Abstract
The natural history of ductal carcinoma in situ (DCIS) is highly variable and difficult to predict. Biomarkers are needed to stratify patients with DCIS for adjuvant therapy. We investigated the prognostic and predictive relevance of cell cycle progression (CCP) score in women with DCIS. We measured the expression of 23 genes involved in CCP with quantitative RT-PCR on RNA extracted from formalin-fixed paraffin-embedded tumor samples, and assessed the correlation of a predefined score with histopathologic features and recurrence. The signature was analyzed in a cohort of 909 consecutive DCIS with full histopathological features treated in a single institution. The main outcome measure was ipsilateral breast event (IBE) as first event observed, be it in situ or invasive. Median follow-up time was 8.7 years (IQR 6.5–10.5 years). There were 150 ipsilateral IBEs, 84 (56%) of which were invasive. In the first 5 years of follow-up, the score provided statistically different findings (p = 0.009), with IBE rates of 14.7% (95% CI, 10.4–19.7) for the highest quartile of CCP score (Q4) and 8.7% (95% CI, 6.7–11.0) for the lowest quartiles (Q1–3). The prognostic value for IBEs approached significance also in women treated with mastectomy (adjusted hazard ratio [HR] Q4 vs. Q1–3 = 2.60; 95% CI: 0.96–7.08; P = 0.06). Radiotherapy provided a greater benefit in women with higher CCP score. In addition, Q4 predicted a different risk after tamoxifen depending on menopausal status, with a beneficial trend on IBEs in postmenopausal women (HR 0.30; 95% CI, 0.07–1.39), and an opposite trend in premenopausal women (HR 1.68; 95% CI, 0.38–7.44) (P-interaction = 0.03). The results of this study provide for the first time the evidence that CCP score is a prognostic marker, which, after additional validation, could have an important role in personalizing the management of DCIS.
Similar content being viewed by others
Introduction
Most patients with ductal carcinoma in situ (DCIS) are eligible for breast conservation treatment. The key management decision is whether to add radiotherapy (RT) and/or endocrine therapy to minimize the risk of a subsequent recurrence. The National Comprehensive Cancer Network and the European Society of Medical Oncology guidelines suggest that RT might be omitted in some low risk patients [1, 2]. At variance, the National Institute of Health and Care Excellence guidelines recommend offering RT to all patients with DCIS treated by breast conservative surgery [3]. The data from Surveillance, Epidemiology, and End Results (SEER) indicated that the 20-year mortality of DCIS is only 3.3% without significant benefit from RT [4]. According to our very recent data from the randomized placebo-controlled, phase III TAM-01 clinical trial, treatment with a low dose of tamoxifen (5 mg per day) for 3 years halves the risk of disease recurrence and new disease for women who underwent surgery for breast intraepithelial neoplasia [5]. The goal is now to distinguish subtypes that would have good prognosis without any intervention from those requiring combined radio-hormonal therapy to achieve optimal outcomes yet avoiding overtreatment.
Different approaches to stratify DCIS into prognostic groups have been attempted, including nomograms based on clinical–pathological factors [6], gene expression signatures [7, 8], and proliferation markers [9]. All have shown to correlate with disease recurrence but none of them have identified unequivocally a cohort of patients that does not benefit from adjuvant therapies in terms of local relapses [10].
The study of RNA signatures in invasive breast cancer revealed a common component of cell-cycle-regulated mRNAs containing the major prognostic power of each expression profile [11,12,13]. Since the expression levels of cell cycle progression (CCP) genes measure tumor growth irrespective of the underlying genetic aberrations, these genes might be useful to predict outcomes in DCIS patients. We measured expression of a set of CCP genes in a large series of consecutive patients treated for DCIS in a single institution over a period of 10 years. Using a predefined score, we analyzed the correlation with histopathologic features and tested its prognostic and predictive value on breast cancer recurrence.
Material and methods
DCIS cohort
The study cohort consisted of all consecutive women who underwent primary breast surgery for DCIS at the European Institute of Oncology (IEO) between 1997 and 2007. A dedicated database (the IEO Breast Cancer Database) was developed in order to collect prospectively all relevant clinical data. This is a cohort study reported in accordance with the REMARK criteria (McShane et al. [14]).
Gene expression
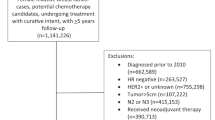
From January 1997 to December 2007, a total of 1023 female patients with DCIS were referred to the interdisciplinary evaluation, and their data were included in the institutional database. After exclusion of cases with insufficient tissue available (n = 31) and poor-quality CCP scores (n = 83), 909 (88.7%) samples were judged valid for statistical analysis.
CCP expression was measured by multiplex quantitative PCR on low density Taqman arrays (TLDA, Thermo Fisher Scientific, Waltham, MA, USA) as described before [15, 16]. Briefly, total RNA was extracted with the RNeasy FFPE kit (Qiagen, Valencia, CA, USA) from macrodissected DCIS tissue and total RNA converted to cDNA by reverse transcription with the High Capacity cDNA Archive kit (Thermo Fisher Scientific) modified by addition of gene-specific primers. Target cDNAs were enriched by 14 cycles of preamplification with pooled Taqman assays before loading of the samples onto custom TLDA cards. Each TLDA card allows analysis of eight samples and contains all CCP and housekeeper genes per sample. Expression data were recorded as threshold cycle values (Ct) at a predefined threshold. All samples were run in duplicate.
The 23 proliferation genes in the CCP score and nine housekeeper genes for normalization are listed in Table 1. Details of the CCP score calculation have been described [15, 16]. At least seven housekeeper genes with evaluable expression data per replicate were required for normalization. Similarly, a minimum of 19 CCP genes with passing expression values were needed to calculate a score. The CCP score is the unweighted average of the CCP gene expression normalized by the average of the housekeeper gene expression. A unit change in the CCP score corresponds to a doubling in the expression level.
Treatment assignments
Treatment assignments were discussed by a multidisciplinary team on a weekly basis. Some differences in treatment selection over the 10-year follow-up period were observed, as previously reported [9]. Women irradiated after nipple sparing mastegctomy received nipple–areola intraoperative RT. Whole breast RT was generally not offered to women with low-grade disease. Furthermore, unless a clinical trial was available, no hormone therapy was routinely recommended to ER-positive DCIS until 2004, after which low-dose tamoxifen (either 10 mg on alternate days or 20 mg once a week) was offered.
Pathology methods
The criteria adopted for the evaluation of DCIS characteristics (histological type, grade, intrinsic subtype, stage, presence of necrosis and microcalcifications, ER, PgR, Ki-67, and Her-2 expression) have been previously described [9]. ER/PgR and Her-2 immunoreactivity were assessed in line with the clinical practice procedures applicable at diagnosis. In line with the St. Gallen recommendations for invasive cancer [17], DCIS were classified as luminal A-like (ER and PgR positive, absence of Her-2 overexpression, and Ki-67 < 14%), luminal B-like (ER and PgR positive, absence of Her-2 overexpression, and Ki-67 ≥ 14%), luminal B-like/Her-2 positive (same as above plus Her-2 3+), Her-2 positive (ER and PgR < 1%, Her-2 3+), and triple negative (ER and PgR < 1% and absence of Her-2 overexpression).
Statistical analysis
Demographic and clinical characteristics of the study sample were analyzed using descriptive statistics. CCP score was considered in the analysis both as continuous and categorical variable based on the distribution quartiles. The correlation between CCP score and Ki-67 was evaluated with Spearman’s correlation coefficient. ANOVA was used to test the association between CCP score and tumor subtype.
The main outcome measure was the ipsilateral breast event (IBE) as first event observed, whether in situ or invasive. The cumulative incidence of IBE was defined as the time from the date of surgery to the date of recurrence. Other first events such as contralateral recurrences, other primary tumors, or deaths for nonbreast related causes were considered as competing risk. In case of no events, the observation was censored at the last follow-up visit. The Gray’s test was used to test the difference in the cumulative incidence of IBE between subgroups of patients. Fine and Gray’s proportional sub-distribution hazard model was used to evaluate the predictive effect of CCP score on IBE. Univariable models and multivariable models, adjusted by age, necrosis, ER, PgR, Her-2 expression, Ki-67, size and grade, overall and by local treatment, were computed.
The added prognostic value of CCP score, beyond that obtained from IHC4, Van Nuys prognostic index (VNPI), and Rudloff’s nomogram, was evaluated using likelihood ratio test, comparing the Fine and Gray’s proportional sub-distribution hazard model with only IHC4 (or VNPI or Rudloff’s nomogram) as covariate with the model including both IHC4 (or VNPI or Rudloff’s nomogram) and CCP score.
All analyses were performed using SAS software v. 9.4 (SAS Institute, Cary, NC, USA).
Results
Association between CCP score and clinical–pathological factors
Table 2 summarizes the main baseline characteristics of the entire cohort. Two hundred and sixty patients (28.6%) were treated with mastectomy and 287 patients of 649 women who underwent quadrantectomy received RT (44.2%). Preventive systemic treatment (low-dose tamoxifen for up to 5 years) was proposed to 711 ER-positive DCIS patients but only 403 women accepted it. Among women treated with mastectomy, 47 received only intraoperative RT, 57 only endocrine treatment, and 36 received both treatments.
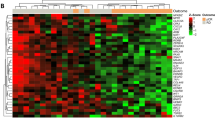
Figure 1a illustrates the correlation and distribution of the CCP score with Ki-67, according to DCIS grade. CCP score and Ki-67 were significantly correlated (Rho = 0.53, p < 0.001), and both increased progressively with cellular anaplasia. Figure 1b shows the relationship between the CCP score and molecular phenotype. As expected, luminal A molecular phenotype had the lowest CCP score (median: −0.6, min: −2.7, max: 1.9). Her-2 phenotype had the highest CCP score (median: +0.6, min: −2.2, max: +3.3), followed by the triple negative, luminal B/Her-2 positive and luminal A/B subtypes (P < 0.001).
Association between CCP score and IBEs
After a median follow up of 8.7 years, 150 IBEs (66 in situ, 84 invasive) were observed. As expected, breast events occurred more frequently in women treated with quadrantectomy (129 events: 60 in situ, 69 invasive), but 21 IBEs occurred in the 260 women treated with mastectomy (6 in situ, 15 invasive), 5 of which received RT, 7 received tamoxifen, and 3 RT + tamoxifen. Contralateral breast cancers were 58 (41 invasive and 17 in situ). In women treated with mastectomy, more than half of recurrences (6/10) were outside the nipple–areola complex.
Overall, the score provided statistically different information in the first 5 years of follow-up (P = 0.009), with IBE rates of 14.7% (95% confidence interval [CI], 10.4–19.7) for the highest quartile of CCP score (Q4) and 8.7% (95% CI, 6.7–11.0) for the lowest quartiles (Q1–3) (Fig. 2a). The prognostic effect of CCP score decreased with increasing follow-up time. Since the indication of local treatment was associated with known prognostic factors (e.g., grading, presence of necrosis) and CCP score was also highly associated with them, the effect of CCP score was evaluated in strata defined by local treatment.
As shown in Fig. 2b, Q4 suggested a possible increased risk of IBE also in patients treated with mastectomy, (HRQ4 vs. Q1–3 = 2.60; 95% CI: 0.96–7.08; P = 0.06; adjusted for age, presence of necrosis, ER, PgR, Her-2 expression, Ki-67, grade, and size).
All women treated with quadrantectomy had a benefit from RT in terms of IBEs (Fig. 3). In the subgroup of patients who underwent quadrantectomy without RT (Fig. 2c, Table 3), CCP score was prognostic, when comparing the Q4 vs. Q1–3 (P = 0.044). CCP score was not prognostic when quadrantectomy was followed by RT (Fig. 2d). CCP score was not predictive of response to tamoxifen overall, but the Q4 suggested a different predictive value depending upon menopausal status, with a beneficial trend on IBEs in postmenopausal women (hazard ratio (HR): 0.30; 95% CI, 0.07–1.39), and an opposite trend in premenopausal women (HR 1.68; 95% CI, 0.38–7.44) (P-interaction = 0.03) (Fig. 4).
Comparison of CCP score with IHC4 score, VNPI, and Rudloff’s nomogram
VNPI was not computable in 342 patients, whereas for Rudloff’s Nomogram data were missing only for 17 patients. Overall, CCP score did not have an additional prognostic value compared with IHC4 (p value LRT = 0.27), VNPI (p value LRT = 0.11), and Rudloff’s nomogram (p value LRT = 0.40). However, within the highest tertile of IHC4 (Fig. 5d) and VNPI (Fig. 6d), and within the medium tertile of the Rudloff’s nomogram (Fig. 7c), Q4 of CCP score identified a subset of patients with a significant higher risk of relapse.
Discussion
Our results showed that CCP score is significantly associated with the risk for IBEs in the first 5 years after diagnosis of DCIS. In addition patients in the highest quartile had a greater benefit to RT and a different response to low-dose tamoxifen according to menopausal status. At the present time, patients and their clinicians may be presented with three choices related to the treatment of DCIS: (i) whether to choose a conservative approach, omitting adjuvant therapy or even surgery in selected patients [18], since recent analyses indicated no significant benefit of RT in terms of breast cancer-associated mortality [4]; (ii) whether to add RT after conservative surgery, given the 40% reduction of local relapse of DCIS and invasive cancers, and discussing individually the risk/benefit ratio of omitting RT in case of low risk DCIS (G1, luminal A, Ki-67 < 14%); and (iii) whether it is beneficial to consider endocrine therapy, including low-dose tamoxifen, since it provides a 50% risk reduction in the ipsilateral and contralateral breast cancer recurrence [5].
Multiple prognostic algorithms have been developed to provide information on residual risk for patients facing these choices, but none of them have identified unequivocally a cohort of patients that does not benefit from adjuvant therapies in terms of local recurrences.
In particular, the Oncotype DX DCIS score has been developed to define a risk of recurrence (prognostic), but not providing information about the effectiveness of RT or endocrine treatment (predictive).
CCP score is an important prognostic factor in prostate cancer [16] and has recently shown to be superior to Ki-67 for predicting outcome after radical prostatectomy [19]. Promising results have been published also in lung cancer patients [15, 20], while very recent data have questioned its role in renal cancer [21]. To date no data on CCP score and invasive breast cancer are available and only one abstract communication investigated its role in DCIS.
In our cohort of DCIS, CCP score performed statistically better with shorter follow-up compared with a longer follow-up. The independent predictive value of Q4 vs. other quartiles was restricted to the first 5 years of follow-up, after which there was no evidence that the score was associated with IBEs (Fig. 2a). Non proportional effects of prognostic scores have been reported in invasive breast cancer, with better prediction for patients at high risk of early relapse rather than for those at risk for later recurrence [22,23,24,25,26]. In particular, two independent analyses [25, 26] confirmed a significant prognostic ability of the risk model IHC4 (combined immunohistochemical assessment of ER, PgR, Her-2, and Ki-67 proteins in the tumor), for early distant recurrence only (0–5 years). In agreement with other authors [22,23,24], possible explanations of this nonproportional effects might be: (i) the biology for the appearance of early and late relapses might be different [27]; (ii) the statistical method (scores are developed on cohorts based on median follow-up); and (iii) the quality of survival data, which might decrease over prolonged follow-up (high level of censoring) [24]. However, a prognostic significance at five years should not be ruled out a priori. For example, very recently the ASCO Clinical Practice Guideline Update supported low-dose tamoxifen as a valid alternative in women with intraepithelial neoplasia [28] based on our previous randomized trial with a median follow-up time of five years [5][].
To our knowledge this is the only study published so far on the role of CCP score in DCIS. In addition, Thorat et al. presented an abstract on 521 cases (134 recurrence events) enrolled in the UK/ANZ DCIS trial, a randomized 2 × 2 factorial trial investigating role of tamoxifen, RT, or both as adjuvant treatment in DCIS [29]. The score was analyzed in tertiles and was not independently associated with the risk of IBEs [29], but the four-arm trial design may have been responsible of a small study size and low power of each single patient group.
In our series, the CCP score seemed to be prognostic also in patients treated with mastectomy. This finding is in line with other publications in invasive breast cancer, where histologic grade has been associated with an increased risk of locoregional recurrence after mastectomy [30, 31]. In our cohort, women irradiated after nipple sparing mastectomy received nipple–areola intraoperative RT. Since more than half of ipsilateral recurrences in this subgroup were outside the nipple–areola complex, we could not assess the value of CCP score in predicting who benefited the most from post mastectomy RT (PMRT). Nevertheless, whether or not to irradiate the chest wall of women after mastectomy for DCIS is a topical issue. Risk factors for local recurrence after mastectomy in DCIS are a gray area and the identification of risk factors for recurrence is mandatory to select suitable candidates for PMRT [32]. In that contest, CCP score, after additional validation, could have a role in the choice of PMRT.
We analyzed not only the prognostic but also a possible predictive value of CCP score in terms of benefit derived from the addition of RT and/or tamoxifen. The highest CCP score DCIS received a greater benefit from RT in terms of ipsilateral breast cancer events. However, DCIS with lower scores also had a mild benefit from RT (Fig. 3). Interestingly, the predictive role of CCP score in terms of tamoxifen benefit differed on the basis of menopausal status. Low-dose tamoxifen protected postmenopausal women with the highest CCP score, whereas premenopausal women with highest CCP score showed a detrimental trend (Fig. 4). Even though this predictive result was obtained in a small subset of patients, thus not allowing to draw any definitive conclusion, this differential effect is in line with the results of our largest cohort [33]. Full-dose tamoxifen is associated with an increase of circulating estrogen in premenopausal women [34]. A hyperestrogenism, combined with a higher proliferating burden hypothesized by the high CCP score DCIS, might explain the detrimental trend observed in this subgroup. Although our findings are not derived from a randomized trial and may contain a selection bias, a phase III trial of low-dose tamoxifen has recently shown that tamoxifen 5 mg/day halves the risk for new and recurrent disease among women with intraepithelial neoplasia [5], providing practice changing results and opening new questions on which subgroup of patients can derive the greatest benefits. We are currently investigating the levels of circulating hormones in the present trial to test the hypothesis that low-dose tamoxifen could be insufficient to compensate the increase of estradiol concentrations due to ovarian stimulation.
Many scores such as IHC4, the VNPI, and nomogram described by Rudloff and colleagues, involve a combination of several clinical and pathologic features to predict local recurrence without requiring tissue or additional testing. Compared with these indices, CCP score did not offer a better predictive ability overall. However, CCP score was able to better discriminate the risk of relapse in specific subgroups of patients. In particular, CCP score was able to better stratify the Rudloff’s nomogram “intermediate” risk category, making the tissue requirement and gene testing worthwhile. Different studies found clinical–pathological indices to have prognostic power, but often to lack utility in advising treatment, as most patients (59–79%) were placed into the “intermediate” grouping [35, 36]. Therefore, one possible strategy to obtain the maximum cost-effectiveness from CCP score could be just resort to it in selected cases (intermediate risk). This approach to patient management could be a step forward to minimize the risk of over or undertreatment of DCIS.
In conclusion, the CCP score was significantly associated with the risk for IBEs in the first 5 years after diagnosis of DCIS and provided further value over conventional clinical factors. CCP score may add insights to patients and clinicians seeking informed decision about optimal management of DCIS.
References
National Comprehensive Cancer Network. Breast cancer version 1.2019. National Comprehensive Cancer Network. 2019. https://www.nccn.org/professionals/physician_gls/pdf/breast_blocks.pdf.
Senkus E, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rutgers E, et al. Primary breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26 Suppl 5:v8–30.
National Institute for Health and Care Excellence (NICE). Early and locally advanced breast cancer: diagnosis and management. National Institute for Health and Care Excellence. 2018. https://www.nice.org.uk/guidance/ng101.
Narod SA, Iqbal J, Giannakeas V, Sopik V, Sun P. Breast cancer mortality after a diagnosis of ductal carcinoma in situ. JAMA Oncol. 2015;1:888–96.
Decensi A, Puntoni M, Guerrieri-Gonzaga A, Caviglia S, Avino F, Cortesi L, et al. Randomized placebo controlled trial of low-dose tamoxifen to prevent local and contralateral recurrence in breast intraepithelial neoplasia. J Clin Oncol. 2019;37:1629–37
Rudloff U, Jacks LM, Goldberg JI, Wynveen CA, Brogi E, Patil S, et al. Nomogram for predicting the risk of local recurrence after breast-conserving surgery for ductal carcinoma in situ. J Clin Oncol. 2010;28:3762–9.
Solin LJ, Gray R, Baehner FL, Butler SM, Hughes LL, Yoshizawa C, et al. A multigene expression assay to predict local recurrence risk for ductal carcinoma in situ of the breast. J Natl Cancer Inst. 2013;105:701–10.
Nofech-Mozes S, Hanna W, Rakovitch E. Molecular evaluation of breast ductal carcinoma in situ with oncotype DX DCIS. Am J Pathol. 2019;189:975–80.
Lazzeroni M, Guerrieri-Gonzaga A, Botteri E, Leonardi MC, Rotmensz N, Serrano D, et al. Tailoring treatment for ductal intraepithelial neoplasia of the breast according to Ki-67 and molecular phenotype. Br J Cancer. 2013;108:1593–601.
Lazzeroni M, Dunn BK, Pruneri G, Jereczek-Fossa BA, Orecchia R, Bonanni B, et al. Adjuvant therapy in patients with ductal carcinoma in situ of the breast: the Pandora’s box. Cancer Treat Rev. 2017;55:1–9.
Mosley JD, Keri RA. Cell cycle correlated genes dictate the prognostic power of breast cancer gene lists. BMC Med Genom. 2008;1:11.
Starmans MH, Krishnapuram B, Steck H, Horlings H, Nuyten DS, van d V, et al. Robust prognostic value of a knowledge-based proliferation signature across large patient microarray studies spanning different cancer types. Br J Cancer. 2008;99:1884–90.
Wirapati P, Sotiriou C, Kunkel S, Farmer P, Pradervand S, Haibe-Kains B, et al. Meta-analysis of gene expression profiles in breast cancer: toward a unified understanding of breast cancer subtyping and prognosis signatures. Breast Cancer Res. 2008;10:R65.
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM. REporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res. Treat. 2006;100:229-235.
Bueno R, Hughes E, Wagner S, Gutin AS, Lanchbury JS, Zheng Y, et al. Validation of a molecular and pathological model for five-year mortality risk in patients with early stage lung adenocarcinoma. J Thorac Oncol. 2015;10:67–73.
Cuzick J, Swanson GP, Fisher G, Brothman AR, Berney DM, Reid JE, et al. Prognostic value of an RNA expression signature derived from cell cycle proliferation genes in patients with prostate cancer: a retrospective study. Lancet Oncol. 2011;12:245–55.
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thurlimann B, Senn HJ. Strategies for subtypes-dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22:1736–47.
Ryser MD, Weaver DL, Zhao F, Worni M, Grimm LJ, Gulati R, et al. Cancer outcomes in DCIS patients without locoregional treatment. J Natl Cancer Inst. 2019;111:952–60.
Leon P, Cancel-Tassin G, Drouin S, Audouin M, Varinot J, Comperat E, et al. Comparison of cell cycle progression score with two immunohistochemical markers (PTEN and Ki-67) for predicting outcome in prostate cancer after radical prostatectomy. World J Urol. 2018;36:1495–1500.
Eguchi T, Kadota K, Chaft J, Evans B, Kidd J, Tan KS, et al. Cell cycle progression score is a marker for five-year lung cancer-specific mortality risk in patients with resected stage I lung adenocarcinoma. Oncotarget. 2016;7:35241–56.
Ueno D, Dancik GM, Shuch B. The cell cycle progression score: unclear role in renal cell carcinoma. Eur Urol. 2018;74:128–9.
Buyse M, Loi S, Van’t Veer L, Viale G, Delorenzi M, Glas AM, et al. Validation and clinical utility of a 70-gene prognostic signature for women with node-negative breast cancer. J Natl Cancer Inst. 2006;98:1183–92.
Desmedt C, Piette F, Loi S, Wang Y, Lallemand F, Haibe-Kains B, et al. Strong time dependence of the 76-gene prognostic signature for node-negative breast cancer patients in the TRANSBIG multicenter independent validation series. Clin Cancer Res. 2007;13:3207–14.
Haibe-Kains B, Desmedt C, Piette F, Buyse M, Cardoso F, Van’t VL, et al. Comparison of prognostic gene expression signatures for breast cancer. BMC Genom. 2008;9:394.
Stephen J, Murray G, Cameron DA, Thomas J, Kunkler IH, Jack W, et al. Time dependence of biomarkers: non-proportional effects of immunohistochemical panels predicting relapse risk in early breast cancer. Br J Cancer. 2014;111:2242–7.
Sgroi DC, Sestak I, Cuzick J, Zhang Y, Schnabel CA, Schroeder B, et al. Prediction of late distant recurrence in patients with oestrogen-receptor-positive breast cancer: a prospective comparison of the breast-cancer index (BCI) assay, 21-gene recurrence score, and IHC4 in the TransATAC study population. Lancet Oncol. 2013;14:1067–76.
Klein CA, Blankenstein TJ, Schmidt-Kittler O, Petronio M, Polzer B, Stoecklein NH, et al. Genetic heterogeneity of single disseminated tumour cells in minimal residual cancer. Lancet. 2002;360:683–9.
Visvanathan K, Fabian CJ, Bantug E, Brewster AM, Davidson NE, Decensi A, et al. Use of endocrine therapy for breast cancer risk reduction: ASCO clinical practice guideline update. J Clin Oncol. 2019;37:3152–65.
Thorat MA, Wagner S, Jones LJ, Levey PM, Bulka K, Hoff R, et al. Prognostic and predictive relevance of cell cycle progression (CCP) score in ductal carcinoma in situ: Results from the UK/ANZ DCIS trial. Cancer Res. 2017;77 Suppl 4 :P1–09-06.
Houghton J, Baum M, Haybittle JL. Role of radiotherapy following total mastectomy in patients with early breast cancer. The Closed Trials Working Party of the CRC Breast Cancer Trials Group. World J Surg. 1994;18:117–22.
O’Rourke S, Galea MH, Morgan D, Euhus D, Pinder S, Ellis IO, et al. Local recurrence after simple mastectomy. Br J Surg. 1994;8:386–9.
Montero-Luis A, Aristei C, Meattini I, Arenas M, Boersma L, Bourgier C, et al. The Assisi Think Tank Meeting Survey of post-mastectomy radiation therapy in ductal carcinoma in situ: suggestions for routine practice. Crit Rev Oncol Hematol. 2019;138:207–13.
Guerrieri-Gonzaga A, Sestak I, Lazzeroni M, Serrano D, Rotmensz N, Cazzaniga M, et al. Benefit of low-dose tamoxifen in a large observational cohort of high risk ER positive breast DCIS. Int J Cancer. 2016;139:2127–34.
Jordan VC, Fritz NF, Langan-Fahey S, Thompson M, Tormey DC. Alteration of endocrine parameters in premenopausal women with breast cancer during long-term adjuvant therapy with tamoxifen as the single agent. J Natl Cancer Inst. 1991;83:1488–91.
Wang SY, Shamliyan T, Virnig BA, Kane R. Tumor characteristics as predictors of local recurrence after treatment of ductal carcinoma in situ: a meta-analysis. Breast Cancer Res Treat. 2011;127:1–14.
Solin LJ, Yeh I, Kurtz J, Fourquet A, Recht A, Kuske R, et al. Ductal carcinoma in situ (intraductal carcinoma) of the breast treated with breast–conserving surgery and definitive irradiation correlation of pathologic parameters with outcome of treatment. Cancer. 1993;71:2532–42.
Acknowledgements
We thank Margherita Omesso for writing assistance and all cohort participants for making this research possible.
Funding
The work was supported by the Italian Ministry of Health (GR-2013-02355967 to ML).
Author information
Authors and Affiliations
Contributions
ML and AD contributed jointly to the study. SW was the supervisor of CCP score and was blinded to patients’ information. EP and VB conducted the data analysis. Data were interpreted by all authors. ML wrote the first draft of the manuscript. All authors read and approved the final manuscript. EP and VB had full access to the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. BB and GV are guarantors of the article. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Conflict of interest
SW is an employee and a stockholder of Myriad Genetics. No potential conflicts of interest were disclosed by the other authors.
Ethical approval and consent to participate
This study was approved by “Comitato Etico degli IRCCS Istituto Europeo di Oncologia e Centro Cardiologico Monzino” (registration number: R 383/16- IEO 399—20.01.2016), and conducted in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lazzeroni, M., DeCensi, A., Guerrieri-Gonzaga, A. et al. Prognostic and predictive value of cell cycle progression (CCP) score in ductal carcinoma in situ of the breast. Mod Pathol 33, 1065–1077 (2020). https://doi.org/10.1038/s41379-020-0452-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-0452-0