Abstract
The pathologist’s role in the breast cancer treatment team has evolved from rendering a diagnosis of breast cancer, to providing a growing list of prognostic and predictive parameters such that individualized treatment decisions can be made based on likelihood of benefit from additional treatments and potential benefit from specific therapies. In all stages, ER and HER2 status help segregate breast cancers into treatment groups with similar outcomes and treatment response rates, however, traditional pathologic parameters such as favorable histologic subtype, size, lymph node status, and Nottingham grade also have remained clinically relevant in early stage disease decision-making. This is especially true for the most common subtype of breast cancer; ER positive, HER2 negative disease. For this same group of breast cancers, an ever-expanding list of gene-expression panels also can provide prediction and prognostication about potential chemotherapy benefit beyond standard endocrine therapies, with the 21-gene Recurrence Score, currently the only prospectively validated predictive test for this purpose. In the more aggressive ER-negative cancer subtypes, response to neoadjuvant therapy and` the extent of tumor infiltrating lymphocytes (TILs) are more recently recognized powerful prognostic parameters, and clinical guidelines now offer additional treatment options for those high-risk patients with residual cancer after standard neoadjuvant therapy. In stage four disease, predictive tests like germline BRCA status, tumor PIK3CA mutation status (in ER+ metastatic disease) and PDL-1 status (in triple negative metastatic disease) are now used to determine additional new treatment options. The objective of this review is to describe the latest in prognostic and predictive parameters in breast cancer as they are relevant to standard pathology reporting and how they are used in breast cancer clinical treatment decisions.
Similar content being viewed by others
Introduction
Every breast cancer pathology report includes multiple parameters that help inform prognosis and prediction in breast cancer. These parameters help clinical teams determine individualized treatment decisions for each breast cancer patient. The pathologist’s role in cancer diagnosis has become that of a “Diagnostic Oncologist,” with assessment of predictive pathology tests determining if a particular patient is eligible for specific therapies and prognostic parameters determining if additional treatments should be considered [1,2,3,4,5,6]. Pathologists should understand both the latest testing and reporting requirements and guidelines but also should have an understanding of their clinical relevance and be familiar with gray zones and unusual results so that they can serve as effective consultants.
While several of these parameters have had relevance for many decades, such as anatomic TNM staging, others have more recently proven their clinical relevance (especially in the metastatic setting) and still others are gaining new traction as evidence continues to evolve [7, 8]. The objective of this review is to describe the latest in prognostic and predictive parameters in breast cancer as they are relevant to standard pathology reporting and how they are used in breast cancer clinical treatment decisions. The reader will become familiar with how these parameters are used in the latest clinical guideline recommendations for prognostic/predictive testing in breast cancer and the evidence supporting their utility.
Prognostic vs. predictive factors overview
Prognostic factors in breast cancer are those that define the natural history or outcomes of the disease, either without therapy or with standard therapy [9]. These factors help define who might need treatment in general based on the likelihood of a worse outcome. For example, estrogen receptor (ER) is a major prognostic factor in breast cancer because ER-negative breast cancers have a significantly worse 5-year overall survival than ER positive cancers [10, 11]. This major difference in outcomes also is supported by vast differences in the underlying biology between ER positive and ER-negative breast cancers [12,13,14,15]. Other traditional and evolving prognostic factors in breast cancer are listed in Table 1. Each factor plays a specific role in treatment pathways because of their association with systemic or local recurrence.
Predictive factors in breast cancer are those that are associated with likelihood of benefit from a specific treatment [9, 16]. These factors help inform which particular treatments may benefit an individual breast cancer patient. For example, ER is a prognostic factor because of its association with outcomes but it is also a predictive factor in breast cancer since cancers with ≥1% ER expression by immunohistochemistry testing receive a statistically significant disease free and overall survival benefit when treated with hormone-targeted therapies such a tamoxifen or selective estrogen receptor modulators (SERMS) [17, 18]. As shown in Table 1, the major predictive factors in early stage breast cancer remain biomarkers ER and HER2, but in stage four disease there has been a rapid evolution to include biomarkers predictive of drug benefit that include germline BRCA testing for all, and PDL1 immunoassays and PI3KCA mutation testing for specific subgroups of stage four patients.
Together, prognostic factors that help determine who needs treatment and predictive factors that help determine what specific treatments might be of benefit are used together to inform overall therapy choices for an individual patient. When multiple factors are combined together, overall treatment algorithms and calculators (such as the United Kingdom’s Predict breast cancer tool) become more powerful at developing successful outcome predictors and treatment pathways for breast cancer patients (https://breast.predict.nhs.uk). The most powerful prognostic and predictive factors have become the major initial dividing points between different breast cancer treatment pathways in clinical guidelines such as the National Comprehensive Cancer Network (NCCN), American Society of Clinical Oncology (ASCO), and St Gallen International Consensus Guidelines. Probably the largest impact factors are ER and HER2 status, which used together create treatment-relevant subgroups of the four major breast cancer “intrinsic subtypes” (ER+/HER2−, ER+/HER2+, ER−/HER2+, and ER−/HER2−) within which different prognostic and predictive factors become relevant.
However, across all of these subtypes, the traditional pathologic TNM stage (based on size, lymph node status, and distant metastases) remains one of the most relevant prognostic factors. For each ER/HER2 subtype, there are significant differences in breast cancer specific survival by stage at diagnosis, with earlier detection making survival differences in each subtype [10, 19, 20]. For ER-negative cancers, differences in TNM anatomic stage remain relevant for the first 5 years of diagnosis, reflecting the more aggressive biology of these cancers and shorter timeline to recurrence and progression [10]. For ER positive cancers, differences in anatomic TNM stage at diagnosis remain relevant over many decades, reflecting the longer timeline to recurrence in this generally more indolent, slow-to-progress group of breast cancers [20].
Another factor that remains relevant across ER and HER2 subtypes is histologic subtype. In fact, the 2020 NCCN guidelines have histologic subtype as the very first branch point in treatment algorithms, even above ER and HER2 status [21] (www.nccn.org). While the ductal/not otherwise specified histologic group is a very broad diagnostic category without much prognostic relevance, cancers with a “favorable histologic type” have entirely different, less aggressive treatment pathways. Pure tubular, pure mucinous, pure cribriform, encapsulated papillary, or solid papillary are cancers that should be ER positive and HER2 negative, and in contrast to typical ER+/HER2− cancers, treatment beyond endocrine therapy is typically only considered in the lymph node positive setting for these special histologic subtypes because of their associations with excellent outcomes [22,23,24,25,26,27,28]. In addition, ER and HER negative good histologic subtypes such as adenoid cystic carcinomas and salivary or secretory carcinomas (or other rare histologic subtypes like low grade adeno-squamous or low grade fibromatosis-like carcinomas) are treated less aggressively than typical “triple negative” breast cancers with consideration for systemic therapies only in lymph node positive disease [23, 25, 29,30,31,32,33,34,35]. For these reasons, it is important for pathologists to follow strict diagnostic criteria when considering a favorable prognosis subtype diagnosis. If there are features that are atypical for a favorable histologic subtype diagnosis (such as high grade or HER2 positivity), these very specific diagnoses should be avoided and/or the pathologist should make it clear in their report that the outcomes typically associated with the standard or pure form of the favorable histologic subtype may not apply to a case with nonstandard features.
Threshold setting and gray zones in predictive vs. prognostic biomarker use
With biomarkers such as ER and HER2 being the first major branch point in treatment pathways, it is important to note that thresholds for a positive result were created for their predictive value, not necessarily for overall treatment pathways decisions. Setting thresholds for biomarkers depends on what you are trying to prognosticate or predict [36, 37]. When predictive, the threshold set will also depend to some extent on the risk-benefit profile of the drug the test makes the patient a candidate for. For example, the risk profile of endocrine therapies, like tamoxifen, is quite low for its potential benefit, so the threshold for a positive result is set quite low (at 1% of cancer cells staining by IHC) to include as many patients as possible that might benefit from this low-risk drug category [38, 39]. With this very sensitive definition of ER positive, a 50–66% reduction in recurrences and 30–40% reduction in overall mortality is observed for patients with ER positive breast cancers treated with endocrine therapy [17]. Even for the lowest levels of ER expression (10–19 fmols by ligand binding assay, which correlates with 1–10% protein expression by IHC) the limited evidence available points to a one third reduction in recurrences with 5 years of tamoxifen, even though many of these cancers have other characteristics more similar to ER-negative cancers [17, 18, 40,41,42,43,44,45,46,47,48,49,50,51]. For HER2 testing, a positive result should predict potential benefit from HER2-targeted therapies, which are currently routinely given with chemotherapy [52,53,54,55,56,57,58]. The risk profile of chemotherapy with HER2-targeted therapies is higher (and more expensive) than endocrine therapy alone with a high risk with both false positive and false-negative results. Testing strategies that use IHC testing as an initial HER2 screening test, with reflex to the more complex in situ hybridization (ISH) testing for IHC equivocal results (or dual IHC and ISH testing) helps to ensure the accuracy of HER2 results.
It is important to acknowledge that there will also usually be a gray zone near the threshold set for a positive vs. negative result, around which there will be both more variability in test results and less clear clinical implications [59]. Both the ER and HER2 testing ASCO/CAP guidelines updates have focused on fine tuning guidelines for these more gray zone results, recommending correlation, confirmation, and explanation in reporting for certain scenarios (see Table 2). For ER testing, the 2020 ASCO/CAP Guidelines Update recognized that cases with <10% or weak staining may need additional steps to confirm the results and recommended that labs set up their own standard operating procedures (such as review of controls, having a second pathologist confirm results, or use a digital-aided interpretation) to confirm or adjudicate these results [38]. In addition, the update also created the ER Low Positive reporting category for cases with 1–10% ER staining, which is to be reported with a comment that acknowledges the limitations of the data on cancers with Low Positive ER. Similarly, HER2 testing gray zones include 2+ results by IHC (which should be reflexed to ISH testing) as well as the unusual result groups by ISH (Groups 2–4 in the 2018 ASCO/CAP HER2 testing update) [56, 58]. Similar to the strategy for ER testing near the threshold for positive, for unusual HER2 ISH group testing additional steps are recommended in the evaluation and work-up of these cases prior to reporting a final overall HER2 status. Reporting comments are also recommended to clarify issues with these unusual HER2 ISH result categories so clinicians and patients can better understand that the HER2 status is non standard. The same holds true for commercial tests like Genomic Health’s 21-gene Recurrence Score (RS), which is now prospectively validated to predict the potential additional benefit of adding chemotherapy to endocrine therapy in ER positive, lymph node negative cancers [60]. Results that are in the middle of the RS range have less clear implications, that differ by age group, than results at the ends of the RS result spectrum [60].
Prognostic stage groupings
When individual factors are combined together, they can become even more powerful predictors of outcomes. With this concept in mind, the 8th edition of the AJCC Cancer Staging Manual expanded their traditional anatomic TNM factors to include tumor grade, ER, HER, and Oncotype RS as part of a new “prognostic stage groupings” to further refine outcome prediction [7, 8, 61]. Initially based on data from the MD Anderson Bioscore and Risk Score using California Cancer Registry (CCR) and National Cancer Database databases, it has since been further validated to outperform the anatomic stage using over 50,000 breast cancer patients in the CCR [62,63,64,65]. Using the prognostic stage, which combines the TNM stage with these additional factors, ~40% of breast cancer patients were restaged into higher or lower prognostic stage groups. This staging system is definitely more complex, requiring reference to large tables with over 150 possible combinations of factors listed. Initially, some combinations were not listed, requiring updating of the original version. As the AJCC prognostic stage groupings and other methods of prognostication continue to evolve, perhaps they will incorporate new prognostic factors in more dynamic ways using risk calculator tools or more dynamic risk assessments at different timepoints in disease progression [66, 67]. Risk calculator tools and nomograms already exist but are not necessarily validated in multiple data sets. As mentioned above, the United Kingdom’s PREDICT breast cancer online calculator tool (https://breast.predict.nhs.uk) is an example of one of these tools. It was created to using outcomes data from the National Health Service to incorporate standard clinicopathologic parameters like age, menopausal status, ER, HER2, Ki67, tumor size, grade, and lymph node status to calculate overall 5, 10, and 15 years survival differences with and without additional therapies [68,69,70].
ER and HER2 status have created groupings of breast cancers, within which, different factors are relevant. However, another important consideration is that different prognostic factors have very different relevance at different timepoints, from initial diagnosis where the initial question is whether a patient will need additional therapies beyond methods used for local control (surgery ± radiation), to post treatment when additional therapies may be needed if there is residual disease, to recurrence and progression. Traditionally, there has been a focus on initial diagnosis but a better understanding of indicators of outcomes in the post treatment and recurrence/progression timepoints has been a rapidly evolving area. Prognostic and predictive factors are presented in the next few sections grouped similar to treatment guidelines, with the various combinations of ER and HER2 status creating subgroups within the early stage vs. metastatic settings.
Prognostic and predictive factors in stage 1–3 ER positive, HER2 negative breast cancers
Because nonmetastatic ER positive, HER2 negative cancers are the largest group of breast cancers overall, much of the historical data on prognosis and outcomes were largely related to this group. Traditional factors like size, lymph node status, and age at diagnosis are highly relevant to recurrence risk in this group over many decades. Additional important prognostic segregators of outcome that reflect the spectrum of underlying biology of these cancers include Nottingham grade, proliferation, and PgR levels. Higher grade, more proliferative ER positive cancers have a higher risk of recurrence earlier than ER positive cancers with a low grade and proliferative rate. In addition, the high grade, high proliferation ER positive cancers potentially stand to benefit more from the addition of chemotherapy in addition to endocrine therapy. However, there are no specific predictive thresholds for grade or proliferation (such as scored with Ki67 IHC) that are clinically validated to predict chemotherapy benefit, so these factors remain prognostic. In addition, since most ER positive cancers have very high levels of ER expression by IHC (rather than a spectrum of ER expression), the downstream hormone receptor, PgR, which has more of a spectrum of expression, turns out to be a more powerful prognostic indicator in ER positive cancers. ER positive breast cancers with low levels of PgR expression are believed to have a less “intact” or responsive hormone-driven pathway, and subsequently are hypothesized to have decreased responsiveness to endocrine therapy alone [71,72,73,74,75,76,77]. However, as with grade and proliferation rates, specific PgR IHC thresholds to predict decreased response to endocrine therapy or potential benefit from the addition of chemotherapy are not validated and therefore, PgR remains a prognostic rather than predictive factor.
What has emerged as a validated predictive factor to help determine potential chemotherapy benefit in the lymph node negative subset of ER positive, HER2 negative breast cancers is the 21-gene RS (Oncotype DX) [78, 79]. This RT-PCR assay generates a RS that is heavily weighted by the level of the five proliferation-related genes assayed but also includes PgR levels (as well as ER, HER2, and a few additional genes). The RS has now been prospectively validated in the TAILOR RX trial to predict the benefit of adding chemotherapy to endocrine therapy (a result which is modified by age) [79]. As such, it is the only validated predictive test in this setting. NCCN and ASCO guidelines currently recommend this test to predict which ER positive, HER2 negative, lymph node negative cancers >0.5 cm may benefit from the addition of chemotherapy [21, 80]. However, other treatment recommendations, such as the St Gallen consensus recommendations, recommend individualized decision-making based on multiple factors, recognizing that gene-expression profile testing may not be available in all settings [81, 82].
While predictive in lymph node negative cancers, it currently serves only as a prognostic test in lymph node positive, ER positive, HER2 negative patients, with the results of another prospective trial, the RxPONDER trial, anticipated to resolve if it is predictive or remains only prognostic in the lymph node positive population [83]. Other gene-expression tests have shown prognostic value as well, helping stratify which ER positive cancers are at a higher risk of recurrence, but have not shown specific predictive value to date [84,85,86,87,88,89].
Prognostic and predictive factors in stage 1–3 HER2 positive breast cancers
HER2 positivity is considered a poor prognostic factor in both ER positive and negative breast cancers. HER2 positive cancers are typically higher grade, with higher proliferative rates and are more rapidly progressive than ER positive, HER2 negative cancers. Outcomes for HER2 positive cancers were similar to or worse than triple negative breast cancers prior to the advent of HER2-targeted therapies. In addition to being prognostic, HER2 is a powerful predictive factor, used to select which patients might benefit from HER2-targeted therapies in combination with chemotherapy [90,91,92,93,94,95]. Because of its aggressive biology, chemotherapy plus HER2-targeted therapy with trastuzumab is considered in invasive HER2 positive cancers of any size or lymph node status, and higher risk features such as size ≥2 cm or positive lymph nodes are used to determine if a second HER2-targeted therapy (pertuzumab) can be added to additionally reduce risk [96,97,98]. De-escalation of the therapy regimen for early stage HER2 positive cancers is considered if the cancer is <1 cm and lymph node negative because of good outcomes in this setting. Unlike the ER positive, HER2 negative group, grade, and proliferation are not considered useful prognostic parameters in this group. Instead, response to neoadjuvant therapies, frequently measured as the “residual cancer burden” is a more powerful prognostic indicator, with excellent long-term outcomes for HER2 positive cancers treated to a complete pathologic response and those with a high residual disease burden at the highest risk of progression [99,100,101,102,103,104,105,106,107,108]. It is for this reason that clinical treatment guidelines consider adding on additional treatments like the antibody-drug conjugate (ADC), TDM-1 (ado-trastuzumab-emtansine), to patients that remain at high risk of recurrence because of residual HER2 positive cancer after neoadjuvant treatment [109]. This drug, first approved in the metastatic HER2 positive setting, delivers a powerful chemotherapy intracellularly once the trastuzumab HER2 antibody binds to HER2 positive cells and avoids many of the side effects of traditional systemic chemotherapy regimens. Other ADCs are being developed and tested that may target lower levels of HER2, which if approved, may dramatically alter how HER2 testing is used as a predictive test [110].
Tumor infiltrating lymphocytes (TILs) have also turned out to be prognostic in HER2 positive cancers. HER2 positive cancers with higher TIL levels are reported to have better response rates to neoadjuvant treatment, which typically correlates with overall survival rates as well [111,112,113,114,115]. The hypothesis is that more TILs present may create a “primed” immune environment, helping to create durable responses to eliminating a cancer. While TILs reporting has not uniformly become standard practice, there are guidelines for standard evaluation and reporting [111, 116,117,118] (www.tilsinbreastcancer.org).
Prognostic and predictive factors in stage 1–3 ER-negative, HER2 negative breast cancers
Similar to the HER2 positive cancers, ER-negative/HER2 negative cancers are typically higher grade and higher proliferation, making these factors less prognostic in this higher risk group. Most treatment guidelines will only risk not treating these aggressive cancers with chemotherapy when they are lymph node negative and less than 0.5 cm, with consideration for treatment when pN1mi or the primary is 0.6–1.0 cm. Chemotherapy is more standard for any lymph node positive triple negative breast cancer or one that is over 1 cm. The exception to this would be the unusual good prognosis triple negative histologic subtypes as mentioned above (adenoid cystic and some other salivary type carcinomas, etc.). Response to neoadjuvant chemotherapy is a powerful prognostic factor in the treated group of triple negative breast cancers (similar to HER2 positive cancers) with additional therapy considered if there is residual disease post treatment (with agents such as capecitabine, an oral chemotherapy) [80]. Similarly, TILs have shown prognostic relevant in determining better response to neoadjuvant chemotherapy [111, 112, 116,117,118]. Many triple negative breast cancers have high genomic instability and there is great interest in determining if immunogenic markers of this instability (such as BRCA mutations or Tumor Mutational Burden) might serve as a predictive biomarkers for additional therapies such as poly-ADP ribose polymerase (PARP) inhibitors and immunotherapies. However, these are still largely investigational in early stage triple negative disease, with approval for use currently only in the advanced or metastatic setting (see next section).
Predictive factors in stage 4 breast cancer
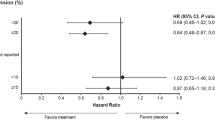
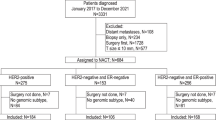
The testing and treatment landscape of metastatic breast cancer has changed dramatically in the last 5 years, with new predictive testing available to help guide treatment in this traditionally very challenging treatment group. (See Figure 1) In a more recent development, all patients with newly metastatic or recurrent breast cancers are now recommended to undergo germline BRCA1/2 testing since the identification of a significant germline mutation predicts potential benefit from adding PARP inhibitors (based on the OlympiAD and EMRACA trials) [119, 120]. In addition, any new metastatic breast cancer should be tested for ER and HER2, since the metastatic status can be different from the primary (although treatment path can also be based on the status of the primary cancer). Similar to in the nonmetastatic setting, ER and HER2 testing is predictive of benefit from specific therapies in the metastatic setting and results of these tests creates subgroups where additional tests may identify candidates for additional treatments.
All newly recurrent or metastatic breast cancer patients should have their disease sampled and tested for current ER/PR and HER2 status with additional testing dependent on results and possible treatment pathways as shown. All patients can also be considered for germline BRCA testing to determine if PARP inhibtor treatments are an option.
Patients with ER positive, HER2 negative cancers may derive benefit from not only an aromatase inhibitor or SERM but also from the addition of a CDK4/6 inhibitor (such as abemaciclib, lapbociclib, or ribociclib). Based on results of the SOLAR1 trial, PIK3CA mutation testing (of the tumor or ctDNA in blood) may also identify patients who can benefit from an alpelisib–fluvesterant combination to inhibit the PI3K and ER pathways [121]. These oral medications can allow slowly progressive ER positive stage 4 breast cancer patients to save more aggressive chemotherapy regimens for later timepoints in progression or metastatic crisis.
Patients with ER-negative, HER2 negative metastatic disease now also have a predictive marker that is a companion diagnostic. These metastatic (or prior primary cancers) can be tested for PD-L1 expression using the SP142 IHC antibody and the Immune Cell scoring system to determine if immune therapy with atezolizumab with alb-paclitaxel chemotherapy may be of benefit [122]. Pembrolizumab (in combination with chemotherapy) was also recently shown to increase progression free survival in triple negative metastatic breast cancer in cancers that tested PD-L1 positive using the 22C3 antibody and a ≥ 10% threshold with the Combined Positive Score system. (KEYNOTE-355 unpublished data, ClinicalTrials.gov Identifier: NCT02819518) Pembrolizumab also may provide survival benefit for patients with MSI-H/dMMR positive cancers (agnostic of site of origin) and was also recently FDA-approved for treating tumor mutation burden high (≥10 mutations/megabase) metastatic cancers from any site [123] (KEYNOTE-158, NCT02628067). This testing and treatment landscape is rapidly changing.
Lastly, rare mutations like NTRK fusions, which are seen in over 90% of secretory carcinomas of the breast (and <5% of other breast cancers), allow for treatment in the metastatic setting with inhibitors of tropomyosin kinase receptors [124]. Frequently, comprehensive genomic profiling is performed on metastatic cancers in practice in an attempt to identify these targetable mutations.
Conclusions
Prognostic and predictive parameters in breast cancer have expanded as our understanding of their relevance in specific biologic subtypes and stages of breast cancer has deepened. New therapies, especially in the metastatic breast cancer setting, have resulting in new predictive tests. Clinical treatment guidelines continue to evolve with new data on these pathology parameters. Pathologists should remain up to date with current testing and treatment guidelines.
References
Allison KH. Molecular pathology of breast cancer: what a pathologist needs to know. Am J Clin Pathol. 2012;138:770–80.
Mandong BM. Diagnostic oncology: role of the pathologist in surgical oncology-a review article. Afr J Med Med Sci. 2009;38:81–8.
Han HS, Magliocco AM. Molecular testing and the pathologist’s role in clinical trials of breast cancer. Clin Breast Cancer. 2016;16:166–79.
Allison KH. Ancillary prognostic and predictive testing in breast cancer: focus on discordant, unusual, and borderline results. Surg Pathol Clin. 2018;11:147–76.
Rakha EA, Green AR. Molecular classification of breast cancer: what the pathologist needs to know. Pathology. 2017;49:111–9.
Leong AS, Zhuang Z. The changing role of pathology in breast cancer diagnosis and treatment. Pathobiology. 2011;78:99–114.
Giuliano AE, Connolly JL, Edge SB, Mittendorf EA, Rugo HS, Solin LJ, et al. Breast cancer—major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67:290–303.
American Joint Committee on Cancer, Amin MB. AJCC cancer staging manual. 8th ed. New York: Springer; 2017. p. XVII, 1024 str.
Pritzker KP. Predictive and prognostic cancer biomarkers revisited. Expert Rev Mol Diagn. 2015;15:971–4.
Foulkes WD, Smith IE, Reis-Filho JS. Triple-negative breast cancer. N Engl J Med. 2010;363:1938–48.
Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, Sawka CA, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007;13:4429–34.
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000;406:747–52.
Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98:10869–74.
Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA. 2003;100:8418–23.
Reis-Filho JS, Pusztai L. Gene expression profiling in breast cancer: classification, prognostication, and prediction. Lancet. 2011;378:1812–23.
Clark GM, Zborowski DM, Culbertson JL, Whitehead M, Savoie M, Seymour L, et al. Clinical utility of epidermal growth factor receptor expression for selecting patients with advanced non-small cell lung cancer for treatment with erlotinib. J Thorac Oncol. 2006;1:837–46.
Early Breast Cancer Trialists’ Collaborative G, Davies C, Godwin J, Gray R, Clarke M, Cutter D, et al. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 2011;378:771–84.
Harvey JM, Clark GM, Osborne CK, Allred DC. Estrogen receptor status by immunohistochemistry is superior to the ligand-binding assay for predicting response to adjuvant endocrine therapy in breast cancer. J Clin Oncol. 1999;17:1474–81.
Howlader N, Cronin KA, Kurian AW, Andridge R. Differences in breast cancer survival by molecular subtypes in the United States. Cancer Epidemiol Biomark Prev. 2018;27:619–26.
Pan H, Gray R, Braybrooke J, Davies C, Taylor C, McGale P, et al. 20-Year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N Engl J Med. 2017;377:1836–46.
Telli ML, Gradishar WJ, Ward JH. NCCN guidelines updates: breast cancer. J Natl Compr Canc Netw. 2019;17:552–5.
Dieci MV, Orvieto E, Dominici M, Conte P, Guarneri V. Rare breast cancer subtypes: histological, molecular, and clinical peculiarities. Oncologist. 2014;19:805–13.
WHO Classification of Tumours Editorial Board. Breast tumours. Lyon (France): INternational Agency for Research on Cancer; 2019. (WHO classification of tumours series, 5th ed; vol. 2). https://publications.iarc.fr/581
Weigelt B, Horlings HM, Kreike B, Hayes MM, Hauptmann M, Wessels LF, et al. Refinement of breast cancer classification by molecular characterization of histological special types. J Pathol. 2008;216:141–50.
Diab SG, Clark GM, Osborne CK, Libby A, Allred DC, Elledge RM. Tumor characteristics and clinical outcome of tubular and mucinous breast carcinomas. J Clin Oncol. 1999;17:1442–8.
Rakha EA, Lee AH, Evans AJ, Menon S, Assad NY, Hodi Z, et al. Tubular carcinoma of the breast: further evidence to support its excellent prognosis. J Clin Oncol. 2010;28:99–104.
Page DL, Dixon JM, Anderson TJ, Lee D, Stewart HJ. Invasive cribriform carcinoma of the breast. Histopathology. 1983;7:525–36.
Di Saverio S, Gutierrez J, Avisar E. A retrospective review with long term follow up of 11,400 cases of pure mucinous breast carcinoma. Breast Cancer Res Treat. 2008;111:541–7.
Van Hoeven KH, Drudis T, Cranor ML, Erlandson RA, Rosen PP. Low-grade adenosquamous carcinoma of the breast. A clinocopathologic study of 32 cases with ultrastructural analysis. Am J Surg Pathol. 1993;17:248–58.
Louwman MW, Vriezen M, van Beek MW, Nolthenius-Puylaert MC, van der Sangen MJ, Roumen RM, et al. Uncommon breast tumors in perspective: incidence, treatment and survival in the Netherlands. Int J Cancer. 2007;121:127–35.
Li CI, Uribe DJ, Daling JR. Clinical characteristics of different histologic types of breast cancer. Br J Cancer. 2005;93:1046–52.
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thurlimann B, Senn HJ, et al. Strategies for subtypes-dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22:1736–47.
Ghabach B, Anderson WF, Curtis RE, Huycke MM, Lavigne JA, Dores GM. Adenoid cystic carcinoma of the breast in the United States (1977 to 2006): a population-based cohort study. Breast Cancer Res. 2010;12:R54.
Kulkarni N, Pezzi CM, Greif JM, Suzanne Klimberg V, Bailey L, Korourian S, et al. Rare breast cancer: 933 adenoid cystic carcinomas from the National Cancer Data Base. Ann Surg Oncol. 2013;20:2236–41.
Horowitz DP, Sharma CS, Connolly E, Gidea-Addeo D, Deutsch I. Secretory carcinoma of the breast: results from the survival, epidemiology and end results database. Breast. 2012;21:350–3.
Altman DG, McShane LM, Sauerbrei W, Taube SE. Reporting recommendations for tumor marker prognostic studies (REMARK): explanation and elaboration. PLoS Med. 2012;9:e1001216.
Hayes DF. Biomarker validation and testing. Mol Oncol. 2015;9:960–6.
Allison KH, Hammond MEH, Dowsett M, McKernin SE, Carey LA, Fitzgibbons PL, et al. Estrogen and Progesterone Receptor Testing in Breast Cancer: ASCO/CAP Guideline Update. J Clin Oncol. 2020;38:1346–66.
Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. Arch Pathol Lab Med. 2010;134:907–22.
Yi M, Huo L, Koenig KB, Mittendorf EA, Meric-Bernstam F, Kuerer HM, et al. Which threshold for ER positivity? a retrospective study based on 9639 patients. Ann Oncol. 2014;25:1004–11.
Bouchard-Fortier A, Provencher L, Blanchette C, Diorio C. Prognostic and predictive value of low estrogen receptor expression in breast cancer. Curr Oncol. 2017;24:e106–14.
Khoshnoud MR, Lofdahl B, Fohlin H, Fornander T, Stal O, Skoog L, et al. Immunohistochemistry compared to cytosol assays for determination of estrogen receptor and prediction of the long-term effect of adjuvant tamoxifen. Breast Cancer Res Treat. 2011;126:421–30.
Badve SS, Baehner FL, Gray RP, Childs BH, Maddala T, Liu ML, et al. Estrogen- and progesterone-receptor status in ECOG 2197: comparison of immunohistochemistry by local and central laboratories and quantitative reverse transcription polymerase chain reaction by central laboratory. J Clin Oncol. 2008;26:2473–81.
Fisher ER, Anderson S, Dean S, Dabbs D, Fisher B, Siderits R, et al. Solving the dilemma of the immunohistochemical and other methods used for scoring estrogen receptor and progesterone receptor in patients with invasive breast carcinoma. Cancer. 2005;103:164–73.
Molino A, Micciolo R, Turazza M, Bonetti F, Piubello Q, Corgnati A, et al. Prognostic significance of estrogen receptors in 405 primary breast cancers: a comparison of immunohistochemical and biochemical methods. Breast Cancer Res Treat. 1997;45:241–9.
Raghav KP, Hernandez-Aya LF, Lei X, Chavez-Macgregor M, Meric-Bernstam F, Buchholz TA, et al. Impact of low estrogen/progesterone receptor expression on survival outcomes in breast cancers previously classified as triple negative breast cancers. Cancer. 2012;118:1498–506.
Honma N, Horii R, Iwase T, Saji S, Younes M, Ito Y, et al. Proportion of estrogen or progesterone receptor expressing cells in breast cancers and response to endocrine therapy. Breast. 2014;23:754–62.
Chen T, Zhang N, Moran MS, Su P, Haffty BG, Yang Q. Borderline ER-positive primary breast cancer gains no significant survival benefit from endocrine therapy: a systematic review and meta-analysis. Clin Breast Cancer. 2018;18:1–8.
Balduzzi A, Bagnardi V, Rotmensz N, Dellapasqua S, Montagna E, Cardillo A, et al. Survival outcomes in breast cancer patients with low estrogen/progesterone receptor expression. Clin Breast Cancer. 2014;14:258–64.
Gloyeske NC, Dabbs DJ, Bhargava R. Low ER+ breast cancer: Is this a distinct group? Am J Clin Pathol. 2014;141:697–701.
Deyarmin B, Kane JL, Valente AL, van Laar R, Gallagher C, Shriver CD, et al. Effect of ASCO/CAP guidelines for determining ER status on molecular subtype. Ann Surg Oncol. 2013;20:87–93.
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013;31:3997–4013.
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. Arch Pathol Lab Med. 2014;138:241–56.
Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. Arch Pathol Lab Med. 2007;131:18–43.
Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25:118–45.
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, et al. Human Epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. J Clin Oncol. 2018;36:2105–22.
Wolff AC, Hammond MEH, Allison KH, Harvey BE, McShane LM, Dowsett M. HER2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update Summary. J Oncol Pract. 2018;14:437–41.
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. Arch Pathol Lab Med. 2018;142:1364–82.
Allison KH. Estrogen receptor expression in breast cancer: we cannot ignore the shades of gray. Am J Clin Pathol. 2008;130:853–4.
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, et al. Adjuvant chemotherapy guided by a 21-gene expression assay in breast cancer. N Engl J Med. 2018;379:111–21.
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67:93–9.
Mittendorf EA, Chavez-MacGregor M, Vila J, Yi M, Lichtensztajn DY, Clarke CA, et al. Bioscore: a staging system for breast cancer patients that reflects the prognostic significance of underlying tumor biology. Ann Surg Oncol. 2017;24:3502–9.
Yi M, Mittendorf EA, Cormier JN, Buchholz TA, Bilimoria K, Sahin AA, et al. Novel staging system for predicting disease-specific survival in patients with breast cancer treated with surgery as the first intervention: time to modify the current American Joint Committee on Cancer staging system. J Clin Oncol. 2011;29:4654–61.
Kantor O, Niu J, Zhao H, Giordano SH, Hunt KK, King TA, et al. Comparative analysis of proposed strategies for incorporating biologic factors into breast cancer staging. Ann Surg Oncol. 2020;27:2229–37.
Weiss A, Chavez-MacGregor M, Lichtensztajn DY, Yi M, Tadros A, Hortobagyi GN, et al. Validation Study of the American Joint Committee on cancer eighth edition prognostic stage compared with the anatomic stage in breast cancer. JAMA Oncol. 2018;4:203–9.
Kattan MW, Hess KR, Amin MB, Lu Y, Moons KG, Gershenwald JE, et al. American Joint Committee on Cancer acceptance criteria for inclusion of risk models for individualized prognosis in the practice of precision medicine. CA Cancer J Clin. 2016;66:370–4.
Kurtz DM, Esfahani MS, Scherer F, Soo J, Jin MC, Liu CL, et al. Dynamic risk profiling using serial tumor biomarkers for personalized outcome prediction. Cell. 2019;178:699–713.e19.
Gray E, Marti J, Brewster DH, Wyatt JC, Hall PS, Group SA. Independent validation of the PREDICT breast cancer prognosis prediction tool in 45,789 patients using Scottish Cancer Registry data. Br J Cancer. 2018;119:808–14.
Wishart GC, Azzato EM, Greenberg DC, Rashbass J, Kearins O, Lawrence G, et al. PREDICT: a new UK prognostic model that predicts survival following surgery for invasive breast cancer. Breast Cancer Res. 2010;12:R1.
Candido Dos Reis FJ, Wishart GC, Dicks EM, Greenberg D, Rashbass J, Schmidt MK, et al. An updated PREDICT breast cancer prognostication and treatment benefit prediction model with independent validation. Breast Cancer Res. 2017;19:58.
Regan MM, Francis PA, Pagani O, Fleming GF, Walley BA, Viale G, et al. Absolute benefit of adjuvant endocrine therapies for premenopausal women with hormone receptor-positive, human epidermal growth factor receptor 2-negative early breast cancer: TEXT and SOFT trials. J Clin Oncol. 2016;34:2221–31.
Albert JM, Gonzalez-Angulo AM, Guray M, Sahin A, Tereffe W, Woodward WA, et al. Patients with only 1 positive hormone receptor have increased locoregional recurrence compared with patients with estrogen receptor-positive progesterone receptor-positive disease in very early stage breast cancer. Cancer. 2011;117:1595–601.
Ahn SG, Yoon CI, Lee JH, Lee HS, Park SE, Cha YJ, et al. Low PR in ER(+)/HER2(−) breast cancer: high rates of TP53 mutation and high SUV. Endocr Relat Cancer. 2019;26:177–85.
Cuzick J, Dowsett M, Pineda S, Wale C, Salter J, Quinn E, et al. Prognostic value of a combined estrogen receptor, progesterone receptor, Ki-67, and human epidermal growth factor receptor 2 immunohistochemical score and comparison with the Genomic Health recurrence score in early breast cancer. J Clin Oncol. 2011;29:4273–8.
Dowsett M, Smith IE. Presurgical progesterone in early breast cancer: so much for so little? J Clin Oncol. 2011;29:2839–41.
Dowsett M, Allred C, Knox J, Quinn E, Salter J, Wale C, et al. Relationship between quantitative estrogen and progesterone receptor expression and human epidermal growth factor receptor 2 (HER-2) status with recurrence in the Arimidex, Tamoxifen, Alone or in Combination trial. J Clin Oncol. 2008;26:1059–65.
Prat A, Cheang MC, Martin M, Parker JS, Carrasco E, Caballero R, et al. Prognostic significance of progesterone receptor-positive tumor cells within immunohistochemically defined luminal A breast cancer. J Clin Oncol. 2013;31:203–9.
Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351:2817–26.
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, et al. Prospective validation of a 21-gene expression assay in breast cancer. N Engl J Med. 2015;373:2005–14.
Andre F, Ismaila N, Henry NL, Somerfield MR, Bast RC, Barlow W, et al. Use of biomarkers to guide decisions on adjuvant systemic therapy for women with early-stage invasive breast cancer: ASCO clinical practice guideline update-integration of results from TAILORx. J Clin Oncol. 2019;37:1956–64.
Balic M, Thomssen C, Wurstlein R, Gnant M, St. Harbeck N. Gallen/Vienna 2019: a brief summary of the consensus discussion on the optimal primary breast cancer treatment. Breast Care. 2019;14:103–10.
Burstein HJ, Curigliano G, Loibl S, Dubsky P, Gnant M, Poortmans P, et al. Estimating the benefits of therapy for early-stage breast cancer: the St. Gallen International Consensus Guidelines for the primary therapy of early breast cancer 2019. Ann Oncol. 2019;30:1541–57.
Ramsey SD, Barlow WE, Gonzalez-Angulo AM, Tunis S, Baker L, Crowley J, et al. Integrating comparative effectiveness design elements and endpoints into a phase III, randomized clinical trial (SWOG S1007) evaluating oncotypeDX-guided management for women with breast cancer involving lymph nodes. Contemp Clin Trials. 2013;34:1–9.
Nitz U, Gluz O, Christgen M, Kates RE, Clemens M, Malter W, et al. Reducing chemotherapy use in clinically high-risk, genomically low-risk pN0 and pN1 early breast cancer patients: five-year data from the prospective, randomised phase 3 West German Study Group (WSG) PlanB trial. Breast Cancer Res Treat. 2017;165:573–83.
Cardoso F, van’t Veer LJ, Bogaerts J, Slaets L, Viale G, Delaloge S, et al. 70-gene signature as an aid to treatment decisions in early-stage breast cancer. N Engl J Med. 2016;375:717–29.
Laenkholm AV, Jensen MB, Eriksen JO, Rasmussen BB, Knoop AS, Buckingham W, et al. PAM50 risk of recurrence score predicts 10-year distant recurrence in a comprehensive danish cohort of postmenopausal women allocated to 5 years of endocrine therapy for hormone receptor-positive early breast cancer. J Clin Oncol. 2018;36:735–40.
Sestak I, Buus R, Cuzick J, Dubsky P, Kronenwett R, Denkert C, et al. Comparison of the performance of 6 prognostic signatures for estrogen receptor-positive breast cancer: a secondary analysis of a randomized clinical trial. JAMA Oncol. 2018;4:545–53.
Sestak I, Martin M, Dubsky P, Kronenwett R, Rojo F, Cuzick J, et al. Prediction of chemotherapy benefit by EndoPredict in patients with breast cancer who received adjuvant endocrine therapy plus chemotherapy or endocrine therapy alone. Breast Cancer Res Treat. 2019;176:377–86.
Bartlett JMS, Sgroi DC, Treuner K, Zhang Y, Ahmed I, Piper T, et al. Breast cancer index and prediction of benefit from extended endocrine therapy in breast cancer patients treated in the adjuvant tamoxifen—to offer more? (aTTom) trial. Ann Oncol. 2019;30:1776–83.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344:783–92.
Goldhirsch A, Gelber RD, Piccart-Gebhart MJ, de Azambuja E, Procter M, Suter TM, et al. 2 years versus 1 year of adjuvant trastuzumab for HER2-positive breast cancer (HERA): an open-label, randomised controlled trial. Lancet. 2013;382:1021–8.
Perez EA, Romond EH, Suman VJ, Jeong JH, Davidson NE, Geyer CE Jr, et al. Four-year follow-up of trastuzumab plus adjuvant chemotherapy for operable human epidermal growth factor receptor 2-positive breast cancer: joint analysis of data from NCCTG N9831 and NSABP B-31. J Clin Oncol. 2011;29:3366–73.
Swain SM, Kim SB, Cortes J, Ro J, Semiglazov V, Campone M, et al. Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA study): overall survival results from a randomised, double-blind, placebo-controlled, phase 3 study. Lancet Oncol. 2013;14:461–71.
Baselga J, Bradbury I, Eidtmann H, Di Cosimo S, de Azambuja E, Aura C, et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2012;379:633–40.
Verma S, Miles D, Gianni L, Krop IE, Welslau M, Baselga J, et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367:1783–91.
von Minckwitz G, Procter M, de Azambuja E, Zardavas D, Benyunes M, Viale G, et al. Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer. N Engl J Med. 2017;377:122–31.
Gianni L, Pienkowski T, Im YH, Tseng LM, Liu MC, Lluch A, et al. 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): a multicentre, open-label, phase 2 randomised trial. Lancet Oncol. 2016;17:791–800.
Denduluri N, Somerfield MR, Giordano SH. Selection of optimal adjuvant chemotherapy and targeted therapy for early breast cancer: ASCO clinical practice guideline focused update summary. J Oncol Pract. 2018;14:508–10.
von Minckwitz G, Untch M, Blohmer JU, Costa SD, Eidtmann H, Fasching PA, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30:1796–804.
Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, Collichio F, et al. The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res. 2007;13:2329–34.
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–72.
Bossuyt V, Provenzano E, Symmans WF, Boughey JC, Coles C, Curigliano G, et al. Recommendations for standardized pathological characterization of residual disease for neoadjuvant clinical trials of breast cancer by the BIG-NABCG collaboration. Ann Oncol. 2015;26:1280–91.
Campbell JI, Yau C, Krass P, Moore D, Carey LA, Au A, et al. Comparison of residual cancer burden, American Joint Committee on Cancer staging and pathologic complete response in breast cancer after neoadjuvant chemotherapy: results from the I-SPY 1 TRIAL (CALGB 150007/150012; ACRIN 6657). Breast Cancer Res Treat. 2017;165:181–91.
Müller HD, Posch F, Suppan C, Bargfrieder U, Gumpoldsberger M, Hammer R, et al. Validation of residual cancer burden as prognostic factor for breast cancer patients after neoadjuvant therapy. Ann Surg Oncol. 2019;26:4274–83.
Provenzano E, Bossuyt V, Viale G, Cameron D, Badve S, Denkert C, et al. Standardization of pathologic evaluation and reporting of postneoadjuvant specimens in clinical trials of breast cancer: recommendations from an international working group. Mod Pathol. 2015;28:1185–201.
Steenbruggen TG, van Seijen M, Janssen LM, van Ramshorst MS, van Werkhoven E, Vrancken Peeters M, et al. Prognostic value of residual disease after neoadjuvant therapy in HER2-positive breast cancer evaluated by residual cancer burden, neoadjuvant response index, and neo-bioscore. Clin Cancer Res. 2019;25:4985–92.
Symmans WF, Peintinger F, Hatzis C, Rajan R, Kuerer H, Valero V, et al. Measurement of residual breast cancer burden to predict survival after neoadjuvant chemotherapy. J Clin Oncol. 2007;25:4414–22.
Symmans WF, Wei C, Gould R, Yu X, Zhang Y, Liu M, et al. Long-term prognostic risk after neoadjuvant chemotherapy associated with residual cancer burden and breast cancer subtype. J Clin Oncol. 2017;35:1049–60.
von Minckwitz G, Huang CS, Mano MS, Loibl S, Mamounas EP, Untch M, et al. Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N Engl J Med. 2019;380:617–28.
Rinnerthaler G, Gampenrieder SP, Greil R. HER2 directed antibody-drug-conjugates beyond T-DM1 in breast cancer. Int J Mol Sci. 2019;20:1115.
Dieci MV, Radosevic-Robin N, Fineberg S, van den Eynden G, Ternes N, Penault-Llorca F, et al. Update on tumor-infiltrating lymphocytes (TILs) in breast cancer, including recommendations to assess TILs in residual disease after neoadjuvant therapy and in carcinoma in situ: a report of the International Immuno-Oncology Biomarker Working Group on Breast Cancer. Semin Cancer Biol. 2018;52:16–25.
Luen SJ, Salgado R, Dieci MV, Vingiani A, Curigliano G, Gould RE, et al. Prognostic implications of residual disease tumor-infiltrating lymphocytes and residual cancer burden in triple-negative breast cancer patients after neoadjuvant chemotherapy. Ann Oncol. 2019;30:236–42.
Loi S, Michiels S, Salgado R, Sirtaine N, Jose V, Fumagalli D, et al. Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: results from the FinHER trial. Ann Oncol. 2014;25:1544–50.
Loi S, Sirtaine N, Piette F, Salgado R, Viale G, Van Eenoo F, et al. Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98. J Clin Oncol. 2013;31:860–7.
Salgado R, Denkert C, Campbell C, Savas P, Nuciforo P, Aura C, et al. Tumor-infiltrating lymphocytes and associations with pathological complete response and event-free survival in HER2-positive early-stage breast cancer treated with lapatinib and trastuzumab: a secondary analysis of the NeoALTTO trial. JAMA Oncol. 2015;1:448–54.
Denkert C, von Minckwitz G, Darb-Esfahani S, Lederer B, Heppner BI, Weber KE, et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 2018;19:40–50.
Hwang HW, Jung H, Hyeon J, Park YH, Ahn JS, Im YH, et al. A nomogram to predict pathologic complete response (pCR) and the value of tumor-infiltrating lymphocytes (TILs) for prediction of response to neoadjuvant chemotherapy (NAC) in breast cancer patients. Breast Cancer Res Treat. 2019;173:255–66.
Stanton SE, Disis ML. Clinical significance of tumor-infiltrating lymphocytes in breast cancer. J Immunother Cancer. 2016;4:59.
Robson M, Im SA, Senkus E, Xu B, Domchek SM, Masuda N, et al. Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med. 2017;377:523–33.
Litton JK, Rugo HS, Ettl J, Hurvitz SA, Goncalves A, Lee KH, et al. Talazoparib in patients with advanced breast cancer and a germline BRCA mutation. N Engl J Med. 2018;379:753–63.
Andre F, Ciruelos E, Rubovszky G, Campone M, Loibl S, Rugo HS, et al. Alpelisib for PIK3CA-mutated, hormone receptor-positive advanced breast cancer. N Engl J Med. 2019;380:1929–40.
Schmid P, Adams S, Rugo HS, Schneeweiss A, Barrios CH, Iwata H, et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med. 2018;379:2108–21.
Le DT, Durham JN, Smith KN, Wang H, Bartlett BR, Aulakh LK, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357:409–13.
Drilon A, Laetsch TW, Kummar S, DuBois SG, Lassen UN, Demetri GD, et al. Efficacy of larotrectinib in TRK fusion-positive cancers in adults and children. N Engl J Med. 2018;378:731–9.
Allison KH, Hammond MEH, Dowsett M, McKernin SE, Carey LA, Fitzgibbons PL, et al. Estrogen and progesterone receptor testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Guideline Update. Arch Pathol Lab Med. 2020;144:545–63.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Allison, K.H. Prognostic and predictive parameters in breast pathology: a pathologist’s primer. Mod Pathol 34 (Suppl 1), 94–106 (2021). https://doi.org/10.1038/s41379-020-00704-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-00704-7
This article is cited by
-
Searching for the “Holy Grail” of breast cancer recurrence risk: a narrative review of the hunt for a better biomarker and the promise of circulating tumor DNA (ctDNA)
Breast Cancer Research and Treatment (2024)
-
High-grade HER2-positive mucoepidermoid carcinoma of the breast: a case report and review of the literature
Journal of Medical Case Reports (2023)
-
Updates on breast biomarkers
Virchows Archiv (2022)