate sodium, without corticosteroids. Recipient and donor demographics (age, sex, and race), end-stage renal disease etiology, immunologic transplant baseline characteristics (HLA mismatch and pre-transplant DSA), history of previous renal transplantation, induction therapy, and cold ischemia time and donor cause of death (for DRTx) were extracted from medical records.
Histologic evaluation
Time-zero allograft biopsies were FFPE needle biopsies that were stained with standard H&E, periodic acid Schiff (PAS), methenamine silver and trichrome. Time-zero biopsies were assessed for the degree of glomerulosclerosis (%) and tubulointerstitial scarring (%). The severity of arteriosclerosis and arteriolosclerosis/hyalinosis were semi-quantitatively (0–3) assessed according to 1997 Banff criteria [13]. Consistent with prior reports [5, 8], time-zero biopsies were classified as having “optimal histology” when showing ≤10% glomerulosclerosis, ≤10% tubulointerstitial scarring, no more than mild arteriosclerosis, and no more than mild arteriolar hyalinosis. “Suboptimal histology” was defined by having any of the following: >10% glomerulosclerosis, >10% tubulointerstitial scarring, moderate/severe arteriosclerosis, or moderate/severe arteriolar hyalinosis (Fig. 1).
A Global glomerulosclerosis. In this post-reperfusion biopsy, the percentage of global glomerulosclerosis exceeded 10%. Thus, this sample was classified as “suboptimal histology” (periodic acid–Schiff stain; original magnification ×200). B Tubulointerstitial scarring. In this post-reperfusion biopsy, the percentage of tubulointerstitial scarring exceeded 10% of the sampled cortex. Thus, this sample was classified as “suboptimal histology” (periodic acid–Schiff stain; original magnification ×100). C Moderate arteriosclerosis. This artery displays arterial narrowing of 26-50% of the luminal areas. Therefore, this post-reperfusion biopsy was classified as “suboptimal histology” (periodic acid–Schiff stain; original magnification ×400). D Arteriolar hyalinosis. A representative photomicrograph of arterioles with moderate to severe hyalinosis. In this particular sample, several arterioles showed similar changes. Hence, the biopsy was classified as “suboptimal histology” (periodic acid–Schiff stain; original magnification ×600).
Subsequent allograft biopsies were assessed according to the 2019 Banff recommendations [14]. Acute T cell-mediated rejection (TCMR) was defined by the presence of borderline or greater changes (grades IA–III). At our center, patients with “borderline changes” were treated similarly to grade 1A TCMR (intravenous methylprednisolone) and were found to have similar clinical courses to that of overt TCMR [15, 16]. Given the lack of vigorous monitoring of post-transplant DSA during the study period, allograft biopsies with histologic evidence of acute antibody-mediated tissue injury and evidence of current/recent antibody interaction with vascular endothelium but without available data on concurrent DSA were classified as AMR (n = 19). To eliminate reproducibility as a confounding factor, time-zero biopsies, follow-up allograft biopsies with “borderline changes” and selected follow-up biopsies with findings suggestive of AMR were re-evaluated by a single pathologist (IB).
Comparison groups, follow-up, and outcome
Since we were interested in studying the reasons why DRTx/suboptimal histology had worse outcome than DRTx/optimal histology and LRTx (regardless of histology) [8], we classified our cohort into three groups: DRTx/suboptimal histology (n = 194), DRTx/optimal histology (n = 166), and LRTx (n = 336). Recipients were followed-up till 5/2016 or development of allograft failure. Acute rejection was regarded as the primary outcome. The first biopsy showing acute rejection was considered index biopsy and used for analyses. Death censored allograft failure, defined as chronic re-initiation of renal replacement therapy or re-transplantation, was considered a secondary outcome. We also documented the development of glomerular diseases, including immune-mediated glomerulonephritis, primary focal segmental glomerulosclerosis, and collapsing glomerulopathy.
Statistics
Statistical analysis was performed using SPSS Statistics 26 (IBM, Arkmonk, NY) or Prism-5 (GraphPad Inc, San Diego CA). Categorical variables were compared using Fisher’s exact or Chi Square test when multiple groups were compared. Continuous variables were compared using Mann–Whitney or Kruskal–Wallis test followed by Dunn’s comparison. Time-to-event analyses, such as allograft survival and rejection-free survival, were assessed by the Kaplan-Meier curves and comparisons were performed using log-rank test or Cox proportional hazards (PH). Univariate Cox PH was used to guide the selection of variables for multivariable analysis whenever P values were <0.1. P values < 0.05 with a two-sided hypothesis testing were considered statistically significant.
Results
Part-1: DRTx have enhanced immunogenic profile at transplant baseline
Gene expression was assessed in 39 time-zero biopsies (11 DRTx/suboptimal histology, 11 DRTx/optimal histology, and 17 LRTx) using the 770 PanCancer Immune Profiling Panel. Heat map of normalized genes revealed clustering of the samples based on the type of the allograft (DRTx vs. LRTx) but not based on the presence of chronic histologic changes in DRTx samples (DRTx/suboptimal vs. DRTx/optimal) (Supplementary Fig. 1A). On follow-up, acute rejection episodes developed in 15 patients (13 TCMR and 2 AMR). This small sample revealed lack of clustering or difference in immune pathways scores when grouped according to subsequent development of acute rejection episodes (TCMR, AMR, or no rejection) (Supplementary Fig. 1A, B). We then studied the association between baseline immunogenicity in DRTx and cold ischemia-time. No significant difference in expression was seen in any individual gene (Supplementary Fig. 1C). While most immune pathways showed numerically higher scores in patients with prolonged ischemia time, none of these differences reached statistical significance. Furthermore, there was no significant correlation between immune pathway scores and cold ischemia time (Supplementary Fig. 1D).
Next, we focused on gene expression in our three groups of interest (DRTx/suboptimal histology, DRTx/optimal histology, and LRTx). We first compared gene expression between DRTx/suboptimal histology and LRTx. Differential expression identified 115 genes whose expression differed significantly (adjusted P < 0.05). Of these 115 genes, 103 were upregulated and only 12 were downregulated in DRTx/suboptimal histology as compared to LRTx (Fig. 2A, Supplementary Table 1). Majority of the immune-related pathways were upregulated in DRTx/suboptimal histology (Fig. 2B) and the most significant results were obtained by comparing complement, cytotoxicity, toll-like receptors (TLRs,) and cell cycle scores (each P < 0.0001) (Fig. 2C). Second, we compared gene expression between DRTx/suboptimal histology and DRTx/optimal histology. In contrast to the above findings, no significant differences were seen at the levels of differential expression in any individual gene or in pathway scores between DRTx/suboptimal histology and DRTx/optimal histology (Supplementary Fig. 2).
A Volcano plot showing differentially expressed genes between DRTx/suboptimal histology (n = 11) and LRTx (n = 17, which was considered as reference). The 115 genes with significant increased and decreased expression in DRTx/suboptimal histology as compared to LRTx are presented in Supplementary Table 1. B Signature of the 20 assessed immune pathways in LRTx and DRTx/suboptimal histology. C Boxplots for complement, cytotoxicity, toll like receptors, and cell cycle pathway scores, which are the four most significantly altered pathways (all P < 0.0001). Pathway scores were calculated in each biopsy using nSofter Software that take into consideration individual gene expression scores for complement (C1R, C1S, C1QA, C1QB, C2, C4B, C5, C6, C7, C8G, and C9), cytotoxicity [granzyme and perforin associated genes (GZMB, PRF1, GZMA, GZMK) as well as HLA class-I genes (HLA-A, HLA-B, and HLA-C)], TLRs (TLR1-6 and MYD88) and cell cycle (BAX, TNFSF10, BCL2, CASP3, NUP107, THBS1, ABL1, CXCR4, ATM, BIRC5, CCND3, CDKN1A). Other significantly upregulated pathways included leukocyte functions (P = 0.0001), cell functions (P = 0.0001), transporter functions (P = 0.0002), macrophage functions (P = 0.0002), chemokines (P = 0.0003), TNF superfamily (P = 0.0003), cytokines (P = 0.0004), adhesion (P = 0.0005), interleukins (P = 0.0006), and immune regulation (P = 0.0006) (individual boxplots not shown). Remaining pathway scores that did not reach statistical significance according to the Bonferroni cutoff value of P < 0.0025 included B cell function (P = 0.003), T cell function (P = 0.004), NK cell function (P = 0.006), pathogen defense (P = 0.01), and P > 0.1 each of antigen processing and senescence. Pathway scores were compared using Mann–Whitney test. Abbreviations: subop hist: suboptimal histology.
In summary, our pilot analyses of gene expression in time zero biopsy revealed an increase in baseline immunogenicity in DRTx/suboptimal histology compared to LRTx but not to DRTx/optimal histology. Our next step was to assess whether there is any role of donor’s chronic histologic changes in translating increased baseline immunogenicity to acute rejection and worse allograft outcome. To address this, we studied a large cohort of adult kidney allograft recipients grouped according to allograft type and histology at time-zero biopsy.
Part-2: Patient demographic and clinical characteristics
We studied a cohort of 696 consecutive adult kidney transplant recipients (336 LRTx, 166 DRTx/optimal histology, and 194 DRTx/suboptimal histology). In total, patients had a median age of 52 years and included 40% women, 17% self-identified Black, 15% recipients of allografts from Black donors, and a median of four donor-recipient HLA mismatches (Table 1). A small proportion of recipients had pre-formed DSA (16%) or a history of prior transplantation (14%). Diabetes (25%), immune-mediated glomerulonephritis (20%), and hypertension (17%) were the most common causes of native kidney failure. The majority of the patients received induction therapy with Thymoglobulin (79%). In DRTx, median cold ischemia time was 32 h and 28% of donor deaths were attributed to trauma (Table 1).
During a median follow-up of 6 years (IQRs: 2.9, 7.7 years), allograft failure occurred in 168 (24%) recipients at an event rate of 4.5 per 100 person-years follow-up. Approximately a third of the patients (n = 249, 36%) experienced one or more episodes of acute rejection at an event rate of 8.9 per 100 person-years follow-up. Notably, most index biopsies with acute rejection (172/249, 69%) were encountered within the first year of transplantation (early acute rejection episodes).
As seen in Table 1, DRTx/suboptimal histology, DRTx/optimal histology, and LRTx had different demographic and clinical characteristics among recipients and donors.
DRTx/suboptimal histology is associated with increased incidence of acute rejection
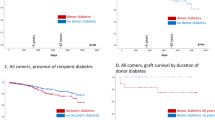
As expected, allograft survival was different amongst the three groups (P < 0.001) (Fig. 3A). DRTx/suboptimal histology had shorter allograft survival than LRTx (P < 0.001) and tended to have shorter allograft survival than DRTx/optimal histology (P = 0.05) (Fig. 3A). Notably, acute rejection episodes (combining TCMR and AMR) were also different amongst the three groups (P = 0.001). DRTx/suboptimal histology had more acute rejection episodes than LRTx (P < 0.001) and tended to have more rejection episodes than DRTx/optimal histology (P = 0.05) (Fig. 3B). When types of acute rejection were dissected further, it became apparent that the difference was more pronounced in TCMR (P = 0.007) (Fig. 3C) while it did not reach statistical significance in AMR (P = 0.38) (Fig. 3D).
A Kaplan–Meier curves for post-transplant cumulative kidney allograft survival [P < 0.001; DRTx/suboptimal histology and DRTx/optimal histology vs. LRTx (each P < 0.001), DRTx/suboptimal histology vs. DRTx/optimal histology (P = 0.05)]. B Acute rejection episodes-free graft survival, combining TCMR and AMR [P = 0.001; DRTx/suboptimal histology vs. LRTx (P < 0.001), DRTx/suboptimal histology vs. DRTx/optimal histology (P = 0.05), DRTx/optimal histology vs. LRTx (P = 0.20)]. C TCMR episodes-free graft survival [P = 0.007; DRTx/suboptimal histology vs. LRTx (P = 0.002), DRTx/suboptimal histology vs. DRTx/optimal histology (P = 0.10), DRTx/optimal histology vs. LRTx (P = 0.27)]. D AMR episodes-free graft survival (P = 0.38).
Next, we attempted to exclude that the observed differences of incidence of acute rejection in “DRTx/suboptimal histology” were not simply a reflection of other confounding clinical and demographic variables. Univariate analyses identified each of “DRTx/suboptimal histology”, recipient’s age, recipient’s female sex, recipient’s Black race, HLA mismatches, pre-transplant DSA, native kidney disease secondary to hypertension, and previous transplantation, as significant predictors for subsequent acute rejection (Table 2). In contrast, thymoglobulin induction therapy was associated with lower incidence of acute rejection. Notably, cold ischemia time or donor’s cause of death, which were only applicable for “DRTx”, did not predict acute rejection. In multivariable analysis, DRTx/suboptimal histology was an independent predictor for acute rejection (HR: 1.34, P = 0.046) (Table 2). Other independent predictors included recipient’s age, recipient’s Black race, HLA mismatches, pre-transplant DSA, native kidney failure secondary to hypertension, and previous transplantation while induction therapy with Thymoglobulin remained a negative predictor for acute rejection.
Early TCMR and AMR independently predict inferior allograft survival in DRTx/suboptimal histology
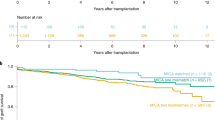
Since the majority of acute rejection episodes occurred in the first year after transplantation and because the first year of transplant is an appropriate period for intervention to prevent acute rejection and improve allograft survival [17], we focused on early acute rejection episodes and on the type of rejection. Amongst the three groups of recipients, DRTx/suboptimal histology had inferior allograft survival after early TCMR compared to LRTx (P = 0.001) and DRTx/optimal histology (P = 0.03) (Fig. 4A). DRTx/suboptimal histology also had inferior allograft survival after early AMR compared to LRTx (P = 0.009) but not to DRTx/optimal histology (P = 0.51) (Fig. 4B).
A Kaplan–Meier curves for kidney graft survival after early TCMR (within 1st year post-transplantation) [P = 0.002; DRTx/suboptimal histology vs. each of LRTx (P = 0.001) and DRTx/optimal histology (P = 0.03); DRTx/optimal histology vs. LRTx (P = 0.57)]. B Kaplan–Meier curves for kidney graft survival after early AMR (within 1st year post-transplantation) [P = 0.02; DRTx/suboptimal histology vs. LRTx (P = 0.009), DRTx/optimal histology vs. LRTx (P = 0.03)] and DRTx/suboptimal histology vs. DRTx/optimal histology (P = 0.51)].
To study the independent association of each of early TCMR and early AMR with allograft failure, we conducted multivariable analyses after adjusting for potentially relevant variables. These included recipient demographics (age, sex, and Black race), donor demographics (age, sex, and Black race), previous transplantation, number of HLA mismatches, presence of pre-transplant DSA, and development of glomerular diseases. As demonstrated in Table 3, each of early TCMR (HR = 2.13, P = 0.005) and early AMR (HR = 4.14, P = 0.001) were independent predictors of allograft failure in “DRTx/suboptimal histology”. While early TCMR could not predict allograft failure in DRTx/optimal histology, early AMR (HR: 2.98, P = 0.03) was an independent predictor of allograft failure in this group. In contrast, neither early TCMR nor early AMR could predict allograft failure in LRTx.
Discussion
While kidney transplantation is the treatment of choice for patients with end-stage renal disease, the number of patients on the waiting list is far in excess for the number of kidneys available for transplantation. Given the increase in demand on donor kidneys, clinicians need to expand the deceased donor organ pool by decreasing the rate of discarded kidneys. However, this strategy is not easily implemented since long term allograft survival is typically worse in DRTx compared to LRTx [6, 7], particularly when DRTx are associated with chronic histologic changes (also referred to as “suboptimal histology”) [8]. This report represents the first clinical attempt to begin to clarify the reasons behind worse long-term allograft survival in DRTx with baseline chronic histologic changes (e.g., “suboptimal histology”). Exploring the reasons for such guarded outcome may open avenues for future development of successful preventive therapies. We hypothesized that the inferior allograft survival in “DRTx with suboptimal histology” is, at least partially, secondary to acute rejection.
Cumulative data from animal models of solid organ transplantation have shown that brain death and ischemia-reperfusion injury stimulate inflammatory cascades that contribute to acute rejection and subsequent allograft failure [18,19,20]. In the transplant setting, transcriptomic technologies are increasingly utilized to study immune responses. Using pre- or post-implantation biopsies of donor kidneys, previous studies have shown that DRTx is associated with upregulation of proinflammatory pathways including complements, proinflammatory cytokines (e.g., IFN-γ, TGF-β1, PDGF-B, IL-2, IL-6, IL-1β) intercellular adhesion molecule (e.g., ICAM)-1, chemokine (e.g., CCR7), and TLR (e.g., TLR4) when compared to LRTx [21,22,23,24,25,26].
The NanoString nCounter is a new platform that utilizes barcode-labeled probe-based methodology to provide direct quantification of gene expression without amplification. A major advantage is its ability to provide robust results using archival FFPE tissue [27, 28]. Nanostring has several predesigned panels including the 770 genes PanCancer Immune Profiling Panel and the newest 758 gene Banff Human Organ Transplant (B-HOT) Panel that was created based on the published list of genes that are associated with post-transplant allograft phenotypes, such as TCMR, AMR, tolerance, drug toxicity, and viral infections [29]. While these panels show significant overlapping (401 genes are shared), B-HOT panel is expected to be superior for post-transplant complications while the traditional PanCancer Immune Profiling Panel may have some advantages when assessing time zero biopsies and non-alloimmune conditions, such as post-transplant glomerulonephritis since it is more enriched in overall immune-related genes.
In this report, we could not find specific genes or immune pathways that were significantly associated with cold ischemia time or subsequent development of acute rejection. In contrast, many genes were upregulated and only 12 genes, including CXCL10 and CXCL12 (SDF-1), were down-regulated in DRTx/suboptimal histology as compared to LRTx. While the expression of CXCL10 and CXCL12 is expected to increase in the transplant setting especially in rejecting allografts, some studies have shown a rapid decrease in their expression directly after reperfusion injury [30, 31]. Compared to LRTx, DRTx/suboptimal histology was associated with significant upregulation of several immune pathways with complement and cytotoxicity pathways being the most strikingly upregulated. In contrast to the above findings, DRTx/suboptimal and DRTx/optimal histology had similar baseline immune gene expression. Taken together, the above findings suggest that DRTx rather than donor histologic changes or cold ischemia time in isolation are the main contributors to gene expression in time zero biopsies.
Following these preliminary studies, we aimed to evaluate the association of donor source and donor chronic histologic changes with subsequent acute rejection and allograft survival. We found that subsequent acute rejection episodes, especially TCMR, are more commonly encountered in DRTx/suboptimal histology compared to LRTx, and, to a lesser extent, to DRTx/optimal histology. In contrast to TCMR, the incidence of AMR was not different amongst the three groups. Multivariable analyses revealed that DRTx/suboptimal histology was a modest but independent predictor for subsequent acute rejection (HR = 1.34, P = 0.046). It is conceivable that chronic histologic changes in DRTx may promote early TCMR by offering increased collagen surface that facilitate adherence of antigen-presenting cells and accumulation of T cells [32].
More remarkable than the increased incidence of acute rejection in DRTx was the strong association of early rejection with poor allograft survival. While survival after early AMR was significantly reduced in each of DRTx/suboptimal histology and DRTx/optimal histology compared to LRTx, allograft survival after early TCMR was significantly decreased in DRTx/suboptimal histology compared to each of LRTX and DRTx/optimal histology. Only in DRTx/suboptimal histology, early TCMR was a strong independent predictors for allograft failure (HR = 2.13, P = 0.005). A prior study that assessed only DRTx has shown that, contrary to interstitial rejection in kidneys from younger donors, interstitial rejection in kidney allografts from donors >50 year-old (who presumably have more chronic changes) adversely affected allograft survival [33]. Taken together, the above findings propose significant detrimental effects of TCMR on allograft survival in patients with baseline chronic histologic changes. Kidneys with chronic histologic changes have lower reserve of healthy parenchyma and impaired capability to tolerate oxidative stress and to repair injury caused by allograft rejection [34,35,36].
An important advantage of the current study is the large and well-characterized cohort of patient with extended follow-up by the same group of clinicians with relatively stable immunosuppressive protocols for the majority of patients. However, we should acknowledge that the results should be interpreted in light of several limitations. These include the retrospective nature of the study and the lack of rigorous monitoring of DSA post-transplantation. An additional limitation includes restricting the assessment of subsequent alloimmune changes to acute rejection episodes. While we acknowledge the importance of assessing chronic rejection features in future studies, we decided to constrain the assessment in this study to acute rejection because it is better defined histologically, and more responsive to therapeutic intervention. Finally, our DRTx was characterized by long cold ischemia time. Thus, the generalizability of these findings will require validation in independent cohorts from different centers.
In summary, we have shown that DRTx/suboptimal histology has increased baseline immunogenicity compared to LRTx but not to DRTx/optimal histology. We have also demonstrated that DRTx/suboptimal histology is associated with modest increase risk of early acute rejection (especially TCMR) but with significantly decreased allograft survival when early TCMR is encountered.
These findings would inform the approach to immunosuppressive management of recipients of organs from deceased donors with chronic histologic changes including the increased use of thymoglobulin for induction therapy and/or steroid maintenance among other approaches, especially in the presence of other variables that can further enhance the risk of acute rejection, such as increased number of HLA mismatches or the presence of pre-transplant DSA. Determination of specific cellular and molecular mechanisms that lead to increased incidence of acute rejection in recipients of DRTx/suboptimal histology offers productive opportunities for future investigations that may potentially lead to improvement of long-term allograft survival in this group of recipients.
Data availability
Access to primary data is not available within the article but can be provided from the corresponding author with reasonable request after approval from Institutional Review Board.
References
Aubert O, Reese PP, Audry B, Bouatou Y, Raynaud M, Viglietti D, et al. Disparities in acceptance of deceased donor kidneys between the United States and France and estimated effects of increased US acceptance. JAMA Intern Med. 2019;179:1365–74.
Husain SA, Chiles MC, Lee S, Pastan SO, Patzer RE, Tanriover B, et al. Characteristics and performance of unilateral kidney transplants from deceased donors. Clin J Am Soc Nephrol. 2018;13:118–27.
Mohan S, Foley K, Chiles MC, Dube GK, Patzer RE, Pastan SO, et al. The weekend effect alters the procurement and discard rates of deceased donor kidneys in the United States. Kidney Int. 2016;90:157–63.
Mohan S, Chiles MC, Patzer RE, Pastan SO, Husain SA, Carpenter DJ, et al. Factors leading to the discard of deceased donor kidneys in the United States. Kidney Int. 2018;94:187–98.
Carpenter D, Husain SA, Brennan C, Batal I, Hall IE, Santoriello D, et al. Procurement biopsies in the evaluation of deceased donor kidneys. Clin J Am Soc Nephrol. 2018;13:1876–85.
Cecka, JM. The OPTN/UNOS renal transplant registry. Clin Transpl., 2005;1–16.
Nemati E, Einollahi B, Lesan Pezeshki M, Porfarziani V, Fattahi MR. Does kidney transplantation with deceased or living donor affect graft survival? Nephrourol Mon. 2014;6:e12182.
Mohan S, Campenot E, Chiles MC, Santoriello D, Bland E, Crew RJ, et al. Association between reperfusion renal allograft biopsy findings and transplant outcomes. J Am Soc Nephrol. 2017;28:3109–17.
Gaston RS. Our evolving understanding of late kidney allograft failure. Curr Opin Organ Transpl. 2011;16:594–9.
Tomfohr J, Lu J, Kepler TB. Pathway level analysis of gene expression using singular value decomposition. BMC Bioinforma. 2005;6:225.
Haeggblom L, Ahrlund-Richter A, Mirzaie L, Farrajota Neves da Silva P, Ursu RG, Ramqvist T, et al. Differences in gene expression between high-grade dysplasia and invasive HPV(+) and HPV(-) tonsillar and base of tongue cancer. Cancer Med. 2019;8:6221–32.
Norton N, Advani PP, Serie DJ, Geiger XJ, Necela BM, Axenfeld BC, et al. Assessment of tumor heterogeneity, as evidenced by gene expression profiles, pathway activation, and gene copy number, in patients with multifocal invasive lobular breast tumors. PLoS One. 2016;11:e0153411.
Racusen LC, Solez K, Colvin RB, Bonsib SM, Castro MC, Cavallo T, et al. The Banff 97 working classification of renal allograft pathology. Kidney Int. 1999;55:713–23.
Loupy A, Haas M, Roufosse C, Naesens M, Adam B, Afrouzian M, et al. The Banff 2019 Kidney Meeting Report (I): Updates on and clarification of criteria for T cell- and antibody-mediated rejection. Am J Transpl. 2020;20:2318–31.
McRae M, Bouchard-Boivin F, Beland S, Noel R, Cote I, Lapointe I, et al. Impact of the current versus the previous diagnostic threshold on the outcome of patients with borderline changes suspicious for T cell-mediated rejection diagnosed on indication biopsies. Transplantation. 2018;102:2120–5.
Dale LA, Brennan C, Batal I, Morris H, Jain NG, Valeri A, et al. Treatment of borderline infiltrates with minimal inflammation in kidney transplant recipients has no effect on allograft or patient outcomes. Clin Transplant. 2020. e14019. https://doi.org/10.1111/ctr.14019.
Cooper JE. Evaluation and treatment of acute rejection in kidney allografts. Clin J Am Soc Nephrol. 2020;15:430–8.
Land WG. Emerging role of innate immunity in organ transplantation part II: potential of damage-associated molecular patterns to generate immunostimulatory dendritic cells. Transpl Rev. 2012;26:73–87.
Nakamura K, Kageyama S, Kupiec-Weglinski JW. Innate immunity in ischemia-reperfusion injury and graft rejection. Curr Opin Organ Transpl. 2019;24:687–93.
Pratschke J, Wilhelm MJ, Kusaka M, Beato F, Milford EL, Hancock WW, et al. Accelerated rejection of renal allografts from brain-dead donors. Ann Surg. 2000;232:263–71.
Yang J, Snijders MLH, Haasnoot GW, van Kooten C, Mallat M, de Fijter JW, et al. Elevated intragraft expression of innate immunity and cell death-related markers is a risk factor for adverse graft outcome. Transpl Immunol. 2018;48:39–46.
uillen-Gomez E, Dasilva I, Silva I, Arce Y, Facundo C, Ars E, et al. Early macrophage infiltration and sustained inflammation in kidneys from deceased donors are associated with long-term renal function. Am J Transpl. 2017;17:733–43.
Kotsch K, Kunert K, Merk V, Reutzel-Selke A, Pascher A, Fritzsche F, et al. Novel markers in zero-hour kidney biopsies indicate graft quality and clinical outcome. Transplantation. 2010;90:958–65.
Naesens M, Li L, Ying L, Sansanwal P, Sigdel TK, Hsieh SC, et al. Expression of complement components differs between kidney allografts from living and deceased donors. J Am Soc Nephrol. 2009;20:1839–51.
Kruger B, Krick S, Dhillon N, Lerner SM, Ames S, Bromberg JS, et al. Donor Toll-like receptor 4 contributes to ischemia and reperfusion injury following human kidney transplantation. Proc Natl Acad Sci USA. 2009;106:3390–5.
Kaminska D, Tyran B, Mazanowska O, Rabczynski J, Szyber P, Patrzalek D, et al. Cytokine gene expression in kidney allograft biopsies after donor brain death and ischemia-reperfusion injury using in situ reverse-transcription polymerase chain reaction analysis. Transplantation. 2007;84:1118–24.
Veldman-Jones MH, Brant R, Rooney C, Geh C, Emery H, Harbron CG, et al. Evaluating robustness and sensitivity of the nanostring technologies ncounter platform to enable multiplexed gene expression analysis of clinical samples. Cancer Res. 2015;75:2587–93.
Balko JM, Cook RS, Vaught DB, Kuba MG, Miller TW, Bhola NE, et al. Profiling of residual breast cancers after neoadjuvant chemotherapy identifies DUSP4 deficiency as a mechanism of drug resistance. Nat Med. 2012;18:1052–9.
Mengel M, Loupy A, Haas M, Roufosse C, Naesens M, Akalin E, et al. Banff 2019 Meeting Report: Molecular diagnostics in solid organ transplantation-Consensus for the Banff Human Organ Transplant (B-HOT) gene panel and open source multicenter validation. Am J Transpl. 2020;20:2305–17.
Zhang W, Zhao J, Cao F, Li S. Regulatory effect of immunosuppressive agents in mice with renal ischemia-reperfusion injury. Exp Ther Med. 2018;16:3584–8.
Moradzadeh K, Nassiri SM, Gheisari Y. Valproic acid restores the down-regulation of SDF-1 following kidney ischemia; experimental validation of a mathematical prediction. Res Pharm Sci. 2020;15:191–9.
Batal I, De Serres SA, Safa K, Bijol V, Ueno T, Onozato ML, et al. Dendritic cells in kidney transplant biopsy samples are associated with T cell infiltration and poor allograft survival. J Am Soc Nephrol. 2015;26:3102–13.
de Fijter JW, Mallat MJ, Doxiadis II, Ringers J, Rosendaal FR, Claas FH, et al. Increased immunogenicity and cause of graft loss of old donor kidneys. J Am Soc Nephrol. 2001;12:1538–46.
Nankivell BJ, Chapman JR. Chronic allograft nephropathy: current concepts and future directions. Transplantation. 2006;81:643–54.
Land WG. Ageing and immunosuppression in kidney transplantation. Exp Clin Transpl. 2004;2:229–37.
Huisman A, Vos I, van Faassen EE, Joles JA, Grone HJ, Martasek P, et al. Anti-inflammatory effects of tetrahydrobiopterin on early rejection in renal allografts: modulation of inducible nitric oxide synthase. FASEB J. 2002;16:1135–7.
Acknowledgements
We thank Maria Lourdes Diaz Belvis, Tao Su, and Xiang Y. Wang at Columbia University Irving Medical Center for their excellent technical assistance and Allison Songstad Ph.D., NanoString Technologies, Inc, Seattle, WA for assisting with data analysis. The work was presented in part as oral presentation at the 2019 USCAP annual meeting (National Harbor, MA).
Funding
IB is supported by a Faculty Development Grant from the American Society of Transplantation (AST) Research Network. MAH is partially supported by NIH/NHLBI T32HL007854-20. SM is supported by NIH (DK114893, DK116066, and MD014161).
Author information
Authors and Affiliations
Contributions
IB, SAH, SMC, and LR performed study concept and design; IB, DJC, VDD, GM, and MAH performed development of methodology, writing, review, and revision of the manuscript; IB, GS, SM, SAH, ERV, RJC, GD, PRS, DS, MBS, and GM provided acquisition, analysis and interpretation of data, and statistical analysis; All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval/consent to participates
This study was approved by the Institutional Review Board and was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Batal, I., Serban, G., Mohan, S. et al. The clinical significance of receiving a kidney allograft from deceased donor with chronic histologic changes. Mod Pathol 34, 1795–1805 (2021). https://doi.org/10.1038/s41379-021-00815-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-021-00815-9