Abstract
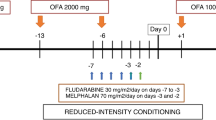
Anti-PD-1 monoclonal antibodies yield high response rates in patients with relapsed/refractory classic Hodgkin lymphoma (cHL), but most patients will eventually progress. Allogeneic hematopoietic cell transplantation (alloHCT) after PD-1 blockade may be associated with increased toxicity, raising challenging questions about the role, timing, and optimal method of transplantation in this setting. To address these questions, we assembled a retrospective cohort of 209 cHL patients who underwent alloHCT after PD-1 blockade. With a median follow-up among survivors of 24 months, the 2-year cumulative incidences (CIs) of non-relapse mortality and relapse were 14 and 18%, respectively; the 2-year graft-versus-host disease (GVHD) and relapse-free survival (GRFS), progression-free survival (PFS), and overall survival were 47%, 69%, and 82%, respectively. The 180-day CI of grade 3–4 acute GVHD was 15%, while the 2-year CI of chronic GVHD was 34%. In multivariable analyses, a longer interval from PD-1 to alloHCT was associated with less frequent severe acute GVHD, while additional treatment between PD-1 and alloHCT was associated with a higher risk of relapse. Notably, post-transplant cyclophosphamide (PTCy)-based GVHD prophylaxis was associated with significant improvements in PFS and GRFS. While awaiting prospective clinical trials, PTCy-based GVHD prophylaxis may be considered the optimal transplantation strategy for this patient population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Chen R, Zinzani PL, Lee HJ, Armand P, Johnson NA, Brice P. et al. Pembrolizumab in relapsed or refractory Hodgkin lymphoma: 2-year follow-up of KEYNOTE-087. Blood. 2019;134(Oct):1144–53.
Armand P, Engert A, Younes A, Fanale M, Santoro A, Zinzani PL, et al. Nivolumab for relapsed/refractory classic Hodgkin lymphoma after failure of autologous hematopoietic cell transplantation: extended follow-up of the multicohort single-arm phase II CheckMate 205 trial. J Clin Oncol. 2018;36(May):1428–39. http://www.ncbi.nlm.nih.gov/pubmed/29584546
Rashidi A, Ebadi M, Cashen AF. Allogeneic hematopoietic stem cell transplantation in Hodgkin lymphoma: a systematic review and meta-analysis. Bone Marrow Transpl. 2016;51(Apr):521–8. http://www.ncbi.nlm.nih.gov/pubmed/26726948
Merryman RW, Kim HT, Zinzani PL, Carlo-Stella C, Ansell SM, Perales M-A. et al. Safety and efficacy of allogeneic hematopoietic stem cell transplant after PD-1 blockade in relapsed/refractory lymphoma. Blood. 2017;129(Mar):1380–8.
Kasamon YL, de Claro RA, Wang Y, Shen YL, Farrell AT, Pazdur R. FDA approval summary: nivolumab for the treatment of relapsed or progressive classical Hodgkin lymphoma. Oncologist. 2017;22:585–91. http://www.ncbi.nlm.nih.gov/pubmed/28438889
Ijaz A, Khan AY, Malik SU, Faridi W, Fraz MA, Usman M, et al. Significant risk of graft-versus-host disease with exposure to checkpoint inhibitors before and after allogeneic transplantation. Biol Blood Marrow Transpl. 2019;25:94–9. http://www.ncbi.nlm.nih.gov/pubmed/30195074
Schoch LK, Cooke KR, Wagner-Johnston ND, Gojo I, Swinnen LJ, Imus P. et al. Immune checkpoint inhibitors as a bridge to allogeneic transplantation with posttransplant cyclophosphamide. Blood Adv. 2018;2(Sep):2226–9.
Casadei B, Broccoli A, Stefoni V, Pellegrini C, Marangon M, Morigi A, et al. PD-1 blockade as bridge to allogeneic stem cell transplantation in relapsed/refractory Hodgkin lymphoma patients: a retrospective single center case series. Haematologica. 2019;104(Nov):e521–2. http://www.ncbi.nlm.nih.gov/pubmed/30890595
De Philippis C, Legrand-Izadifar F, Bramanti S, Giordano L, Montes de Oca C, Duléry R, et al. Checkpoint inhibition before haploidentical transplantation with posttransplant cyclophosphamide in Hodgkin lymphoma. Blood Adv. 2020;4(Apr):1242–9. http://www.ncbi.nlm.nih.gov/pubmed/32227210
Paul S, Zahurak M, Luznik L, Ambinder RF, Fuchs EJ, Bolaños-Meade J, et al. Non-myeloablative allogeneic transplantation with post-transplant cyclophosphamide after immune checkpoint inhibition for classic Hodgkin lymphoma: a retrospective cohort study. Biol Blood Marrow Transpl. 2020. http://www.ncbi.nlm.nih.gov/pubmed/32592857. Accessed 13 Jul 2020
Herbaux C, Merryman R, Devine S, Armand P, Houot R, Morschhauser F, et al. Recommendations for managing PD-1 blockade in the context of allogeneic HCT in Hodgkin lymphoma: taming a necessary evil. Blood. 2018;132(Jul):9–16. http://www.ncbi.nlm.nih.gov/pubmed/29720488
Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, et al. Recommendations for initial evaluation, staging, and response assessment of hodgkin and non-hodgkin lymphoma: the lugano classification. J Clin Oncol. 2014;32(Sep):3059–67. http://www.ncbi.nlm.nih.gov/pubmed/25113753
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National institutes of health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 diagnosis and staging working group report. Biol Blood Marrow Transpl. 2015;21:389. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4329079/
Lee DW, Santomasso BD, Locke FL, Ghobadi A, Turtle CJ, Brudno JN, et al. ASTCT consensus grading for cytokine release syndrome and neurologic toxicity associated with immune effector cells. Biol Blood Marrow Transpl. 2019;25:625–38.
Gray RJ. A class of k-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16:1140–54.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(Jun):496–509. http://www.tandfonline.com/doi/abs/10.1080/01621459.1999.10474144
Ahmed S, Kanakry JA, Ahn KW, Litovich C, Abdel-Azim H, Aljurf M, et al. Lower graft-versus-host disease and relapse risk in post-transplant cyclophosphamide–based haploidentical versus matched sibling donor reduced-intensity conditioning transplant for Hodgkin lymphoma. Biol Blood Marrow Transpl. 2019;25(Sep):1859–68. http://www.ncbi.nlm.nih.gov/pubmed/31132455
Martínez C, Gayoso J, Canals C, Finel H, Peggs K, Dominietto A, et al. Post-transplantation cyclophosphamide-based haploidentical transplantation as alternative to matched sibling or unrelated donor transplantation for Hodgkin lymphoma: a registry study of the lymphoma working party of the European society for blood and marrow transplantation. J Clin Oncol. 2017;35(Oct):3425–32. http://ascopubs.org/doi/10.1200/JCO.2017.72.6869
Michonneau D, Sagoo P, Breart B, Garcia Z, Celli S, Bousso P. The PD-1 axis enforces an anatomical segregation of CTL activity that creates tumor niches after allogeneic hematopoietic stem cell transplantation. Immunology. 2016;44(Jan):143–54. http://www.ncbi.nlm.nih.gov/pubmed/26795248
Saha A, Aoyama K, Taylor PA, Koehn BH, Veenstra RG, Panoskaltsis-Mortari A, et al. Host programmed death ligand 1 is dominant over programmed death ligand 2 expression in regulating graft-versus-host disease lethality. Blood. 2013;122(Oct):3062–73. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3811178&tool=pmcentrez&rendertype=abstract
Blazar BR, Carreno BM, Panoskaltsis-Mortari A, Carter L, Iwai Y, Yagita H, et al. Blockade of programmed death-1 engagement accelerates graft-versus-host disease lethality by an IFN-gamma-dependent mechanism. J Immunol. 2003;171(Aug):1272–7. http://www.ncbi.nlm.nih.gov/pubmed/12874215
Ikegawa S, Meguri Y, Kondo T, Sugiura H, Sando Y, Nakamura M. et al. PTCy ameliorates GVHD by restoring regulatory and effector T-cell homeostasis in recipients with PD-1 blockade. Blood Adv. 2019;3(Dec):4081–94.
Nieto JC, Roldán E, Jiménez I, Fox L, Carabia J, Ortí G, et al. Posttransplant cyclophosphamide after allogeneic hematopoietic cell transplantation mitigates the immune activation induced by previous nivolumab therapy. Leukemia. 2020; http://www.ncbi.nlm.nih.gov/pubmed/32393842. Accessed 27 Jul 2020 .
Abboud R, Keller J, Slade M, DiPersio JF, Westervelt P, Rettig MP, et al. Severe cytokine-release syndrome after T cell–replete peripheral blood haploidentical donor transplantation is associated with poor survival and anti–IL-6 therapy is safe and well tolerated. Biol Blood Marrow Transpl. 2016;22(Oct):1851–60. http://linkinghub.elsevier.com/retrieve/pii/S1083879116301458
Wachsmuth LP, Patterson MT, Eckhaus MA, Venzon DJ, Gress RE, Kanakry CG. Post-transplantation cyclophosphamide prevents graft-versus-host disease by inducing alloreactive T cell dysfunction and suppression. J Clin Investig. 2019;129:2357–73. http://www.ncbi.nlm.nih.gov/pubmed/30913039
Oran B, Garcia-Manero G, Saliba RM, Alfayez M, Al-Atrash G, Ciurea SO, et al. Posttransplantation cyclophosphamide improves transplantation outcomes in patients with AML/MDS who are treated with checkpoint inhibitors. Cancer. 2020;126(May):2193–205. http://www.ncbi.nlm.nih.gov/pubmed/32125707
Pasic I, Lipton JH, Kim DD, Viswabandya A, Kumar R, Lam W. et al. Post-transplant cyclophosphamide combined with anti-thymocyte globulin for graft-vs-host disease prophylaxis improves survival and lowers non-relapse mortality in older patients undergoing allogeneic hematopoietic cell transplantation. Ann Hematol. 2020;99(Jun):1377–87.
El-Cheikh J, Devillier R, Dulery R, Massoud R, Al Chami F, Ghaoui N, et al. Impact of adding antithymocyte globulin to posttransplantation cyclophosphamide in haploidentical stem-cell transplantation. Clin Lymphoma Myeloma Leuk 2020;20:617–23.
Mariotti J, Devillier R, Bramanti S, Sarina B, Furst S, Granata A, et al. T cell-replete haploidentical transplantation with post-transplantation cyclophosphamide for Hodgkin lymphoma relapsed after autologous transplantation: reduced incidence of relapse and of chronic graft-versus-host disease compared with HLA-identical related donors. Biol Blood Marrow Transpl. 2018;24:627–32. http://www.ncbi.nlm.nih.gov/pubmed/29197681
Acknowledgements
RWM acknowledges support from an ASH Research Training Award for Fellows, the ASH Clinical Research Training Institute, an ASBMT New Investigator Award, and the LRF Lymphoma Clinical Research Mentoring Program. This research was supported in part by National Institutes of Health award number P01 CA23766 and National Institutes of Health/National Cancer Institute Cancer Center Support Grant P30 CA008748. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work was supported in part by a grant from the Italian Association for Cancer Research (AIRC, grant #20575 to CC-S).
Author information
Authors and Affiliations
Contributions
RWM designed the research, collected and analyzed data, and wrote the paper. LC, LG, CdP, PA, PLZ, and CC-S designed the research, collected and analyzed data, and edited the paper. VTH, PC, AG, BC, DAB, SJ, MAS, SA, RL, GLS, M-AP, JMSdC, DB, AFH, GS, CS, SMA, YN, TB, MH, TAF, LD, AKS, JPM, TN, JC, AVS, JK, MM, RD, AS, RH, GM, M-PM-M, CO, KB, DM, RR, LL, AB, MJF, Y-BC, RCL, SDS, UR, MTB, JTR, JBC, SN, TP, RMJ, MR, AB, HJB, JS, VT, MS, MM, and AS collected data and edited the paper.
Corresponding author
Ethics declarations
Conflict of interest
RWM, LC, LG, VTH, PC, AG, BC, MAS, SA, RL, JMSdC, DB, LD, AKS, TB, GS, CS, SMA, AVS, M-PM-M, CO, KB, LL, A Beitinjaneh, UR, MM, RD, SN, TP, RMJ, MR, A Bashey, HJB, JTR, VT, MS, CdP, and MM—none. DAB—Honoraria: Seattle Genetics. SJ—Honoraria: Novartis, Kite, Juno, Takeda, CRISPR Therapeutics. GLS—Research funding: Janssen, Amgen. M-AP—honoraria from Abbvie, Bellicum, Celgene, Bristol-Myers Squibb, Incyte, Kite/Gilead, Merck, Novartis, Nektar Therapeutics, Omeros, and Takeda. He serves on DSMBs for Cidara Therapeutics, Servier and Medigene, and the scientific advisory boards of MolMed and NexImmune. He has received research support for clinical trials from Incyte, Kite/Gilead, and Miltenyi Biotec. He serves in a volunteer capacity as a member of the Board of Directors of Be The Match (National Marrow Donor Program, NMDP), as well as on the CIBMTR Cellular Immunotherapy Data Resource (CIDR) Executive Committee. AFH—Research funding: BMS, Merck, Genentech, Inc./F. Hoffmann-La Roche Ltd., Gilead Sciences, Seattle Genetics, Immune Design, AstraZeneca, Pharmacyclics. Consultancy: BMS, Merck, Genentech, Inc./F. Hoffmann-La Roche Ltd., Gilead Sciences, Seattle Genetics, Karyopharm. Travel, Accommodation, Expenses: BMS. YN—Consultant: Affimed. Research funds: Astra Zeneca, Affimed, Novartis, Secura Bio. MH—Research Support/Funding: Takeda Pharmaceutical Company; Astellas Pharma. Consultancy: Incyte Corporation; ADC Therapeutics; Celgene Corporation; Pharmacyclics, Magenta Therapeutics, Omeros, AbGenomics, Verastem, TeneoBio. Speaker’s Bureau: Sanofi Genzyme, AstraZeneca. TAF—Consultant./Ad Board: Seattle Genetics/BMS/Celgene/Karyopharm/KITE. Honoraria: Takeda/Celgene/Seattle Genetics/AbbVie/Pharmacyclics/Janssen/KITE/BMS. Speaker Bureau: Takeda/Celgene/Seattle Genetics/AbbVie/Pharmacyclics/Janssen/KITE/BMS. JPM—Research funding from Novartis, Fresenius Biotech, Astellas, Bellicum Pharmaceuticals, Gamida Cell, Kite Pharmaceuticals, Pluristem Ltd., Juno Therapeutics, and AlloVir. Advisory board and travel accommodations/expenses from Kite Pharmaceuticals, Juno Therapeutics AlloVir. Honoraria from Kite Pharmaceuticals and AlloVir. TN—Research funding: Novartis and Karypharm. JC—Personal fees: Kite/Gilead, Novartis, Morphosys, Bayer, Epyzime, AstraZeneca, Genentech, Karyopharm, Celgene/Juno. Research Support: Merck. JK—Research funding: Merck. AS—Honoraria: Celgene. Consultancy: Takeda. Other: Pfizer. RH—Honoraria: BMS, MSD, Gilead, Kite, Roche, Novartis, Janssen, and Celgene. GM—Honoraria: Bristol Myers Squibb. DM—Editorial board: MorphoSys. RR—Research funding: Merck. Consultancy/Advisory: BMS. MJF—Consultancy/Advisory board: Novartis, Kite/Gilead, Celgene/BMS, and Arcellx. Y-BC—Consulting: Magenta, Incyte, Abbvie, Daiichi, Equilium, Actinium, Takeda. RCL—Research funding: Juno Therapeutics, Takeda, TG Therapeutics, Incyte, Rhizen Pharmaceuticals, Bayer, Cyteir, Genentech. Consultancy: MorphoSys. SDS—Research funding: Acerta Pharma BV, Astrazeneca, Bayer, Beigene, Ayala, Bristol Myers Squibb, De Novo Biopharma, Genentech, Ignyta, Incyte Corporation, Merck, Sharp and Dohme Corp., Pharmacyclics, Portola Pharmaceuticals, Seattle Genetics. Consultancy or Advisory Board: Astrazeneca, Millenium/Takeda, Beigene, Karyopharm, KITE pharma. MTB—Research funding: Karyopahrm. Consulting: Concert, Celgene/Celularity. JBC—Research funding: BMS/Celgene. JS—Consultancy: Adaptive, AstraZeneca, Atara, BMS, Genmab, Imbrium, Pharmacyclics, and Seattle Genetics. Research Funding: AstraZeneca, BMS, Incyte, Merck, Pharmacyclics, Seattle Genetics, and TG. AS—Advisory Board: BMS, Servier, Gilead, Pfizer, Eisai, Bayer, MSD. Consultancy: Arqule, Sanofi. Speaker’s Bureau: Takeda, BMS, Roche, Abbvie, Amgen, Celgene, Servier, Gilead, AstraZeneca, Pfizer, Arqule, Lilly, Sandoz, Eisai, Novartis, Bayer, MSD. PA—Consultancy: Merck, BMS, Pfizer, Affimed, Adaptive, Infinity, ADC Therapeutics, Celgene, Morphosys, Daiichi Sankyo, Miltenyi, Tessa, GenMab, C4, Enterome. Research funding (inst): Merck, BMS, Affimed, Adaptive, Roche, Tensha, Otsuka, Sigma Tau, Genentech, IGM, Kite. Honoraria: Merck, BMS. PLZ—Consultancy: Verastem, MSD, Eusapharma, Sanofi. Speaker’s Bureau: Verastem, Celltrion, Gilead, Janssen-Cilag, BMS, Servier, MSD, Immune Design, Celgene, Portola, Roche, Eusapharma, Kyowa Kirin. Advisory Board: Verastem, Celltrion, Gilead, Janssen-Cilag, BMS, Servier, Sandoz, MSD, Immune Design, Celgene, Portola, Roche, Eusapharma, Kyowa Kirin, Sanofi. CC-S—Consultancy: Servier, ADC Therapeutics, Roche, Sanofi, BMS, Merck, Karyopharm. Honoraria: Janssen Oncology AstraZeneca. Research support: ADC Therapeutics, Rhizen Pharmaceuticals.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Merryman, R.W., Castagna, L., Giordano, L. et al. Allogeneic transplantation after PD-1 blockade for classic Hodgkin lymphoma. Leukemia 35, 2672–2683 (2021). https://doi.org/10.1038/s41375-021-01193-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-021-01193-6
This article is cited by
-
GVHD like skin eruption post-autologous stem cell transplantation
Bone Marrow Transplantation (2024)
-
Outcomes of allogeneic hematopoietic cell transplantation after bispecific antibodies in non-Hodgkin lymphomas
Bone Marrow Transplantation (2023)
-
Safety and efficacy of immune checkpoint inhibitors after allogeneic hematopoietic cell transplantation
Bone Marrow Transplantation (2023)
-
Single-center phase 2 study of PD-1 inhibitor combined with DNA hypomethylation agent + CAG regimen in patients with relapsed/refractory acute myeloid leukemia
Cancer Immunology, Immunotherapy (2023)
-
Allogeneic hematopoietic stem cell transplantation for NK/T-cell lymphoma: an international collaborative analysis
Leukemia (2023)