Abstract
Merkel cell carcinoma is an aggressive neuroendocrine skin tumor, for which several non-conclusive prognostic factors of adverse clinical behavior have been reported. As promoter methylation of the immune checkpoint receptor CD279/PD-1/PDCD1(mPDCD1) has been shown to be a prognostic factor in different cancers, we investigated its role in Merkel cell carcinoma. mPDCD1was assessed retrospectively in a cohort of 69 Merkel cell carcinoma patients from the University of Bologna, University of Turin and University of Insubria. Kaplan-Meier curves and log-rank tests were calculated for all variables. To assess the influence of mPDCD1, the Cox proportional hazards model and different Royston-Parmar models were evaluated. High PDCD1 methylation (mPDCD1high) was associated with a higher overall mortality at both the univariate analysis (log rank test: χ2 = 5.17, p = 0.023; permutation test: p = 0.023) and the multivariate analysis (HR = 2.111, p = 0.042). The other variables associated with a higher overall mortality at the multivariate analysis were clinical stage III-IV (HR = 2.357, p = 0.008), size > 2 cm (HR = 2.248, p = 0.031) and Merkel cell polyomavirus (HR = 0.397, p = 0.015). Further, mPDCD1high was strongly associated with older age (81 vs 76 years, p = 0.042), absence of immune cells (92.6%, p < 0.001), no expression of PD-L1 by immune cells (70.4%, p = 0.041) and by both immune and tumor cells (70.4%, p = 0.001). mPDCD1 is a valid prognostic parameter in patients affected by Merkel cell carcinoma. In addition, it could provide an estimate of the global PD-1/PD-L1 expression with potentially relevant implications from a therapeutic point of view.
Similar content being viewed by others
Introduction
Merkel cell carcinoma is an aggressive neuroendocrine skin tumor, mostly affecting elderly individuals [1, 2]. Although Merkel cell carcinoma is rare, with an annual incidence of 0.79 per 100,000 people in the United States, its frequency is increasing probably due to ageing of the population, improvement of diagnostic tools, and increase of risk-factors [3]. Several non-conclusive predictors of adverse clinical behavior have been reported, including age > 55 years, head and neck localization, immunosuppression, tumor thickness, >10 mitoses per single high-power field, and many others [4, 5]. Previously, we reported that p63 expression is an independent prognostic marker in Merkel cell carcinoma, especially in localized disease (stage I-II) [6, 7]. So far, there is no definitively established prognostic marker in Merkel cell carcinoma, except for UICC/AJCC clinical and pathologic staging [4]. Despite intensive treatment, Merkel cell carcinoma has an unsatisfactory outcome, with a 5-year overall mortality of about 33%, more than twice that observed in cutaneous melanoma [4, 8, 9]. Furthermore, chemotherapy regimens have obtained discouraging results of chemotherapy in advanced Merkel cell carcinoma (stage III-IV). As several lines of evidence support Merkel cell carcinoma as the paradigm of immunogenic cancer, different trials involving immune check-point blocking agents (avelumab, pembrolizumab and nivolumab) have been started [10,11,12,13]. As promoter methylation of the immune checkpoint receptor CD279/PD-1/PDCD1(mPDCD1) has been shown to be a prognostic factor in different cancers [14,15,16], we investigated whether mPDCD1 is independently associated with overall mortality in Merkel cell carcinoma patients and its relationship with several clinic-pathological features. Furthermore, mPDCD1 was correlated with immunohistochemical assessment of PD-L1 for better insight into the PD-1/PD-L1 pathway in Merkel cell carcinoma.
Materials and methods
Patients and specimens
This is a multicentric study enrolling 69 subjects from three different Italian University Hospitals: University of Bologna (31 cases), University of Turin (31 cases) and University of Insubria (7 cases). Patients with a diagnosis of Merkel cell carcinoma from 1990 to 2015 were enrolled in the study and followed up until 31 December 2017, or death. Clinical parameters (patient age, sex, tumor site, tumor size, clinical lymph node evaluation) and follow up data (outcome and overall survival) were obtained by clinical registries of the centers and are summarized in Table 1. All tumors were re-staged according to the 8th edition of the AJCC Cancer Staging Manual [4]. Tissues were fixed in 10% formalin, embedded in paraffin and stained with hematoxylin and eosin (H&E). Slides from each case were reviewed by four pathologists (S.A., S.U., S.L.R., F.M.) to confirm the diagnosis of Merkel cell carcinoma, to assess pathological data (tumor thickness, angioinvasion, mitotic count, pattern of growth, immune cells) and to choose one representative paraffin block for additional analyses. In this study, we evaluated the immune cells rather than the tumor-infiltrating lymphocytes as previously reported [17, 18]. Immune cells has been defined as immune infiltrates including T and B-lymphocytes, monocytes and myeloid-derived suppressor cells [17, 18]. For lymph node metastatic Merkel cell carcinoma with unknown primary tumor (cases 2, 13, 16, and 18; see Table 1), immune cells evaluation was restricted to those with immune cells permeating the metastatic deposits. Cases with immune cells bordering the metastatic deposits were considered immune cells-negative.
Immunohistochemistry
Immunohistochemistry was performed on formalin-fixed, paraffin embedded tissue using following antibodies: PD-L1 (clone 123 C3SP142, Ventana-Diapath, dilution 1:50), CD3 (clone 2GV6, Ventana-Diapath, dilution RTU), cytokeratin 20 (CK 20, clone SP33, Ventana, dilution RTU), Synpatophysin (SP 11 mono-rabbit,Neomarkers, Fremont, CA, 1:100), Chromogranin A (clone LK2H10, Ventana, dilution RTU), Thyroid Trascript Factor-1 (TTF-1, clone 847G3/1, Ventana, dilution RTU), Ki67 (clone MIB-1, Dako, dilution 1:100), Merkel cell polyoma virus (MCPyV, clone CM2B4, Santa Cruz Biotechnology Inc, dilution 1:50).
PD-L1 immunohistochemical assessment in immune cells and tumor cells
The PD-L1 immunohistochemical assessment for Merkel cell carcinoma suggested by Lipson et al. has been applied [18]. Percentages of tumor cells or immune cells, demonstrating membranous PD-L1 expression were scored on a representative slide from each case by three independent pathologists (S.A., S.U., F.M.), who were blinded to clinical outcomes. Cases with at least 5% of PD-L1 membranous expression were considered positive. In addition, a global evaluation of PD-L1 expression was performed as follows: negative (immune cells absent and no PD-L1 expression by tumor cells or no PD-L1 expression by both the components), positive (PD-L1 expression by one of the components or by both).
Quantitative DNA methylation analysis of PDCD1 (mPDCD1)
DNA purification: DNA from macrodissected tumor tissue was digested at 56 °C for 3 hours using the Quick ExtractTM FFPE DNA extraction kit (Epicentre, Madison, WI, USA). After a denaturation step at 95 °C for 5 min, the solution was centrifuged at 10,000 × g at 4 °C for 5 min to pellet the undigested tissue and solidify the paraffin afloat. DNA ready to use for bisulfite treatment was collected from the interphase and stored at 4 °C. Bisulfite treatment of genomic DNA was carried out with the EZDNA Methylation-LightningTM Kit (Zymo Research, cod. D5031) according to the manufacturer’s protocol.
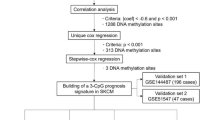
Next Generation Sequencing library preparation: A flow chart representing target enrichment, library preparation and bioinformatic data analysis is summarized in Fig. 1. Quantitative DNA methylation analysis was performed by bisulfite-Next Generation Sequencing as previously described [19], with some modifications. The library was prepared in two steps: a first multiplex PCR amplification for target enrichment, and a second round of amplification with a low number of cycles allowing the barcoding of the template-specific amplicons obtained from the first amplification step. Barcoding was performed using the NexteraTM index kit as previously described [20]. MethPrimer (http://www.urogene.org/cgi-bin/methprimer/methprimer.cgi) [21] was applied to identify CpGs and the best primers of choice for promoter of PDCD1 and PD-L1. Regions of interest and mapping coordinates are listed in Table 2. Locus-specific bisulfite amplicon libraries were generated with tagged primers using Phusion U DNA polymerase (Thermo Fisher, cod. F555L). Amplification products were purified using MagSi-NGSPREP beads (Magnamedics, GeleenThe Netherlands), quantified with Fluorometer Quantus™ (Promega, cod. E6150) and then employed as template (100 ng) for a second round of PCR (8 cycles). Sample-specific barcode sequences were added in this second PCR. The amplicon library was purified using MagSi-NGSPREP beads (Magnamedics, Geleen, The Netherlands), quantified with the Fluorometer Quantus (Promega, cod. E6150), pooled and loaded on MiSEQ (Illumina, San Diego, CA, USA, cod. 15027617) according to the manufacturer’s protocol. Next Generation Sequencing data analysis: FASTQ files were processed for quality control (>Q30) and for read lengths (>100 bp) and converted into FASTA format in a Galaxy Project environment [22]. To evaluate the methylation ratio of each CpG, we loaded FASTA files into the bisulfite sequencing pattern analysis tool (BSPAT-http://cbc.case.edu/BSPAT/index.jsp) [23]. Methylation plotter (http://gattaca.imppc.org:3838/methylation_plotter/) was used to create Fig. 2.
Flow chart representing Bisulfite Next Generation Sequencing analysis of PDCD1 and PD-L1. Formalin fixed paraffin embedded tissues were macrodissected and DNA was purified. Bisulfite treatment preceded target enrichment using primers listed in Table 2. A second low cycles PCR was then used for barcoding. Amplicons were purified by magnetic beads, quantified and pooled before loading onto MiSEQ. FASTQ files were processed for quality control (>Q30), for read lengths (>100 bp) and converted into FASTA format in a Galaxy Project environment. The methylation ratio of each CpGwas calculated using BSPAT. FFPE formalin-fixed paraffin-embedded, PCR polymerase chain reaction; BSAPT: bisulfite sequencing pattern analysis tool, mPDCD1low low level of mPDCD1, mPDCD1high high level of mPDCD1
MethPLotter PD1OD profile Methylation Profile Plot for PDCD1 methylation among different groups:dead of disease, dead of other causes, alive with disease, no evidence of disease. Each line represents for each group of samples the mean methylation for each position. Asterisks indicate a statistical significance as calculated by the Kruskal-Wallis test (KW). Position 242800974 and 242800903 are statistically significant (p < 0.05)
Statistical analysis
Methylation data were dichotomized as previously described [14]. In brief, patients were stratified according to methylation level tertiles (T1-T3) in two groups: mPDCD1high (T2/3 > 0.32) and mPDCD1low (T1 ≤ 0.32), in analogy to other graduation systems commonly used in pathologic scores (e.g., immunohistochemical staining intensity in immunoreactive scores). Regarding promoter methylation of PD-L1, we have found values very close to 0 for all cases (data not shown) and therefore no additional statistical evaluation was needed.
The study population was described and compared across subgroups using chi-square test or Fisher’s exact test when comparing categorical variables, and Mann-Whitney or Kruskal-Wallis test when comparing a continuous and a categorical variable. Post-hoc analyses of significant Kruskal-Wallis tests were conducted using Conover-Iman pairwise comparison with Bonferroni correction. Survival analysis methods were used to investigate all-cause mortality. At first, Kaplan-Meier curves and log-rank tests were calculated for all categorical variables examined singularly. Given the small size of the study population, a two-sided permutation test was run to confirm the p-values obtained by each log-rank test, randomly reassigning patients across the subgroups of each variable 10,000 times. The p-value reported by permutation test corresponds to the null hypothesis that there is no difference between subgroups, so that patients could be randomly exchanged between subgroups. To assess the influence of methylation on time to death, adjusted for possible confounders, the Cox proportional hazards model and different Royston-Parmar models were evaluated. Royston-Parmar models make assumptions about the form of the survival function, and thus could be more efficient than the Cox proportional hazards model when the baseline survival function follows a specific pattern [24]. In particular, the exponential and Weibull models impose a monotonic function to the data, while proportional hazards, loglogistic and probit spline models can be modeled to fit non-monotone functions with various turning points, according to the hypothesized number of splines. The Cox proportional hazards, the exponential and the Weibull model, and proportional hazards, loglogistic and probit models with 1 to 5 splines, were tested using the methylation indicator as predictor. Among all tested models, the one with the best fit to the data was identified by the lowest Akaike and Bayesian information criteria statistics and used for the analysis. In the multivariate survival model methylation was included as the main risk predictor, along with age, sex, clinical stage and all the other variables that in the univariate survival analyses obtained p-values ≤ 0.25. From this initial model all non-significant covariates at α = 0.05 were removed one at a time in decreasing order of p-value, to obtain a final parsimonious model. Estimations of the survival functions for specific subgroups of patients were obtained from the final model to highlight the related mortality risk. Stata v.15.1 was used for all analyses; stpm2 procedure was used to estimate Royston-Parmar models [25].
Results
Patients’ characteristics
The study cohort included 69 patients, predominantly male (55%) and with a median age at diagnosis of 77 years. Tumors were located mainly on the extremities (41%) or in the head and neck region (38%). Median tumor size was 2.5 cm, with a median tumor thickness of 12 mm. Localized disease (AJCC Clinical Stage I-II) was more prevalent (65%) than advanced disease (AJCC Clinical Stage III-IV, 35%), among which only two patients had distant metastases (3% AJCC Clinical Stage IV). Pathological stage was available only for 28 patients (41%), because at the time of enrolment, the sentinel lymph node biopsy was not routinely performed. Merely from 2010, after an extensive review of literature and analysis of a high number of cases recorded in the National Cancer Database, the recommendation for routinely performed sentinel lymph node biopsy in all patients with localized Merkel cell carcinoma was strongly supported [4, 9, 26,27,28]. For these 28 patients, the pathological stage was equivalent to clinical stage, except for one (case 21) that was re-staged as pIIIA rather than cIIA. The clinical stage of the remaining 41 patients was stage cI (19/41, 46%), stage cIIA (19/41, 46%) and stage cIIB (3/41, 8%), respectively. Pathological parameters and mPDCD1 results are summarized in Table 3. Patients were followed-up for a maximum time of 180 months. At the end of follow-up, 35 (51%) patients died, including 31 (44%)of Merkel cell carcinoma and 4 (5%) of other causes. The median follow-up time was 30 months (range 2–180) for patients dead of disease, 20 months (range 2–72) for those dead of other causes and 51 months (range 8-180) for patients still alive at follow-up. At the end of follow up, 9 patients (13%) were alive with disease progression and 25 (36%) had no evidence of disease.
mPDCD1: correlation with other clinico-pathological features and prognostic relevance
Among various PDCD1 CpGs, the best performances were retrieved by those located on Chromosome position 242800903 and 242800974 (Fig. 2: MethPlotterPD1OD; Fig. 3 MethPlotterPD1OD Box). The distribution of methylation levels of PDCD1 in groups of patients with different outcomes, with the mean, the standard deviation, the minimum and the maximum for each position and group of samples are summarized in Supplementary File 1. Low methylation level of mPDCD1 (mPDCD1low) was found in 42 (61%) patients. It was associated with younger age (76 vs 81 years, p = 0.042), presence of immune cells (79%, p < 0.001), PD-L1 expression by immune cells (55%, p = 0.041) and PD-L1 expression by both immune cells and tumor cells (69%, p = 0.001). Merkel cell polyomavirus was more frequently detected in mPDCD1low rather that mPDCD1high group (60% and 37% respectively, p = 0.068) (p = 0.023). Comparison of clinico-pathological characteristics between mPDCD1low and mPDCD1high groups are summarized in Table 4. Clinical stage, angioinvasion, mitotic count, infiltrative growth pattern and Ki67 did not differ between mPDCD1low and mPDCD1high groups. At the univariate survival analysis (Table 5), the only parameters significantly associated with a higher overall mortality risk were mPDCD1high (p = 0.023), tumor size > 2 cm (p = 0.019) and absence of Merkel cell polyomavirus (p = 0.001). These results were confirmed by permutation tests. A milder evidence was found for angioinvasion (p = 0.070), clinical stage III-IV (p = 0.093), absence of immune cells (p = 0.112) and no PD-L1 expression by tumor cells (p = 0.093), and Kaplan-Meier survival curves are showed in Fig. 4. These seven variables, together with age and gender were included in the multivariable parametric survival model. The best fit for the baseline survival function of the model was found for the proportional hazards model with two spline points (proportional hazard 2 model). This survival function shows a steep decline in the first 50 months of follow-up, more pronounced for the subgroups at higher risk, after which it declines more gently. In the final model (Table 6), four variables remained significantly associated to a higher risk of mortality: mPDCD1high (HR = 2.111, p = 0.042), clinical stage III-IV (HR = 2.357, p = 0.018), size > 2 cm (HR = 2.248, p = 0.031) and absence of Merkel cell polyomavirus (HR = 0.397, p = 0.015). A graphical representation of the model-estimated survival of the four subgroups of patients identified by mPDCD1 and clinical stage is shown in Fig. 5. The subgroup defined by clinical stage I and mPDCD1low have a much lower mortality risk compared to the other subgroups, with an estimated survival at 180 months from surgery around 50%. For the subgroup defined by clinical stage III-IV and mPDCD1high, survival falls below 10% at around 70 months from surgery. Interestingly, the subgroup with clinical stage I-II and mPDCD1high showed a mortality risk similar to the subgroup with clinical stage III-IV and mPDCD1low.
Kaplan-Meier survival curves (univariate survival analysis). The only threevariables significantly associated to a higher risk of mortality were mPDCD1high (p = 0.023) and tumor size > 2 cm (p = 0.019) and the absence of Merkel cell polyomavirus (p = 0.001).Milder evidence was found for angioinvasion (p = 0.070), clinical stage III-IV (p = 0.093), absence of immune cells (p = 0.112) and no PD-L1 expression by tumor cells (p = 0.093). mPDCD1 methylation status of PDCD1
Three main findings come out from this study: mPDCD1 is a valid prognostic parameter in patients affected by Merkel cell carcinoma; mPDCD1 could provide an estimate of the global PD-1/PD-L1 expression rather than being an indirect measure of the immune cells infiltrate; different mPDCD1 levels seem to identify two distinct clinical-pathological families of Merkel cell carcinomas.
Merkel cell carcinoma is an aggressive tumor with a 5-year relative-specific survival rates of 41%, depending on the stage [3, 4]. Because of poor prognosis, especially for advanced Merkel cell carcinoma (stage III-IV sec. AJCC 8th/2017), many efforts have been made to identify prognostic factors, such as immunosuppression status, advanced age, tumor thickness, high number of mitosis, tumor-infiltrating lymphocytes, angioinvasion, p63 and Merkel cell polyomavirus positivity [4,5,6,7,8,9]. Nevertheless, the only prognostic factor independently validated by multiple cohorts was clinical and pathological staging (sec. AJCC 8th/2017). In this study, at the multivariate survival analysis, the parameters associated with a worse survival rate were clinical stage III-IV, tumor size > 2 cm, absence of Merkel cell polyomavirus and mPDCD1high. Nevertheless, mPDCD1high,, absence of Merkel cell polyomavirus and tumor size > 2 cm were the only parameters associated with a worse survival rate, both at univariate survival analysis (p = 0.023; p = 0.001; and p = 0.019, respectively) and at multivariate survival analysis (p = 0.042; p = 0.015 and p = 0.031, respectively). In our opinion, these are highly statistically reliable results because they were obtained with a proportional hazards model, considering the typical survival trend of population affected by Merkel cell carcinoma (an elderly population with a steep decline in the first months of follow-up, more pronounced for the subgroups at higher risk, after that it declines slightly). In addition, combining mPDCD1 and clinical staging, we obtained four subgroups of patients having a more detailed prognostic stratification (Fig. 5). Although this result needs to be validated in larger case series before being proposed as a survival predictive-model, it could represent a valid and easily adoptable prognostic tool in a tumor with few established prognostic factors. Encouragingly, these results have not been influenced by the low number of stage IV patients and by the adoption of clinical rather than pathological staging. As previously validated in head and neck squamous cell carcinoma (HSCNN) [14], the current study provides a strong association between mPDCD1high and a short survival in Merkel cell carcinoma.
In previous studies, it was assumed that mPDCD1 reflects variations in the immune compartment and that could be used as an indirect measure of tumor-infiltrating lymphocytes [14, 15]. Nevertheless, the same authors showed a tumor-intrinsic PD-1 expression by the prostatic adenocarcinoma [16].They found as prostatic adenocarcinoma cells contains PD-1 mRNA subjected to epigenetic control, by promoter methylation (mPDCD1), as known for human T-lymphocytes [16]. Previously, PD-1 expression had just been described in malignant melanoma cells [29, 30], and Mitteldorf et al. reported as PD-1 could be expressed by tumor cells also in Merkel cell carcinoma (in their case series, 2/12 cases, 16%) [17]. All these data suggest that the relationship between PD-1 expression and mPDCD1(also in Merkel cell carcinoma) could be more complex than firstly suspected. In present study, the association of mPDCD1 with the global expression (by both tumor cells and immune cells) of PD-L1 (69%, p = 0.001) was stronger than that with PD-L1 expression by immune cells (55%, p = 0.041). In our opinion, in line with what already hinted in previous studies on other cancers, this finding suggests that mPDCD1should be interpreted as an estimate of the global PD-1/PD-L1 expression by all the tumor components, rather than an indirect measure of the immune cells. If this assumption was true, it could have important therapeutic repercussions. Since Avelumab became the first ever FDA approved drug for both chemotherapy-naïve and chemotherapy-resistant metastatic Merkel cell carcinoma, many efforts have been made to find predictive clinico-pathological features to select responsive patients [10, 11, 31, 32]. Although a significant association between the presence of Merkel cell polyomavirus infection, moderate-severe tumor-infiltrating lymphocytes, and PD-L1 expression by tumor cells was found, a paradoxical response to anti-PD-1/PD-L1 therapy was also observed in Merkel cell polyomavirus and PD-L1 negative Merkel cell carcinomas [11, 31,32,33]. Avelumab response was observed in 26% of Merkel cell polyomavirus positive and 35% of Merkel cell polyomavirus negative tumors, respectively [11, 32]. Again, 34% of PD-L1 positive and 19% of PD-L1 negative tumors responded to treatment [11, 32]. Analogous results were found for Nivolumab, with PD-L1 expression by tumor-infiltrating lymphocytes and tumor cells not significantly correlated with clinical response [31,32,33]. This has an important impact on daily management of Merkel cell carcinoma patients, because PD-1/PD-L1 axis blocking agents could induce treatment-related adverse events, some of which potentially life-threatening and requiring therapy discontinuation or glucocorticoid treatment. Based on the preliminary analyses of phase I/ II trials, all PD-1/PD-L1 axis blocking agents had similar toxicity profiles, with adverse events occurring in 68–77% of patients, 5–21% of grade 3 and 4. As result, in the current clinical practice, we do not have any tools to select patients for anti-PD-1/PD-L1 therapy and highly expensive immunotherapies were indiscriminately administered to all patients, with a high risk to develop adverse events [10,11,12,13, 31,32,33].The strong association between mPDCD1 and the PD-L1 global expression found in our study, proves that mPDCD1 could be a simple and reproducible laboratory tool to estimate the global PD-1/PD-L1 expression (by all the tumor components), that in our opinion could potentially accurately predict the tumor responsivity to anti-PD-1/PD-L1 therapies.
Lastly, in recent years, in parallel with all the studies investigating prognostic parameters in Merkel cell carcinoma, many authors focused on pathogenic mechanisms involved in Merkel cell carcinoma, demonstrating that Merkel cell polyoma virus and ultraviolet light-induced DNA damage identified, respectively, two different pathways with specific clinical, prognostic and therapeutic implications [33,34,35,36,37]. Merkel cell polyoma virus-positive Merkel cell carcinoma is preferentially located on the extremities, with a lower mutational burden, moderate-severe tumor-infiltrating lymphocytes, PD-L1 expression by tumor cells and a better prognosis than Merkel cell polyoma virus-negative Merkel cell carcinoma [34,35,36]. These findings, similarly to what was observed for human papilloma virus in head and neck squamous cell carcinoma, suggested that Merkel cell polyoma virus could induce a tumor-specific immune response with a central pathogenic role played by PD-1/PD-L1 cross-talking [18, 33]. In our study, as shown by the comparison of mPDCD1low and mPDCD1high groups, mPDCD1 status seems to identify two distinct families of Merkel cell carcinomas, with marked clinico-pathological differences (Table 4). In addition, we observed a statistically trend (p = 0.068) between the presence of Merkel cell polyomavirus, detected by immunohistochemistry, and mPDCD1low. In particular, 25 out of 35 Merkel cell polyomavirus-positive tumors showed mPDCD1low, levels. mPDCD1lowgroup was associated with clinico-pathological features related with Merkel cell polyomavirus-positive Merkel cell carcinoma (age < 75 years, presence of immune cells, PD-L1 expression) and with a better prognosis. By contrast, mPDCD1high group was associated with clinico-pathological features related with Merkel cell polyoma virus negative Merkel cell carcinoma (age > 75 years, absence of immune cells, no PD-L1 expression) and with a worse prognosis. Globally, these findings suggest that mPDCD1 could be the “genetic link” between the Merkel cell polyomavirus, the PD-1/PD-L1 tumor-specific immune response and the prognosis in Merkel cell carcinoma.
In conclusion, the current study proves that mPDCD1 is an important prognostic marker in Merkel cell carcinoma. Further studies are needed to clarify if it could be combined with staging to obtain a survival predictive-model, to define its pathogenic role, and to find possible therapeutic implications in selecting patients potentially benefitting from anti-PD-1/PD-L1 therapies.
References
Toker C. Trabecular carcinoma of the skin. Arch Dermatol. 1972;105:107–10.
Sibley RK, Rosai J, Foucar E, et al. Neuroendocrine (Merkel cell) carcinoma of the skin. Am J Surg Pathol. 1980;4:211–21.
Busam, KJ, Walsh N, Woods BA. Merkel cell carcinoma. In: Elder DE, Massi D, Scolyer RA, Willemze R, editors. World Health Organization classification of skin tumors. Lyon: IARC Press; 2018. p. 48–50.
Amin MB, Edge SB, Greene FL, et al., editors. AJCC cancer staging manual. 8th ed. New York: Springer; 2017.
Iyer JG, Storer BE, Paulson KG, et al. Relationships among primary tumor size, number of involved nodes, and survival for 8044 cases of Merkel cell carcinoma. J Am Acad Dermatol. 2014;70:637–43.
Asioli S, Righi A, de Biase D, et al. Expression of p63 is the sole independent marker of aggressiveness in localised (stage I-II) Merkel cell carcinomas. Mod Pathol. 2011;24:1451–61.
Asioli S, Righi A, Volante M, et al. expressionas a new prognostic marker in Merkelcell carcinoma. Cancer. 2007;640-7:p63.
Harms KL, Healy MA, Nghiem P, et al. Analysis of prognostic factors from 9387 merkel cell carcinoma cases forms the basis for the new 8th edition AJCC staging system. Ann Surg Oncol. 2016;23:3564–71.
Lemos BD, Storer BE, Iyer JG, et al. Pathologic nodal evaluation improves prognostic accuracy in Merkel cell carcinoma: analysis of 5823 cases as the basis of the first consensus staging system. J Am Acad Dermatol. 2010;63:751–61.
Nghiem PT, Bhatia S, Lipson EJ, et al. PD-1 Blockade with pembrolizumab in advanced Merkel-cell carcinoma. N Engl J Med. 2016;374:2542–52.
Kaufman HL, Russell J, Hamid O, et al. Avelumabin patients with chemotherapy-refractory metastatic Merkel cell carcinoma: a multicentre, single-group, open-label, phase 2 trial. Lancet Oncol. 2016;17:1374–85.
Kaufman HL, Russell J, Hamid O, et al. Updated efficacy of avelumab in patients with previously treated metastatic Merkel cell carcinoma after ≥ 1 year of follow-up: JAVELIN Merkel 200, a phase 2 clinical trial. J Immunother Cancer. 2018;7.
D’Angelo SP, Russell J, Lebbé C, et al. Efficacy and safety of first-line avelumab treatment in patients with stage IV metastatic Merkel cell carcinoma: a preplanned interim analysis of a clinical trial. JAMA Oncol. 2018;4:e180077.
Goltz D, Gevensleben H, Dietrich J, et al. PDCD1 (PD-1) promoter methylation predicts outcome in head and neck squamous cell carcinoma patients. Oncotarget. 2017;8:41011–20.
Röver LK, Gevensleben H, Dietrich J, et al. PD-1(PDCD1) Promoter methylationis a prognostic factor in patients with diffuse lower-grade gliomas harboring isocitrate dehydrogenase (IDH) mutations. E Bio Medicine. 2018;28:97–104.
Goltz D, Gevensleben H, Dietrichb J, et al. Promoter methylation of the immune checkpoint receptor PD-1 (PDCD1) is an independent prognostic biomarker for biochemical recurrence-free survival in prostate cancer patients following radical prostatectomy. Oncoimmunology. 2016;5:e1221555.
Mitteldorf C, Berisha A, Tronnier M, et al. PD-1 and PD-L1 in neoplasticcells and the tumor microenvironment of Merkel cell carcinoma. J Cutan Pathol. 2017;44:740–6.
Lipson EJ, Vincent JG, Loyo M, et al. PD-L1 expression in the Merkel cell carcinoma microenvironment: Association with inflammation, Merkel cellpolyomavirus and overall survival. Cancer Immunol Res. 2013;1:54–63.
Morandi L, Gissi D, Tarsitano A, et al. DNA methylationanalysis by bisulfitenext-generationsequencing for earlydetection of oralsquamouscellcarcinomaandhigh-gradesquamousintraepitheliallesion from oral brushing. J Craniomaxillofac Surg. 2015;43:1494–1500.
Morandi L, GissiD,Tarsitano A, et al.CpG location and methylation level are crucial factors for the early detection of oral squamous cell carcinoma in brushing samples using bisulfite sequencing of a 13-gene panel. Clin Epigenet. 2017:85.
Li LC, Dahiya R. MethPrimer: designing primers for methylation PCRs. Bioinformatics. 2002;18:1427–31.
Afgan E, Baker D, van denBeek M, et al. The Galaxyplatformfor accessible, reproducible and collaborative biomedical analyses: 2016 update. Nucleic Acids Res. 2016;44:W3–10.
Shen W, Le S, Li Y, et al. SeqKit: a cross-platform and ultrafast toolkit for FASTA/Q file manipulation. PLoS One. 2016;11:e0163962.
Ng R, Kornas K, Sutradhar R, et al. The current application of the Royston-Parmar model for prognostic modeling in health research: a scoping review. Diagnostic Progn Res. 2018;4.
Lambert PC, Royston P. Further development of flexible parametric models for survival analysis. Stata J. 2009;9:265–90.
Kamo R, Kumei A, Ueoku S, et al.Importance of sentinel lymph node biopsy in Merkel cell carcinoma.J Dermatol. 2010;37:1068–70.
Fields RC, Busam KJ, Chou JF, et al. Recurrence and survival in patients undergoing sentinel lymphnode biopsy for Merkel-cell carcinoma: analysis of 153 patients from a singleinstitution. Ann Surg Oncol. 2011;18:2529–37.
Paulson KG, Iyer JG, Byrd DR, et al. Pathologic nodal evaluation is increasingly commonly performed for patients with Merkel-cell carcinoma. J Am Acad Dermatol. 2013;69:653–4.
Kleffel S, Posch C, Barthel SR, et al. Melanoma cell-intrinsic PD-1 receptorfunctions promote tumor growth. Cell. 2015:162:1242–56.
Schatton T, Schutte U, Frank NY, et al. Modulation of T-cellactivation by malignant melanoma initiating cells. Cancer Res. 2010;70:697–708.
Bichakjian CK, Olencki T, Aasi SZ, et al. Merkel-cell Carcinoma, version 1.2018, NCCN Clinical Practice Guidelines in oncology. J Natl Compr Canc Netw. 2018;16:742–74.
Barkdull S, Brownell I PD-L1blockade with avelumab: a new paradigm for treating Merkel cell carcinoma. Cancer Biol Ther. 2017;2:937-9.
Colunga A, Pulliam T, Nghiem P. Merkel-cell carcinoma in the age of immunotherapy: facts and hopes. Clin Cancer Res. 2018;24:2035–43.
Feng H, Shuda M, Chang Y, et al. Clonal integration of a polyomavirus in human Merkel cell carcinoma. Science. 2008;319:1096–100.
The Rockwell Merkel Cell Carcinoma Group. Merkel cell carcinoma: recent progress and current priorities on etiology, pathogenesis, and clinical management. J ClinOncol. 2009;27:4021–6.
Harms PW, Vats P, Verhaegen ME, et al. The distinctive mutational spectra of polyomavirus-negative Merkel-cell carcinoma. Cancer Res. 2015;75:3720–7.
González-Vela MD, Curiel-Olmo S, Derdak S, et al. Shared oncogenic pathways implicated in both virus-positive and uv-induced merkel cell carcinomas. J Invest Dermatol. 2017;137:197–206.
Acknowledgements
This work was supported by Ricerca Fondamentale Orientata (RFO) to Dr. Sofia Asioli, University of Bologna, Italy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics statement
All clinical investigations were conducted according to the principles of the Declaration of Helsinki. The study was approved by the Institutional Review Board and the local ethics committee (study number CE18083, DIBINEM-UNIBO-rif. CE AVEC number 377/2018/OSS/AUSLBO). All information regarding the human material used in this study was managed using anonymous numerical codes.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work will be partially presented as a Poster Session at the 108th Meeting of the United States and Canadian Academy of Pathology in National Harbor, Maryland, 16-21 March 2019
Supplementary information
Rights and permissions
About this article
Cite this article
Ricci, C., Morandi, L., Righi, A. et al. PD-1 (PDCD1) promoter methylation in Merkel cell carcinoma: prognostic relevance and relationship with clinico-pathological parameters. Mod Pathol 32, 1359–1372 (2019). https://doi.org/10.1038/s41379-019-0261-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-019-0261-5
This article is cited by
-
Pan-immune-inflammation value independently predicts disease recurrence in patients with Merkel cell carcinoma
Journal of Cancer Research and Clinical Oncology (2022)
-
Characterizing DNA methylation signatures and their potential functional roles in Merkel cell carcinoma
Genome Medicine (2021)
-
Intron 4–5 hTERT DNA Hypermethylation in Merkel Cell Carcinoma: Frequency, Association with Other Clinico-pathological Features and Prognostic Relevance
Endocrine Pathology (2021)
-
Exploring the Prognostic Role of Ki67 Proliferative Index in Merkel Cell Carcinoma of the Skin: Clinico-Pathologic Analysis of 84 Cases and Review of the Literature
Endocrine Pathology (2020)