Abstract
There is limited data on the spectrum of molecular alterations in goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids of the appendix. We used next generation sequencing to determine mutations of potential pathogenetic and therapeutic significance in this rare group of tumors. Adequate DNA was successfully extracted in 34/46 cases and the final group included 18 goblet cell carcinoids and 16 adenocarcinoma ex goblet cell carcinoids. Illumina TruSeq™ was used for sequencing exons of a custom 282 gene panel using an Illumina HiSeq 2000. All cases had a minimum coverage depth of at least 50 reads. After filtering through the Exome Sequencing Project, the number of mutations per case ranged from 0–9 (mean:3). The mutational burden in adenocarcinoma ex goblet cell carcinoids was significantly higher than goblet cell carcinoids (mean 5 vs. 3; p < 0.05) but the spectrum of alterations overlapped between the two groups. The most frequent mutations included ARID1A (4/34), ARID2 (4/34), CDH1 (4/34), RHPN2 (4/34), and MLL2 (3/34). Some mutations typically seen in conventional colorectal adenocarcinomas were also identified but with much lower frequency (APC :4/34; KRAS :2/34). MLL2 and KRAS mutations were only seen in adenocarcinoma ex goblet cell carcinoids and TP53 mutations were limited to poorly differentiated adenocarcinoma ex goblet cell carcinoids (2/34). Copy number changes could be evaluated in 15/34 cases and showed low copy number gains in CDKN1B (6/15) and NFKBIA (6/15), among others. The overlapping molecular alterations suggest that goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids are best considered two grades of differentiation of the same tumor rather than two distinct histological types. Mutations in TP53, CDH1 and MLL2 mutations were predominantly present in the adenocarcinoma ex goblet cell carcinoid group consistent with transformation to a higher grade lesion. The unique mutational profile also offers an explanation for the poor chemosensitivity in these tumors and highlights the need for developing new targeted therapies.
Similar content being viewed by others
Introduction
Goblet cell carcinoids are rare primary appendiceal tumors described previously under various names such as mucinous carcinoid tumors, mixed crypt cell carcinoma, adenocarcinoid-goblet cell type and microglandular goblet cell carcinoma [1]. Goblet cell carcinoids show both glandular and neuroendocrine differentiation and are distinct from typical carcinoids and conventional adenocarcinomas of the gastrointestinal tract [2, 3]. At one end of the morphological spectrum, recognized as goblet cell carcinoid, the tumor consists almost entirely of infiltrating tubular glands with goblet cells, endocrine cells and Paneth cells, in varying proportions, recapitulating the constituents of a normal colonic crypt. At the other end, a high-grade signet-ring cell or poorly differentiated adenocarcinoma component is seen admixed with typical goblet cell carcinoid-like areas. It is unclear whether adenocarcinoma ex goblet cell carcinoid and goblet cell carcinoid represent two distinct histological subtypes, as the current nomenclature suggests, or two grades of differentiation of the same tumor with shared pathogenetic pathways. In the absence of robust molecular data to guide therapy, current protocols for treating these tumors vary but in most cases follow protocols similar to conventional colorectal adenocarcinomas [4]. 5-FU-based regimens are often used for treatment and some recent studies have also proposed use of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for advanced adenocarcinoma ex goblet cell carcinoids [5]. This highlights the need for molecular data of possible pathogenetic and therapeutic significance for this unique group of tumors. Two prior studies have reported that goblet cell carcinoids have a molecular phenotype distinct from typical carcinoid tumors and from conventional adenocarcinomas of the appendix, citing the decrease in NALP1 (also known as NLRP1) expression and LOH of chromosomes 11q, 16q and 18q in goblet cell carcinoids [6, 7] but neither study differentiated adenocarcinoma ex goblet cell carcinoids from goblet cell carcinoids.
In this study, we used next generation sequencing to evaluate the molecular profile of a series of morphologically well-characterized goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids to determine: (1) whether goblet cell carcinoid and adenocarcinoma ex goblet cell carcinoid share a similar spectrum of molecular abnormalities or represent distinct groups at the molecular level; (2) whether the genetic alterations present in adenocarcinoma ex goblet cell carcinoid overlap significantly with conventional colorectal adenocarcinomas; (3) and whether any mutational targets of therapeutic significance can be identified in these tumors.
Materials and methods
The surgical pathology files of participating institutions were searched for cases diagnosed as “Goblet cell carcinoid”, “Mixed adenoneuroendocrine carcinoma”, “Mucinous Carcinoid Tumor” and “Adenocarcinoma ex goblet cell carcinoid”. Cases for which H&E slides as well as paraffin blocks were available for review and additional work up were included in the study. All slides were then reviewed by two study pathologists (JM, AS) to separate the tumors into a goblet cell carcinoid or adenocarcinoma ex goblet cell carcinoid (Fig. 1a–c). Goblet cell carcinoids were defined as lesions with well-formed glandular structures that recapitulated constituents of a normal colonic crypt with goblet cells, neuroendocrine cells, or Paneth cells. Tumors in this group showed a low nuclear:cytoplasmic ratio and only a mild to moderate degree of nuclear atypia. Tumors with pools of extracellular mucin but with retained glandular tumor architecture, as described above, and absence of any floating strips or sheets of neoplastic epithelium and/or high-grade nuclear atypia were considered acceptable for the goblet cell carcinoid category in this study. In contrast, tumors with a clearly defined signet-ring-cell component or a poorly differentiated adenocarcinoma component composed of non-gland forming aggregates or sheets of neoplastic cells with high-grade nuclei or tumors resembling conventional mucinous colorectal adenocarcinoma were all classified as adenocarcinoma ex goblet cell carcinoid. The adenocarcinoma component in all cases in the adenocarcinoma ex goblet cell carcinoid group comprised at least 50% or more of the entire tumor, to enable macrodissection and DNA extraction without risk of contamination from the goblet cell carcinoid-like component. However, a minor, definitive goblet cell carcinoid component was required to be present in all adenocarcinoma ex goblet cell carcinoid cases sequenced for the study, as was the lack of a precursor conventional adenoma involving the appendiceal mucosa. The adenocarcinoma ex goblet cell carcinoid group was not further sub-classified into signet-ring-cell and poorly differentiated adenocarcinoma, as proposed by Tang et al. due to the small number of cases and hence the low likelihood of finding significant molecular differences between these two subgroups. Immunohistochemical data for neuroendocrine differentiation (synaptophysin and/or chromogranin) was available in eight goblet cell carcinoids and 8 adenocarcinoma ex goblet cell carcinoids and focal positivity for at least one marker was present in 15/16 cases.
All tumors analyzed in the study were classified by two study pathologists into one of three groups using the classification previously proposed by Tang et al. Pure goblet cell carcinoids (a) recapitulated the constituents of a normal colonic crypt with goblet cells, neuroendocrine cells, or Paneth cells while those classified as adenocarcinoma ex goblet cell carcinoid showed either a significant (>50%) component of signet ring cell carcinoma (b) or a non-gland forming conventional poorly differentiated adenocarcinoma (c)
Additional sections were cut and the last section stained with hematoxylin and eosin to ensure tumor adequacy for DNA extraction. Tumors with <20% cellularity were excluded from further analysis. The area of highest tumor percentage was then selected for macrodissection from ten unstained 4-μm tissue sections using a razor blade. DNA was isolated using a Qiasymphony (Qiagen, Valencia, CA) automated DNA extractor according to the manufacturer’s recommendations. All cases with at least 50 ng of DNA were sequenced.
Somatic mutations in the tumor DNA were detected by Illumina HiSeq using the exome-sequencing platform OncoPanel in the CLIA-certified Center for Advanced Molecular Diagnostics laboratory at BWH [8]. The OncoPanel assay detects mutations in 282 cancer associated genes and is enriched for genes with known pathogenetic and therapeutic significance (Suppl Table 1). All detected variants with a minimum coverage depth of at least 50 reads were filtered for known SNPs (single nucleotide polymorphisms) using the Exome Sequencing Project databases. A subsequent search in COSMIC and Pubmed for known pathogenic variants was performed to rule out passenger mutations. Clinical data including age, gender and patient outcome data were retrieved by medical chart review. Pathologic data including TNM (Tumor, Node, Metastasis) stage was also recorded for each case using a combination of slide and medical chart review. Statistical analysis was performed using the Student t test to detect significance of observed differences between groups. The study was approved by the Institutional Review Boards of all the participating institutions.
Results
Study group
A total of 142 cases were retrieved from the initial archival search. Of these, 46 tumors with additional tissue (either paraffin blocks or unstained slides), sufficient tumor percentage (>20%) and adenocarcinoma ex goblet cell carcinoid component (>50%) were selected for macrodissection and DNA extraction. Three cases failed DNA extraction while another nine had less than the required minimum number of 50 reads for quality control and were excluded from the study. The final study group consisted of 34 patients (16 male; 11 female; 7 consultation cases with missing gender information) ranging in age from 36–73 years (mean age: 54 years) and included 18 goblet cell carcinoids and 16 adenocarcinoma ex goblet cell carcinoids. The mean age of patients with goblet cell carcinoid was slightly younger (53 years) than those with adenocarcinoma ex goblet cell carcinoid (56 years) but this difference was not statistically significant (p = 0.3). Both groups showed a slight male predominance (goblet cell carcinoid:ten males, six females; adenocarcinoma ex goblet cell carcinoid: six males, five females). Complete AJCC Classification (8th edition) TNM staging information was available for 21 of the 34 cases. The majority of tumors in both groups were deeply invasive T3 (goblet cell carcinoid: seven; adenocarcinoma ex goblet cell carcinoid: seven) or T4 (goblet cell carcinoid: four; adenocarcinoma ex goblet cell carcinoid: three) lesions. Nodal metastasis was present in only one goblet cell carcinoid in contrast to seven adenocarcinoma ex goblet cell carcinoids that showed either nodal (n=4) or distant metastasis (n=3) at initial presentation. Clinical outcome data was available for 21/34 patients (goblet cell carcinoid = 12; adenocarcinoma ex goblet cell carcinoid = 9) and follow up duration ranged from 3 to 341 months (mean: 102 months). Two patients with adenocarcinoma ex goblet cell carcinoid and four with goblet cell carcinoid died of disease within 1 to 5 years from the date of initial diagnosis. Six of 12 patients in the goblet cell carcinoid group were alive with no evidence of disease at last follow up while two died of unrelated causes. Five of the nine patients in the adenocarcinoma ex goblet cell carcinoid group were alive with disease and two were alive with no evidence of disease at last follow up. The clinical and demographic data of the entire study group is summarized in Table 1.
Pathology review
Two GI pathologists (JM and AS) reviewed all cases to ensure morphological consensus regarding tumor classification using the criteria described in the methods section above. In view of the relatively low number of adenocarcinoma ex goblet cell carcinoid (n = 16) with adequate DNA for sequencing these tumors were not further sub-classified into signet-ring cell or poorly differentiated subtypes as proposed in the classification by Tang et al. and were considered as a single group when comparing molecular alterations in pure goblet cell carcinoids to those classified as adenocarcinoma ex goblet cell carcinoid. The overall tumor cellularity was also estimated in all cases by one of the authors (MEJ) on the slides that were used for macrodissection and DNA extraction. The unique growth pattern of these tumors and presence of a dominant stromal component made it difficult to macrodissect areas with very high cellularity and in most cases the cellularity ranged from 20–30%.
Mutational analysis
At least one mutation was identified in 33/34 tumors analyzed in the study with a range of 0–6 mutations in the goblet cell carcinoid group and 1–9 in the adenocarcinoma ex goblet cell carcinoid group. Overall, the mean number of mutations was significantly more in the adenocarcinoma ex goblet cell carcinoid compared to the goblet cell carcinoid group (5 vs. 3; p = 0.01). A complete list of specific gene mutations found in these tumors is included in Supplementary Table 2.
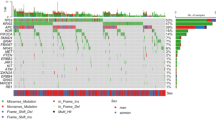
Multiple low frequency mutations in several genes were present in both goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids. These included ARID2, ARID1A, APC, CDH1, RHPN2, ATRX, ALOX12B, MECOM, PALB2 and PIK3R1 (Fig. 2), all at allelic frequencies consistent with the estimated tumor percentage. A specific novel RHPN2 (p.L385I) missense mutation was present in two goblet cell carcinoids and two adenocarcinoma ex goblet cell carcinoids. In one case, we were able to macrodissect and analyze both the pure goblet cell carcinoid and adenocarcinoma ex goblet cell carcinoid components separately and a TCF7L2 alteration was seen in both the adenocarcinoma ex goblet cell carcinoid and the goblet cell carcinoid component, confirming that the two components were clonally related to each other.
Altered genes in goblet cell carcinoids (samples 1–18) and adenocarcinoma ex goblet cell carcinoids (samples 19–34). Asterisk indicates two or more mutations in the same gene (See Supplemental Table 1 for additional information on mutations)
Mutations present exclusively in the goblet cell carcinoid group included SOX9, AR, PRPF8, ABL1, CARD11, CHEK2, CREBBP, CRKL, CYLD, DNMT3A, EGFR, ERCC2, ESR, ETV1, FANCA1, FUS, GATA3, GNAQ, INSIG1, JAK2, KDM6B, MLH1, MSH6, NTRK1, PDGFRA, SUFU, SUZ12 and MSH2 (Fig. 2). No family or personal history was available for the patient with MSH2 mutation to determine whether this was a somatic mutation or a manifestation of Lynch syndrome.
In contrast, mutations seen exclusively in the adenocarcinoma ex goblet cell carcinoid group included BRCA2, MLL2, BCORL1, BLM, DMD, GNAS, KRAS, TP53, BCL6, BRAF, BRCA1, BRD4, BUB1B, CDK1, CDK6, CRTC2, CSF1R, DICER1, EP300, ERBB4, ERCC4, FANCG, FLT1, FLT4, GLI2, HNF1A, KDM6A, KDR, NFKBIZ, NPRL2, PARK2, PHF6, PMS1, PRAME, PTPRD, RARA, RECQL4, SMAD2, SMAD4 and TET2 (Fig. 2). As mentioned above, we did not compare mutational profiles separately in the signet ring cell and poorly differentiated subgroups of adenocarcinoma ex goblet cell carcinoid because of the low number of cases in each subgroup. However, it is interesting to note that all KRAS, BRAF and TP53 mutations found in our study were present in the poorly differentiated adenocarcinoma ex goblet cell carcinoid subgroup of tumors.
Copy number changes
Copy number changes were evaluated in only 15/34 cases since the tumor percentage was too low in the remaining cases for an accurate determination. Copy number analysis was performed on five goblet cell carcinoid and ten adenocarcinoma ex goblet cell carcinoids with sufficient tumor cellularity for this analysis. The mean number of copy number changes was 6 in the adenocarcinoma ex goblet cell carcinoid group and 5 in the goblet cell carcinoid group (p = 0.7). Three of five pure goblet cell carcinoid tumors and all adenocarcinoma ex goblet cell carcinoids showed low level copy number gains involving CDKN1B, CDK4 and CDK2, and also of two genes on chromosome 1(ID3 and MCL1) and one gene on chromosome 4 (NFKBIA). No copy number deletions were identified in any of the 15 cases evaluated including on chromosome 17p, that contains the NALP1 gene previously reported to have decreased expression in goblet cell carcinoids [7]. The OncoPanel platform gene panel does not include NALP1 and mutations in this gene could not be analyzed.
Discussion
In this study, we used next generation sequencing to characterize the genetic landscape of goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids and found largely overlapping molecular signatures in the two groups (Fig. 3) with mutations in chromatin remodeling genes being the most prevalent abnormality. Mutations found in these tumors were significantly different from those described previously in typical intestinal carcinoids [6], mucinous appendiceal neoplasms [9] and conventional colorectal adenocarcinomas. Moreover, the mutation frequency was also much lower than usually found in sporadic colon cancers. The Cancer Genome Atlas study reported APC and CTNNB1 mutations in >80% of all colorectal carcinomas [10]. In contrast, APC mutations were detected in <15% of tumors in our study and no CTNNB1 mutations were identified. Overlapping mutations in ten genes, including ARID1A and ARID2, CDH1, and a novel missense mutation in the RHPN2 gene (p.L385I), among others, were present in both of goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids. This provides molecular evidence to support the hypothesis that goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids are best considered two grades of differentiation of the same tumor rather than two distinct histological types. This is further supported by the presence of a TCF7L2 mutation in both the goblet cell carcinoid and the adenocarcinoma component of an adenocarcinoma ex goblet cell carcinoid, and the fact that the average mutational burden was significantly higher in adenocarcinoma ex goblet cell carcinoids compared to goblet cell carcinoids. In addition, mutations involving KRAS, BRAF and TP53, characteristic of colorectal adenocarcinomas, were present in low frequency and only in the poorly differentiated adenocarcinoma ex goblet cell carcinoid subgroup of tumors. This favors the concept of multiple sequential genetic hits leading to the development of a higher grade malignancy.
Pathway specific mutations observed in tumors in the entire cohort (a) and within the goblet cell carcinoid (b) and adenocarcinoma ex goblet cell carcinoid (c) groups, respectively. The overlapping mutational profile in Groups b and c suggests that adenocarcinoma ex goblet cell carcinoids and goblet cell carcinoids are varying grades of differentiation of the same tumor type
In the study by Tang et al. adenocarcinoma ex goblet cell carcinoids that were categorized as either group B or C based on signet-ring cell or poor differentiation, respectively, behaved far more aggressively than the group A tumors that were similar to the “pure” goblet cell carcinoids included in our study [10]. The 5-year survival, in their study, was 100% for Group A, 36% for Group B, and 0% for Group C tumors in the Tang et al. study. This classification scheme was also applied in a Danish cohort of 83 patients and found to be prognostically useful but on regression analysis only Stage IV disease, focal synaptophysin positivity and non-radical surgery were found to be independent negative prognostic factors [11]. The morphological distinction of goblet cell carcinoids from adenocarcinoma ex goblet cell carcinoids, therefore, clearly has prognostic significance but implies two distinct histological types, with adenocarcinoma ex goblet cell carcinoid being adenocarcinomatous transformation of a neuroendocrine tumor rather than two grades of differentiation of the same tumor type. Others have attempted to morphologically distinguish the likelihood of aggressive behavior in these unique tumors by quantifying the proportion of adenocarcinoma-like component, into <25%, 25–50% and >50% categories [12]. Our data suggest that this classification more accurately reflects the underlying biology of the tumor by considering them to be part of the same continuum but may, at times, be difficult to apply in practice. Goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids are staged like colorectal adenocarcinomas and not like typical appendiceal carcinoids but the use of “carcinoid” often causes confusion among oncologists as to the choice of chemotherapy in these patients. In current practice, most adenocarcinoma ex goblet cell carcinoids are treated similar to conventional colorectal adenocarcinomas with 5-FU-based chemotherapy but the outcomes are poor [4, 13]. This is not surprising given the molecular findings reported in our study since mutations commonly seen in colorectal cancers, such as APC, BRAF, KRAS and TP53 occurred at a much lower frequency in these tumors as did GNAS mutations that have been described in a high proportion of mucinous adenocarcinomas of the appendix [14].
Previous molecular analyses of goblet cell carcinoids have mostly interrogated a single gene or a limited panel of genes with the focus largely on exploring differences from typical intestinal carcinoids. Expression of the apoptotic marker NALP1 was reported to be decreased in goblet cell carcinoids compared to typical carcinoid tumors and LOH on chromosomes 11q, 16q and 18q has been reported to distinguish goblet cell carcinoids from typical carcinoids [7]. The contradictory findings reported in literature regarding lack of SMAD4, KRAS or TP53 mutations in these tumors [6] and TP53 mutations being present in up to 25% of goblet cell carcinoids [15] are most likely related to the proportion of goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids included in these studies, as well as the histological criteria used to make the distinction between the two groups. In our study, using a 282 gene panel, mutations in chromatin remodeling genes ARID2 and ARID1A, were found in a relatively high proportion of goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids. ARID2, located on chromosome 12 (12q13.11) encodes a subunit of the PBAF SWI/SNF chromatin remodeling complex while ARID1A encodes a subunit of the BAF SWI/SNF complex. Mutations in ARID2 have been reported recently in hepatocellular and renal cell carcinomas [16, 17] while ARID1A mutations have been reported in gastric, esophageal [18] and ovarian carcinomas [19, 20] and also at a much lower frequency in colorectal adenocarcinomas [21, 22]. Similarly, mutations in the subunits of the SWI/SNF chromatin remodeling complex spanning about 20 genes have been reported in almost a third of all gastric carcinomas [22]. Taken together, this suggests a role for epigenetic modification in the early stage of tumorigenesis of goblet cell carcinoids followed by additional hits, such as TP53 or CDH1, that lead to transformation into a poorly differentiated or signet-ring-cell type adenocarcinoma ex goblet cell carcinoid. Mutations in ARID2 and ARID1A may also be of therapeutic relevance since EZH2 inhibitor based combination drug strategies have been recently proposed for carcinomas with ARID1A and other SWI/SWF chromatin remodeling complex gene mutations [23]. The rare adenocarcinoma ex goblet cell carcinoids with the BRAF V600E mutation may also be potentially targetable by vemurafenib.
CDH1 mutations have also not been reported in ileal carcinoids or in goblet cell carcinoids but both tumors show LOH of 16q with loss of the 16q21–q24.2 locus that harbors the tumor suppressor genes CTCF and E-cadherin/CDH-1. [6] CDH1 mutations are frequently found in gastric [24] and breast carcinomas [25] and it is not entirely surprising that we found similar mutations in adenocarcinoma ex goblet cell carcinoids because the Group B tumors in the Tang classification show a discohesive, single cell infiltrative growth pattern much like lobular breast cancer and diffuse type gastric cancer. Clusters of tumor cells in goblet cell carcinoids streaming through the muscularis propria may mimic signet ring cell carcinoma and lead to erroneous upgrading as adenocarcinoma ex goblet cell carcinoid on morphology. It is tempting to speculate that E-cadherin immunohistochemistry might be helpful in this scenario but given the low prevalence of CDH1 mutations in adenocarcinoma ex goblet cell carcinoids found in our study, intact membranous staining for E-cadherin cannot be used to exclude a diagnosis of adenocarcinoma ex goblet cell carcinoid with certainty.
Similar to CDH1, MLL2, also known as KMT2D, has not been reported previously in either ileal carcinoids or goblet cell carcinoids and is a gene that encodes a histone methyltransferase and is located very close to ARID2 on chromosome 12 (12q13.12). It has been implicated recently in numerous malignant tumors [26] including non-small cell lung cancers, head and neck carcinomas and lymphomas. A recent study [24] also found mutations in MLL2 to be typically paired with ARID1A mutations in gastric carcinomas. While both MLL2 and ARID1A mutations were identified in our study, we did not find any tumor with concurrent MLL2 and ARID1A mutations.
In summary, our study provides molecular evidence that goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids are indeed unique tumors distinct from both typical carcinoids and conventional colorectal adenocarcinomas. The overlapping mutational profile of goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids suggests that they are best considered a single tumor type with varying grades of differentiation rather than two distinct histological subtypes. Our findings also indicate that the poor response of these tumors to 5-FU based chemotherapy is related to the low frequency of mutations, such as APC, KRAS, BRAF and TP53, that are typically prevalent in colorectal adenocarcinomas. Sequencing data can be helpful in guiding choice of targeted chemotherapy, when indicated, in patients with of goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids.
References
Roy P, Chetty R. Goblet cell carcinoid tumors of the appendix: an overview. World J Gastrointest Oncol. 2010;2:251–8.
Gagne F, Fortin P, Dufour V, Delage C. Tumors of the appendix associating histologic features of carcinoid and adenocarcinoma. Ann Anat Pathol (Paris). 1969;14:393–406.
Subbuswamy SG, Gibbs NM, Ross CF, Morson BC. Goblet cell carcinoid of the appendix. Cancer. 1974;34:338–44.
Pape UF, Perren A, Niederle B, Gross D, Gress T, Costa F, Arnold R, Denecke T, Plockinger U, Salazar R, Grossman A, Barcelona Consensus Conference participants. ENETS consensus guidelines for the management of patients with neuroendocrine neoplasms from the jejuno-ileum and the appendix including goblet cell carcinomas. Neuroendocrinology. 2012;95:135–56.
McConnell YJ, Mack LA, Gui X, Carr NJ, Sideris L, Temple WJ, Dube P, Chandrakumaran K, Moran BJ, Cecil TD. Cytoreductive surgery with hyperthermic intraperitoneal chemotherapy: an emerging treatment option for advanced goblet cell tumors of the appendix. Ann Surg Oncol. 2014;21:1975–82.
Stancu M, Wu TT, Wallace C, Houlihan PS, Hamilton SR, Rashid A. Genetic alterations in goblet cell carcinoids of the vermiform appendix and comparison with gastrointestinal carcinoid tumors. Mod Pathol. 2003;16:1189–98.
Modlin IM, Kidd M, Latich I, Zikusoka MN, Eick GN, Mane SM, Camp RL. Genetic differentiation of appendiceal tumor malignancy: a guide for the perplexed. Ann Surg. 2006;244:52–60.
Wagle N, Berger MF, Davis MJ, Blumenstiel B, Defelice M, Pochanard P, Ducar M, Van Hummelen P, Macconaill LE, Hahn WC, Meyerson M, Gabriel SB, Garraway LA. High-throughput detection of actionable genomic alterations in clinical tumor samples by targeted, massively parallel sequencing. Cancer Discov. 2012;2:82–93.
Alakus H, Babicky ML, Ghosh P, Yost S, Jepsen K, Dai Y, Arias A, Samuels ML, Mose ES, Schwab RB, Peterson MR, Lowy AM, Frazer KA, Harismendy O. Genome-wide mutational landscape of mucinous carcinomatosis peritonei of appendiceal origin. Genome Med. 2014;6:43.
Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330–7.
Lamarca A, Nonoka D, Lopez Escola C, Hubner RA, O’Dwyer S, Chakrabarty B, Fulford P, Valle JW. Appendiceal goblet cell carcinoids: management considerations from a reference peritoneal tumour service centre and ENETS centre of excellence. Neuroendocrinology. 2016;103:500–17.
Tang LH, Shia J, Soslow RA, Dhall D, Wong WD, O’Reilly E, Qin J, Paty P, Weiser MR, Guillem J, Temple L, Sobin LH, Klimstra DS. Pathologic classification and clinical behavior of the spectrum of goblet cell carcinoid tumors of the appendix. Am J Surg Pathol. 2008;32:1429–43.
Olsen IH, Holt N, Langer SW, Hasselby JP, Gronbaek H, Hillingso J, Mahmoud M, Ladekarl M, Iversen LH, Kjaer A, Federspiel BH, Knigge U. Goblet cell carcinoids: characteristics of a Danish cohort of 83 patients. PLoS One. 2015;10:e0117627.
Taggart MW, Abraham SC, Overman MJ, Mansfield PF, Rashid A. Goblet cell carcinoid tumor, mixed goblet cell carcinoid-adenocarcinoma, and adenocarcinoma of the appendix: Comparison of clinicopathologic features and prognosis. Arch Pathol Lab Med. 2015;139:782–90.
Ramnani DM, Wistuba II, Behrens C, Gazdar AF, Sobin LH, Albores-Saavedra J. K-ras and p53 mutations in the pathogenesis of classical and goblet cell carcinoids of the appendix. Cancer. 1999;86:14–21.
Zucman-Rossi J, Villanueva A, Nault JC, Llovet JM. The genetic landscape and biomarkers of hepatocellular carcinoma. Gastroenterology. 2015;149:1226-1239.
Kovac M, Navas C, Horswell S, Salm M, Bardella C, Rowan A, Stares M, Castro-Giner F, Fisher R, de Bruin EC, Kovacova M, Gorman M, Makino S, Williams J, Jaeger E, Jones A, Howarth K, Larkin J, Pickering L, Gore M, Nicol DL, Hazell S, Stamp G, O’Brien T, Challacombe B, Matthews N, Phillimore B, Begum S, Rabinowitz A, Varela I, Chandra A, Horsfield C, Polson A, Tran M, Bhatt R, Terracciano L, Eppenberger-Castori S, Protheroe A, Maher E, El Bahrawy M, Fleming S, Ratcliffe P, Heinimann K, Swanton C, Tomlinson I. Recurrent chromosomal gains and heterogeneous driver mutations characterise papillary renal cancer evolution. Nat Commun. 2015;6:6336.
Drage MG, Tippayawong M, Agoston AT, Zheng Y, Bueno R, Hornick JL, Odze RD, Srivastava A. Morphological features and prognostic significance of ARID1A-deficient esophageal adenocarcinomas. Arch Pathol Lab Med. 2017;141:970-977.
Wiegand KC, Shah SP, Al-Agha OM, Zhao Y, Tse K, Zeng T, Senz J, McConechy MK, Anglesio MS, Kalloger SE, Yang W, Heravi-Moussavi A, Giuliany R, Chow C, Fee J, Zayed A, Prentice L, Melnyk N, Turashvili G, Delaney AD, Madore J, Yip S, McPherson AW, Ha G, Bell L, Fereday S, Tam A, Galletta L, Tonin PN, Provencher D, Miller D, Jones SJ, Moore RA, Morin GB, Oloumi A, Boyd N, Aparicio SA, Shih I, Mes-Masson AM, Bowtell DD, Hirst M, Gilks B, Marra MA, Huntsman DG. ARID1A mutations in endometriosis-associated ovarian carcinomas. N Engl J Med. 2010;363:1532–43.
Wang K, Kan J, Yuen ST, Shi ST, Chu KM, Law S, Chan TL, Kan Z, Chan AS, Tsui WY, Lee SP, Ho SL, Chan AK, Cheng GH, Roberts PC, Rejto PA, Gibson NW, Pocalyko DJ, Mao M, Xu J, Leung SY. Exome sequencing identifies frequent mutation of ARID1A in molecular subtypes of gastric cancer. Nat Genet. 2011;43:1219–23.
Cajuso T, Hanninen UA, Kondelin J, Gylfe AE, Tanskanen T, Katainen R, Pitkanen E, Ristolainen H, Kaasinen E, Taipale M, Taipale J, Bohm J, Renkonen-Sinisalo L, Mecklin JP, Jarvinen H, Tuupanen S, Kilpivaara O, Vahteristo P. Exome sequencing reveals frequent inactivating mutations in ARID1A, ARID1B, ARID2 and ARID4A in microsatellite unstable colorectal cancer. Int J Cancer. 2014;135:611–23.
Shain AH, Pollack JR. The spectrum of SWI/SNF mutations, ubiquitous in human cancers. PLoS One. 2013;8:e55119.
Bitler BG, Fatkhutdinov N, Zhang R. Potential therapeutic targets in ARID1A-mutated cancers. Expert Opin Ther Targets. 2015;19:1419–22.
Ali SM, Sanford EM, Klempner SJ, Rubinson DA, Wang K, Palma NA, Chmielecki J, Yelensky R, Palmer GA, Morosini D, Lipson D, Catenacci DV, Braiteh F, Erlich R, Stephens PJ, Ross JS, Ou SH, Miller VA. Prospective comprehensive genomic profiling of advanced gastric carcinoma cases reveals frequent clinically relevant genomic alterations and new routes for targeted therapies. Oncologist. 2015;20:499–507.
Dossus L, Benusiglio PR. Lobular breast cancer: Incidence and genetic and non-genetic risk factors. Breast Cancer Res. 2015;17:37.
David J. Ford, Andrew K. Dingwall, (2015) The cancer COMPASS: navigating the functions of MLL complexes in cancer. Cancer Genetics 208 (5):178-191.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Johncilla, M., Stachler, M., Misdraji, J. et al. Mutational landscape of goblet cell carcinoids and adenocarcinoma ex goblet cell carcinoids of the appendix is distinct from typical carcinoids and colorectal adenocarcinomas. Mod Pathol 31, 989–996 (2018). https://doi.org/10.1038/s41379-018-0003-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-018-0003-0
This article is cited by
-
Appendiceal Goblet Cell Carcinoma: Role of Cytoreductive Surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC)
Indian Journal of Surgical Oncology (2023)
-
Clinicopathological features of appendiceal goblet cell adenocarcinoma in Japan: a multicenter retrospective study
Surgery Today (2023)
-
Genetic alterations in gastric amphicrine carcinomas and comparison with gastric mixed neuroendocrine-non-neuroendocrine neoplasms
Modern Pathology (2022)
-
Knowledge gaps in the appendix: a multi-institutional study from seven academic centers
Modern Pathology (2019)