Abstract
Intrahepatic cholangiocarcinomas (iCCs) are primary tumors of the liver characterized by the presence of a desmoplastic stroma. While tumor stroma may have a protective or a pejorative value depending on the type of malignant disease, the precise role of the desmoplastic stroma in iCC remains poorly understood. The aim of the present study was to evaluate the prognostic value of stromal compartment in iCC through a multiparametric morphological analysis. Forty-nine surgically resected iCCs were included. For all cases, tumor paraffin blocks of iCCs were selected for stromal morphological characterization through quantitative and qualitative approaches using immunohistochemistry and second-harmonic generation imaging. Intratumor heterogeneity was also evaluated in regards with the different stromal features. High proportionated stromal area (PSA) (defined by stromal to tumor area ratio) was inversely correlated with vascular invasion (62.5% vs 95.7%, p = 0.006) and positively correlated with well-differentiated grade (60% vs 12.5%, p = 0.001). Patients with high PSA had a better disease-free survival (DFS) than patients with low stromal area (60% vs 10%, p = 0.077). Low activated stroma index (defined by cancer-associated fibroblasts number to stromal area ratio) was associated with a better DFS (60% vs 10%, p = 0.05). High collagen reticulation index (CRI), defined as the number of collagen fiber branches within the entire length of the collagen network, was associated with a poorer overall survival (42% vs NR, p = 0.026). Furthermore, we showed that CRI was also an homogeneous marker throughout the tumor. Based on morphological features, desmoplastic stroma seems to exert a protective effect in patients with iCC. Stromal collagen reticulation may provide additional clinically relevant information. In addition, these data support the potential value to evaluate CRI in biopsy specimen.
Similar content being viewed by others
Introduction
Intrahepatic cholangiocarcinoma (iCC) represents the second most frequent primary malignancy of the liver, accounting for 10–15% of all primary liver cancers [1]. Up to now, iCC remains associated with a poor prognosis with an overall survival (OS) barely reaching 5% at 5 years, mainly due to lack of effective chemotherapy regimen [2]. Morphologically, iCCs are characterized by an abundant desmoplastic stroma, which refers to growth of dense connective tissue, characterized by low cellularity with hyalinized or sclerotic collagen fibers and disorganized blood vessel infiltration. It is mostly composed of activated stellate cells (also known as cancer-associated fibroblasts, CAFs), which produce and secrete extracellular matrix (ECM) proteins [3, 4]. It is now well recognized that tumor stroma is a dynamic compartment potentially involved in overall prognosis [5]. Beyond the amount of stroma, increasing evidence highlighted the importance of its 3D structural network, which may impair the biodisponibility of antineoplastic agents. In this setting, studying the different constituents of the tumor stroma and their respective role could represent a promising axis in order to identify new therapeutic targets.
Molecularly, two prognostic classes of iCC have been described. These include the “proliferative” and the “inflammatory” classes, which are associated with poorer and better survivals, respectively [6]. Although no genotype/phenotype correlations have been specifically studied, available molecular data may suggest a potential role of immune cell infiltration within iCC, especially in the therapeutic era of immune checkpoint inhibitors [7]. In addition, characteristics of the fibrous component in terms of cell density and ECM architecture may also impact the prognosis of iCC, similarly to what has been reported in hepatocellular carcinoma where tumor encapsulation was related to less aggressive tumor with lower invasion and venous permeation, and better outcome [8].
Hence, the aims of our study were to provide a precise description of tumor stroma in a set of iCCs by focusing on fibrous (CAF density, activity, and ECM architecture) compartment, and to assess the impact of their spatial distribution. To address these issues, we applied a multimodal approach, based on morphological, immunophenotypical, and second-harmonic generation (SHG) techniques on a surgical series of 49 resected iCCs.
Materials and methods
Patients and samples
Forty-nine surgically resected small ducts iCC cases retrieved from the surgical pathology files of Beaujon Hospital from 2002 to 2014 were included. None of the cases received preoperative treatment and informed consent was obtained in all cases. The study was approved by the local institutional review board CPPRB No. 2019-022.
The following clinicopathological data were collected: age, gender, presence and type of underlying chronic liver disease, tumor size, presence of satellite nodules, lymph node metastasis, R0 resection, and pTNM stage according the 7th edition of the AJCC. Satellite nodules were defined as well-circumscribed accessory malignant nodule clearly separated from the main tumor and with identical histologic characteristics. Follow-up data were obtained from the medical records, including tumor recurrence, DFS and OS.
Pathological analysis
All cases were reviewed by two experienced pathologists specialized in liver diseases (NG, VP). The following histological features were assessed: tumor differentiation (well, moderate, and poor), lymph node metastasis, perineural involvement, and vascular invasion on hematein and eosin (H&E) staining. The most representative slide section covering tumor and nontumoral liver was selected for sirius red staining and immunohistochemical analysis.
Quantitative analysis of iCC stroma
For all cases, sirius red stainings were scanned (ScanScope AT turbo®, Leica) at ×20 magnification, and digital images were analyzed using a dedicated algorithm positive pixel (Indica Labs, Albuquerque) to estimate the PSA defined as the ratio between the red stained tumor area (corresponding to the fibrous area) and the total tumor section (Fig. 1). Positive pixels (red stained pixel defined by RGB composite) were quantified by algorithm on total pixels (total tumor area) detected. Tumor area was previously delimited by the pathologist (ImageScope, Leica). The pattern of tumor invasion was considered on H&E and sirius red stainings as either noninvasive when the tumor was separated from the liver parenchyma by collagen bundles forming a fibrous pseudocapsule representing at least 50% of the circumference of the interface tumor/nontumoral liver, or as invasive when tumor cells were directly in close contact with the nontumoral liver (Fig. 2a, b).
Immunohistochemistry
Tumor stroma was phenotypically characterized by immunohistochemistry on whole tumor paraffin section using a panel of antibodies related to CAF [alpha-smooth muscle actin (AML, 1:500, clone M851, Dako)], microvessel density (MVD) [CD31 (1:200, M82301, Dako)], and ECM protein [periostin (1/1500, EPR19936, Abcam)]. An automated immunohistochemical stainer was used according to the manufacturer’s guidelines (streptavidin-peroxidase protocol; Benchmark, Ventana, Tucson, AZ). All markers were quantitatively assessed using an algorithm detecting pixels with DAB staining (ratio of stained pixels on total pixels) except for CD31 staining for which a dedicated algorithm (Indica Labs) was used. For all cases, activated stroma index (ASI) was obtained by calculating the ratio between the area of AML positive cells and the area of collagen stained by sirius red staining.
Collagen profile analysis and characterization
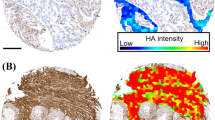
In addition to the quantitative analysis of tumor stroma, qualitative aspect was also investigated in terms of collagen density and 3D structure by SHG and two photon excitation fluorescence (TPEF) microscopy (HistoIndex Pte Ltd).This morphological approach was applied on tissue microarrays (TMA) from a subset of 26 iCCs. Five to seven tissue cores of 1 mm each were punched from the most representative tumor areas in all cases and brought into a recipient paraffin block at defined array coordinates using a tissue-arraying instrument (MTA-1, Beecher Instruments, Inc, Sun Prairie, WI). A total of 147 unstained cores were imaged on ×20 objective by the laser-based Genesis 200 multiphoton imaging system.
SHG signals were detected when a laser of femtosecond range interacts with tissues that have unique (noncentrosymetric) structure within the ECM such as collagen fibers and elastin. When this SHG signal was combined with autofluorescence signal from the cells using TPEF, multiphoton imaging is able to penetrate deep into tissues to generate a high-resolution image that reflects both the architecture of the ECM and surrounding cellular structure. Embedded within the proprietary stain-free imaging technology and analysis software lies the capability to detect and quantify fine collagen dynamics that are otherwise unobserved with traditional staining techniques. The analysis provided by Clinnovate Health UK Ltd identified and characterized specific SHG collagen characteristics that corresponded with the stroma profile of the severity of cancer grades, in terms of various parameters (Table 1) including collagen area ratio (CAR), which is defined as the relative amount of collagen compared to the total region of interest, collagen tissue proportion (CTP) defined by the relative amount of collagen compared to the total tissue area, and collagen reticulation index (CRI) defined as a measure of number of collagen fiber branches within the entire length of the collagen network. Intratumoral heterogeneity in terms of stromal features was investigated for all available parameters between the different tissue cores from each iCC case.
Statistical analysis
Continuous variables are presented as median (range) and were compared using the student’s test or the Mann–Whitney U test, as appropriate. Categorical variables are shown as numbers with percentages, and were compared using chi square or Fisher’s exact test. For survival analyses, variables of interest were categorized as high or low when higher or lower than the median value of a given variable. Heterogeneity of tumor markers (CAR, TAR, SCAR, UCAR, CFD, UFCD, CART, SCART, UCART, CTP, TD, CFDT, CRI, CARD, TRI, TARD) (defined in Table 1) was assessed on TMAs cores from 27 tumor samples. Four to six TMAs cores were available for each tumor sample. For each marker, median and IQR 25–75% of all TMA values were calculated from the analysis of all TMA core values of all samples for a given marker (27 samples with 4–6 TMA cores, total of TMA cores n = 147 values for each marker). Thereafter, each individual TMA core value was categorized in the following IQRs: <IQR 25%; between IQR 25–75% and >IQR 75% for each marker. Thereafter, the homogeneity of a given marker between cores of a given tumor sample was considered when more than 2/3 of the values belonged to the same IQR. Finally, the percentage of samples with homogeneous TMA core values was calculated for each marker. Overall and recurrence-free survival were calculated according to Kaplan–Meier method. All statistical tests were two-sided, and p ≤ 0.050 was considered statistically significant in all analyses. Statistical analyses were performed with Excelstats and Prism® and SPSS® version 24.0 (IBM, Armonk, New York, USA).
Results
Patients
The study population consisted of 22 (44.9%) males and 27 (55.1%) females. Mean age was 61 years (range 28–79). The main clinicopathological characteristics are summarized in Table 2. The mean tumor size was 77.8 mm. Eighteen (37%) tumors were well differentiated, 23 (47%) were moderately differentiated, and 8 (16%) were poorly differentiated. Median follow-up was 36.3 months (range 1.2–162.0), and median OS was 40.5 months. OS rates at 1, 3, and 5 years were 87.4%, 57.2%, and 36.8%, respectively. Recurrence occurred in 31 (63%) patients. Median DFS was 19.5 months. DFS rates at 1, 3, and 5 years were 55.3%, 43.6%, and 34.5%, respectively.
PSA, ASI, and tumor invasion pattern
In the overall series, median PSA value was 44.65. Patients with high PSA showed a trend toward better DFS than patients with low PSA (60 months vs 10 months, p = 0.077). Furthermore, tumors with high PSA were associated with lower rate of vascular invasion (62.5% vs 95.7%, p = 0.006) and higher rate of well-differentiated grade (60% vs 12.5%, p = 0.001). These data suggest that high PSA tumors define a group of better phenotype.
Median ASI value was 14.13. Low ASI, corresponding to poorly cellular stroma, was significantly associated with improved DFS (60 months vs 10 months, p = 0.050). ASI was not correlated with OS and was not found to be significant in multivariate analysis both with DFS and OS.
The noninvasive pattern of tumor growth, defined by the presence of a fibrous border, was significantly associated with a better OS compared to the invasive pattern (40 months vs not reached, p = 0.016).
Stromal features according to SHG microscopy and tumor heterogeneity
Median CAR, CTP, and CRI values were 34.95, 0.52, and 2.76, respectively. High CAR and CTP were significantly associated with improved DFS (9.8 vs 60.1 months, p = 0.041) and (9.0 vs 60.1 months, p = 0.013), respectively. CAR and CTP were not correlated with OS. High CRI patients were significantly associated with poorer OS (not reached vs 42 months, p = 0.026). CRI parameter was not found to be significant in multivariate analysis both with OS and DFS.
In order to evaluate potential intratumoral heterogeneity of stromal features in iCC, the 16 stromal features obtained by SHG microscopy were analyzed tissue core per tissue core from a total of 147 tissue cores available for 27 tumor samples (mean of 5.4 cores per patient, range 4–6). Median (IQR 25–75) TMA core values and percentages of homogeneous samples for each marker are provided in Table 3. Eleven (CAR, TAR, SCAR, UFCD, CART, SCART, CTP, TD, CFDT, TRI, and TARD) out of 16 markers were homogeneous in less than 50% of the cases. Only one marker (CRI) showed homogeneity in more than 70% of the cases. Figure 3 illustrates representative cores of two different iCCs.
MVD and periostin expression
Median value of MVD was 5.47E−5. On univariate, high MVD was significantly associated with poorer DFS (60.0 vs 10.5 months, p = 0.050). MVD was an independent prognostic factor on multivariate analysis (p = 0.007). Figure 4b–d illustrates MVD using CD31 immunostaining.
a Immunostaining of smooth muscle actin (magnification ×250): cancer-associated fibroblasts are immunostained (red). b Immunostaining of CD31: intratumoral vessels are immunostained (brown, magnification ×400). c Immunostaining of periostin: mild positivity in the stromal part, mostly in the extracellular compartment (magnification ×250). d Automated quantification of MVD using a specific algorithm (Indica Labs). Vessels immunostained by CD31 were automatically contouring in green.
A total of 28 iCCs (57%) were positive for periostin by immunohistochemistry, with a mild staining in the stromal part of the tumor (Fig. 4c). Median value of periostin expression was 0.118. On univariate analysis, high expression of periostin was not significant with OS (42 months vs 45.5 months, p = 0.929) and with DFS (23.6 months vs 14.9 months p = 0.920). All results are detailed in Tables 4 and 5.
Discussion
iCCs are characterized by an extensive and desmoplastic fibrous stroma, which surrounds and infiltrates tumor proliferation. In addition to its diagnostic value, used on imaging and pathology, the desmoplastic feature may yield a prognostic value as it supports tumor growth and may be targeted [9]. Indeed, it remains unclear whether such a desmoplastic reaction represents a host barrier against neoplastic invasiveness or, on the contrary, promotes tumor invasion. Using combined morphological analysis of the stromal compartment, we identified two different types of iCCs, the more fibrous and less cellular (defining desmoplasia) being associated with better outcome. These data are in agreement with previous studies showing a better survival in colorectal carcinomas and pancreatic carcinoma patients with desmoplasia [10,11,12,13,14]. In addition, using SHG imaging allowing the 3D analysis of stromal compartment, iCC with high CAR, which reflects CAR, displayed improved survival. As previously reported in colorectal liver metastases and hepatocellular carcinoma [8, 15], we also observed the presence of a fibrous capsule at the interface between iCC and peritumoral liver, namely as “noninvasive pattern” in as much as 50% of the tumors, which a significant impact on the prognosis. Altogether, these data support the protective role of a desmoplastic stroma in iCC, potentially through a limitation of tumor invasiveness by building a barrier against tumor diffusion, similarly to wound healing, within and at the periphery of the tumor [16,17,18]. In line with these results, Barsky et al. showed that inhibition of desmoplastic response by daily injection of L34 dehydroproline led to an increase in spontaneous metastasis in experimental murine melanomas [19].
Periostin is a modular glycoprotein frequently observed to be a major constituent of the extracellular milieu of mass-forming iCC. In iCC, periostin is overexpressed and hypersecreted in large part, if not exclusively, by CAFs within the tumor stroma [20]. High periostin expression, assessed by immunostaining, was reported as an independent risk factor for the poor prognosis of ICC patients after hepatectomy [21]. In our study, we failed to find periostin expression significant in terms of survival. This discrepancy can be explained by a different method of quantifying periostin expression. Indeed, while we used an automated quantification, Utispan et al. performed a semiquantitative analysis.
In addition to classical features of stroma reaction in iCC, we also aimed at investigating the prognostic role of collagen cross-linkings. To such end, we performed SHG microscopy analysis, which has been mainly used to selectively investigate collagen fiber orientation and their structural changes within tumor microenvironment [22,23,24]. Using this approach, we observed that patients with tumor displaying high degree of collagen cross-linkings had a worsened prognosis. These results are in accordance with those of Levental et al. who established a correlation between collagen crosslinking and matrix stiffness in vivo but also implicating the ECM crosslinking enzyme lysyl oxidase (LOX) as a culprit driving stiffness associated tumor progression [25]. Interestingly, Bergeat et al. described an overexpression of LOXL2, a LOX, in tumor stroma of iCC. They showed that high expression of LOXL2 was an independent prognostic factor of worse OS and DFS [26].
Tumor heterogeneity is a common hallmark of cancer, and especially iCC. Beyond molecular heterogeneity, we were interested to investigate the potential heterogeneity of stromal features within tumor. As expected, parameters reflecting quantitative aspect of stroma reaction showed significant heterogeneity between core samples. However, we showed that CRI, a qualitative feature reflecting degree of reticulation, is homogeneous throughout the tumor. In addition, CRI was also associated with prognosis. Altogether, these data support the potential value to evaluate CRI in biopsy specimen.
Angiogenesis, which is defined as the development of new blood vessels from preexisting vasculature, has become a well-established hallmark of cancer [27, 28]. Angiogenesis maintains the aggressive growth and metastatic potential of tumors by supplying nutrients and oxygen [29]. Vascular endothelial growth factor A (VEGFA) has an important role in tumor angiogenesis and correlates with vessel count in various solid cancers [30,31,32]. Patients with solid tumors with a high MVD exhibited shorter survival than patients with a low MVD [33,34,35,36]. In line with previous findings, we observed that iCC with high MVD had a worse prognosis than iCC with low MVD. Interestingly, a novel molecular mechanism for increased angiogenesis resulting from the interaction between LOXL2 and GATA6 that enhances VEGFA expression, and promotes angiogenesis and tumor growth in iCC has been reported [37]. In agreement with this and previous data, LOX2 could represent an interesting therapeutic target to study.
As far as DFS is concerned, only MVD and satellite nodules, which may reflect angiogenesis and cell dissemination, were independent factors. As far as OS is concerned, none of the features identified in the univariate analysis were found independent.
As far as we know, morphological analysis focusing on tumor stroma reaction including SHG approach is limited. However, we acknowledge that the present study yields several limitations. First, the limited sample size is likely to lead to insufficient statistical power and comparative results should be interpreted with caution. Second, the prolonged study period associated with retrospective collection of clinical data may have led to suboptimal data analysis. Finally and above all, the present study only included surgically resected specimen. This obviously introduces a selection bias as only iCC patients with the most favorable prognosis were included. Hence, results of the present study should be confirmed on biopsy specimen arising from locally advanced or metastatic lesions. However, the reported results provide original insights regarding the influence of tumor stroma. The next logical step would be to analyze the influence of perioperative chemotherapy, including validated regimen but also immunotherapies and specifically targeted therapies according to the nature of the stroma.
To conclude, by combining morphological approaches focusing on tumor stroma, we were able to identify two main groups of iCCs associated with prognostic value. This also supports the potential benefit to develop therapeutic strategies targeting the tumor microenvironment of iCC, especially drugs able to modulate reticulation and angiogenesis properties, such as lysyl oxydase enzyme. Furthermore, we identified CRI as an homogenous marker throughout the tumor, suggesting that this feature may be relevant to assess in biopsy specimen.
References
Razumilava N, Gores GJ. Cholangiocarcinoma. Lancet. 2014;383:2168–79.
Rizvi S, Khan SA, Hallemeier CL, Kelley RK, Gores GJ. Cholangiocarcinoma—evolving concepts and therapeutic strategies. Nat Rev Clin Oncol. 2018;15:95–111.
Krasinskas AM. Cholangiocarcinoma. Surg Pathol Clin. 2018;11:403–29.
Zhang X-F, Dong M, Pan Y-H, Chen JN, Huang XQ, Jin Y, et al. Expression pattern of cancer-associated fibroblast and its clinical relevance in intrahepatic cholangiocarcinoma. Hum Pathol. 2017;65:92–100.
Cadamuro M, Stecca T, Brivio S, Mariotti V, Fiorotto R. The deleterious interplay between tumor epithelia and stroma in cholangiocarcinoma. Biochim Biophys Acta Mol Basis Dis. 2018;1864:1435–43.
Sia D, Villanueva A, Friedman SL, Llovet JM. Liver cancer cell of origin, molecular class, and effects on patient prognosis. Gastroenterology. 2017;152:745–61.
Darvin P, Toor SM, Sasidharan Nair V, Elkord E. Immune checkpoint inhibitors: recent progress and potential biomarkers. Exp Mol Med. 2018;50:1–11.
Nagao T, Inoue S, Goto S, Mizuta T, Omori Y, Kawano N, et al. Hepatic resection for hepatocellular carcinoma. Clinical features and long-term prognosis. Ann Surg. 1987;205:33–40.
Høgdall D, Lewinska M, Andersen JB. Desmoplastic tumor microenvironment and immunotherapy in cholangiocarcinoma. Trends Cancer. 2018;4:239–55.
Erkan M, Michalski CW, Rieder S, Reiser-Erkan C, Abiatari I, Kolb A, et al. The activated stroma index is a novel and independent prognostic marker in pancreatic ductal adenocarcinoma. Clin Gastroenterol Hepatol. 2008;6:1155–61.
Caporale A, Vestri AR, Benvenuto E, Mariotti M, Cosenza UM, Scarpini M, et al. Is desmoplasia a protective factor for survival in patients with colorectal carcinoma? Clin Gastroenterol Hepatol. 2005;3:370–5.
Caporale A, Amore Bonapasta S, Scarpini M, Ciardi A, Vestri A, Ruperto M, et al. Quantitative investigation of desmoplasia as a prognostic indicator in colorectal cancer. J Investig Surg. 2010;23:105–9.
Wang LM, Silva MA, D’Costa Z, Bockelmann R, Soonawalla Z, Liu S, et al. The prognostic role of desmoplastic stroma in pancreatic ductal adenocarcinoma. Oncotarget. 2016;7:4183–94.
Sinn M, Denkert C, Striefler JK, Pelzer U, Stieler JM, Bahra M, et al. α-Smooth muscle actin expression and desmoplastic stromal reaction in pancreatic cancer: results from the CONKO-001 study. Br J Cancer. 2014;111:1917–23.
Okano K, Yamamoto J, Kosuge T, Yamamoto S, Sakamoto M, Nakanishi Y, et al. Fibrous pseudocapsule of metastatic liver tumors from colorectal carcinoma. Clinicopathologic study of 152 first resection cases. Cancer. 2000;89:267–75.
Dvorak HF. Tumors: wounds that do not heal-redux. Cancer Immunol Res. 2015;3:1–11.
Erkan M. Understanding the stroma of pancreatic cancer: co-evolution of the microenvironment with epithelial carcinogenesis. J Pathol. 2013;231:4–7.
Zeisberg M, Kalluri R. Cellular mechanisms of tissue fibrosis. 1. Common and organ-specific mechanisms associated with tissue fibrosis. Am J Physiol, Cell Physiol. 2013;304:C216–225.
Barsky SH, Gopalakrishna R. Increased invasion and spontaneous metastasis of BL6 melanoma with inhibition of the desmoplastic response in C57 BL/6 mice. Cancer Res. 1987;47:1663–7.
Sirica AE, Almenara JA, Li C. Periostin in intrahepatic cholangiocarcinoma: pathobiological insights and clinical implications. Exp Mol Pathol. 2014;97:515–24.
Utispan K, Thuwajit P, Abiko Y, Charngkaew K, Paupairoj A, Chau-in S, et al. Gene expression profiling of cholangiocarcinoma-derived fibroblast reveals alterations related to tumor progression and indicates periostin as a poor prognostic marker. Mol Cancer. 2010;9:13.
Natal RA, Vassallo J, Paiva GR, Pelegati VB, Barbosa GO, Mendonça G, et al. Collagen analysis by second-harmonic generation microscopy predicts outcome of luminal breast cancer. Tumour Biol. 2018;40:1010428318770953.
Okoro C, Kelkar V, Sivaguru M, Emmadi R, Toussaint KC. Second-harmonic patterned polarization-analyzed reflection confocal microscopy of stromal collagen in benign and malignant breast tissues. Sci Rep. 2018;8:16243.
Zhou Z-H, Ji C-D, Xiao H-L, Zhao HB, Cui YH, Bian XW. Reorganized collagen in the tumor microenvironment of gastric cancer and its association with prognosis. J Cancer. 2017;8:1466–76.
Levental KR, Yu H, Kass L, Lakins JN, Egeblad M, Erler JT, et al. Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell. 2009;139:891–906.
Bergeat D, Fautrel A, Turlin B, Merdrignac A, Rayar M, Boudjema K, et al. Impact of stroma LOXL2 overexpression on the prognosis of intrahepatic cholangiocarcinoma. J Surg Res. 2016;203:441–50.
Jayson GC, Kerbel R, Ellis LM, Harris AL. Antiangiogenic therapy in oncology: current status and future directions. Lancet. 2016;388:518–29.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74.
Butler JM, Kobayashi H, Rafii S. Instructive role of the vascular niche in promoting tumour growth and tissue repair by angiocrine factors. Nat Rev Cancer. 2010;10:138–46.
Kim KJ, Li B, Winer J, Armanini M, Gillett M, Phillips HS, et al. Inhibition of vascular endothelial growth factor-induced angiogenesis suppresses tumour growth in vivo. Nature. 1993;362:841–4.
Takahashi Y, Kitadai Y, Bucana CD, Cleary KR, Ellis LM. Expression of vascular endothelial growth factor and its receptor, KDR, correlates with vascularity, metastasis, and proliferation of human colon cancer. Cancer Res. 1995;55:3964–8.
Koh YW, Han J-H, Yoon DH, Suh C, Huh J. PD-L1 expression correlates with VEGF and microvessel density in patients with uniformly treated classical Hodgkin lymphoma. Ann Hematol. 2017;96:1883–90.
Benckert C, Thelen A, Cramer T, Weichert W, Gaebelein G, Gessner R, et al. Impact of microvessel density on lymph node metastasis and survival after curative resection of pancreatic cancer. Surg Today. 2012;42:169–76.
Tynninen O, Sjöström J, von Boguslawski K, Bengtsson NO, Heikkilä R, Malmström P, et al. Tumour microvessel density as predictor of chemotherapy response in breast cancer patients. Br J Cancer. 2002;86:1905–8.
Thelen A, Scholz A, Weichert W, Wiedenmann B, Neuhaus P, Gessner R, et al. Tumor-associated angiogenesis and lymphangiogenesis correlate with progression of intrahepatic cholangiocarcinoma. Am J Gastroenterol. 2010;105:1123–32.
Möbius C, Demuth C, Aigner T, Wiedmann M, Wittekind C, Mössner J, et al. Evaluation of VEGF A expression and microvascular density as prognostic factors in extrahepatic cholangiocarcinoma. Eur J Surg Oncol. 2007;33:1025–9.
Peng T, Deng X, Tian F, Li Z, Jiang P, Zhao X, et al. The interaction of LOXL2 with GATA6 induces VEGFA expression and angiogenesis in cholangiocarcinoma. Int J Oncol. 2019;55. https://doi.org/10.3892/ijo.2019.4837.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guedj, N., Blaise, L., Cauchy, F. et al. Prognostic value of desmoplastic stroma in intrahepatic cholangiocarcinoma. Mod Pathol 34, 408–416 (2021). https://doi.org/10.1038/s41379-020-00656-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-00656-y
This article is cited by
-
Spatiotemporal regulation of cholangiocarcinoma growth and dissemination by peritumoral myofibroblasts in a Vcam1-dependent manner
Oncogene (2023)
-
Friend or foe? The elusive role of hepatic stellate cells in liver cancer
Nature Reviews Gastroenterology & Hepatology (2023)
-
Apparent diffusion coefficient correlates with different histopathological features in several intrahepatic tumors
European Radiology (2023)
-
Advances of cancer-associated fibroblasts in liver cancer
Biomarker Research (2022)
-
Immunophenotypic and molecular characterization of pancreatic neuroendocrine tumors producing serotonin
Modern Pathology (2022)