Abstract
Lobular neoplasia (LN) is an atypical proliferation of small, dyscohesive epithelial cells within the terminal duct lobular unit (TDLU), with or without pagetoid extension and encompasses both lobular carcinoma in situ (LCIS) and atypical lobular hyperplasia (ALH). LN is a non-obligate precursor of invasive breast carcinoma and the diagnosis of LN confers an increased risk of invasive carcinoma development, compared to the general population. Diagnostic challenges arise in the accurate classification of LCIS into classic, pleomorphic and florid subtypes, in distinguishing between LCIS and ductal carcinoma in situ (DCIS) and in the appropriate use and interpretation of E-cadherin immunohistochemistry. Due to the paucity of robust data on the natural history of LCIS, and hence its clinical significance, the management is often pragmatic rather than entirely evidence-based and requires a multidisciplinary approach. In this review, we discuss the clinicopathologic and molecular features of LCIS and address the key challenges that arise in the diagnosis and management of LCIS.
Similar content being viewed by others
Background
Definition
In the current 5th edition of the WHO Breast Tumour Classification (2019), the term lobular neoplasia includes the entire spectrum of atypical epithelial lesions originating in the terminal duct lobular unit and is characterized by a proliferation of generally small, non-cohesive monomorphic cells, with or without pagetoid involvement of terminal ducts [1]. The designations ALH and LCIS are used to describe the variable extent of acinar involvement, however, the distinction is quantitative and arbitrary. In both lesions there is a proliferation of cytologically identical cells, but in LCIS more than half of the acini in a TDLU are filled and expanded by neoplastic cells, whereas in ALH less than fifty percent of the acini are involved (Fig. 1). Given the arbitrary nature of this cut off, the diagnosis of ALH and LCIS is subject to intra- and inter-observer variability. In practice, the term LN can be utilized to encompass both lesions. However, given that LCIS confers a higher risk of subsequent breast cancer development compared to ALH [2], together with the recognition of pleomorphic and florid variants, the distinction is still clinically relevant.
Historical perspective
The first detailed description of LCIS was published in 1941 by Foote and Stewart [3]. The authors reported a rare form of non-infiltrative mammary cancer, termed LCIS that was incidental, multicentric and associated with invasive ductal (IDC) and lobular carcinoma (ILC). They hypothesized that LCIS was a precursor to invasive breast carcinoma – analogous to DCIS, and mastectomy became the recommended treatment for LCIS for several decades. The term ALH was introduced in 1978 as a descriptor for less extensive LCIS which was also associated with an increased risk of breast carcinoma development [4]. However, subsequent long-term outcome data showed that the rate of progression to invasive carcinoma after a diagnosis of LCIS was lower than expected [5, 6]. Indeed, the term LN was introduced to convey the more indolent nature of this proliferative process, necessitating less radical treatment [5]. Currently, LCIS is considered to be both a risk factor for and a non-obligate precursor of invasive breast carcinoma.
Epidemiology
Classic LCIS (CLCIS) is most commonly diagnosed in premenopausal females (mean age range 45–50 years) [1, 7], while pleomorphic (PLCIS) and florid LCIS (FLCIS) are typically seen in postmenopausal women (mean age range 60–70 years) [8]. The true incidence of LN in the general population is unknown, given that most women are asymptomatic and there are no specific clinical or radiological features in the majority of cases. The incidence of LCIS in benign breast core biopsies is 0.5–3.6% and in reduction mammoplasty specimens is 0.04–1.2% [1].
Clinical features
CLCIS is clinically silent and usually an incidental finding in core biopsies performed for other indications [3, 5]. In less than 2% of cases, CLCIS may be associated with imaging abnormalities that result in a targeted biopsy [9, 10]. Conversely, PLCIS [11, 12] and FLCIS [8] are frequently identified on screening mammography, as they are typically associated with microcalcifications. Rarely, FLCIS may present as a mass lesion detected on imaging [8].
Pathology and natural history
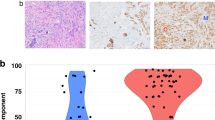
There are three major morphologic subtypes of LCIS recognized in the current WHO Classification: classic, pleomorphic and florid [1]. CLCIS is characterized by a proliferation of monomorphic, loosely cohesive type A and/or type B cells. Type A cells are typically small and round, with hyperchromatic nuclei and minimal cytoplasm. Type B cells show more variation in size and shape, have larger nuclei (up to double the size of a lymphocyte) with vesicular chromatin and small nucleoli. In many cases, cytoplasmic vacuoles can also be identified, with occasional eosinophilic globules. Signet ring morphology can be appreciated when cytoplasmic vacuolation is pronounced. PLCIS (Fig. 2) is composed of atypical cells, with variable sized nuclei, at least some of which are more than four times the size of a lymphocyte or equivalent to nuclei in high-grade DCIS [13, 14]. Apocrine differentiation may be seen in a subset of cases [14]. FLCIS (Fig. 2) refers to confluent mass-forming CLCIS with little intervening stroma [8, 15]. At a minimum, an expanded acinus or duct should fill at least one high-power field. Both PLCIS and FLCIS are more frequently associated with comedo-type necrosis and microcalcifications.
CLCIS is typically multifocal, multicentric and bilateral [16,17,18]. Compared to the general population, CLCIS increases the risk of invasive carcinoma development 7–10 fold [2, 5, 6, 19,20,21,22,23], with a 1-2% absolute risk of invasive carcinoma per year and 30-40% lifetime risk. Subsequent invasive carcinoma can be ipsilateral or contralateral and both ILC and IDC have been described [24, 25]. However, consistent with the precursor nature of LCIS, there is a much higher risk of developing ILC in the ipsilateral breast [25,26,27,28]. Long-term outcome data on the natural history of PLCIS and FLCIS is limited and the risk of local recurrence following resection has not been well established [29].
Biomarker profile
CLCIS is typically estrogen receptor (ER) and progesterone receptor (PR) positive, HER2 negative [30]. PLCIS may occasionally show HER2 amplification, however it is most commonly HER2 negative. The apocrine variant of PLCIS can be ER/PR negative, HER2 positive [14].
Genomic correlates
The clonal nature of LCIS has been established through loss of heterozygosity [31], comparative genomic hybridization [32,33,34] and single nucleotide polymorphism array [35] analyses. ALH and CLCIS are genetically similar, demonstrating recurrent deletions of 16q and gains of 1q with a similar pattern of unbalanced chromosomal aberrations [32, 34]. Furthermore, LCIS subtypes carry the same genetic signature of 16q loss and 1q gain, with additional molecular changes, including amplification of 17q in FLCIS [8] and deletions of 8p and 13q and gains of 8q in PLCIS [36,37,38], as well as overall increased genetic complexity compared to CLCIS. Indeed, FLCIS and PLCIS are thought to be genetically more advanced lesions, originating along the low-grade breast neoplasia pathway and de-differentiating from CLCIS to develop a high-grade phenotype [8, 39].
The loss of heterozygosity at 16q with resultant bi-allelic inactivation of CDH1 and impaired E-cadherin protein function is central to the pathogenesis of lobular neoplasms, both in situ and invasive. Approximately 60–80% of ILC show somatic mutations in CDH1 and the initial identification of the same CDH1 mutations in synchronous LCIS and ILC provided direct support for LCIS being a precursor lesion to ILC [40]. The clonal origin for LCIS and synchronous ER-positive ILC has since been demonstrated in a number of other studies [33, 35, 41]. In addition, PLCIS and pleomorphic ILC have also been shown to share the same genetic aberrations [39]. Next generation sequencing techniques have also highlighted the same combination of somatic mutations in LCIS and ILC [42,43,44], including mutations in CDH1, PIK3CA and CBFB. Although CDH1 mutations and E-cadherin dysfunction have a clear role in the pathogenesis of lobular neoplasms, germline mutations of CDH1 are infrequent in familial lobular carcinoma [45].
Key diagnostic challenges
Classic LCIS versus pleomorphic LCIS
Type B cells of CLCIS can be distinguished from PLCIS using nuclear size. Compared to a lymphocyte, the nuclei of type B cells are up to two times larger, whereas in PLCIS, at least some nuclei are more than four times the size [13]. In borderline cases, or if in doubt, the diagnosis of CLCIS is recommended [1]. Apocrine differentiation alone should not be used as a defining feature of PLCIS.
Classic LCIS versus florid LCIS
Both FLCIS and CLCIS are characterized by a proliferation of cytologically similar cells, however in FLCIS the proliferation results in marked distension of acini and ducts forming a bulky mass-like lesion. FLCIS may be associated with comedo-type necrosis, which is not typically seen in CLCIS. In borderline cases, the diagnosis of CLCIS is recommended [1].
Florid versus extensive LCIS
It is important to note that the term ‘florid’ is not synonymous with ‘extensive’ or ‘diffuse’. When LCIS is described as ‘extensive’, the presumptive interpretation is that of diffuse involvement of multiple TDLUs without marked acinar expansion. FLCIS refers to a specific morphologic subtype of LCIS, with distinct diagnostic criteria [1].
Classic LCIS versus low-grade DCIS
CLCIS and low-grade DCIS of solid type can appear morphologically similar. The identification of cribriform areas and cellular cohesion is more in keeping with a ductal lesion. Immunohistochemistry can be helpful, by demonstrating lost or aberrant membranous E-cadherin staining in LCIS.
Pleomorphic LCIS versus high-grade DCIS
The distinction between PLCIS and high-grade DCIS may be difficult, given that both lesions comprise large atypical cells, with frequent comedo-type necrosis and calcifications. Furthermore, both lesions can show aberrant E-cadherin staining on immunohistochemistry [14, 46]. However, PLCIS should be suspected when the proliferation comprises dyscohesive cells with intracytoplasmic vacuoles and eosinophilic globules. Surrounding CLCIS may also be a clue to the lobular nature of the lesion.
Mixed lesions
In some cases, both LCIS and DCIS can occur in the same TDLU. Morphologic features such as loss of cellular cohesion as well as absent/aberrant E-cadherin staining can be used to identify the LCIS component (Fig. 3). Both components should be reported. Similarly, multiple morphologic subtypes of LCIS may be identified in the same specimen and should be reported separately, with margin status recorded for pleomorphic and florid subtypes.
E-cadherin application and interpretation
Immunohistochemistry for E-cadherin is frequently used to differentiate between lobular and ductal neoplasia. The cells of ductal proliferations typically show strong, circumferential membranous E-cadherin expression. In the majority of lobular neoplasms, E-cadherin shows complete absence of membranous staining (Fig. 2). However, up to 10% of cases may demonstrate an aberrant pattern of expression of E-cadherin, characterized by incomplete, fragmented or beaded membranous staining, diffuse cytoplasmic staining or perinuclear dot-like pattern of staining [29, 47]. When the lobular proliferation only partially replaces a TDLU, admixed ductal epithelial and myoepithelial cells may show intact membranous expression of E-cadherin, which may be a pitfall in E-cadherin interpretation. Since the accurate distinction between LN and DCIS has important clinical implications, E-cadherin staining is recommended in problematic cases. When the E-cadherin stain is difficult to interpret, additional immunohistochemical stains can be utilized, including other members of the cadherin-catenin complex such as beta-catenin and p120. Demonstrating loss of membranous staining for beta-catenin and cytoplasmic accumulation of p120 will lend support to a lobular phenotype [48].
Management implications
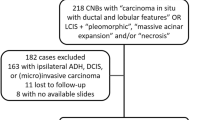
Significance of LCIS in core needle biopsies
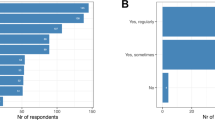
Identification of CLCIS in core needle biopsies requires careful clinical, radiologic and pathologic correlation. Recent evidence shows that CLCIS has a low upgrade rate (1–4%) to DCIS and invasive carcinoma when there are concordant imaging findings [49,50,51,52,53]. Therefore, excision is not required in incidental cases of CLCIS on core needle biopsy following multidisciplinary review. Excision is recommended when there are discordant radiological findings [50, 54], in cases with a mixed ductal/lobular phenotype, when there is an indeterminate focus of in situ carcinoma and when PLCIS and FLCIS [55] are identified, as both lesions are associated with significantly higher upgrade rates (averaging 40%) [15, 29].
LCIS in excision specimens
Positive margins in CLCIS are not clinically relevant and are not recorded, given the multifocal and bilateral nature of the disease process and the relatively low progression rate to invasive carcinoma. The relevance of margin status in PLCIS and FLCIS is not well established. The significance of positive margins in PLCIS is controversial with very few studies addressing the risk of local recurrence in this context [12, 56]. The local recurrence rate of FLCIS has not been determined. However, the current recommendation is to record margin status for both PLCIS and FLCIS, given the high-grade morphology and large volume disease. This ensures that appropriate management decisions are made in a multidisciplinary setting, with thorough clinical, radiologic and pathologic correlation.
Staging
The current 8th edition of the American Joint Committee on Cancer (AJCC) staging manual no longer assigns a T stage to LCIS, which was previously staged as Tis. This decision is controversial as it separates the staging of LCIS from that of DCIS. While CLCIS, and increasingly, low-grade DCIS are managed conservatively, the molecular nature of both the proliferations is clonal/neoplastic. Therefore, it seems paradoxical that CLCIS and low-grade DCIS are staged differently. Furthermore, the pleomorphic and florid subtypes of LCIS are characterized by more complex genomic abnormalities, and within the limits of the current data, appear to be more aggressive than CLCIS. Consequently, the current management of PLCIS and FLCIS more closely resembles that of high-grade DCIS, yet this is not reflected in the current staging system. The question of whether there should be a category of Stage 0 for any in situ disease is a separate issue for the academic community to discuss.
Conclusions
LCIS is a clonal, neoplastic proliferation that creates challenges in clinical practice with regards to accurate diagnosis, classification and management. Key challenges include distinguishing classic from pleomorphic and florid variants, LCIS from DCIS and appropriate use and interpretation of E-Cadherin immunohistochemistry. Although there is some long-term outcome data on the natural history of CLCIS, there is only limited data for PLCIS and FLCIS. Therefore, the clinical significance of these lesions is not currently well established, with management decisions being pragmatic rather than fully evidence based and hence, best carried out in a multidisciplinary setting in challenging cases.
References
WHO classification of tumours of the breast. 5 ed. Lyon: International Agency for Research on Cancer, 2019.
Page DL, Kidd TE Jr., Dupont WD, Simpson JF, Rogers LW. Lobular neoplasia of the breast: higher risk for subsequent invasive cancer predicted by more extensive disease. Hum Pathol. 1991;22:1232–9.
Foote FW, Stewart FW. Lobular carcinoma in situ: a rare form of mammary cancer. Am J Pathol. 1941;17:491–6 3.
Page DL, Vander Zwaag R, Rogers LW, Williams LT, Walker WE, Hartmann WH. Relation between component parts of fibrocystic disease complex and breast cancer. J Natl Cancer Inst. 1978;61:1055–63.
Haagensen CD, Lane N, Lattes R, Bodian C. Lobular neoplasia (so-called lobular carcinoma in situ) of the breast. Cancer. 1978;42:737–69.
Rosen PP, Kosloff C, Lieberman PH, Adair F, Braun DW Jr. Lobular carcinoma in situ of the breast. Detailed analysis of 99 patients with average follow-up of 24 years. Am J Surg Pathol. 1978;2:225–51.
Beute BJ, Kalisher L, Hutter RV. Lobular carcinoma in situ of the breast: clinical, pathologic, and mammographic features. AJR Am J Roentgenol. 1991;157:257–65.
Shin SJ, Lal A, De Vries S, Suzuki J, Roy R, Hwang ES, et al. Florid lobular carcinoma in situ: molecular profiling and comparison to classic lobular carcinoma in situ and pleomorphic lobular carcinoma in situ. Hum Pathol. 2013;44:1998–2009.
Maxwell AJ, Clements K, Dodwell DJ, Evans AJ, Francis A, Hussain M, et al. The radiological features, diagnosis and management of screen-detected lobular neoplasia of the breast: Findings from the Sloane Project. Breast. 2016;27:109–15.
Scoggins M, Krishnamurthy S, Santiago L, Yang W. Lobular carcinoma in situ of the breast: clinical, radiological, and pathological correlation. Acad Radio. 2013;20:463–70.
Fasola CE, Chen JJ, Jensen KC, Allison KH, Horst KC. Characteristics and clinical outcomes of pleomorphic lobular carcinoma in situ of the breast. Breast J. 2018;24:66–69.
Flanagan MR, Rendi MH, Calhoun KE, Anderson BO, Javid SH. Pleomorphic lobular carcinoma in situ: radiologic-pathologic features and clinical management. Ann Surg Oncol. 2015;22:4263–9.
Sneige N, Wang J, Baker BA, Krishnamurthy S, Middleton LP. Clinical, histopathologic, and biologic features of pleomorphic lobular (ductal-lobular) carcinoma in situ of the breast: a report of 24 cases. Mod Pathol. 2002;15:1044–50.
Chen YY, Hwang ES, Roy R, DeVries S, Anderson J, Wa C, et al. Genetic and phenotypic characteristics of pleomorphic lobular carcinoma in situ of the breast. Am J Surg Pathol. 2009;33:1683–94.
Shamir ER, Chen YY, Chu T, Pekmezci M, Rabban JT, Krings G. Pleomorphic and florid lobular carcinoma in situ variants of the breast: a clinicopathologic study of 85 cases with and without invasive carcinoma from a single academic center. Am J Surg Pathol. 2019;43:399–408.
Rosen PP, Senie R, Schottenfeld D, Ashikari R. Noninvasive breast carcinoma: frequency of unsuspected invasion and implications for treatment. Ann Surg. 1979;189:377–82.
Rosen PP, Braun DW Jr, Lyngholm B, Urban JA, Kinne DW. Lobular carcinoma in situ of the breast: preliminary results of treatment by ipsilateral mastectomy and contralateral breast biopsy. Cancer. 1981;47:813–9.
Urban JA. Bilaterality of cancer of the breast. Biopsy of the opposite breast. Cancer. 1967;20:1867–70.
Zurrida S, Bartoli C, Galimberti V, Raselli R, Barletta L. Interpretation of the risk associated with the unexpected finding of lobular carcinoma in situ. Ann Surg Oncol. 1996;3:57–61.
Bodian CA, Perzin KH, Lattes R. Lobular neoplasia. Long term risk of breast cancer and relation to other factors. Cancer. 1996;78:1024–34.
Habel LA, Moe RE, Daling JR, Holte S, Rossing MA, Weiss NS. Risk of contralateral breast cancer among women with carcinoma in situ of the breast. Ann Surg. 1997;225:69–75.
Warnberg F, Yuen J, Holmberg L. Risk of subsequent invasive breast cancer after breast carcinoma in situ. Lancet 2000;355:724–5.
Franceschi S, Levi F, La Vecchia C, Randimbison L, Te VC. Second cancers following in situ carcinoma of the breast. Int J Cancer. 1998;77:392–5.
Chuba PJ, Hamre MR, Yap J, Severson RK, Lucas D, Shamsa F, et al. Bilateral risk for subsequent breast cancer after lobular carcinoma-in-situ: analysis of surveillance, epidemiology, and end results data. J Clin Oncol. 2005;23:5534–41.
Ansquer Y, Delaney S, Santulli P, Salomon L, Carbonne B, Salmon R. Risk of invasive breast cancer after lobular intra-epithelial neoplasia: review of the literature. Eur J Surg Oncol. 2010;36:604–9.
King TA, Pilewskie M, Muhsen S, Patil S, Mautner SK, Park A, et al. Lobular carcinoma in situ: a 29-year longitudinal experience evaluating clinicopathologic features and breast cancer risk. J Clin Oncol. 2015;33:3945–52.
Coopey SB, Mazzola E, Buckley JM, Sharko J, Belli AK, Kim EM, et al. The role of chemoprevention in modifying the risk of breast cancer in women with atypical breast lesions. Breast Cancer Res Treat. 2012;136:627–33.
Li CI, Malone KE, Saltzman BS, Daling JR. Risk of invasive breast carcinoma among women diagnosed with ductal carcinoma in situ and lobular carcinoma in situ, 1988-2001. Cancer 2006;106:2104–12.
Schnitt SJ, Brogi E, Chen YY, King TA, Lakhani SR. American registry of pathology expert opinions: the spectrum of lobular carcinoma in situ: diagnostic features and clinical implications. Ann Diagn Pathol. 2020;45:151481.
Mohsin SK, O’Connell P, Allred DC, Libby AL. Biomarker profile and genetic abnormalities in lobular carcinoma in situ. Breast Cancer Res Treat. 2005;90:249–56.
Lakhani SR, Collins N, Sloane JP, Stratton MR. Loss of heterozygosity in lobular carcinoma in situ of the breast. Clin Mol Pathol. 1995;48:M74–8.
Lu YJ, Osin P, Lakhani SR, Di Palma S, Gusterson BA, Shipley JM. Comparative genomic hybridization analysis of lobular carcinoma in situ and atypical lobular hyperplasia and potential roles for gains and losses of genetic material in breast neoplasia. Cancer Res. 1998;58:4721–7.
Hwang ES, Nyante SJ, Yi Chen Y, Moore D, DeVries S, Korkola JE, et al. Clonality of lobular carcinoma in situ and synchronous invasive lobular carcinoma. Cancer 2004;100:2562–72.
Mastracci TL, Shadeo A, Colby SM, Tuck AB, O’Malley FP, Bull SB, et al. Genomic alterations in lobular neoplasia: a microarray comparative genomic hybridization signature for early neoplastic proliferationin the breast. Genes Chromosomes Cancer. 2006;45:1007–17.
Andrade VP, Ostrovnaya I, Seshan VE, Morrogh M, Giri D, Olvera N, et al. Clonal relatedness between lobular carcinoma in situ and synchronous malignant lesions. Breast Cancer Res. 2012;14:R103.
Simpson PT, Reis-Filho JS, Lambros MB, Jones C, Steele D, Mackay A, et al. Molecular profiling pleomorphic lobular carcinomas of the breast: evidence for a common molecular genetic pathway with classic lobular carcinomas. J Pathol. 2008;215:231–44.
Reis-Filho JS, Simpson PT, Jones C, Steele D, Mackay A, Iravani M, et al. Pleomorphic lobular carcinoma of the breast: role of comprehensive molecular pathology in characterization of an entity. J Pathol. 2005;207:1–13.
Vargas AC, Lakhani SR, Simpson PT. Pleomorphic lobular carcinoma of the breast: molecular pathology and clinical impact. Future Oncol. 2009;5:233–43.
Lopez-Garcia MA, Geyer FC, Lacroix-Triki M, Marchio C, Reis-Filho JS. Breast cancer precursors revisited: molecular features and progression pathways. Histopathology 2010;57:171–92.
Vos CB, Cleton-Jansen AM, Berx G, de Leeuw WJ, ter Haar NT, van Roy F, et al. E-cadherin inactivation in lobular carcinoma in situ of the breast: an early event in tumorigenesis. Br J Cancer. 1997;76:1131–3.
Aulmann S, Penzel R, Longerich T, Funke B, Schirmacher P, Sinn HP. Clonality of lobular carcinoma in situ (LCIS) and metachronous invasive breast cancer. Breast Cancer Res Treat. 2008;107:331–5.
Begg CB, Ostrovnaya I, Carniello JV, Sakr RA, Giri D, Towers R, et al. Clonal relationships between lobular carcinoma in situ and other breast malignancies. Breast Cancer Res. 2016;18:66.
Sakr RA, Schizas M, Carniello JV, Ng CK, Piscuoglio S, Giri D, et al. Targeted capture massively parallel sequencing analysis of LCIS and invasive lobular cancer: repertoire of somatic genetic alterations and clonal relationships. Mol Oncol. 2016;10:360–70.
Shah V, Nowinski S, Levi D, Shinomiya I, Kebaier Ep Chaabouni N, Gillett C, et al. PIK3CA mutations are common in lobular carcinoma in situ, but are not a biomarker of progression. Breast Cancer Res. 2017;19:7.
Schrader KA, Masciari S, Boyd N, Salamanca C, Senz J, Saunders DN, et al. Germline mutations in CDH1 are infrequent in women with early-onset or familial lobular breast cancers. J Med Genet. 2011;48:64–8.
Gupta SK, Douglas-Jones AG, Jasani B, Morgan JM, Pignatelli M, Mansel RE. E-cadherin (E-cad) expression in duct carcinoma in situ (DCIS) of the breast. Virchows Arch. 1997;430:23–8.
Jorns J, Sabel MS, Pang JC. Lobular neoplasia: morphology and management. Arch Pathol Lab Med. 2014;138:1344–9.
Dabbs DJ, Schnitt SJ, Geyer FC, Weigelt B, Baehner FL, Decker T, et al. Lobular neoplasia of the breast revisited with emphasis on the role of E-cadherin immunohistochemistry. Am J Surg Pathol. 2013;37:e1–11.
Atkins KA, Cohen MA, Nicholson B, Rao S. Atypical lobular hyperplasia and lobular carcinoma in situ at core breast biopsy: use of careful radiologic-pathologic correlation to recommend excision or observation. Radiology. 2013;269:340–7.
Hwang H, Barke LD, Mendelson EB, Susnik B. Atypical lobular hyperplasia and classic lobular carcinoma in situ in core biopsy specimens: routine excision is not necessary. Mod Pathol. 2008;21:1208–16.
Murray MP, Luedtke C, Liberman L, Nehhozina T, Akram M, Brogi E. Classic lobular carcinoma in situ and atypical lobular hyperplasia at percutaneous breast core biopsy: outcomes of prospective excision. Cancer. 2013;119:1073–9.
Nakhlis F, Gilmore L, Gelman R, Bedrosian I, Ludwig K, Hwang ES, et al. Incidence of adjacent synchronous invasive carcinoma and/or ductal carcinoma in-situ in patients with lobular neoplasia on core biopsy: results from a prospective multi-institutional registry (TBCRC 020). Ann Surg Oncol. 2016;23:722–8.
Renshaw AA, Derhagopian RP, Martinez P, Gould EW. Lobular neoplasia in breast core needle biopsy specimens is associated with a low risk of ductal carcinoma in situ or invasive carcinoma on subsequent excision. Am J Clin Pathol. 2006;126:310–3.
Rendi MH, Dintzis SM, Lehman CD, Calhoun KE, Allison KH. Lobular in-situ neoplasia on breast core needle biopsy: imaging indication and pathologic extent can identify which patients require excisional biopsy. Ann Surg Oncol. 2012;19:914–21.
Susnik B, Day D, Abeln E, Bowman T, Krueger J, Swenson KK, et al. Surgical outcomes of lobular neoplasia diagnosed in core biopsy: prospective study of 316 cases. Clin Breast Cancer. 2016;16:507–13.
Downs-Kelly E, Bell D, Perkins GH, Sneige N, Middleton LP. Clinical implications of margin involvement by pleomorphic lobular carcinoma in situ. Arch Pathol Lab Med. 2011;135:737–43.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sokolova, A., Lakhani, S.R. Lobular carcinoma in situ: diagnostic criteria and molecular correlates. Mod Pathol 34 (Suppl 1), 8–14 (2021). https://doi.org/10.1038/s41379-020-00689-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-00689-3
This article is cited by
-
Immediate and delayed risk of breast cancer associated with classic lobular carcinoma in situ and its variants
Breast Cancer Research and Treatment (2024)
-
Invasive lobular carcinoma of the breast: the increasing importance of this special subtype
Breast Cancer Research (2021)
-
Machine learning-based image analysis for accelerating the diagnosis of complicated preneoplastic and neoplastic ductal lesions in breast biopsy tissues
Breast Cancer Research and Treatment (2021)