Abstract
Pathological risk factors for metastatic disease in patients with testicular non-seminomatous germ cell tumors are debated. The tumor-node-metastasis (TNM) classification eighth edition for testicular cancers includes divergent versions, by the International Union Against Cancer (UICC) and by the American Joint Committee for cancer (AJCC). We investigated pathological predictors of metastatic disease at presentation in 219 non-seminomatous germ cell tumors with reference to both classifications. Age, tumor size, percentage of embryonal carcinoma, lymphovascular invasion, invasion of stromal rete testis, hilar soft tissue, epididymis, spermatic cord, and tunica vaginalis, as well as tumor at spermatic cord margin, were assessed and correlated with clinical stage at presentation. Of the 219 NSGCT cases, 151 (69%) were clinical stage I, 68 (31%) were clinical stage II/III. On univariate analysis, tumor size (P = 0.028), percentage of embryonal carcinoma (P = 0.004), lymphovascular invasion (P = 0.001), stromal rete testis invasion (P = 0.001), hilar soft tissue invasion (P = 0.010), epididymis invasion (P = 0.010), direct spermatic cord invasion (P = 0.001), and tumor at spermatic cord margin ((P = 0.009) were associated with higher clinical stage. On multivariate analysis, lymphovascular invasion (P = 0.003), tumor size (P = 0.005), percentage of embryonal carcinoma (P = 0.005), stromal rete testis invasion (P = 0.008) remained significant. A tumor size of 6 cm and an embryonal carcinoma percentage of 70% were the significant cut-off values. We conclude that in addition to lymphovascular invasion, stromal rete testis invasion, tumor size, and embryonal carcinoma percentage are strong predictors of metastatic disease at presentation and their inclusion should be considered in any future TNM revision. Further, our results support the changes in the AJCC TNM eighth edition as invasion of the epididymis and hilar soft tissue were both univariately significant.
Similar content being viewed by others
Introduction
Testicular germ cell cancer is the most common malignancy in men aged 15-44 years [1], with non-seminomatous germ cell tumors (NSGCTs) diagnosed in 40% of the cases [2]. Approximately 70% of them present a testis-confined disease, clinical stage I, without clinical, serologic, or radiological evidence of metastases [2]. However, up to one-third of these patients have occult metastatic disease at presentation and will relapse after orchiectomy alone [2, 3]. It is crucial then to identify the pathological risk factors that could help to recognize and to accurately treat those patients [4, 5].
Lymphovascular invasion (LVI) is a validated prognostic factor for relapse in clinical stage I NSGCTs [2, 6,7,8,9]. Its presence guides many clinicians in decisions on adjuvant treatment [4, 10,11,12]. However, more uncertainty emerges in regard to the identification of other pathological risk factors, such as the percentage of embryonal carcinoma (EC) and invasion into various paratesticular structures, which may in part be due to controversy regarding the reporting and staging of testicular tumors [13].
Prior to the eighth edition of the American Joint Committee for cancer (AJCC) Tumor-Node-Metastasis (TNM) [10, 14] staging system, one of the disagreements between pathologists was the staging of epididymal and hilar soft tissue invasion without lymphovascular invasion. This was clearly highlighted by the results of a survey developed by the European Network of Uro-Pathology (ENUP) [11]. For instance, hilar soft tissue invasion was staged as pT1, pT2, or pT3 by different pathologists. This discrepancy is an example of how an inaccurate or misleading staging could affect both multicenter studies and even decisions of adjuvant therapy. The results of the survey have been taken into account by the AJCC TNM staging eighth edition [10, 14]: both hilar soft tissue invasion and epididymal invasion have been upstaged to pT2. Tumor size has been included in the classification for pure seminoma: pT1 is substaged as pT1a (<3 cm) and pT1b (≥3 cm). However, no size evaluations are included in the staging of NSGCTs. None of these changes have been adopted by the Union for International Cancer Control (UICC) TNM eighth edition [12], which is the same as the seventh edition. Hence, epididymis invasion is still staged as pT1, the staging of hilar soft tissue invasion is unclear and tumor size is also not included. Therefore, we wished to identify pathological predictors of higher clinical stage with reference to both AJCC and UICC TNM staging eighth edition classifications, aiming to investigate and to clarify which staging method is more helpful in predicting metastatic disease at presentation in NSGCTs.
Materials and methods
Pathologic and clinical data
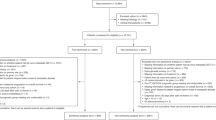
Barts Health NHS Trust Database was searched from January 2007 to December 2017. Anonymized pathological reports were collected from all patients treated at Barts Health NHS Trust and from our supraregional network for cases referred in for review. The Systematized Nomenclature of Medicine Clinical Terms (SNOMED CT) and various text search terms were used for data retrieval and to search for the anatomical sites, surgical procedures, and final histological diagnosis. In total, 275 pathological reports were found for NSGCTs; of them, 219 were selected because of complete pathological and clinical information available. The pathology reports were reviewed by two genitourinary expert pathologists (DB and LB) both of whom had diagnosed or reassessed the cases at presentation. The following pathological features were initially recorded without knowledge of the clinical stage: the percentage of embryonal carcinoma, tumor size (maximum tumor diameter recorded macroscopically), lymphovascular invasion, stromal rete testis invasion (pagetoid invasion is not routinely assessed as it probably represents spread from GCNIS), invasion of hilar soft tissue, epididymis, spermatic cord, and tunica vaginalis as well as tumor at the spermatic cord margin. Stromal rete testis invasion versus pagetoid involvement was specifically recorded (Fig. 1). Age and clinical data were obtained from medical records. Patients were deemed to have clinical stage I disease if their post-operative serum tumor markers were normal and there was no evidence of metastases on a computer tomography (CT) scan of chest, abdomen, and pelvis. Patients with metastatic disease (clinical stage II/III) went on to receive chemotherapy.
Ethical approval was obtained by Local Ethics Committee (REC No: 09/H0704/4+5) for the use of anonymized data from Barts Health NHS Trust.
Statistical analysis
An independent t-test was used to compare the means of two of the continuous variables, age and tumor size, normally distributed, between patients with clinical stage I and clinical stage II/III. Median was also calculated for tumor size. Embryonal carcinoma was considered both as a continuous and categorical variable. As continuous, the recorded percentage was recorded and median was calculated because of a skewed distribution; the median percentages of the clinical stage I and clinical stage II/III were then compared using Mann–Whitney. Binary categorical variables (presence of embryonal carcinoma, lymphovascular invasion, invasion of rete testis both pagetoid and stromal, hilar soft tissue, epididymis, spermatic cord, and tunica vaginalis as well as tumor at spermatic margin) were collected for clinical stage I and clinical stage II/III; frequencies and proportions were assessed. Univariate and multivariate analyses were performed to compare clinical stage I versus clinical stage II/III in relation to the pathological variables. Univariate analysis was performed using Fisher’s exact test of independence. Logistic regression was performed in a forward stepwise model. The stability of the model was measured by a received operating curve (ROC) to assess the performance of the significant variables involved in the prediction of metastatic disease. Odds ratio (OR) and its 95% confidence interval (CI) were calculated for each pathological variable. Fisher’s exact test of independence was also used to evaluate the optimal tumor size cut-off (3, 4, 5, 6 cm) and percentage of embryonal carcinoma cut-off (60%, 70%) to determine higher clinical stage. P < 0.05 was set to be statistically significant for all tests. All statistical analyses were completed using SPSS version 24 software (SPSS Inc, IBM Corp).
Results
Clinical findings
Of the 219 cases, 151 cases (69%) were clinical stage I and 68 (31%) were clinical stage II/III (Table 1).
Pathologic findings
Of the 219 cases, lymphovascular invasion was found in 115/219 (52.5%), stromal rete testis invasion 70/219 (32%), pagetoid rete testis invasion 15/219 (7%), hilar fat invasion 12/219 (5%), epididymis invasion 12/219 (5%), direct spermatic cord invasion 9/219 (4%), tumor at spermatic cord margins 4/219 (2%), and tunica vaginalis 6/219 (3%). The clinical and pathological features in patients with clinical stage I disease versus clinical stage II and III are compared in Table 1.
Thirty-six cases (16%) had pure histology and 183 (84%) cases showed a mixed component; 105 (57%) included a seminomatous component (Table 2).
On univariate analysis, the parameters significantly associated with higher clinical stage were: tumor size (P = 0.028), percentage of embryonal carcinoma (P = 0.004), lymphovascular invasion (P = 0.001), stromal rete testis invasion (P = 0.001), hilar soft tissue invasion (P = 0.010), epididymis invasion (P = 0.010), direct spermatic cord invasion (P = 0.001), and tumor at spermatic cord margin (P = 0.009). However, on multivariate analysis, lymphovascular invasion (P = 0.003), tumor size (P = 0.005), percentage of embryonal carcinoma (P = 0.005), and stromal rete testis invasion (P = 0.008) were significant (Table 3).
A logistic regression model using the four variables has been tested and it is represented by the ROC curve, with an area under the curve (AUC) of 0.757 (Fig. 2).
A tumor size of 6 cm was defined as optimal cut-off (P = 0.03) to predict higher clinical stage (Table 4). The optimal percentage of embryonal carcinoma cut-off point to predict higher clinical stage was 70% (P = 0.020) (Table 5).
Discussion
In the present study, we identified lymphovascular invasion, tumor size, percentage of embryonal carcinoma, and stromal rete testis invasion as strong predictors of metastatic disease at presentation in patients with NSGCTs. We found that the optimal cut-off values to predict metastatic disease at presentation were 6 cm and 70%, respectively, for tumor size and percentage of embryonal carcinoma. Additionally, although only significant in the univariate analysis, our data support the upstaging of epididymis invasion and hilar soft tissue invasion as pT2 in the AJCC TNM eighth edition classification.
Despite much effort in the last four decades in identifying pathological risk factors for metastatic disease in NSGCTs, these are still debated, as clearly shown in the differences reported in the two TNM classifications, AJCC and the UICC TNM staging eighth editions. So far, only lymphovascular invasion is considered a consistent predictor of metastatic disease and relapse in NSGCT as shown in the EAU [15], NCCN [16], ESMO [17] guidelines, confirmed in the literature [18,19,20] and further in our study. Its presence highly influences the treatment decision toward chemotherapy, rather than surveillance as the patients are diagnosed as high risk of relapse. However, clinicians cannot only be led by this single parameter, because it will increase the chances of overtreatment, considering also the fact that sometimes lymphovascular invasion is reported as uncertain feature [21]. Daugaard et al. [2] shown that there is a 5-year relapse rate of 18% if lymphovascular invasion is the only pathological variable involved, while there is an increase of 50% when there is a combination of lymphovascular invasion, rete testis invasion, and presence of embryonal carcinoma; without these risk factors, the relapse rate was 12%. Our study focused on a further selection and identification of specific pathological risk factors involved in the prediction of metastatic disease and/or relapse, to help clinicians, who have to weigh pros and cons of treatments, to both minimize relapse rate and to avoid unnecessary overtreatment and toxicities in these young patients with a long life expectancy. A list of previous studies reporting on histopathological risk factors of relapse in patients with clinical stage I in NSGCTs is summarized in Table 6.
Although it is well known that embryonal carcinoma is considered a risk factor of relapse [15, 17, 22], one of the main concerns in its evaluation is whether to assess it as a percentage or a dichotomous variable (absent/present). In a recent systematic review and meta-analysis, Blok et al. [18] have evaluated the role of embryonal carcinoma in relapse, in patients diagnosed with clinical stage I NSGCT. They showed that the ORs for the presence and percentage of embryonal carcinoma are similar in the risk of occult metastatic disease, concluding that only the presence of embryonal carcinoma is sufficient to identify patients at high-risk. However, in our study, when embryonal carcinoma was considered a dichotomous variable, no significant differences were identified between clinical stage I and clinical stage II/III. Only the percentage of embryonal carcinoma was a significant predictor of higher clinical stage and the best percentage cut-off was ≥70%. This percentage is in line with the cut-off range suggested in previous studies, which varies between 50 and 100% component in mixed tumors [2, 23,24,25,26,27].
Differently from seminomas, where tumor size is a well-known prognostic factor for metastatic disease and it is also included in AJCC TNM eighth edition, there are discordant opinions regarding its involvement in metastatic disease for NSGCTs. Gumus et al. [28] have found that in a cohort of 201 clinical stage I NSGCTs, undergoing both on surveillance or adjuvant treatment, tumor size, percentage of embryonal carcinoma, and treatment options were independent factors for relapse on multivariate analysis. The significant tumor size cut-off was 4 cm. Roeleveld et al. [29] also found an association of tumor size with relapse. The cut-off value found significant in this case was 5 cm. However, several other studies have not shown significant correlation [19, 23, 30,31,32,33]. In our cohort, tumor size was a significant predictor of higher stage in both univariate and multivariate analyses but the definition of an accurate and reliable cut-off has not been found. As the NSGCTs are known to be more aggressive than seminoma, and although tumor size seems to cover an important role in affecting the clinical stage, the uncertainty of a specific cut-off requires further studies to clarify the matter, prospectively and in untreated series [34].
There is limited information in regard to rete testis invasion as a risk factor of metastatic disease in NSGCTs. Yilmaz et al. [19] have identified stromal spread into rete testis as risk factor in metastatic disease at presentation, in both univariate and multivariate analyses in a cohort of 148 NSGCTs cases. The involvement of rete testis invasion, in combination with other factors such as testis histology, clinical symptoms, tumor length, lymphovascular invasion, and level of enzymes as lactate dehydrogenase (LDH), β-Human chorionic gonadotropin (β-hCG), alpha-fetoprotein (AFP), and follicle-stimulating hormone (FSH) in metastatic NSGCTs was found also by Ruf et al. [35]. Our results support these findings. We have recorded and assessed the role of the stromal rete testis invasion to the clinical stage. Analysis showed that stromal rete testis invasion is a strong significant variable involved in the prediction of higher clinical stage. However, rete testis invasion in the AJCC TNM and UICC staging eighth edition is still considered as pT1. This can be explained by the fact that there is insufficient evidence to upstage it. One of the possible reasons for this is that there has not been a clear distinction between pagetoid and stromal spread in the previous studies, especially when the data have been collected from numerous centers and not centrally validated. Further prospective studies should be conducted to better understand the role, with particular regard to distinguish pagetoid from stromal invasion [36].
Invasion of hilar soft tissue soft tissue and epididymis were significant in our cohort on univariate analysis only. The role of both variables in clinical stage I has not been really well investigated previously but both have been upstaged as pT2 in the AJCC TNM eighth edition. One of the first studies to consider the prognostic role of hilar fat invasion in metastatic disease by Yimaz et al. [19] indicated that hilar soft tissue invasion was strongly associated with metastatic disease at presentation on multivariate analysis but it has not been specified whether there is association with the risk of relapse in clinical stage I. Because epididymis and hilar soft tissue are both anatomically connected and tumors usually cannot invade epididymis without also invading hilar soft tissue, the epididymis invasion has also been upstaged to pT2 under the AJCC eighth edition [37]. Further, all of these factors are intimately associated with tumor size. However, despite the fact that both variables represent a potential risk factor and that have been just recently upstaged in the main guidelines, more studies are required to clarify the role of prognastic risk factors, especially in view of the AJCC eighth edition [21].
In our cohort, direct spermatic cord invasion was univariately significant in prediction of higher clinical stage, confirming previous results by Yilmaz et al. [19]. Moreover, Sanfrancesco et al. [38] showed that spermatic cord invasion was more frequently found in clinical stage II/III disease compared with clinical stage I. However, evidences demonstrating the involvement of spermatic cord invasion in predicting higher clinical stage are limited. Tumor at spermatic cord margins was not significantly associated with higher clinical stage. It is a rare event and no further studies have assessed it before.
Tunica vaginalis invasion is still considered pT2 in both the UICC and AJCC TNM eighth editions. In our study, it was not significantly associated with higher clinical stage or relapse. This further emphasizes the lack of critical thought in the UICC eighth edition TNM classification, which includes as T2 factors with no evidence of higher risk disease while excluding others where good evidence exists.
Limitations to this study include the fact that although slides were centrally reviewed, the specimens were grossed in a number of institutions leading to possible variability. In our experience, however, most of the errors in reporting by community pathologists are those of slide interpretation. In the UK, the Royal College of Pathologists provides clear grossing criteria for testicular tumors. However, as the reports on the associations of soft tissue invasion were not well reported at the time that the earliest cases of this cohort were reported, and the fact that some were grossed in district general hospital settings, it is possible that that this is an underestimate of soft tissue invasion in this cohort.
We recognize that some of the proposed risk factors may be prone to intra-observer variation. This is seen in a number of studies where re-review of germ cell tumors has found a significant error rate when tumors are reviewed by experienced pathologists [39], and also the previous survey result which showed differences in interpretation of findings [11]. The AJCC eighth edition has made considerable efforts to standardize some criteria such as the definition of cord invasion to minimize this. Also recent guidance by ESMO has suggested that where possible, germ cell pathology should be reviewed by experts who see a sufficient number of cases [17, 40].
One of the limitations of previous studies has been the fact that they refer to old data not reviewed according to the AJCC TNM eighth edition. Moreover, the vast majority of studies, including our own, use either pathological surrogates for outcomes and non-standardized treatments.
In conclusion, while the pTNM classification should help clinicians to better understand diagnosis and to treat patients accurately, instead the presence of the two separate TNM classification systems, AJCC and UICC eighth with their significant discrepancies, generates uncertainty. In regard to the role of the tumor size and the cut-off, we recommend more prospective studies for a better understanding, in relation also to the new AJCC eighth edition staging. Moreover, considering that NSGCTs and seminomas have different risk factors, including the embryonal carcinoma and as shown in our previous study in seminoma [41], we continue to advocate a separate TNM classification for pure seminomas and mixed germ cell tumors. We suggest also the inclusion of embryonal carcinoma for NSGCTs in any further TNM classification. We would like also to highlight the absolute importance of developing and implementing one unified TNM classification to guarantee a worldwide, standard and uniform staging system.
References
Trabert B, Chen J, Devesa SS, Bray F, McGlynn KA. International patterns and trends in testicular cancer incidence, overall and by histologic subtype, 1973-2007. Andrology. 2015;3:4–12.
Daugaard G, Gundgaard MG, Mortensen MS, Agerbaek M, Holm NV, Rorth M, et al. Surveillance for stage I nonseminoma testicular cancer: outcomes and long-term follow-up in a population-based cohort. J Clin Oncol. 2014;32:3817–23.
Nayan M, Jewett MA, Hosni A, Anson-Cartwright L, Bedard PL, Moore M, et al. Conditional risk of relapse in surveillance for clinical stage I testicular cancer. Eur Urol. 2017;71:120–7.
Warde P, Specht L, Horwich A, Oliver T, Panzarella T, Gospodarowicz M, et al. Prognostic factors for relapse in stage I seminoma managed by surveillance: a pooled analysis. J Clin Oncol. 2002;20:4448–52.
Trevino KE, Esmaeili-Shandiz A, Saeed O, Xu H, Ulbright TM, Idrees MT. Pathological risk factors for higher clinical stage in testicular seminomas. Histopathology. 2018;73:741–7.
Feldman DR. Treatment options for stage i nonseminoma. J Clin Oncol. 2014;32:3797–800.
Sturgeon JF, Moore MJ, Kakiashvili DM, Duran I, Anson-Cartwright LC, Berthold DR, et al. Non-risk-adapted surveillance in clinical stage I nonseminomatous germ cell tumors: the Princess Margaret Hospital’s experience. Eur Urol. 2011;59:556–62.
Alexandre J, Fizazi K, Mahe C, Culine S, Droz JP, Theodore C, et al. Stage I non-seminomatous germ-cell tumours of the testis: identification of a subgroup of patients with a very low risk of relapse. Eur J Cancer. 2001;37:576–82.
Gels ME, Hoekstra HJ, Sleijfer DT, Marrink J, de Bruijn HW, Molenaar WM, et al. Detection of recurrence in patients with clinical stage I nonseminomatous testicular germ cell tumors and consequences for further follow-up: a single-center 10-year experience. J Clin Oncol. 1995;13:1188–94.
Paner GP, Stadler WM, Hansel DE, Montironi R, Lin DW, Amin MB. Updates in the eighth edition of the tumor-node-metastasis staging classification for urologic cancers. Eur Urol. 2018;73:560–9.
Berney DM, Algaba F, Amin M, Delahunt B, Comperat E, Epstein JI, et al. Handling and reporting of orchidectomy specimens with testicular cancer: areas of consensus and variation among 25 experts and 225 European pathologists. Histopathology. 2015;67:313–24.
James DB, Mary KG, Christian W. TNM classification of malignant tumours. 8th ed. Wiley Blackwell, 2017.
Delahunt B, Egevad L, Samaratunga H, Varma M, Verrill C, Cheville J, et al. UICC drops the ball in the 8th edition TNM staging of urological cancers. Histopathology. 2017;71:5–11.
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The Eighth Edition AJCC Cancer Staging Manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67:93–9.
Albers P, Albrecht W, Algaba F, Bokemeyer C, Cohn-Cedermark G, Fizazi K, et al. Guidelines on testicular cancer: 2015 Update. Eur Urol. 2015;68:1054–68.
Motzer RJ, Jonasch E, Agarwal N, Beard C, Bhayani S, Bolger GB, et al. Testicular cancer, version 2.2015. J Natl Compr Canc Netw. 2015;13:772–99.
Honecker F, Aparicio J, Berney D, Beyer J, Bokemeyer C, Cathomas R, et al. ESMO Consensus Conference on testicular germ cell cancer: diagnosis, treatment and follow-up. Ann Oncol. 2018;29:1658–86.
Blok JM, Pluim I, Daugaard G, Wagner T, Jozwiak K, Wilthagen EA, et al. Lymphovascular invasion and presence of embryonal carcinoma as risk factors for occult metastatic disease in clinical stage I nonseminomatous germ cell tumour: a systematic review and meta-analysis. BJU Int. 2019;125:355–68.
Yilmaz A, Cheng T, Zhang J, Trpkov K. Testicular hilum and vascular invasion predict advanced clinical stage in nonseminomatous germ. cell tumors. Mod Pathol. 2013;26:579–86.
Vergouwe Y, Steyerberg EW, Eijkemans MJ, Albers P, Habbema JD. Predictors of occult metastasis in clinical stage I nonseminoma: a systematic review. J Clin Oncol. 2003;21:4092–9.
Berney D, Verrill C. Standards and datasets for reporting cancers. Dataset for histopathological reporting of testicular neoplasms. 2020. https://www.rcpath.org/uploads/assets/6c10e277-2d7f-4e2a-b2db6d424cb0825a/G046-Dataset-for-the-histopathological-reporting-of-testicular-neoplasms.pdf.
Albers P, Siener R, Kliesch S, Weissbach L, Krege S, Sparwasser C, et al. Risk factors for relapse in clinical stage I nonseminomatous testicular germ cell tumors: results of the German Testicular Cancer Study Group Trial. J Clin Oncol. 2003;21:1505–12.
Divrik RT, Akdogan B, Ozen H, Zorlu F. Outcomes of surveillance protocol of clinical stage I nonseminomatous germ cell tumors-is shift to risk adapted policy justified?. J Urol. 2006;176(4 Pt 1):1424–29.
Lago-Hernandez CA, Feldman H, O’Donnell E, Mahal BA, Perez V, Howard S, et al. A refined risk stratification scheme for clinical stage 1 NSGCT based on evaluation of both embryonal predominance and lymphovascular invasion. Ann Oncol. 2015;26:1396–401.
Jacobsen GK, Rorth M, Osterlind K, von der Maase H, Jacobsen A, Madsen EL, et al. Histopathological features in stage I non-seminomatous testicular germ cell tumours correlated to relapse. Danish Testicular Cancer Study Group. APMIS. 1990;98:377–82.
Atsu N, Eskicorapci S, Uner A, Ekici S, Gungen Y, Erkan I, et al. A novel surveillance protocol for stage I nonseminomatous germ cell testicular tumours. BJU Int. 2003;92:32–5.
Spratt DE, Suresh K, Osawa T, Schipper M, Jackson WC, Abugharib A, et al. Detailed pathologic analysis on the co-occurrence of non-seminomatous germ cell tumor subtypes in matched orchiectomy and retroperitoneal lymph node dissections. Med Oncol. 2018;35:21.
Gumus M, Bilici A, Odabas H, Ustaalioglu BBO, Kandemir N, Demirci U, et al. Outcomes of surveillance versus adjuvant chemotherapy for patients with stage IA and IB nonseminomatous testicular germ cell tumors. World J Urol. 2017;35:1103–10.
Roeleveld TA, Horenblas S, Meinhardt W, van de Vijver M, Kooi M, ten Bokkel, et al. Surveillance can be the standard of care for stage I nonseminomatous testicular tumors and even high risk patients. J Urol. 2001;166:2166–70.
Dunphy CH, Ayala AG, Swanson DA, Ro JY, Logothetis C. Clinical stage I nonseminomatous and mixed germ cell tumors of the testis. A clinicopathologic study of 93 patients on a surveillance protocol after orchiectomy alone. Cancer. 1988;62:1202–6.
Li X, Guo S, Wu Z, Dong P, Li Y, Zhang Z, et al. Surveillance for patients with clinical stage I nonseminomatous testicular germ cell tumors. World J Urol. 2015;33:1351–7.
Yetisyigit T, Babacan N, Urun Y, Seber ES, Cihan S, Arpaci E, et al. Predictors of outcome in patients with advanced nonseminomatous germ cell testicular tumors. Asian Pac J Cancer Prev. 2014;15:831–5.
Chovanec M, Hanna N, Cary KC, Einhorn L, Albany C. Management of stage I testicular germ cell tumours. Nat Rev Urol. 2016;13:663–73.
Wagner T, Toft BG, Engvad B, Lauritsen J, Kreiberg M, Bandak M, et al. Prognostic factors for relapse in patients with clinical stage I testicular cancer: protocol for a Danish nationwide cohort study. BMJ Open. 2019;9:e033713.
Ruf CG, Sachs S, Khalili-Harbi N, Isbarn H, Wagner W, Matthies C, et al. Prediction of metastatic status in non-seminomatous testicular cancer. World J Urol. 2014;32:1205–11.
Verrill C, Yilmaz A, Srigley JR, Amin MB, Comperat E, Egevad L, et al. Reporting and staging of testicular germ cell tumors: The International Society of Urological Pathology (ISUP) Testicular Cancer Consultation Conference Recommendations. Am J Surg Pathol. 2017;41:e22–32.
Sahin AA, Gilligan TD, Caudell JJ. Challenges with the 8th edition of the AJCC Cancer Staging Manual for Breast, Testicular, and Head and Neck Cancers. J Natl Compr Canc Netw. 2019;17:560–4.
Sanfrancesco JM, Trevino KE, Xu H, Ulbright TM, Idrees MT. The significance of spermatic cord involvement by testicular germ cell tumors: should we be staging discontinuous invasion from involved lymphovascular spaces differently from direct extension? Am J Surg Pathol. 2018;42:306–11.
Delaney RJ, Sayers CD, Walker MA, Mead GM, Theaker JM. The continued value of central histopathological review of testicular tumours. Histopathology. 2005;47:166–9.
Purshouse K, Watson RA, Church DN, Richardson C, Crane G, Traill Z, et al. Value of supraregional multidisciplinary review for the contemporary management of testicular tumors. Clin Genitourin Cancer. 2017;15:152–6.
Scandura G, Wagner T, Beltran L, Alifrangis C, Shamash J, Berney DM. Pathological risk factors for metastatic disease at presentation in testicular seminomas with focus on the recent pT changes in AJCC TNM eighth edition. Hum Pathol. 2019;94:16–22.
Funding
This work was supported by Orchid and Barts and the London Charity.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Scandura, G., Wagner, T., Beltran, L. et al. Pathological predictors of metastatic disease in testicular non-seminomatous germ cell tumors: which tumor-node-metastasis staging system?. Mod Pathol 34, 834–841 (2021). https://doi.org/10.1038/s41379-020-00717-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-00717-2
This article is cited by
-
Associations of serum levels of microRNA-371a-3p (M371) with risk factors for progression in nonseminomatous testicular germ cell tumours clinical stage 1
World Journal of Urology (2022)
-
Testicular Germ-Cell Tumors with Spermatic Cord Involvement: A Retrospective International Multi-Institutional Experience
Modern Pathology (2022)