Abstract
Ocular adnexal sebaceous carcinoma (OASeC) is an aggressive eyelid carcinoma. Analysis of molecular-genetic drivers of this disease could reveal new prognostic markers and actionable targets for treatment. To identify somatically acquired genomic mutations in OASeC and explore their associations with metastasis, whole-exome sequencing on DNA extracted from retrospectively collected tumor samples was performed. Thirty-one patients in two orbital oncology centers with OASeC were included. Sequencing results were analyzed to detect mutations and explore their possible association with metastasis. The median patient age was 64 years. A total of 1780 candidate somatic mutations were identified with median mutation rate of 1.0/Mb (range, 0.2–13.6). The five most commonly mutated genes (as determined by MutSig; q value < 0.25) were TP53 (mutated in 22 cases), ZNF750 (13 cases), RB1 (12 cases), NOTCH1 (8 cases), and PCDH15 (5 cases). Mutations in ZNF750 or NOTCH1 pathway genes were present in 24 (77%) of the 31 cases; there was a trend toward mutual exclusivity of ZNF750 and NOTCH1 mutations. All eight tumors with NOTCH1 mutations also had TP53 and/or RB1 mutations. Four of the five PCDH15 mutations and all four PCDH15 missense mutations were identified in patients with metastatic disease, including one patient with distant metastasis and three with nodal metastasis. PCDH15 was significantly associated with metastasis (P = 0.01). We identified the most commonly mutated genes in a series of OASeCs and found a previously unreported mutation in OASeC, PCDH15 mutation, that was significantly associated with metastasis. NOTCH1 mutation is an actionable mutation; clinical trials targeting this mutation are available throughout the US and could be considered for patients with metastatic NOTCH1-mutant OASeC. TP53, ZNF750, RB1, and PCDH15 mutations are most likely loss-of-function mutations and may have diagnostic and prognostic importance.
Similar content being viewed by others
Introduction
Sebaceous carcinoma (SeC) of the eyelid and conjunctiva, referred to as ocular adnexal SeC (OASeC), is a rare malignancy derived from the epithelium of the sebaceous glands of eyelid, caruncle, conjunctiva, and ocular surface. OASeC has different clinical, histopathologic, and molecular-genetic characteristics than SeC arising in extraocular sites [1,2,3,4,5]. OASeC accounts for 4.7% of eyelid carcinomas in the United States [6,7,8,9,10,11] but has a higher incidence and morbidity in Asian countries [8,9,10,11,12]. OASeC often exhibits aggressive local behavior and has a propensity to metastasize to regional lymph nodes in 21% and to distant organs in 7% of cases according to a recent well-documented report of 100 patients with OASeC [6]. Surgical extirpation of OASeC remains the standard of care for primary tumors but can result in significant morbidity: in a recently reported series of 100 patients with OASeC treated at our center, orbital exenteration was the surgical procedure that was ultimately needed in 14% of cases [6]. Furthermore, effective systemic therapies for patients with metastatic OASeC are lacking. Also lacking are prognostic molecular-genetic biomarkers for this disease.
Previous studies from our center and others have provided a framework by which to begin to understand key molecular-genetic alterations in OASeC [1, 2, 5, 12]. We defined two subtypes of OASeC: (1) OASeCs with TP53 and RB1 mutations, which frequently co-existed in the same tumor, including a subset harboring NOTCH1 mutations, and (2) OASeCs lacking these mutations but exhibiting integration and expression of high-risk human papillomavirus (HPV) RNA [5]. North et al. performed whole-exome sequencing (WES) of 32 SeCs, including nine OASeCs, and identified the mutations previously reported by our group as well as a mutation in ZNF750, a gene locus not assessed in our previous targeted next-generation sequencing platforms [2].
Given that WES identified this additional mutation that was not detected in our previous targeted sequencing studies, we set out to expand on North et al.’s findings by conducting WES in a larger cohort of OASeC samples from patients recruited from two centers, one in the US and the other in China. Our primary objective was to identify previously unreported mutations and mutations that might be associated with metastatic disease and/or be clinically actionable. Our secondary objective was to determine whether there are mutational differences between white and ethnic Chinese patients with OASeC, given the higher incidence of this disease in Asian countries and the scarcity of previous molecular studies in ethnically Chinese or Asian patients.
Materials and methods
Patients and methods
This retrospective case series was performed according to the guidelines of the Declaration of Helsinki. The study included samples from patients at two centers: The University of Texas MD Anderson Cancer Center in Houston, United States, and the Ninth People’s Hospital Shanghai JiaoTong University School of Medicine in Shanghai, China. Ethics approval for this study was obtained at each institution independently.
The pathology databases at the two participating centers were searched to identify patients diagnosed with OASeC from January 27, 2010, through May 11, 2017, for whom adequate residual archived tissue was available for analysis. Patients who had been treated with radiation or topical chemotherapy prior to surgery were excluded.
The patients’ medical records were reviewed, and clinical data were collected. Diagnosis of OASeC was confirmed by two dermatopathologists (MTT and HY). Tissue samples were obtained from 31 patients with OASeC, including 30 samples of primary OASeC (from eyelids) and 5 samples of metastatic lymph nodes. For four patients, paired samples of primary eyelid tumor tissue and lymph node metastases were analyzed. Matched samples of cancer-negative margins from the primary-tumor surgical excision specimen were used as a source of germline reference DNA in all patients.
DNA extraction
Residual surgical excision samples archived in the pathology department at each institution were retrieved. Ten to twenty 4- to 5-μm formalin-fixed, paraffin-embedded (FFPE) sections were prepared from each sample. Hematoxylin and eosin staining was used to confirm the presence of tumor cells in the tissue and to guide microdissection of the unstained slides for DNA extraction. DNA was extracted and purified from the tumor samples and matched normal tissue using the GeneRead DNA FFPE kit (Catalog no. 180134) and Qiagen QIAamp DNA FFPE tissue kit (Qiagen, Hilden, Germany) at the Ninth People’s Hospital and the PicoPure DNA extraction kit (Arcturus, Mountain View, CA, USA) and AMPureXP kit (Agencourt Biosciences, Beverly, MA, USA) at MD Anderson Cancer Center. All kits were used according to the manufacturers’ instructions [1]. The Qubit DNA HS assay kit (Life Technologies, Carlsbad, CA, USA) was used to quantify purified DNA.
Whole-exome sequencing
Whole-exome libraries were created from the DNA libraries using biotin-labeled probeset SeqCap EZ Exome V3 (Roche, Pleasanton, CA, USA). The captured exome libraries were sequenced on an Illumina HiSeq4000 sequencer (Illumina Inc., San Diego, CA, USA). The DNA sequences from both the Ninth People’s Hospital and MD Anderson samples were analyzed using an in-house pipeline that included mapping to the human reference genome Hg19 using BWA and somatic variants calling using VarScan2. Copy number segments were detected using the DNAcopy R package.
Analysis of WES results
Tumor mutation rates were determined by dividing the number of mutations (≥10% allele frequency) by the number of megabases sequenced by the WES platform. Genes with nonsilent mutations in at least 15% of the individuals were included. Significantly mutated genes were determined using MutSigCV_1.41 using default parameters and the exome coverage and gene covariates provided with the software. The contributions of mutational signatures were determined for each tumor sample using the Bioconductor R package deconstructSigs [13] as follows. The trinucleotide context of all single-nucleotide variants (includes silent) with an allelic fraction greater than 0.1 was determined, and a count of each possible 96-trinucleotide context created a mutational pattern for each tumor sample. A multiple linear model of a combination of the 30 COSMIC mutational signatures (https://cancer.sanger.ac.uk/cosmic/signatures) was fit for each sample’s mutational pattern. Hotnet2 [14] was used to identify important mutated genes. Hotnet2 analysis was performed according to software/authors’ recommendations as follows. Cohort mutation frequencies and MutSig results were mapped to interactions networks (hint + hi2012, irefindex9, and multinet) provided with Hotnet2. The average reads for SeC tumor and normal tissues were 131 million (range, 88.6–254.7) and 114 million (range, 42.3–144.43), respectively, with median coverage of tumor 102 (range, 60.6–172.8), and normal 90.5 (range, 26.8–136.8). The median mutation rate was 1.0/Mb (range, 0.2–13.6).
Viral DNA detection
Viral DNA sequences in the tumor next-generation sequencing results were detected using the PathSeq tool [15] from Genome Analysis Toolkit (GATK) 4.1. The unmapped sequencing reads were checked against HPV complete genomes obtained from https://www.ncbi.nlm.nih.gov/genomes/.
Statistical analysis
Patient characteristics were summarized with descriptive statistics. To compare the Ninth People’s Hospital and MD Anderson cohorts with respect to patient demographics, clinical factors, and outcomes, we performed Fisher’s exact tests for categorical variables and Wilcoxon rank-sum tests for continuous variables.
Results
Characteristics of the study cohort
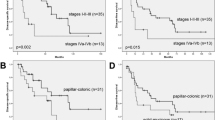
Patients’ demographic and clinical characteristics and outcomes are summarized in Table 1. Of the 31 patients with OASeC included in the study, 17 were from the Ninth People’s Hospital, and 14 were from MD Anderson. The median patient age was 64 years (range, 44–94 years). Eighteen patients were women. Eighteen patients were Asian, eight were white, four were Hispanic, and one was black. The primary tumor arose on the upper lid in 19 patients (61%), lower lid in 5 patients (16%), and both upper and lower eyelids in 7 patients (23%). Twenty-one patients (68%) had highest clinical stage less than IIB according to the 8th edition of the AJCC Cancer Staging Manual (low-risk group), while 10 (32%) had clinical stage IIB or higher (high-risk group). Prognostic stage groups for eyelid carcinoma according to the 8th edition of the AJCC Cancer Staging Manual are described in eTable 1 in the Supplementary. Only one patient from MD Anderson Cancer Center included in this report underwent sentinel lymph node (SLN) biopsy, and the SLN biopsy results in that patient were negative. All cases with metastatic tissue included in our cohort were from MD Anderson, and these all represented clinically or radiologically evident lymph node metastasis; thus an SLN biopsy was not necessary. SLN biopsy was not performed at Ninth People’s Hospital; ultrasonography and computed tomography and/or clinical examination was used for screening for nodal metastasis. None of the patients in this cohort had Muire Torre syndrome.
At the time of surgical excision of the tumor sample analyzed for our study, ten patients (32%) had locally recurrent lesions, and five (16%) had nodal metastasis. The median follow-up time after excision of the sample analyzed for our study was 19.6 months (95% CI, 15.4–23.9 months). During the follow-up period, five patients developed metastasis: two patients developed nodal metastasis only, two patients who previously had nodal metastasis at presentation developed distant metastasis during follow-up, and one patient developed both nodal and distant metastasis during follow-up. Two patients had local recurrence. Six patients died during follow-up, but only two of these deaths were considered to be related to OASeC.
Comparison of the Ninth People’s Hospital and MD Anderson cohorts showed no statistically significant differences in demographic and clinical characteristics or outcomes. Patients from MD Anderson Cancer Center had more advanced final AJCC stage, but this difference did not achieve statistical significance (final stage ≥ IIB, 50% vs 18%; P = 0.121 (see eTable 2 in the Supplementary). There was no difference between the two participating hospitals in the median number of mutations per sample.
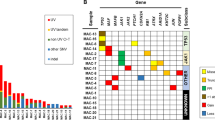
Findings on WES
Examination of WES results from the 35 samples analyzed identified 1780 candidate somatic mutations. The five most commonly mutated genes (as determined by MutSig; q value < 0.25) were TP53, which was mutated in 22 tumors (71%); ZNF750, (which encodes a zinc-finger protein), mutated in 13 tumors (42%); RB1, mutated in 12 tumors (39%); NOTCH1, mutated in 8 tumors (26%); and PCDH15, mutated in 5 tumors (16%) (Fig. 1).
All tumors with NOTCH1 mutation also had TP53 and/or RB1 mutation. Seven of the eight (88%) tumors with NOTCH1 mutation also had TP53 mutation, and 13 of the 15 (87%) tumors with RB1 mutation also had TP53 mutation (Fig. 1).
Given our previously reported finding of two subtypes of OASeC, OASeC with TP53 and RB1 mutations and OASeCs lacking these mutations but expressing high-risk HPV RNA [5], we next examined the transcription level of HPV in samples with mutant NOTCH1, RB1, and TP53 (all three genes mutated) and samples with wild-type versions of these genes. We found that none of the samples with mutant TP53, RB1, and NOTCH1 expressed high-risk HPV, but two of the cases lacking mutations in these genes were positive for HPV—high-risk HPV subtype HPV16 in one case, and alphapapillomavirus 7 in the other. Both patients with HPV expression had advanced AJCC stage (IIB and IV, respectively).
Association between mutated genes and metastasis
We next sought to determine if any genetic alterations identified by WES correlated with a clinically more aggressive phenotype.
We noticed that four of the five PCDH15 mutations and all four PCDH15 missense mutations were identified in tumors from patients who developed metastases, including one patient with distant metastasis and three patients with nodal metastasis. There was a significant association between PCDH15 mutations and metastasis (P = 0.01) (Fig. 1).
We further compared mutations in the primary tumor and nodal metastases in the four patients who had paired primary tumor and lymph node metastasis samples available. All four of these patients had PCDH15 missense mutations. PCDH15 was mutated in both the primary tumor and nodal metastasis in two patients, only in the primary tumor in one patient, and only in the nodal metastasis in the other patient (Fig. 2). In three of the four matched pairs, the primary and metastatic samples carried identical mutations affecting TP53; in one matched pair, the primary and metastatic samples carried an identical mutation in RB1; and in one matched pair, the primary and metastatic samples carried an identical mutation in NOTCH1. A single-nucleotide variation in ZNF750 was noted in a lymph node metastasis in one of the matched pairs (Fig. 2).
There were no significant differences in the frequency of TP53, RB1, ZNF750, and NOTCH1 mutations between primary OASeC tumor samples from patients who did and did not develop metastasis during follow-up after excision of the sample analyzed for this study. (P = 0.66, P ≥ 0.99, P = 0.41, and P = 0.40, respectively).
Discussion
The most important finding of our study is the identification of a previously unreported mutation in OASeC, PCDH15, which was present in 16% of the tumors in our cohort. Importantly, PCDH15 mutations correlated with a more aggressive clinical phenotype: 80% of the PCDH15 mutations and 100% of the PCDH15 missense mutations were identified in patients with metastasis. Other significant findings of our study include lack of significant difference in mutational load or types of mutations between the mostly ethnic Chinese patients from Ninth People’s Hospital and the mostly white and non-Asian cohort at MD Anderson (eTable 2).
Our finding of PCDH15 as a previously unreported mutation associated with metastatic OASeC is noteworthy. PCDH15 mutations were detected in 50% (4/8) of cases that produced nodal and/or distant metastasis but only 4% (1/23) of cases that did not produce metastasis (P = 0.01). PCDH15 codes for protocadherin 15, a member of the cadherin superfamily. Expression of other proteins in the protocadherin family has previously been reported to promote brain metastasis in breast and lung cancers [16]. Of clinical relevance, if our finding of an association between PCDH15 mutation and metastasis of OASeC is confirmed in larger studies, it would be important to test for this mutation in primary OASeCs at the time of initial diagnosis to identify patients who may be at higher risk for nodal and distant metastasis and to offer such patients closer surveillance to enable earlier detection and treatment of metastatic disease.
Our current report expands on WES data reported previously for OASeC by adding data for 31 additional patients with this disease. Consistent with most prior WES and targeted sequencing studies, we found that the most frequent somatically acquired mutations in OASeC were mutations in TP53, RB1, ZNF750, and NOTCH1. The majority of our cases (81%) harbored mutations in one of these genes. Another significant new finding in our report was that mutations affecting NOTCH1 (along with other mutations impacting the NOTCH pathway) co-existed with TP53 or RB1 mutations or both but trended toward mutual exclusivity with mutations affecting ZNF750. While somatic mutations affecting ZNF750 and mutations affecting NOTCH1 (and other Notch pathway genes, including DLL1 and CUL1) were relatively mutually exclusive they may not be entirely independent of one another. Only two out of eight cases with NOTCH1 mutations also had coexisting mutations affecting ZNF750, whereas greater than 75% of cases (24 out of 31 patient tumors) harbored either a mutation affecting NOTCH1 or ZNF750 (Figs. 1 and 3).
Of immediate clinical relevance, NOTCH1 may represent a targetable mutation. Clinical trials are currently available with agents targeting cancers with NOTCH1 mutations, and such therapy could prove effective for patients with metastatic OASeC that also carry this mutation.
Three previous reports have described potentially actionable mutations in OASeC. In a series of targeted sequencing studies of OASeCs from MD Anderson [1, 2, 12], we found TP53 and RB1 and NOTCH-family mutations to be critical, early drivers of OASeC carcinogenesis. Further, we delineated two distinct subtypes of OASeC: (1) tumors with TP53 and/or RB1 mutations and (2) tumors lack of TP53 or RB1 mutations but, in half of cases, harboring transcriptionally active high-risk HPV subtypes [5]. Finally, we identified mutations in genes including PTEN, PIK3Ca, and AKT that together resulted in activation of the phosphatidylinositol-4,5-bisphosphate 3-kinase (PI3K) signaling cascade [1]. In a more recent study, North et al. applied WES to 23 nonocular tumors and nine cases of OASeC [2]. Within the OASeC subset, they found mutations in TP53 in six of nine cases, ZNF750 in eight of nine cases, and NOTCH1 in one of nine cases. Although the frequency of TP53 mutations was similar across these previous studies and our current study, the frequency of ZNF750 mutations was slightly higher in the North et al. study (89%; 8/9 samples) than in our current study (42%; 13/31). Although we did not see enrichment in specific histopathologic features of squamous differentiation in our tumors with ZNF750 mutation, since ZNF750 is a crucial squamous cell carcinoma-specific tumor suppressor [17, 18], detection of ZNF750 mutation in OASeC may suggest a possible relationship between SeC and squamous carcinoma and may also in part explain their morphologic similarity in some cases [19]. Additional epigenetic mechanisms may impact ZNF750 protein expression in tumors lacking ZNF750 mutations.
There were some differences between our findings and the findings of North et al. North et al. did not identify any RB1 mutations in any of the nine OASeCs they tested, whereas we identified RB1 mutations in 39% (12/31) of the OASeCs we tested. Furthermore, North et al. found a NOTCH1 mutation in only one of the nine OASeCs they tested, whereas we found a NOTCH1 mutation in 26% (8/31) of our cases. These differences may be due to differences between the studies in tumor stage or to the lack of any metastatic samples in the North et al. study. North et al. did not provide the AJCC stage for the nine OASeC specimens they tested; thus, a direct comparison between our specimens and their OASeC specimens is difficult. Our finding of NOTCH1 mutation in approximately one quarter of patients tested opens the possibility of offering such patients participation in the currently available NOTCH-mutation-targeted clinical trials in case they develop metastatic disease (https://www.clinicaltrials.gov/ct2/show/NCT03740100?term=notch1&rank=3.).
We found evidence of HPV transcription in 2 of 31 cases, high-risk HPV subtype HPV16 in one case and alphapapillomavirus 7 in the other. Both of these were cases of advanced OASeC (stage IIB and IV disease, respectively) lacking TP53, RB1, and NOTCH1 mutations. As noted above, we previously reported two potentially distinct molecular-genetic subtypes of OASeC [5]. The first harbors mutations in TP53 and/or RB1 with concomitant NOTCH family member mutations, arises in older patients, and exhibits higher-grade histologic features; the other molecular subtype arises in younger patients, lacks mutations in TP53, RB1, or NOTCH, and harbors transcriptionally active high-risk HPV. The finding of an additional virus (alphapapillomavirus 7) in a TP53, RB1, NOTCH1 wild-type OASeC case in the current report is in keeping with our previous findings.
None of the patients in this cohort had Muir–Torre syndrome. This is in keeping with previous reports suggesting that ocular SeCs lack an association with defective mismatch repair, and extraocular SeCs arise through somatically acquired defects in mismatch repair [1, 20].
In a study assessing mismatch repair protein expression [20], whereas 42% of benign sebaceous neoplasms were mismatch repair protein deficient within the head and neck region, only 4% of carcinomas were deficient in the head and neck (the vast majority being ocular). In contrast, the same study showed that in extraocular sebaceous tumors, mismatch repair deficiency was observed to be common in both benign and malignant sebaceous tumors.
The current report is one of the largest to date on WES in OASeC. Our results confirm and expand on previous findings using targeted sequencing and WES. We found that mutations in TP53, RB1, ZNF750, NOTCH1, and PCDH15 accounted for 94% of all mutations seen in OASeC. PCDH15 is a newly reported mutation with significant association with metastasis in patients with OASeC.
To our knowledge, PCDH15 is a novel mutation and has not been previously reported in OASeC, and shows a significant association with metastatic SeC. It would be prudent to look for this mutation at the time of initial diagnosis of OASeC to help select patients who are at a high risk of metastasis and may benefit from closer surveillance. It would be nice to develop immunohistochemical tests to use in tumor samples as a surrogate marker for this mutation. Although TP53, RB1, and ZNF750 mutations likely represent loss-of-function tumor suppressor mutations, NOTCH1 mutations are immediately clinically actionable, and patients with such mutations could be offered treatment in clinical trials targeting the NOTCH pathway.
References
Tetzlaff MT, Singh RR, Seviour EG, Curry JL, Hudgens CW, Bell D, et al. Next-generation sequencing identifies high frequency of mutations in potentially clinically actionable genes in sebaceous carcinoma. J Pathol. 2016;240:84–95.
North JP, Golovato J, Vaske CJ, Sanborn JZ, Nguyen A, Wu W, et al. Cell of origin and mutation pattern define three clinically distinct classes of sebaceous carcinoma. Nat Commun. 2018;9:1894.
Singh RS, Grayson W, Redston M, Diwan AH, Warneke CL, McKee PH, et al. Site and tumor type predicts DNA mismatch repair status in cutaneous sebaceous neoplasia. Am J Surg Pathol. 2008;32:936–42.
Shalin SC, Sakharpe A, Lyle S, Lev D, Calonje E, Lazar AJ. p53 staining correlates with tumor type and location in sebaceous neoplasms. Am J Dermatopathol. 2012;34:129–35.
Tetzlaff MT, Curry JL, Ning J, Sagiv O, Kandl TL, Peng B, et al. Distinct biological types of ocular adnexal sebaceous carcinoma: HPV-driven and virus-negative tumors arise through nonoverlapping molecular-genetic alterations. Clin Cancer Res. 2019;25:1280–90.
Sa HS, Rubin ML, Xu S, Ning J, Tetzlaff M, Sagiv O, et al. Prognostic factors for local recurrence, metastasis and survival for sebaceous carcinoma of the eyelid: observations in 100 patients. Br J Ophthalmol. 2019;103:980–4.
Shields JA, Saktanasate J, Lally SE, Carrasco JR, Shields CL. Sebaceous carcinoma of the ocular region: the 2014 Professor Winifred Mao Lecture. Asia Pac J Ophthalmol. 2015;4:221–7.
Husain A, Blumenschein G, Esmaeli B. Treatment and outcomes for metastatic sebaceous cell carcinoma of the eyelid. Int J Dermatol. 2008;47:276–9.
Takamura H, Yamashita H. Clinicopathological analysis of malignant eyelid tumor cases at Yamagata university hospital: statistical comparison of tumor incidence in Japan and in other countries. Jpn J Ophthalmol. 2005;49:349–54.
Jahagirdar SS, Thakre TP, Kale SM, Kulkarni H, Mamtani M. A clinicopathological study of eyelid malignancies from central India. Indian J Ophthalmol. 2007;55:109–12.
Wong CY, Tang RK, Lam RF, Io IY, Yuen CY, Ho JW, et al. Muir–Torre syndrome in a middle-aged Chinese patient with sebaceous carcinoma of the eyelid. Semin Ophthalmol. 2015;30:420–2.
Tetzlaff MT, Curry JL, Yin V, Pattanaprichakul P, Manonukul J, Uiprasertkul M, et al. Distinct pathways in the pathogenesis of sebaceous carcinomas implicated by differentially expressed microRNAs. JAMA Ophthalmol. 2015;133:1109–16.
Rosenthal R, McGranahan N, Herrero J, Taylor BS, Swanton C. DeconstructSigs: delineating mutational processes in single tumors distinguishes DNA repair deficiencies and patterns of carcinoma evolution. Genome Biol. 2016;17:31.
Leiserson MD, Vandin F, Wu HT, Dobson JR, Eldridge JV, Thomas JL, et al. Pan-cancer network analysis identifies combinations of rare somatic mutations across pathways and protein complexes. Nat Genet. 2015;47:106–14.
Kostic AD, Ojesina AI, Pedamallu CS, Jung J, Verhaak RG, Getz G, et al. PathSeq: software to identify or discover microbes by deep sequencing of human tissue. Nat Biotechnol. 2011;29:393–6.
Chen Q, Boire A, Jin X, Valiente M, Er EE, Lopez-Soto A, et al. Carcinoma-astrocyte gap junctions promote brain metastasis by cGAMP transfer. Nature. 2016;533:493–8.
Hazawa M, Lin DC, Handral H, Xu L, Chen Y, Jiang YY, et al. ZNF750 is a lineage-specific tumour suppressor in squamous cell carcinoma. Oncogene. 2017;36:2243–54.
Yang H, Pan L, Xu C, Zhang Y, Li K, Chen S, et al. Overexpression of tumor suppressor gene ZNF750 inhibits oral squamous cell carcinoma metastasis. Oncol Lett. 2017;14:5591–6.
Shields JA, Demirci H, Marr BP, Eagle RC Jr, Shields CL. Sebaceous carcinoma of the eyelids: personal experience with 60 cases. Ophthalmology. 2004;111:2151–7.
Singh RS, Grayson W, Redston M, Diwan AH, Warneke CL, McKee PH, et al. Site and tumor type predicts DNA mismatch repair status in cutaneous sebaceous neoplasia. Am J Surg Pathol. 2008;32:936–42.
Funding
Supported by the National Cancer Institute under award number P30CA016672, which supports the MD Anderson Cancer Center Clinical Trials Support Resource and by the National Natural Science Foundation of China award number 8180270.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Xu, S., Moss, T.J., Laura Rubin, M. et al. Whole-exome sequencing for ocular adnexal sebaceous carcinoma suggests PCDH15 as a novel mutation associated with metastasis. Mod Pathol 33, 1256–1263 (2020). https://doi.org/10.1038/s41379-020-0454-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-0454-y