Abstract
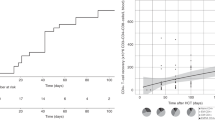
Double unit cord blood (dCB) transplantation (dCBT) is associated with high engraftment rates but delayed myeloid recovery. We investigated adding haplo-identical CD34+ cells to dCB grafts to facilitate early haplo-identical donor-derived neutrophil recovery (optimal bridging) prior to CB engraftment. Seventy-eight adults underwent myeloablation with cyclosporine-A/mycophenolate mofetil immunoprophylaxis (no antithymocyte globulin, ATG). CB units (median CD34+ dose 1.1 × 105/kg/unit) had a median 5/8 unit-recipient human leukocyte antigen (HLA)-match. Haplo-identical grafts had a median CD34+ dose of 5.2 × 106/kg. Of 77 evaluable patients, 75 had sustained CB engraftment that was mediated by a dominant unit and heralded by dominant unit-derived T cells. Optimal haplo-identical donor-derived myeloid bridging was observed in 34/77 (44%) patients (median recovery 12 days). Other engrafting patients had transient bridging with second nadir preceding CB engraftment (20/77 (26%), median first recovery 12 and second 26.5 days) or no bridge (21/77 (27%), median recovery 25 days). The 2 (3%) remaining patients had graft failure. Higher haplo-CD34+ dose and better dominant unit-haplo-CD34+ HLA-match significantly improved the likelihood of optimal bridging. Optimally bridged patients were discharged earlier (median 28 versus 36 days). ATG-free haplo-dCBT can speed neutrophil recovery but successful bridging is not guaranteed due to rapid haplo-identical graft rejection.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Brunstein CG, Gutman JA, Weisdorf DJ, Woolfrey AE, Defor TE, Gooley TA, et al. Allogeneic hematopoietic cell transplantation for hematologic malignancy: relative risks and benefits of double umbilical cord blood. Blood. 2010;116:4693–9.
Milano F, Gooley T, Wood B, Woolfrey A, Flowers ME, Doney K, et al. Cord-blood transplantation in patients with minimal residual disease. N Engl J Med. 2016;375:944–53.
Ponce DM, Hilden P, Devlin SM, Maloy M, Lubin M, Castro-Malaspina H, et al. High disease-free survival with enhanced protection against relapse after double-unit cord blood transplantation when compared with T cell-depleted unrelated donor transplantation in patients with acute leukemia and chronic myelogenous leukemia. Biol Blood Marrow Transplant. 2015;21:1985–93.
Barker JN, Weisdorf DJ, DeFor TE, Blazar BR, McGlave PB, Miller JS, et al. Transplantation of 2 partially HLA-matched umbilical cord blood units to enhance engraftment in adults with hematologic malignancy. Blood. 2005;105:1343–7.
Purtill D, Smith K, Devlin S, Meagher R, Tonon J, Lubin M, et al. Dominant unit CD34+ cell dose predicts engraftment after double-unit cord blood transplantation and is influenced by bank practice. Blood. 2014;124:2905–12.
Cutler C, Stevenson K, Kim HT, Brown J, McDonough S, Herrera M, et al. Double umbilical cord blood transplantation with reduced intensity conditioning and sirolimus-based GVHD prophylaxis. Bone Marrow Transplant. 2011;46:659–67.
Ballen KK, Spitzer TR, Yeap BY, McAfee S, Dey BR, Attar E, et al. Double unrelated reduced-intensity umbilical cord blood transplantation in adults. Biol Blood Marrow Transplant. 2007;13:82–9.
Fernandez MN, Regidor C, Cabrera R, Garcia-Marco JA, Fores R, Sanjuan I, et al. Unrelated umbilical cord blood transplants in adults: early recovery of neutrophils by supportive co-transplantation of a low number of highly purified peripheral blood CD34+ cells from an HLA-haploidentical donor. Exp Hematol. 2003;31:535–44.
Magro E, Regidor C, Cabrera R, Sanjuan I, Fores R, Garcia-Marco JA, et al. Early hematopoietic recovery after single unit unrelated cord blood transplantation in adults supported by co-infusion of mobilized stem cells from a third party donor. Haematologica. 2006;91:640–8.
Bautista G, Cabrera JR, Regidor C, Fores R, Garcia-Marco JA, Ojeda E, et al. Cord blood transplants supported by co-infusion of mobilized hematopoietic stem cells from a third-party donor. Bone Marrow Transplant. 2009;43:365–73.
Kwon M, Bautista G, Balsalobre P, Sanchez-Ortega I, Serrano D, Anguita J, et al. Haplo-cord transplantation using CD34+ cells from a third-party donor to speed engraftment in high-risk patients with hematologic disorders. Biol Blood Marrow Transplant. 2014;20:2015–22.
Liu H, Rich ES, Godley L, Odenike O, Joseph L, Marino S, et al. Reduced-intensity conditioning with combined haploidentical and cord blood transplantation results in rapid engraftment, low GVHD, and durable remissions. Blood. 2011;118:6438–45.
Lindemans CA, Te Boome LC, Admiraal R, Jol-van der Zijde EC, Wensing AM, Versluijs AB, et al. Sufficient Immunosuppression with thymoglobulin is essential for a successful haplo-myeloid bridge in haploidentical-cord blood transplantation. Biol Blood Marrow Transplant. 2015;21:1839–45.
van Besien K, Childs R. Haploidentical cord transplantation—the best of both worlds. Semin Hematol. 2016;53:257–66.
Brunstein CG, Weisdorf DJ, DeFor T, Barker JN, Tolar J, van Burik JA, et al. Marked increased risk of Epstein-Barr virus-related complications with the addition of antithymocyte globulin to a nonmyeloablative conditioning prior to unrelated umbilical cord blood transplantation. Blood. 2006;108:2874–80.
Komanduri KV, St John LS, de Lima M, McMannis J, Rosinski S, McNiece I, et al. Delayed immune reconstitution after cord blood transplantation is characterized by impaired thymopoiesis and late memory T-cell skewing. Blood. 2007;110:4543–51.
Jacobson CA, Turki AT, McDonough SM, Stevenson KE, Kim HT, Kao G, et al. Immune reconstitution after double umbilical cord blood stem cell transplantation: comparison with unrelated peripheral blood stem cell transplantation. Biol Blood Marrow Transplant. 2012;18:565–74.
Jain N, Liu H, Artz AS, Anastasi J, Odenike O, Godley LA, et al. Immune reconstitution after combined haploidentical and umbilical cord blood transplant. Leuk Lymphoma. 2013;54:1242–9.
Lindemans CA, Chiesa R, Amrolia PJ, Rao K, Nikolajeva O, de Wildt A, et al. Impact of thymoglobulin prior to pediatric unrelated umbilical cord blood transplantation on immune reconstitution and clinical outcome. Blood. 2014;123:126–32.
Admiraal R, Lindemans CA, van Kesteren C, Bierings MB, Versluijs AB, Nierkens S, et al. Excellent T-cell reconstitution and survival depend on low ATG exposure after pediatric cord blood transplantation. Blood. 2016;128:2734–41.
Castillo N, Garcia-Cadenas I, Barba P, Canals C, Diaz-Heredia C, Martino R, et al. Early and long-term impaired T lymphocyte immune reconstitution after cord blood transplantation with antithymocyte globulin. Biol Blood Marrow Transplant. 2017;23:491–7.
Pascal L, Mohty M, Ruggeri A, Tucunduva L, Milpied N, Chevallier P, et al. Impact of rabbit ATG-containing myeloablative conditioning regimens on the outcome of patients undergoing unrelated single-unit cord blood transplantation for hematological malignancies. Bone Marrow Transplant. 2015;50:45–50.
Pascal L, Tucunduva L, Ruggeri A, Blaise D, Ceballos P, Chevallier P, et al. Impact of ATG-containing reduced-intensity conditioning after single- or double-unit allogeneic cord blood transplantation. Blood. 2015;126:1027–32.
Shouval R, Ruggeri A, Labopin M, Mohty M, Sanz G, Michel G, et al. An integrative scoring system for survival prediction following umbilical cord blood transplantation in acute leukemia. Clin Cancer Res. 2017;23:6478–86.
Tozatto-Maio K, Giannotti F, Labopin M, Ruggeri A, Volt F, Paviglianiti A, et al. Cord blood unit dominance analysis and effect of the winning unit on outcomes after double-unit umbilical cord blood transplantation in adults with acute leukemia: a retrospective study on behalf of Eurocord, the Cord Blood Committee of Cellular Therapy, Immunobiology Working Party, and the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2018;24:1657–63.
Wakamatsu M, Terakura S, Ohashi K, Fukuda T, Ozawa Y, Kanamori H, et al. Impacts of thymoglobulin in patients with acute leukemia in remission undergoing allogeneic HSCT from different donors. Blood Adv. 2019;3:105–15.
Ballen K, Logan BR, Chitphakdithai P, Kuxhausen M, Spellman SR, Adams A, et al. Unlicensed umbilical cord blood units provide a safe and effective graft source for a diverse population: a study of 2456 umbilical cord blood recipients. Biol Blood Marrow Transplant. 2020;26:745–57.
Dahi PB, Barone J, Devlin SM, Byam C, Lubin M, Ponce DM, et al. Sustained donor engraftment in recipients of double-unit cord blood transplantation is possible despite donor-specific human leukoctye antigen antibodies. Biol Blood Marrow Transplant. 2014;20:735–9.
Barker JN, Byam C, Scaradavou A. How I treat: the selection and acquisition of unrelated cord blood grafts. Blood. 2011;117:2332–9.
Barker JN, Kurtzberg J, Ballen K, Boo M, Brunstein C, Cutler C, et al. Optimal practices in unrelated donor cord blood transplantation for hematologic malignancies. Biol Blood Marrow Transplant. 2017;23:882–96.
Ponce DM, Sauter C, Devlin S, Lubin M, Gonzales AM, Kernan NA, et al. A novel reduced-intensity conditioning regimen induces a high incidence of sustained donor-derived neutrophil and platelet engraftment after double-unit cord blood transplantation. Biol Blood Marrow Transplant. 2013;19:799–803.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
Avery S, Shi W, Lubin M, Gonzales AM, Heller G, Castro-Malaspina H, et al. Influence of infused cell dose and HLA match on engraftment after double-unit cord blood allografts. Blood. 2011;117:3277–85.
Kwon M, Martinez-Laperche C, Balsalobre P, Serrano D, Anguita J, Gayoso J, et al. Early peripheral blood and T-cell chimerism dynamics after umbilical cord blood transplantation supported with haploidentical cells. Bone Marrow Transplant. 2014;49:212–8.
Ramirez P, Wagner JE, DeFor TE, Blazar BR, Verneris MR, Miller JS, et al. Factors predicting single-unit predominance after double umbilical cord blood transplantation. Bone Marrow Transplant. 2012;47:799–803.
Scaradavou A, Smith KM, Hawke R, Schaible A, Abboud M, Kernan NA, et al. Cord blood units with low CD34+ cell viability have a low probability of engraftment after double unit transplantation. Biol Blood Marrow Transplant. 2010;16:500–8.
Tsai SB, Liu H, Shore T, Fan Y, Bishop M, Cushing MM, et al. Frequency and risk factors associated with cord graft failure after transplant with single-unit umbilical cord cells supplemented by haploidentical cells with reduced-intensity conditioning. Biol Blood Marrow Transplant. 2016;22:1065–72.
van Besien K, Koshy N, Gergis U, Mayer S, Cushing M, Rennert H, et al. Cord blood chimerism and relapse after haplo-cord transplantation. Leuk Lymphoma. 2017;58:288–97.
van Besien K, Koshy N, Gergis U, Mayer S, Cushing M, Rennert H, et al. Haplo-cord transplant: HLA-matching determines graft dominance. Leuk Lymphoma. 2017;58:1512–4.
Politikos I, Lavery JA, Hilden P, Cho C, Borrill T, Maloy MA, et al. Robust CD4+ T-cell recovery in adults transplanted with cord blood and no antithymocyte globulin. Blood Adv. 2020;4:191–202.
Stritesky G, Wadsworth K, Duffy M, Buck K, Dehn J. Evaluation of the impact of banking umbilical cord blood units with high cell dose for ethnically diverse patients. Transfusion. 2018;58:345–51.
Magalon J, Maiers M, Kurtzberg J, Navarrete C, Rubinstein P, Brown C, et al. Banking or bankrupting: strategies for sustaining the economic future of public cord blood banks. PLoS ONE. 2015;10:e0143440.
Delaney C, Heimfeld S, Brashem-Stein C, Voorhies H, Manger RL, Bernstein ID. Notch-mediated expansion of human cord blood progenitor cells capable of rapid myeloid reconstitution. Nat Med. 2010;16:232–6.
de Lima M, McNiece I, Robinson SN, Munsell M, Eapen M, Horowitz M, et al. Cord-blood engraftment with ex vivo mesenchymal-cell coculture. N Engl J Med. 2012;367:2305–15.
Butler JM, Gars EJ, James DJ, Nolan DJ, Scandura JM, Rafii S. Development of a vascular niche platform for expansion of repopulating human cord blood stem and progenitor cells. Blood. 2012;120:1344–7.
Fares I, Chagraoui J, Gareau Y, Gingras S, Ruel R, Mayotte N, et al. Cord blood expansion. Pyrimidoindole derivatives are agonists of human hematopoietic stem cell self-renewal. Science. 2014;345:1509–12.
Popat U, Mehta RS, Rezvani K, Fox P, Kondo K, Marin D, et al. Enforced fucosylation of cord blood hematopoietic cells accelerates neutrophil and platelet engraftment after transplantation. Blood. 2015;125:2885–92.
Wagner JE Jr., Brunstein CG, Boitano AE, DeFor TE, McKenna D, Sumstad D, et al. Phase I/II trial of StemRegenin-1 expanded umbilical cord blood hematopoietic stem cells supports testing as a stand-alone graft. Cell Stem Cell. 2016;18:144–55.
Horwitz ME, Wease S, Blackwell B, Valcarcel D, Frassoni F, Boelens JJ, et al. Phase I/II study of stem-cell transplantation using a single cord Blood unit expanded ex vivo with nicotinamide. J Clin Oncol. 2019;37:367–74.
Cohen S, Roy J, Lachance S, Delisle JS, Marinier A, Busque L, et al. Hematopoietic stem cell transplantation using single UM171-expanded cord blood: a single-arm, phase 1-2 safety and feasibility study. Lancet Haematol. 2020;7:e134–45.
Kosuri S, Wolff T, Devlin SM, Byam C, Mazis CM, Naputo K, et al. Prospective evaluation of unrelated donor cord blood and haploidentical donor access reveals graft availability varies by patient ancestry: practical implications for donor selection. Biol Blood Marrow Transplant. 2017;23:965–70.
Milano F, Rezvani AR, Kurtzberg J, Karanes C, Gutman JA, Duncan C, et al. No engraftment advantage after single or double umbilical cord blood transplant (CBT) with the addition of a non-hla matched off-the-shelf expanded cord blood unit compared to conventional cbt: results of a randomized trial. Blood. 2019;134 Suppl 1:146.
Acknowledgements
This work was supported in part by the National Institutes of Health (NIH) Grant P01 CA23766 and NIH/NCI Cancer Center Support Grant P30 CA008748. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
JNB and RJOR designed the clinical trial (NCT01682226). IP and JNB assembled and analyzed the data, and wrote the paper. SMD and IP performed the statistical analysis. MAM, KAN, JDR, and CMM maintained the patient database and procured data for the study. MEA, JCB, and STA were responsible for the whole blood and white cell subset chimerism assays. IP, PBD, SAG, AAJ, EBP, MAP, CSS, RT, DMP, and JNB provided patient care. IP, SMD, JCB, AS, STA, PBD, SAG, KCH, AAJ, EBP, MAP, CSS, RT, DMP, RJOR, and JNB interpreted the data, reviewed and edited the paper. All authors have approved the submitted version of the paper.
Corresponding authors
Ethics declarations
Conflict of interest
IP has received research funding from Merck and serves on a Data and Safety Monitoring Board (DSMB) for ExCellThera. AS serves on a DSMB for ExcellThera and is the medical director of the New York Blood Center/National Cord Blood Program. STA has received honoraria from Abbott Laboratories. SAG has served as a consultant for Amgen, Actinium, Celgene, Johnson & Johnson, Jazz pharmaceutical, Takeda, Novartis, Kite, Spectrum Pharma and has received research funding from Amgen, Actinium, Celgene, Johnson & Johnson, Miltenyi, Takeda. MAP has received honoraria from Abbvie, Bellicum, Bristol-Myers Squibb, Incyte, Merck, Novartis, Nektar Therapeutics, and Takeda; serves on DSMBs for Servier and Medigene, and the scientific advisory boards of MolMed and NexImmune; and has received research support for clinical trials from Incyte, Kite (Gilead) and Miltenyi Biotec. CSS has served as a paid consultant on advisory boards for Juno Therapeutics, Sanofi-Genzyme, Spectrum Pharmaceuticals, Novartis, Genmab, Precision Biosciences, Kite, a Gilead Company, Celgene, Gamida Cell, Pfizer, and GSK, and has received research funding for clinical trials from Juno Therapeutics, Celgene, Precision Biosciences and Sanofi-Genzyme. RJOR receives royalties from Atara Biotherapeutics. JNB has received research funding from Angiocrine Bioscience, Gamida Cell, and Merck. The authors have no other relevant conflicts of interest to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Politikos, I., Devlin, S.M., Arcila, M.E. et al. Engraftment kinetics after transplantation of double unit cord blood grafts combined with haplo-identical CD34+ cells without antithymocyte globulin. Leukemia 35, 850–862 (2021). https://doi.org/10.1038/s41375-020-0922-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-020-0922-x