Abstract
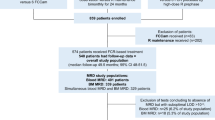
Approximately half of patients with chronic myeloid leukemia (CML) in sustained deep molecular response who discontinue tyrosine kinase inhibitors (TKIs) remain in treatment-free remission (TFR). Some of these patients have measurable residual disease (MRD) by BCR-ABL1 mRNA testing, and most have detectable BCR-ABL1 DNA by highly sensitive methods. We used fluorescence-activated cell sorting and BCR-ABL1 DNA PCR to investigate the lineage of residual CML cells in TFR. Twenty patients in TFR for >1 year provided blood for sorting into granulocytes, monocytes, B cells, T cells, and NK cells. MRD was identified predominantly in the lymphoid compartment and never in granulocytes. B cells were more often BCR-ABL1 positive than T cells (18 vs 11/20 patients) and at higher levels (median 10−4.9 vs 10−5.7; P = 0.014). In 13 CML patients studied at diagnosis lymphocytes expressing BCR-ABL1 mRNA comprised a small proportion of total leukocytes. These data improve our understanding of TFR biology, since it is now clear that MRD in the blood of TFR patients need not imply the persistence of multipotent CML cells. Lineage-specific assessment of MRD could be explored as a means to improve the prediction of TFR.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Ross DM, Branford S, Seymour JF, Schwarer AP, Arthur C, Yeung DT, et al. Safety and efficacy of imatinib cessation for CML patients with stable undetectable minimal residual disease: results from the TWISTER study. Blood. 2013;122:515–22.
Rousselot P, Charbonnier A, Cony-Makhoul P, Agape P, Nicolini FE, Varet B, et al. Loss of major molecular response as a trigger for restarting tyrosine kinase inhibitor therapy in patients with chronic-phase chronic myelogenous leukemia who have stopped imatinib after durable undetectable disease. J Clin Oncol. 2014;32:424–30.
Imagawa J, Tanaka H, Okada M, Nakamae H, Hino M, Murai K, et al. Discontinuation of dasatinib in patients with chronic myeloid leukaemia who have maintained deep molecular response for longer than 1 year (DADI trial): a multicentre phase 2 trial. Lancet Haematol. 2015;2:e528–535.
Etienne G, Guilhot J, Rea D, Rigal-Huguet F, Nicolini F, Charbonnier A, et al. Long-term follow-up of the French Stop Imatinib (STIM1) study in patients with chronic myeloid leukemia. J Clin Oncol. 2017;35:298–305.
Ross DM, Pagani IS, Shanmuganathan N, Kok CH, Seymour JF, Mills AK, et al. Long-term treatment-free remission of chronic myeloid leukemia with falling levels of residual leukemic cells. Leukemia. 2018;32:2572–9.
Ross DM, Masszi T, Casares MTG, Hellmann A, Stentoft J, Conneally E, et al. Durable treatment-free remission in patients with chronic myeloid leukemia in chronic phase following frontline nilotinib: 96-week update of the ENESTfreedom study. J Cancer Res Clin Oncol. 2018;144:945–54.
Saussele S, Richter J, Guilhot J, Gruber FX, Hjorth-Hansen H, Almeida A, et al. Discontinuation of tyrosine kinase inhibitor therapy in chronic myeloid leukaemia (EURO-SKI): a prespecified interim analysis of a prospective, multicentre, non-randomised, trial. Lancet Oncol. 2018;19:747–57.
Rousselot P, Huguet F, Rea D, Legros L, Cayuela JM, Maarek O, et al. Imatinib mesylate discontinuation in patients with chronic myelogenous leukemia in complete molecular remission for more than 2 years. Blood. 2007;109:58–60.
Hochhaus A, Saussele S, Rosti G, Mahon FX, Janssen J, Hjorth-Hansen H, et al. Chronic myeloid leukaemia: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28:iv41–iv51.
Radich JP, Deininger M, Abboud CN, Altman JK, Berman E, Bhatia R, et al. Chronic myeloid leukemia, version 1.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16:1108–35.
Rea D, Ame S, Berger M, Cayuela JM, Charbonnier A, Coiteux V, et al. Discontinuation of tyrosine kinase inhibitors in chronic myeloid leukemia: recommendations for clinical practice from the French Chronic Myeloid Leukemia Study Group. Cancer. 2018;124:2956–63.
Mori S, Vagge E, le Coutre P, Abruzzese E, Martino B, Pungolino E, et al. Age and dPCR can predict relapse in CML patients who discontinued imatinib: the ISAV study. Am J Hematol. 2015;90:910–4.
Nicolini FE, Dulucq S, Boureau L, Cony-Makhoul P, Charbonnier A, Escoffre-Barbe M, et al. Evaluation of residual disease and TKI duration are predictive factors for molecular recurrence after stopping Imatinib first-line in chronic phase CML Patients. Clin Cancer Res. 2019;25:6606–13.
Tang M, Foo J, Gonen M, Guilhot J, Mahon FX, Michor F. Selection pressure exerted by imatinib therapy leads to disparate outcomes of imatinib discontinuation trials. Haematologica. 2012;97:1553–61.
Ross DM, Hughes TP, Melo JV. Do we have to kill the last CML cell? Leukemia. 2011;25:193–200.
Rea D, Henry G, Khaznadar Z, Etienne G, Guilhot F, Nicolini F, et al. Natural killer-cell counts are associated with molecular relapse-free survival after imatinib discontinuation in chronic myeloid leukemia: the IMMUNOSTIM study. Haematologica. 2017;102:1368–77.
Ohyashiki K, Katagiri S, Tauchi T, Ohyashiki JH, Maeda Y, Matsumura I, et al. Increased natural killer cells and decreased CD3(+)CD8(+)CD62L(+) T cells in CML patients who sustained complete molecular remission after discontinuation of imatinib. Br J Haematol. 2012;157:254–6.
Pagani IS, Dang P, Kommers IO, Goyne JM, Nicola M, Saunders VA, et al. BCR-ABL1 genomic DNA PCR response kinetics during first-line imatinib treatment of chronic myeloid leukemia. Haematologica. 2018;103:2026–32.
Pagani IS, Spinelli O, Mattarucchi E, Pirrone C, Pigni D, Amelotti E, et al. Genomic quantitative real-time PCR proves residual disease positivity in more than 30% samples with negative mRNA-based qRT-PCR in Chronic Myeloid Leukemia. Oncoscience. 2014;1:510–21.
Alikian M, Ellery P, Forbes M, Gerrard G, Kasperaviciute D, Sosinsky A, et al. Next-generation sequencing-assisted DNA-based digital PCR for a personalized approach to the detection and quantification of residual disease in chronic myeloid leukemia patients. J Mol Diagn. 2016;18:176–89.
Porta G, Pagani IS, Pirrone C. gDNA Q-PCR for clinical monitoring of CML. Cell Cycle. 2015;14:3659–60.
Ross DM, Branford S, Seymour JF, Schwarer AP, Arthur C, Bartley PA, et al. Patients with chronic myeloid leukemia who maintain a complete molecular response after stopping imatinib treatment have evidence of persistent leukemia by DNA PCR. Leukemia. 2010;24:1719–24.
Newman AM, Bratman SV, Stehr H, Lee LJ, Liu CL, Diehn M, et al. FACTERA: a practical method for the discovery of genomic rearrangements at breakpoint resolution. Bioinformatics. 2014;30:3390–3.
Bustin SA, Benes V, Garson JA, Hellemans J, Huggett J, Kubista M, et al. The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clin Chem. 2009;55:611–22.
Branford S, Hughes TP, Rudzki Z. Monitoring chronic myeloid leukaemia therapy by real-time quantitative PCR in blood is a reliable alternative to bone marrow cytogenetics. Br J Haematol. 1999;107:587–99.
Richards SJ, Morgan GJ, Hillmen P. Immunophenotypic analysis of B cells in PNH: insights into the generation of circulating naive and memory B cells. Blood. 2000;96:3522–8.
Clark RE, Polydoros F, Apperley JF, Milojkovic D, Pocock C, Smith G, et al. De-escalation of tyrosine kinase inhibitor dose in patients with chronic myeloid leukaemia with stable major molecular response (DESTINY): an interim analysis of a non-randomised, phase 2 trial. Lancet Haematol. 2017;4:e310–e316.
Bocchia M, Sicuranza A, Abruzzese E, Iurlo A, Sirianni S, Gozzini A, et al. Residual peripheral blood CD26(+) leukemic stem cells in chronic myeloid leukemia patients during TKI therapy and during treatment-free remission. Front Oncol. 2018;8:194.
Papalexandri A, Saloum R, Touloumenidou T, Papathanasiou M, Lalayanni C, Baldoumi E, et al. Blast crisis of CML after TKI discontinuation in a patient with previous stable deep molecular response. Is it safe to stop? HemaSphere. 2018;2:e157.
Takahashi N, Miura I, Saitoh K, Miura AB. Lineage involvement of stem cells bearing the philadelphia chromosome in chronic myeloid leukemia in the chronic phase as shown by a combination of fluorescence-activated cell sorting and fluorescence in situ hybridization. Blood. 1998;92:4758–63.
Jonas D, Lubbert M, Kawasaki ES, Henke M, Bross KJ, Mertelsmann R, et al. Clonal analysis of bcr-abl rearrangement in T lymphocytes from patients with chronic myelogenous leukemia. Blood. 1992;79:1017–23.
Ziegler-Heitbrock HW, Pechumer H, Petersmann I, Durieux JJ, Vita N, Labeta MO, et al. CD14 is expressed and functional in human B cells. Eur J Immunol. 1994;24:1937–40.
Acknowledgements
The authors are grateful to the patients who donated samples for this study, to the investigators and coordinators of the ALLG CML8 study, and to the staff of the South Australian Cancer Research Biobank. This study was funded by Project Grants #1138935 and #1051965 from the Australian National Health & Medical Research Council (NHMRC). SB and DLW receive fellowship support from the NHMRC (#1104425). DLW also receives fellowship support from the South Australian Cancer Council Beat Cancer Project. This study was undertaken with the financial support of Cancer Council SA’s Beat Cancer Project on behalf of its donors and the State Government through the Department of Health.
Author information
Authors and Affiliations
Contributions
ISP designed and performed experiments, analysed the data, and prepared the paper; PD, VAS, RG, SW, and JM performed experiments and reviewed the paper; NS and DTY contributed essential clinical data and reviewed the paper; LC and ZR assisted with the collection of samples and clinical data; CHK performed the analysis of the next generation sequencing data; JB, HA, and SB contributed RQ-PCR data and reviewed the paper; ASMY and DLW supervised research, and reviewed the paper. TPH and DMR designed the study, supervised research, and reviewed the paper.
Corresponding author
Ethics declarations
Conflict of interest
SB declares research funding from Novartis, advisory board participation for Qiagen, Novartis, and BMS, and honoraria from Qiagen, Novartis, BMS, and Cepheid. ASMY declares research funding from Novartis, BMS, and Celgene and honoraria from Novartis and BMS. DLW declares research funding and honoraria from BMS and honoraria from Amgen. TPH declares research funding and honoraria from Novartis and BMS, and advisory board participation for Novartis, BMS, and Incyte. DMR declares research funding from Novartis and Celgene, and honoraria from Novartis and BMS. The remaining authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pagani, I.S., Dang, P., Saunders, V.A. et al. Lineage of measurable residual disease in patients with chronic myeloid leukemia in treatment-free remission. Leukemia 34, 1052–1061 (2020). https://doi.org/10.1038/s41375-019-0647-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-019-0647-x
This article is cited by
-
What do atomic bomb survivors teach us about therapy-free remission in people with chronic myeloid leukaemia?
Leukemia (2024)
-
Tyrosine Kinase Inhibitor Discontinuation in Chronic Myeloid Leukemia: Strategies to Optimize Success and New Directions
Current Hematologic Malignancy Reports (2024)
-
The SNP rs460089 in the gene promoter of the drug transporter OCTN1 has prognostic value for treatment-free remission in chronic myeloid leukemia patients treated with imatinib
Leukemia (2024)
-
Development and validation of sensitive BCR::ABL1 fusion gene quantitation using next-generation sequencing
Cancer Cell International (2023)
-
European LeukemiaNet laboratory recommendations for the diagnosis and management of chronic myeloid leukemia
Leukemia (2023)