Abstract
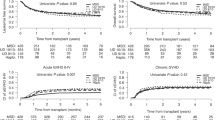
This study aimed to investigate graft-versus-leukemia (GVL) of haploidentical donor (HID) compared with HLA-matched sibling donor (MSD) for high-risk acute myeloid leukemia (H-AML) in first complete remission (CR1). One hundred and eighty-nine patients with H-AML in CR1 were enrolled in this multicentre prospective cohort study. Patients were assigned to groups transplanted with HID (n = 83) or MSD (n = 106) based on donor availability (biological randomization). The primary endpoint was the incidence of MRD positivity posttransplantation (post-MRD+). All post-MRD+ patients received preemptive interventions. The cumulative incidences of post-MRD+ were 18 and 42% in HID and MSD groups, respectively, (p < 0.001). Fifty-two patients received preemptive DLI, including 13 (16%) in HID and 39 cases (37%) in MSD groups (p = 0.001). Among HID and MSD groups, the 3-year cumulative incidence of relapse were 14 and 24% (p = 0.101); the 3-year cumulative incidence of treatment-related mortality were 15 and 10% (p = 0.368); the 3-year overall survival rates were 72 and 68% (p = 0.687); the 3-year disease-free-survival were 71 and 66% (p = 0.579); the 3-year graft-versus-host disease and relapse free survival were 63 and 43% (p = 0.035), respectively. HID might have a stronger GVL than MSD in H-AML patients. HID transplantation as postremission therapy should be recommended as one of the optimal choices for H-AML patients in CR1.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Cornelissen JJ, Gratwohl A, Schlenk RF, Sierra J, Bornhauser M, Juliusson G, et al. The European LeukemiaNet AML Working Party consensus statement on allogeneic HSCT for patients with AML in remission: an integrated-risk adapted approach. Nat Rev Clin Oncol. 2012;9:579–90. https://doi.org/10.1038/nrclinonc.2012.150.
Dohner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Buchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–47. https://doi.org/10.1182/blood-2016-08-733196.
Hamilton BK, Copelan EA. Concise review: the role of hematopoietic stem cell transplantation in the treatment of acute myeloid leukemia. Stem Cells. 2012;30:1581–6. https://doi.org/10.1002/stem.1140.
O’Donnell MR, Tallman MS, Abboud CN, Altman JK, Appelbaum FR, Arber DA, et al. Acute myeloid leukemia, version 3.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2017;15:926–57. https://doi.org/10.6004/jnccn.2017.0116.
Chang YJ, Luznik L, Fuchs EJ, Huang XJ. How do we choose the best donor for T-cell-replete, HLA-haploidentical transplantation? J Hematol Oncol. 2016;9:35 https://doi.org/10.1186/s13045-016-0265-2.
Lee CJ, Savani BN, Mohty M, Labopin M, Ruggeri A, Schmid C, et al. Haploidentical hematopoietic cell transplantation for adult acute myeloid leukemia: a position statement from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2017;102:1810–22. https://doi.org/10.3324/haematol.2017.176107.
Bashey A, Zhang X, Sizemore CA, Manion K, Brown S, Holland HK, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol. 2013;31:1310–6. https://doi.org/10.1200/JCO.2012.44.3523.
Versluis J, Labopin M, Ruggeri A, Socie G, Wu D, Volin L, et al. Alternative donors for allogeneic hematopoietic stem cell transplantation in poor-risk AML in CR1. Blood Adv. 2017;1:477–85. https://doi.org/10.1182/bloodadvances.2016002386.
Wang Y, Liu QF, Xu LP, Liu KY, Zhang XH, Ma X, et al. Haploidentical vs identical-sibling transplant for AML in remission: a multicenter, prospective study. Blood. 2015;125:3956–62. https://doi.org/10.1182/blood-2015-02-627786.
Chang YJ, Wang Y, Liu YR, Xu LP, Zhang XH, Chen H, et al. Haploidentical allograft is superior to matched sibling donor allograft in eradicating pre-transplantation minimal residual disease of AML patients as determined by multiparameter flow cytometry: a retrospective and prospective analysis. J Hematol Oncol. 2017;10:134. https://doi.org/10.1186/s13045-017-0502-3.
Salvatore D, Labopin M, Ruggeri A, Battipaglia G, Ghavamzadeh A, Ciceri F, et al. Outcomes of hematopoietic stem cell transplantation from unmanipulated haploidentical versus matched sibling donor in patients with acute myeloid leukemia in first complete remission with intermediate or high-risk cytogenetics: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2018;103:1317–28. https://doi.org/10.3324/haematol.2018.189258.
Ringden O, Labopin M, Ciceri F, Velardi A, Bacigalupo A, Arcese W, et al. Is there a stronger graft-versus-leukemia effect using HLA-haploidentical donors compared with HLA-identical siblings? Leukemia. 2016;30:447–55. https://doi.org/10.1038/leu.2015.232.
Wang Y, Liu DH, Xu LP, Liu KY, Chen H, Chen YH, et al. Superior graft-versus-leukemia effect associated with transplantation of haploidentical compared with HLA-identical sibling donor grafts for high-risk acute leukemia: an historic comparison. Biol Blood Marrow Transpl. 2011;17:821–30. https://doi.org/10.1016/j.bbmt.2010.08.023.
Araki D, Wood BL, Othus M, Radich JP, Halpern AB, Zhou Y, et al. Allogeneic hematopoietic cell transplantation for acute myeloid leukemia: time to move toward a minimal residual disease-based definition of complete remission? J Clin Oncol. 2016;34:329–36. https://doi.org/10.1200/JCO.2015.63.3826.
Chen X, Xie H, Wood BL, Walter RB, Pagel JM, Becker PS, et al. Relation of clinical response and minimal residual disease and their prognostic impact on outcome in acute myeloid leukemia. J Clin Oncol. 2015;33:1258–64. https://doi.org/10.1200/JCO.2014.58.3518.
Walter RB, Buckley SA, Pagel JM, Wood BL, Storer BE, Sandmaier BM, et al. Significance of minimal residual disease before myeloablative allogeneic hematopoietic cell transplantation for AML in first and second complete remission. Blood. 2013;122:1813–21. https://doi.org/10.1182/blood-2013-06-506725.
Walter RB, Gyurkocza B, Storer BE, Godwin CD, Pagel JM, Buckley SA, et al. Comparison of minimal residual disease as outcome predictor for AML patients in first complete remission undergoing myeloablative or nonmyeloablative allogeneic hematopoietic cell transplantation. Leukemia. 2015;29:137–44. https://doi.org/10.1038/leu.2014.173.
Zhou Y, Othus M, Araki D, Wood BL, Radich JP, Halpern AB, et al. Pre- and post-transplant quantification of measurable ('minimal') residual disease via multiparameter flow cytometry in adult acute myeloid leukemia. Leukemia. 2016;30:1456–64. https://doi.org/10.1038/leu.2016.46.
San Miguel JF, Vidriales MB, Lopez-Berges C, Diaz-Mediavilla J, Gutierrez N, Canizo C, et al. Early immunophenotypical evaluation of minimal residual disease in acute myeloid leukemia identifies different patient risk groups and may contribute to postinduction treatment stratification. Blood. 2001;98:1746–51.
Zhao XS, Liu YR, Zhu HH, Xu LP, Liu DH, Liu KY, et al. Monitoring MRD with flow cytometry: an effective method to predict relapse for ALL patients after allogeneic hematopoietic stem cell transplantation. Ann Hematol. 2012;91:183–92. https://doi.org/10.1007/s00277-011-1285-1.
Zhao XS, Jin S, Zhu HH, Xu LP, Liu DH, Chen H, et al. Wilms tumor gene 1 expression: an independent acute leukemia prognostic indicator following allogeneic hematopoietic SCT. Bone Marrow Transpl. 2012;47:499–507. https://doi.org/10.1038/bmt.2011.121.
Yan CH, Liu DH, Liu KY, Xu LP, Liu YR, Chen H, et al. Risk stratification-directed donor lymphocyte infusion could reduce relapse of standard-risk acute leukemia patients after allogeneic hematopoietic stem cell transplantation. Blood. 2012;119:3256–62. https://doi.org/10.1182/blood-2011-09-380386.
Xu L, Chen H, Chen J, Han M, Huang H, Lai Y, et al. The consensus on indications, conditioning regimen, and donor selection of allogeneic hematopoietic cell transplantation for hematological diseases in China-recommendations from the Chinese Society of Hematology. J Hematol Oncol. 2018;11:33. https://doi.org/10.1186/s13045-018-0564-x.
Han LJ, Wang Y, Fan ZP, Huang F, Zhou J, Fu YW, et al. Haploidentical transplantation compared with matched sibling and unrelated donor transplantation for adults with standard-risk acute lymphoblastic leukaemia in first complete remission. Br J Haematol. 2017;179:120–30. https://doi.org/10.1111/bjh.14854.
Lin R, Wang Y, Huang F, Fan Z, Zhang S, Yang T, et al. Two dose levels of rabbit antithymocyte globulin as graft-versus-host disease prophylaxis in haploidentical stem cell transplantation: a multicenter randomized study. BMC Med. 2019;17:156. https://doi.org/10.1186/s12916-019-1393-7.
Schuurhuis GJ, Heuser M, Freeman S, Bene MC, Buccisano F, Cloos J, et al. Minimal/measurable residual disease in AML: a consensus document from the European LeukemiaNet MRD Working Party. Blood. 2018;131:1275–91. https://doi.org/10.1182/blood-2017-09-801498.
Wang Y, Liu DH, Xu LP, Liu KY, Chen H, Zhang XH, et al. Prevention of relapse using granulocyte CSF-primed PBPCs following HLA-mismatched/haploidentical, T-cell-replete hematopoietic SCT in patients with advanced-stage acute leukemia: a retrospective risk-factor analysis. Bone Marrow Transpl. 2012;47:1099–104. https://doi.org/10.1038/bmt.2011.213.
Xuan L, Huang F, Fan Z, Zhou H, Zhang X, Yu G, et al. Effects of intensified conditioning on Epstein-Barr virus and cytomegalovirus infections in allogeneic hematopoietic stem cell transplantation for hematological malignancies. J Hematol Oncol. 2012;5:46. https://doi.org/10.1186/1756-8722-5-46.
Lu DP, Dong L, Wu T, Huang XJ, Zhang MJ, Han W, et al. Conditioning including antithymocyte globulin followed by unmanipulated HLA-mismatched/haploidentical blood and marrow transplantation can achieve comparable outcomes with HLA-identical sibling transplantation. Blood. 2006;107:3065–73. https://doi.org/10.1182/blood-2005-05-2146.
Holtan SG, DeFor TE, Lazaryan A, Bejanyan N, Arora M, Brunstein CG, et al. Composite end point of graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation. Blood. 2015;125:1333–8. https://doi.org/10.1182/blood-2014-10-609032.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transpl. 1995;15:825–8.
Horwitz ME, Sullivan KM. Chronic graft-versus-host disease. Blood Rev. 2006;20:15–27. https://doi.org/10.1016/j.blre.2005.01.007.
Austin PC, Fine JP. Practical recommendations for reporting fine-gray model analyses for competing risk data. Stat Med. 2017;36:4391–400. https://doi.org/10.1002/sim.7501.
Liu Y, Huang X, Fei Q, Xu L, Zhang X, Liu K, et al. Comparison analysis between haplo identical stem cell transplantation and matched sibling donor stem cell transplantation for high-risk acute myeloid leukemia in first complete remission. Sci China Life Sci. 2018. https://doi.org/10.1007/s11427-018-9361-2.
Ottinger HD, Ferencik S, Beelen DW, Lindemann M, Peceny R, Elmaagacli AH, et al. Hematopoietic stem cell transplantation: contrasting the outcome of transplantations from HLA-identical siblings, partially HLA-mismatched related donors, and HLA-matched unrelated donors. Blood. 2003;102:1131–7. https://doi.org/10.1182/blood-2002-09-2866.
Luo Y, Xiao H, Lai X, Shi J, Tan Y, He J, et al. T-cell-replete haploidentical HSCT with low-dose anti-T-lymphocyte globulin compared with matched sibling HSCT and unrelated HSCT. Blood. 2014;124:2735–43. https://doi.org/10.1182/blood-2014-04-571570.
Wang Y, Liu DH, Fan ZP, Sun J, Wu XJ, Ma X, et al. Prevention of relapse using DLI can increase survival following HLA-identical transplantation in patients with advanced-stage acute leukemia: a multi-center study. Clin Transpl. 2012;26:635–43. https://doi.org/10.1111/j.1399-0012.2012.01626.x.
Platzbecker U, Middeke JM, Sockel K, Herbst R, Wolf D, Baldus CD, et al. Measurable residual disease-guided treatment with azacitidine to prevent haematological relapse in patients with myelodysplastic syndrome and acute myeloid leukaemia (RELAZA2): an open-label, multicentre, phase 2 trial. Lancet Oncol. 2018;19:1668–79. https://doi.org/10.1016/S1470-2045(18)30580-1.
Platzbecker U, Wermke M, Radke J, Oelschlaegel U, Seltmann F, Kiani A, et al. Azacitidine for treatment of imminent relapse in MDS or AML patients after allogeneic HSCT: results of the RELAZA trial. Leukemia. 2012;26:381–9. https://doi.org/10.1038/leu.2011.234.
Xuan L, Wang Y, Huang F, Jiang E, Deng L, Wu B, et al. Effect of sorafenib on the outcomes of patients with FLT3-ITD acute myeloid leukemia undergoing allogeneic hematopoietic stem cell transplantation. Cancer. 2018;124:1954–63. https://doi.org/10.1002/cncr.31295.
Wang Y, Liu QF, Xu LP, Liu KY, Zhang XH, Ma X, et al. Haploidentical versus matched-sibling transplant in adults with philadelphia-negative high-risk acute lymphoblastic leukemia: a biologically phase III randomized study. Clin Cancer Res. 2016;22:3467–76. https://doi.org/10.1158/1078-0432.CCR-15-2335.
Chang YJ, Huang XJ. Is human leukocyte antigen-matched sibling donor transplant always better than haploidentical allograft? Semin Hematol. 2019;56:201–8. https://doi.org/10.1053/j.seminhematol.2018.07.005.
Tang F, Xu Y, Chen H, Xu L, Zhang X, Wang Y, et al. Comparison of the clinical outcomes of hematologic malignancies after myeloablative haploidentical transplantation with G-CSF/ATG and posttransplant cyclophosphamide: results from the Chinese Bone Marrow Transplantation Registry Group (CBMTRG). Sci China Life Sci. 2019. https://doi.org/10.1007/s11427-019-9594-7.
Ruggeri A, Sun Y, Labopin M, Bacigalupo A, Lorentino F, Arcese W, et al. Post-transplant cyclophosphamide versus anti-thymocyte globulin as graft- versus-host disease prophylaxis in haploidentical transplant. Haematologica. 2017;102:401–10. https://doi.org/10.3324/haematol.2016.151779.
Rubio MT, Savani BN, Labopin M, Piemontese S, Polge E, Ciceri F, et al. Impact of conditioning intensity in T-replete haplo-identical stem cell transplantation for acute leukemia: a report from the acute leukemia working party of the EBMT. J Hematol Oncol. 2016;9:25. https://doi.org/10.1186/s13045-016-0248-3.
Ghosh N, Karmali R, Rocha V, Ahn KW, DiGilio A, Hari PN, et al. Reduced-intensity transplantation for lymphomas using haploidentical related donors versus HLA-matched sibling donors: a center for international blood and marrow transplant research analysis. J Clin Oncol. 2016;34:3141–9. https://doi.org/10.1200/JCO.2015.66.3476.
Binkert L, Medinger M, Halter JP, Heim D, Gerull S, Holbro A, et al. Lower dose anti-thymocyte globulin for GvHD prophylaxis results in improved survival after allogeneic stem cell transplantation. Bone Marrow Transpl. 2015;50:1331–6. https://doi.org/10.1038/bmt.2015.148.
Lin R, Liu Q. Diagnosis and treatment of viral diseases in recipients of allogeneic hematopoietic stem cell transplantation. J Hematol Oncol. 2013;6:94. https://doi.org/10.1186/1756-8722-6-94.
Acknowledgements
This work was supported by the National Key Research and Development Programme of China (Grant nos. 2017YFA105500, 2017YFA105504), the National Natural Science Foundation of China (nos. 81770190, 81700176, 81470349, and 81770189), the Science and Technology Program of Guangdong Province (Grant nos. 2014B020226004, 2016B030230003), the Science and Technology Program of Guangzhou (Grant no. 201704020214). We thank all the faculty members that participated in this study.
Author information
Authors and Affiliations
Contributions
Conception and design: Q-FL, X-JH. Acquisition of data (acquired and managed patients, provided facilities, etc.): S-JY, FH, YW, Z-PF, RL, NX, LX, TY, Y-JX, J-YY, W-JY and JS. Analysis and interpretation of data (e.g., statistical analysis, biostatistics, and computational analysis): S-JY, FH, YW. Writing, review, and/or revision of the paper: Q-FL, X-JH, S-JY, FH, and YW. Administrative, technical, or material support (i.e., reporting or organizing data, constructing databases): Q-FL, X-JH. Study supervision: Q-FL, X-JH.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yu, S., Huang, F., Wang, Y. et al. Haploidentical transplantation might have superior graft-versus-leukemia effect than HLA-matched sibling transplantation for high-risk acute myeloid leukemia in first complete remission: a prospective multicentre cohort study. Leukemia 34, 1433–1443 (2020). https://doi.org/10.1038/s41375-019-0686-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-019-0686-3
This article is cited by
-
Haploidentical transplants deliver equal outcomes to matched sibling transplants: a propensity score-matched analysis
Journal of Translational Medicine (2023)
-
Autologous stem cell transplantation in adult patients with intermediate-risk acute myeloid leukemia in first complete remission and no detectable minimal residual disease. A comparative retrospective study with haploidentical transplants of the global committee and the ALWP of the EBMT
Bone Marrow Transplantation (2023)
-
Epstein–Barr virus reactivation correlates with worse outcomes for patients exposed to hepatitis B virus after haploidentical hematopoietic stem cell transplantation
Annals of Hematology (2023)
-
Venetoclax Combined with Azacitidine and Homoharringtonine in Relapsed/Refractory AML: A Multicenter, Phase 2 Trial
Journal of Hematology & Oncology (2023)
-
Non-T-depleted haploidentical transplantation with post-transplant cyclophosphamide in patients with secondary versus de novo AML in first complete remission: a study from the ALWP/EBMT
Journal of Hematology & Oncology (2023)