Abstract
Mutations in RAS occur in 30–50% of metastatic colorectal carcinomas (mCRCs) and correlate with resistance to anti-EGFR therapy. Consequently, mCRC biomarker guidelines state RAS mutational testing should be performed when considering EGFR inhibitor treatment. However, a small subset of mCRCs are reported to harbor RAS amplification. In order to elucidate the clinicopathologic features and anti-EGFR treatment response associated with RAS amplification, we retrospectively reviewed a large cohort of mCRC patients that underwent targeted next-generation sequencing and copy number analysis for KRAS, NRAS, HRAS, BRAF, and PIK3CA. Molecular testing was performed on 1286 consecutive mCRC from 1271 patients as part of routine clinical care, and results were correlated with clinicopathologic findings, mismatch repair (MMR) status and follow-up. RAS amplification was detected in 22 (2%) mCRCs and included: KRAS, NRAS, and HRAS for 15, 5, and 2 cases, respectively (6–21 gene copies). Patients with a KRAS-amplified mCRC were more likely to report a history of inflammatory bowel disease (p < 0.001). In contrast, mutations in KRAS were associated with older patient age, right-sided colonic origin, low-grade differentiation, mucinous histology, and MMR proficiency (p ≤ 0.017). Four patients with a KRAS-amplified mCRC and no concomitant RAS/BRAF/PIK3CA mutations received EGFR inhibitor-based therapy, and none demonstrated a clinicoradiographic response. The therapeutic impact of RAS amplification was further evaluated using a separate, multi-institutional cohort of 23 patients. Eight of 23 patients with KRAS-amplified mCRC received anti-EGFR therapy and all 8 patients exhibited disease progression on treatment. Although the number of KRAS-amplified mCRCs is limited, our data suggest the clinicopathologic features associated with mCRC harboring a KRAS amplification are distinct from those associated with a KRAS mutation. However, both alterations seem to confer EGFR inhibitor resistance and, therefore, RAS testing to include copy number analyses may be of consideration in the treatment of mCRC.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the third most common malignancy in the United States and prognosis is highly dependent on the occurrence of distant metastases [1]. Approximately 30% of newly diagnosed CRC patients present with metastatic disease and up to 50% of all CRC patients will develop metastases as the disease progresses [2]. Unfortunately, metastatic CRC (mCRC) is often considered incurable. Historically, mCRC was associated with an overall survival of 6 months. However, with recent progress in therapy, the median overall survival for mCRC patients has improved to 30 months or longer [3].
Combination systemic chemotherapy is the mainstay of mCRC treatment. The National Comprehensive Care Network (NCCN) currently recommends patients receive a first-line regimen to include 5-fluorouracil, oxaliplatin or irinotecan, and a targeted agent to vascular endothelial growth factor or epidermal growth factor receptor (EGFR) [4]. Cetuximab and panitumumab are monoclonal antibodies that target the EGFR extracellular domain and, consequently, inhibit the mitogen-activated protein kinase signaling pathway. Their efficacy has been demonstrated in several phase III clinical trials but restricted to patients whose mCRC is wild-type for mutations in KRAS and NRAS [5,6,7,8,9,10]. To aid in the identification of patients eligible for treatment with EGFR inhibitors, biomarker testing guidelines from the American Society for Clinical Pathology (ASCP), Association for Molecular Pathology (AMP), College of American Pathologists (CAP), and American Society of Clinical Oncology (ASCO) recommend mutational analysis for exons 2, 3, and 4 for KRAS and NRAS [11].
While mutations in KRAS and NRAS occur in 30–50% of mCRCs and are mutually exclusive, a small subset of mCRCs are reported to harbor KRAS amplification [12,13,14,15]. However, little is known regarding patients harboring KRAS-amplified mCRC and treatment response data to anti-EGFR therapy is lacking. Herein, we retrospectively reviewed our clinical and pathologic experience with targeted next-generation sequencing (NGS) for KRAS, NRAS, HRAS, BRAF, and PIK3CA on a consecutive series of 1271 patients with mCRC. The aims of this study were to: (1) identify the prevalence of RAS-amplified mCRC, (2) evaluate the clinicopathologic features of RAS amplification in comparison to RAS mutations, and (3) correlate RAS amplification with treatment response to EGFR inhibitors.
Materials and methods
Study population and design
Study approval was obtained from the University of Pittsburgh Institutional Review Board (IRB# STUDY19110319). Between February 2016 and December 2019, 1286 consecutive mCRC specimens from 1271 patients were prospectively submitted to the Molecular and Genomic Pathology (MGP) Laboratory at the University of Pittsburgh Medical Center (UPMC) for targeted NGS. mCRC was defined as pathologically confirmed distant organ metastases and/or locoregional recurrence. Patients with metastasis to regional lymph nodes without pathologically confirmed distant organ metastases/locoregional recurrence were excluded from this study. The MGP Laboratory is a Clinical Laboratory Improvement Amendments-certified and CAP-accredited laboratory. Colorectal carcinoma specimens were received from 34 hospitals within the UPMC system and other medical institutions within and outside of Pennsylvania, USA. In all cases, molecular testing was performed to at least determine RAS mutational status for oncologic treatment with EGFR inhibitors (e.g., cetuximab and panitumumab). Medical records and pathology slides/reports were reviewed to document patient demographics, clinical presentation and history, primary tumor location, primary tumor histologic subtype and grade (according to the 2019 WHO Classification of Tumours of the Digestive System [16]), mismatch repair (MMR) status and follow-up to include treatment history and response data. Among 1271 patients, available medical records for 70 patients were insufficient to determine a history of Lynch syndrome and inflammatory bowel disease (IBD).
In order to further evaluate the therapeutic effect of RAS amplification in mCRC, a separate multi-institutional cohort was collected from Henry Ford Health System, University of Texas MD Anderson Cancer Center and UPMC. All three medical institutions utilize the OncomineTM Comprehensive Assay v3 for selected stage IV neoplasms according to the manufacturer’s instructions (Thermo Fisher Scientific, Waltham, MA). Molecular testing archives were retrospectively searched for RAS-amplified mCRC at all three institutions. Twenty-three patients were identified, and individual electronic medical records and pathology slides/reports were reviewed similarly to the aforementioned UPMC consecutive cohort of mCRC patients.
Targeted NGS to include copy number analysis
Tumor DNA was isolated from formalin-fixed paraffin-embedded sections of surgical resection, biopsy, and cytopathology fine needle aspirate cell block material. The DNeasey Blood and Tissue kit on the QIAcube instrument (QIAGEN, Germantown, MD) was used for tumor DNA isolation. Extracted DNA was quantitated on the GloMax Discover Plate Reader using the QuantiFluor ONE dsDNA System (Promega, Madison, WI). Amplification-based targeted NGS was performed using custom AmpliSeq primers for hotspot mutations in KRAS, NRAS, HRAS, BRAF, and PIK3CA with primer sequences and performance characteristics as previously described [17, 18]. Of note, coverage for KRAS, NRAS, and HRAS included exons 2, 3, and 4. Amplicons were barcoded, ligated with specific adapters, and purified. DNA library quantity and quality checks were performed using the 4200 TapeStation (Agilent Technologies, Santa Clara, CA). The Ion Chef was used to prepare and enrich templates and enable testing via Ion Sphere Particles on a semiconductor chip. Massive parallel sequencing was carried out on an Ion S5 XL System according to the manufacturer’s instructions (Thermo Fisher Scientific, Waltham, MA) and data were analyzed with the Torrent Suite Software v5.8 (Thermo Fisher Scientific, Waltham, MA) and in-house Variant Explorer (UPMC, Pittsburgh, PA) for point mutations, small insertions/deletions, and copy number alterations. Each variant was prioritized according to the 2017 AMP/ASCO/CAP joint consensus guidelines [19]. Tier I, Tier II, and Tier III variants were reported; however, only Tier I and Tier II variants were used clinically. The limit of detection was at 3% allele frequency (AF). The minimum depth of coverage for testing was ×300; however, the mean coverage attained was ×3225. For each mutation, an AF was calculated based on the number of reads of the mutant allele versus the wild-type allele and reported as a percentage.
Copy number analysis was performed as previously described and validated [20, 21]. The total depth of sequencing coverage for each sequenced region was normalized and calculated per sequenced case. A decrease in sequencing coverage below established cut-offs was considered a copy number loss. In contrast, an increase in sequencing coverage above established cut-offs was interpreted as a copy number gain. A gene amplification was defined by the presence of ≥6 copies of a variant as previously described and previously validated using fluorescence in situ hybridization (FISH) analysis [20]. Of note, the mechanism of gene amplification, such as chromosomal aneuploidy, cannot be determined using this assay. In addition, results of copy number analysis were not reported clinically in accordance with ASCP/AMP/CAP/ASCO biomarker testing guidelines for mCRC [11].
Statistical analysis
Chi-squared analysis or Fisher exact tests were used to compare categorical data, and Mann–Whitney U test was used to compare continuous variables. All statistical analyses were performed using the SPSS Statistical software, version 24 (IBM, Armonk, NY) and statistical significance was defined as a p value of <0.05.
Results
Metastatic colorectal carcinoma study cohort
The clinicopathologic features of the study cohort are summarized in Table 1. Briefly, 1286 consecutive CRC specimens from 1271 patients with distant metastatic/recurrent CRC were prospectively submitted for targeted NGS. At the time of initial cancer diagnosis, the patient age range was 18–99 years (median, 64.0 years; mean, 63.2 years) and there was a female-to-male ratio of 1:1.2. A history of Lynch syndrome and IBD was documented in 10 of 1201 (1%) patients and 23 of 1201 (2%) patients, respectively. Among the 23 patients with an IBD history, 8 patients had Crohn’s disease and 15 patients had ulcerative colitis.
The specimens used for sequencing consisted of 373 (29%) primary CRCs and 913 (71%) distant metastases/recurrences (Supplementary Table 1). Primary CRCs were used for targeted NGS if sufficient tumor from the corresponding metastasis was unavailable at the time of metastatic presentation. Of note, the NCCN guidelines state RAS testing can be performed on either primary or metastatic/recurrent CRCs as both specimen types are reported to have a similar prevalence in RAS mutational status [4, 22]. The site of colonic origin for the tumors was predominantly left-sided (n = 801, 63%) (Supplementary Table 2). The histologic subtypes of the primary tumors included 1060 (83%) conventional adenocarcinomas, 150 (12%) mucinous adenocarcinomas, 37 (3%) signet-ring cell carcinomas, 11 (1%) neuroendocrine carcinomas, 6 micropapillary carcinomas, 3 medullary, 2 adenosquamous/squamous carcinomas, and 2 undifferentiated carcinomas. In addition, most of the primary tumors were histologically graded as well-to-moderately differentiated (n = 1,042, 82%). Results of targeted NGS among 1286 specimens revealed mutations in KRAS, PIK3CA, BRAF, and NRAS for 563 (44%), 170 (13%), 154 (12%), 29 (2%) mCRCs, respectively. Further, one mCRC harbored an HRAS mutation. Except for one mCRC with KRAS and NRAS mutations, mutations in the RAS genes were mutually exclusive with one another. MMR was also evaluated in 1258 (98%) cases with the identification of 100 (8%) MMR deficient-mCRCs.
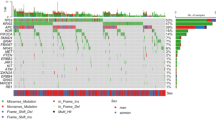
Metastatic colorectal carcinomas with RAS amplification
RAS amplification was detected for 22 (2%) mCRCs and involved KRAS, NRAS, and HRAS for 15, 5, and 2 cases, respectively (Table 2 and Fig. 1). Copy number gains in BRAF and PIK3CA were not identified. Of note, in accordance with mCRC biomarker testing guidelines, RAS amplification results were not reported [11]. Gene amplification ranged from 6 to 21 copies and, among the individual RAS genes, was mutually exclusive with one another. However, this mutually exclusive relationship did not extend between RAS amplification and RAS mutations (p = 0.396). Eight of 22 (36%) RAS-amplified mCRCs harbored mutations in KRAS (n = 7) or NRAS (n = 1). Further, BRAF mutations were found in three RAS-amplified mCRCs. Interestingly, amplification of a RAS gene correlated with a younger median patient age at initial diagnosis (58.0 years vs. 64.0 years, p = 0.042) and a history of IBD (41% [9 of 22] vs. 1% [14 of 1249], p < 0.001). However, upon excluding IBD patients from statistical analysis, the association between RAS amplification and young median age was no longer significant (p = 0.786). Further, there were no statistically significant differences among other clinicopathologic features including site of distant metastasis and/or locoregional recurrence.
Most RAS-amplified mCRC were characterized by histopathologic features of conventional adenocarcinoma (a, Case 1, Table 2), but other histologic subtypes were also identified and included mucinous adenocarcinoma (b, Case 19, Table 2), signet-ring cell carcinoma (c, Case 5, Table 2), and micropapillary carcinoma (d, Case 7, Table 2).
A subanalysis of KRAS status also revealed that patients with a KRAS-amplified mCRC were younger (54.0 years vs. 64.0 years, p = 0.016) and had a history of IBD (60% [9 of 15] vs 1% [14 of 1256], p < 0.001) as compared with patients without a KRAS-amplified mCRC (Table 3). But, after excluding a history of IBD, the association between KRAS amplification and young median age was not statistically significant (p = 0.776). In contrast, KRAS-mutated mCRCs frequently occurred in older patients (65.0 years vs. 63.0 years, p = 0.017), right-sided in origin (42% vs. 33%, p = 0.003), well-to-moderate differentiation (89% vs. 77%, p < 0.001), mucinous histology (17% vs. 7%, p < 0.001) and MMR proficient (96% vs. 89%, p < 0.001) in comparison with KRAS wild-type mCRC. Further, KRAS mutations were essentially mutually exclusive of mutations in NRAS, HRAS, and BRAF (p < 0.001); but, among 170 PIK3CA-mutant mCRCs, 107 (63%) cases harbored a KRAS mutation. Due to the identification of only five NRAS-amplified mCRCs, no statistically significant associations were found (Supplementary Table 3). Mutations in NRAS also did not correlate with any of the evaluated clinicopathologic features.
Follow-up for patients with a RAS-amplified metastatic colorectal carcinoma
Follow-up was available for 20 of 22 RAS-amplified mCRC patients and ranged from 2 to 156 months (median, 16.5 months; mean, 25.2 months). Fourteen of 20 (70%) patients died from disease, and 5 (25%) patients were documented to have received the EGFR inhibitor, panitumumab. Among the five patients treated with panitumumab, other than amplification of KRAS (n = 4) or NRAS (n = 1), no additional genomic alterations were identified. After one cycle of panitumumab-based therapy, the mCRC patient with an NRAS amplification developed a severe grade III skin toxicity necessitating discontinuation of the EGFR inhibitor. The remaining four patients with KRAS-amplified mCRC received a therapeutic regimen that included panitumumab as either first-line or second-line therapy. All four patients demonstrated clinical and radiographic disease progression while on treatment (Fig. 2).
Case 9 (Table 2) was a 60-year-old female with mCRC to the liver (white arrowhead) that failed first line FOLFOX and bevacizumab (a) and continued to progress after 3 months on FOLFIRI and panitumumab (b). Similarly, Case 1 (Table 2) was a 49-year-old male with ulcerative colitis, status post subtotal proctocolectomy, and developed an adenocarcinoma of his rectal cuff (c, white arrowhead). Surgical resection was aborted upon identification of peritoneal carcinomatosis and, thus, the patient received six cycles of FOLFOX and panitumumab. However, the patient’s disease continued to progress within 4 months and resulted in excessive distal colonic stricturing (d).
Treatment data from a multi-institutional cohort of metastatic colorectal carcinomas with RAS amplification
In order to further evaluate the therapeutic impact of RAS amplification in the setting of mCRC, a cohort of RAS-amplified mCRCs without concomitant mutations in KRAS, NRAS, HRAS, BRAF, and PIK3CA were collected from three institutions and identified using the OncomineTM Comprehensive Assay v3 testing platform (Table 4). This cohort consisted of 23 patients ranging in age of 33–81 years (median, 55.0 years; mean, 53.6 years), a female-to-male ratio of 1:1.6 and a history of ulcerative colitis for five (22%) patients. Amplification of RAS included KRAS (n = 21), NRAS (n = 1), and both genes (n = 1) with copy number alterations ranging between 6 and 42 gene copies. Eight mCRC patients with KRAS amplification received cetuximab (n = 6) or panitumumab (n = 2), and all eight patients exhibited clinical and radiographic disease progress while on EGFR inhibitor-based treatment.
Discussion
Effective chemotherapy for mCRC is a key determinant for patient overall survival and is influenced by multiple factors that include clinicoradiographic findings, pathologic features, and molecular biomarkers, such as mutations in the RAS genes when considering anti-EGFR therapy. Consistent with previous studies, the prevalence of a RAS mutation within our mCRC patient cohort was 48% and, except for one case, mutations in the RAS genes were mutually exclusive with one another. In addition, we found 2% of mCRCs harbored a gene amplification in either KRAS, NRAS, or HRAS. None of the RAS-amplified mCRCs had amplification of more than one RAS gene. However, a mutually exclusive relationship between RAS mutations and RAS amplification was not identified.
Likely due to the combination of biomarker guideline recommendations in RAS testing, consequent limitations in testing algorithms and techniques, and its low prevalence, the description of RAS-amplified mCRCs has been restricted to a few publications and is primarily focused on KRAS amplification. Within a study of 1039 cases, Valtorta el al. found 0.7% of mCRCs were KRAS amplified, which was slightly lower than 1% in our patient cohort [12]. While the authors did not assess the status of NRAS or HRAS, they employed a two-tiered immunohistochemical and FISH screen for KRAS overexpression and KRAS amplification, respectively. This screening protocol is similar to what is currently advocated for HER2/neu overexpression and ERBB2 amplification in gastric and gastroesophageal adenocarcinomas [23]. It is, however, important to note that the false negative rate for KRAS immunohistochemistry has not been documented and current mCRC biomarker testing guidelines have not approved its clinical use. To date, the largest published cohort of RAS-amplified mCRCs is by Serebriiskii et al. [13]. The authors retrospectively reviewed Foundation Medicine’s NGS database of 13,336 mCRCs and, consistent with our findings, determined the prevalence of RAS amplification was 2%. However, this database contains minimal clinicopathologic data. Within our cohort, patients with mCRC that harbored a KRAS amplification frequently had a history of IBD. In comparison, mutations in KRAS were associated with older patient age, right-sided colonic origin, low-grade differentiation, mucinous histology, and MMR proficiency. Moreover, considering the lack of mutual exclusivity between KRAS mutation and KRAS amplification, our findings suggest the clinicopathologic features of KRAS-amplified mCRC are different from those of KRAS-mutated mCRC.
Indeed, the relationship between IBD and KRAS-amplified mCRC is intriguing. IBD-associated CRCs are characterized by several clinical, pathologic, and molecular features that contrast those associated with sporadic CRC. For instance, IBD-associated CRCs often occur in young patients [24]. Further, rather than developing from a polypoid adenoma, IBD-associated CRCs frequently arise from flat dysplasia with indistinct margins and a field of inflammation and scarring [25]. Recent genomic studies have also found IBD-associated CRCs are molecularly distinct from their sporadic counterparts. IBD-associated CRCs tend to have a high burden of recurrent chromosomal gains and loss [26, 27]. Interestingly, copy number alterations begin to accrue prior to cancer formation with high-grade dysplastic lesions demonstrating a similar frequency of specific chromosomal gains and losses as matched IBD-associated CRCs, and are distinctly different from sporadic CRCs [26]. Although a defining set of copy number alterations in IBD-associated tumorigenesis has not been elucidated, we found 60% of patients with KRAS-amplified mCRC had a history of IBD. Therefore, our data implicate KRAS amplification in the molecular pathogenesis of IBD-associated CRC.
Besides understanding the clinicopathologic features associated with RAS-amplified mCRC, determining whether amplification of RAS confers resistance to anti-EGFR monoclonal antibodies is critical for patient management. Utilizing preclinical models, Valtorta el al. assessed whether KRAS amplification could affect response to EGFR inhibitors [12]. The authors found the occurrence of KRAS amplification in otherwise anti-EGFR sensitive CRC cell lines dramatically impairs their response to cetuximab. Moreover, silencing of KRAS was able to restore cetuximab sensitivity in the KRAS-amplified NIH-H630 CRC cell line. Prior to our study, the only documented patient with a KRAS-amplified CRC and received anti-EGFR therapy was reported by Mekenkamp et al. [14]. Within a retrospective analysis of the multicenter phase III CAIRO2 trial, a subset of mCRC patients that underwent three cycles of cetuximab-based treatment and either exhibited long or short progression-free survival were evaluated for both KRAS and BRAF status. Among 17 mCRC patients with poor progression-free survival after cetuximab therapy, KRAS amplification was detected in one case. However, no additional patient data were provided regarding clinicopathologic findings or a description of clinical course while on cetuximab. Furthermore, mutational analysis for KRAS was limited to exon 2, and did not include extended RAS testing as recommended by current mCRC biomarker testing guidelines [11]. Considering RAS amplification and RAS mutations are not mutually exclusive, it is uncertain from the authors’ study whether cetuximab resistance was due to the presence of a KRAS amplification, mutations in other KRAS exons, or NRAS and HRAS mutations, which were not evaluated. In contrast, we identified 12 KRAS-amplified mCRCs without additional alterations in KRAS, NRAS, HRAS, BRAF, or PIK3CA, and all 12 exhibited clinicoradiographic resistance to either a cetuximab- or panitumumab-based regimen. While we acknowledge that it is difficult to draw conclusions based on 12 mCRC cases alone, analogous results have been published for other tumor types [28,29,30,31,32,33]. In fact, KRAS-amplified non-small cell lung cancers are well-known to be refractory to anti-EGFR targeted therapies [34]. Altogether, preclinical and clinical evidence points to RAS amplification in mCRC as a potential resistance mechanism for EGFR inhibitors. Thus, it seems prudent to at least consider RAS copy number analysis when determining whether a mCRC patient is a candidate for anti-EGFR therapy.
It is also worth noting that there are a few limitations to our study. It is retrospective by design and although it represents one of the largest series of consecutive mCRCs to be molecularly analyzed for routine patient care, the number of RAS-amplified cases is relatively small. This is, however, to be expected based on the low prevalence of RAS amplification in mCRC. In addition, amplification of the RAS genes was assessed by NGS rather than conventional methods, such as FISH. Classically, FISH has been recognized as the “gold standard” for gene amplification, but NGS is proven to show comparable performance to FISH [20]. NGS testing also permits simultaneous testing of single nucleotide variants, small insertions/deletions, and copy number analysis for KRAS, NRAS, and HRAS at a fraction of the cost to perform FISH for each RAS gene. However, the targeted NGS platform used within this study to evaluate consecutive mCRCs for KRAS, NRAS, HRAS, BRAF, and PIK3CA cannot determine the mechanism of a gene amplification, such as chromosomal aneuploidy. It is also interesting to note that the only NRAS-amplified mCRC patient to receive panitumumab had a severe grade III skin toxicity. An EGFR inhibitor-induced rash has been reported to correlate with improved survival in patients treated with anti-EGFR antibodies [35, 36]. In other words, the presence of these eruptions may predict tumor response. Hence, an NRAS amplification in mCRC may not confer EGFR inhibitor resistance as compared with KRAS-amplified mCRCs. Finally, in the absence of a clinical trial, the true effect of RAS amplification on anti-EGFR therapy remains unknown. The low prevalence of RAS-amplified mCRC will pose a formidable challenge for clinical trial accrual, but the lack of clinical trial data in light of additional studies in other RAS-amplified tumors types should not be a contraindication to modify treatment.
In summary, we report RAS amplification occurs in 2% of mCRC patients and is not mutually exclusive from RAS mutations. Among the RAS genes, KRAS amplification was the most prevalent and frequently found among mCRC patients with a history of IBD. Further, the clinicopathologic features of mCRC associated with KRAS amplification contrasted those associated with KRAS mutations. However, both alterations in mCRC seem to confer resistance to anti-EGFR therapy and, therefore, RAS testing to include copy number analyses may be of consideration in the treatment of mCRC.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34.
Van Cutsem E, Cervantes A, Adam R, Sobrero A, Van Krieken JH, Aderka D, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;27:1386–422.
Lim HJ, Gill S, Speers C, Melosky B, Barnett J, Fitzgerald C, et al. Impact of irinotecan and oxaliplatin on overall survival in patients with metastatic colorectal cancer: a population-based study. J Oncol Pr. 2009;5:153–8.
Benson AB, Venook AP, Al-Hawary MM, Cederquist L, Chen YJ, Ciombor KK, et al. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Colon Cancer, Version 4.2019. 2019. Last access date 1/1/2020. https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf.
Douillard JY, Oliner KS, Siena S, Tabernero J, Burkes R, Barugel M, et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N. Engl J Med. 2013;369:1023–34.
Amado RG, Wolf M, Peeter M, Van Cutsem E, Siena S, Freeman DJ, et al. Wild-type KRAS is required for panitumumab efficacy in patients with metastatic colorectal cancer. J Clin Oncol. 2008;26:1626–34.
Van Cutsem E, Kohne CH, Hitre E, Zaluski J, Chang Chien CR, Makhson A, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N. Engl J Med. 2009;360:1408–17.
Maughan TS, Adams RA, Smith CG, Meade AM, Seymour MT, Wilson RH, et al. Addition of cetuximab to oxaliplatin-based first-line combination chemotherapy for treatment of advanced colorectal cancer: results of the randomised phase 3 MRC COIN trial. Lancet. 2011;377:2103–14.
Lievre A, Bachet JB, Boige V, Cayre A, Le Corre D, Buc E, et al. KRAS mutations as an independent prognostic factor in patients with advanced colorectal cancer treated with cetuximab. J Clin Oncol. 2008;26:374–9.
De Roock W, Claes B, Bernasconi D, De Schutter J, Biesmans B, Fountzilas G, et al. Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol. 2010;11:753–62.
Sepulveda AR, Hamilton SR, Allegra CJ, Grody W, Cushman-Vokoun AM, Funkhouser WK, et al. Molecular biomarkers for the evaluation of colorectal cancer: guideline from the american society for clinical pathology, college of american pathologists, association for molecular pathology, and the american society of clinical oncology. J Clin Oncol. 2017;35:1453–86.
Valtorta E, Misale S, Sartore-Bianchi A, Nagtegaal ID, Paraf F, Lauricella C, et al. KRAS gene amplification in colorectal cancer and impact on response to EGFR-targeted therapy. Int J Cancer. 2013;133:1259–65.
Serebriiskii IG, Connelly C, Frampton G, Newberg J, Cooke M, Miller V, et al. Comprehensive characterization of RAS mutations in colon and rectal cancers in old and young patients. Nat Commun. 2019;10:3722.
Mekenkamp LJ, Tol J, Dijkstra JR, de Krijger I, Vink-Borger ME, van Vliet S, et al. Beyond KRAS mutation status: influence of KRAS copy number status and microRNAs on clinical outcome to cetuximab in metastatic colorectal cancer patients. BMC Cancer. 2012;12:292.
Hartman DJ, Chiosea SI. Colorectal carcinomas, KRAS p.G13D mutant allele-specific imbalance, and anti-epidermal growth factor receptor therapy. Cancer. 2013;119:4366.
Tumours of the Colon and Rectum, In: WHO classification of tumours of the digestive system. 5th edn. Vol. 1. Lyon: International Agency for Research on Cancer; 2019;157–92.
Singhi AD, McGrath K, Brand RE, Khalid A, Zeh HJ, Chennat JS, et al. Preoperative next-generation sequencing of pancreatic cyst fluid is highly accurate in cyst classification and detection of advanced neoplasia. Gut. 2018;67:2131–41.
Singhi AD, Nikiforova MN, Chennat J, Papachristou GI, Khalid A, Rabinovitz M, et al. Integrating next-generation sequencing to endoscopic retrograde cholangiopancreatography (ERCP)-obtained biliary specimens improves the detection and management of patients with malignant bile duct strictures. Gut. 2020;69:52–61.
Li MM, Datto M, Duncavage EJ, Kulkarni S, Lindeman NI, Roy S, et al. Standards and Guidelines for the Interpretation and Reporting of Sequence Variants in Cancer: A Joint Consensus Recommendation of the Association for Molecular Pathology, American Society of Clinical Oncology, and College of American Pathologists. J Mol Diagn. 2017;19:4–23.
Grasso C, Butler T, Rhodes K, Quist M, Neff TL, Moore S, et al. Assessing copy number alterations in targeted, amplicon-based next-generation sequencing data. J Mol Diagn. 2015;17:53–63.
Nikiforova MN, Wald AI, Melan MA, Roy S, Zhong S, Hamilton RL, et al. Targeted next-generation sequencing panel (GlioSeq) provides comprehensive genetic profiling of central nervous system tumors. Neuro Oncol. 2016;18:379–87.
Etienne-Grimaldi MC, Formento JL, Francoual M, Francois E, Formento P, Renee N, et al. K-Ras mutations and treatment outcome in colorectal cancer patients receiving exclusive fluoropyrimidine therapy. Clin Cancer Res. 2008;14:4830–5.
Bartley AN, Washington MK, Colasacco C, Ventura CB, Ismaila N, Benson AB 3rd, et al. HER2 Testing and Clinical Decision Making in Gastroesophageal Adenocarcinoma: Guideline From the College of American Pathologists, American Society for Clinical Pathology, and the American Society of Clinical Oncology. J Clin Oncol. 2017;35:446–64.
Ekbom A, Helmick C, Zack M, Adami HO. Ulcerative colitis and colorectal cancer. A population-based study. N. Engl J Med. 1990;323:1228–33.
Ullman T, Odze R, Farraye FA. Diagnosis and management of dysplasia in patients with ulcerative colitis and Crohn’s disease of the colon. Inflamm Bowel Dis. 2009;15:630–8.
Baker AM, Cross W, Curtius K, Al Bakir I, Choi CR, Davis HL, et al. Evolutionary history of human colitis-associated colorectal cancer. Gut. 2019;68:985–95.
Lai LA, Risques RA, Bronner MP, Rabinovitch PS, Crispin D, Chen R, et al. Pan-colonic field defects are detected by CGH in the colons of UC patients with dysplasia/cancer. Cancer Lett. 2012;320:180–8.
Modrek B, Ge L, Pandita A, Lin E, Mohan S, Yue P, et al. Oncogenic activating mutations are associated with local copy gain. Mol Cancer Res. 2009;7:1244–52.
Poage GM, Christensen BC, Houseman EA, McClean MD, Wiencke JK, Posner MR, et al. Genetic and epigenetic somatic alterations in head and neck squamous cell carcinomas are globally coordinated but not locally targeted. PLoS ONE. 2010;5:e9651.
Sasaki H, Yano M, Fujii Y. Evaluation of Kras gene mutation and copy number in thymic carcinomas and thymomas. J Thorac Oncol. 2010;5:1715–6.
Wagner PL, Stiedl AC, Wilbertz T, Petersen K, Scheble V, Menon R, et al. Frequency and clinicopathologic correlates of KRAS amplification in non-small cell lung carcinoma. Lung Cancer. 2011;74:118–23.
Sasaki H, Hikosaka Y, Kawano O, Moriyama S, Yano M, Fujii Y. Evaluation of Kras gene mutation and copy number gain in non-small cell lung cancer. J Thorac Oncol. 2011;6:15–20.
Hanrahan AJ, Schultz N, Westfal ML, Sakr RA, Giri DD, Scarperi S, et al. Genomic complexity and AKT dependence in serous ovarian cancer. Cancer Discov. 2012;2:56–67.
Ricordel C, Friboulet L, Facchinetti F, Soria JC. Molecular mechanisms of acquired resistance to third-generation EGFR-TKIs in EGFR T790M-mutant lung cancer. Ann Oncol. 2019;30:858.
Abdel-Rahman O, Fouad M. Correlation of cetuximab-induced skin rash and outcomes of solid tumor patients treated with cetuximab: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2015;93:127–35.
Liu HB, Wu Y, Lv TF, Yao YW, Xiao YY, Yuan DM, et al. Skin rash could predict the response to EGFR tyrosine kinase inhibitor and the prognosis for patients with non-small cell lung cancer: a systematic review and meta-analysis. PLoS ONE. 2013;8:e55128.
Acknowledgements
The authors would like to thank Mrs Kate Smith for outstanding administrative assistance. This study was supported in part by the Pittsburgh Liver Research Center (NIH/NIDDK P30DK120531) at the University of Pittsburgh (to ADS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
ADS has received an honorarium from Foundation Medicine, Inc. The remaining authors have disclosed that they have no financial interests, arrangements, affiliations, or commercial interests with the manufacturers of any products discussed in this article or their competitors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Favazza, L.A., Parseghian, C.M., Kaya, C. et al. KRAS amplification in metastatic colon cancer is associated with a history of inflammatory bowel disease and may confer resistance to anti-EGFR therapy. Mod Pathol 33, 1832–1843 (2020). https://doi.org/10.1038/s41379-020-0560-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-0560-x
This article is cited by
-
KRAS mutation as a predictor of insufficient trastuzumab efficacy and poor prognosis in HER2-positive advanced gastric cancer
Journal of Cancer Research and Clinical Oncology (2023)
-
Exome sequencing identifies novel somatic variants in African American esophageal squamous cell carcinoma
Scientific Reports (2021)
-
Antineoplastics
Reactions Weekly (2020)