Abstract
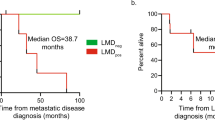
Central nervous system (CNS) involvement by cytospin is associated with increased risk of relapse in childhood acute lymphoblastic leukemia. We investigated if flow cytometric analysis of cerebrospinal fluid (CSF) at diagnosis improves the prediction of relapse. This prospective cohort study included patients (1.0–17.9 years) treated according to the Nordic Society of Pediatric Hematology and Oncology ALL2008 protocol. CSF flow cytometry samples were obtained at 17 centers, preserved with Transfix®, and analyzed at a central laboratory. One-hundred and seventy-one (25.4%) of 673 patients were positive by flow cytometry (CNSflow+). The 4-year cumulative incidence of relapse was higher for patients with cytospin positivity (CNScyto+) (17.1% vs. 7.5%), CNSflow+ (16.5% vs. 5.6%), and cytospin and/or flow positivity (CNScomb+) (16.7% vs. 5.1%). In Cox regression analysis stratified by immunophenotype and minimal residual disease day 29 and adjusted by sex, predictors of relapse were age (hazard ratio [HR] 1.1, 95% CI 1.1–1.2, P < 0.001), white blood cell count at diagnosis (HR 1.4, 95% CI 1.1–1.6, P < 0.001), and CNScomb+ (HR 2.2, 95% CI 1.0–4.7, P = 0.042). Flow cytometric analysis of CSF improves detection of CNS leukemia, distinguishes patients with high and low risk of relapse, and may improve future risk stratification and CNS-directed therapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Change history
08 April 2020
A Correction to this paper has been published: https://doi.org/10.1038/s41375-020-0821-1
References
Inaba H, Greaves M, Mullighan CG. Acute lymphoblastic leukaemia. Lancet. 2013;381:1943–55.
Schultz KR, Pullen DJ, Sather HN, Shuster JJ, Devidas M, Borowitz MJ, et al. Risk- and response-based classification of childhood B-precursor acute lymphoblastic leukemia: a combined analysis of prognostic markers from the Pediatric Oncology Group (POG) and Children’s Cancer Group (CCG). Blood. 2007;109:926–35.
Winick N, Devidas M, Chen S, Maloney K, Larsen E, Mattano L, et al. Impact of initial CSF findings on outcome among patients with national cancer institute standard- and high-risk B-cell acute lymphoblastic leukemia: a report from the Children’s Oncology Group. J Clin Oncol. 2017;35:2527–34.
Pui CH, Howard SC. Current management and challenges of malignant disease in the CNS in paediatric leukaemia. Lancet Oncol. 2008;9:257–68.
Krishnan S, Wade R, Moorman AV, Mitchell C, Kinsey SE, Eden TO, et al. Temporal changes in the incidence and pattern of central nervous system relapses in children with acute lymphoblastic leukaemia treated on four consecutive Medical Research Council trials, 1985-2001. Leukemia. 2010;24:450–9.
Hagedorn N, Acquaviva C, Fronkova E, von Stackelberg A, Barth A, zur Stadt U, et al. Submicroscopic bone marrow involvement in isolated extramedullary relapses in childhood acute lymphoblastic leukemia: a more precise definition of “isolated” and its possible clinical implications, a collaborative study of the Resistant Disease Committee of the International BFM study group. Blood. 2007;110:4022–9.
Buhrer C, Hartmann R, Fengler R, Dopfer R, Gadner H, Gerein V, et al. Superior prognosis in combined compared to isolated bone marrow relapses in salvage therapy of childhood acute lymphoblastic leukemia. Med Pediatr Oncol. 1993;21:470–6.
Tallen G, Ratei R, Mann G, Kaspers G, Niggli F, Karachunsky A, et al. Long-term outcome in children with relapsed acute lymphoblastic leukemia after time-point and site-of-relapse stratification and intensified short-course multidrug chemotherapy: results of trial ALL-REZ BFM 90. J Clin Oncol. 2010;28:2339–47.
Vora A, Andreano A, Pui CH, Hunger SP, Schrappe M, Moericke A, et al. Influence of cranial radiotherapy on outcome in children with acute lymphoblastic leukemia treated with contemporary therapy. J Clin Oncol. 2016;34:919–26.
Krull KR, Hardy KK, Kahalley LS, Schuitema I, Kesler SR. Neurocognitive outcomes and interventions in long-term survivors of childhood cancer. J Clin Oncol. 2018;36:2181–9.
Follin C, Erfurth EM. Long-term effect of cranial radiotherapy on pituitary-hypothalamus area in childhood acute lymphoblastic leukemia survivors. Curr Treat Options Oncol. 2016;17:50.
Chamberlain MC, Glantz M, Groves MD, Wilson WH. Diagnostic tools for neoplastic meningitis: detecting disease, identifying patient risk, and determining benefit of treatment. Semin Oncol. 2009;36:S35–45.
Burger B, Zimmermann M, Mann G, Kuhl J, Loning L, Riehm H, et al. Diagnostic cerebrospinal fluid examination in children with acute lymphoblastic leukemia: significance of low leukocyte counts with blasts or traumatic lumbar puncture. J Clin Oncol. 2003;21:184–8.
Levinsen M, Taskinen M, Abrahamsson J, Forestier E, Frandsen TL, Harila-Saari A, et al. Clinical features and early treatment response of central nervous system involvement in childhood acute lymphoblastic leukemia. Pediatr Blood Cancer. 2014;61:1416–21.
Glantz MJ, Cole BF, Glantz LK, Cobb J, Mills P, Lekos A, et al. Cerebrospinal fluid cytology in patients with cancer: minimizing false-negative results. Cancer. 1998;82:733–9.
de Graaf MT, van den Broek PD, Kraan J, Luitwieler RL, van den Bent MJ, Boonstra JG, et al. Addition of serum-containing medium to cerebrospinal fluid prevents cellular loss over time. J Neurol. 2011;258:1507–12.
Subira D, Castanon S, Roman A, Aceituno E, Jimenez-Garofano C, Jimenez A, et al. Flow cytometry and the study of central nervous disease in patients with acute leukaemia. Br J Haematol. 2001;112:381–4.
Martinez-Laperche C, Gomez-Garcia AM, Lassaletta A, Moscardo C, Vivanco JL, Molina J, et al. Detection of occult cerebrospinal fluid involvement during maintenance therapy identifies a group of children with acute lymphoblastic leukemia at high risk for relapse. Am J Hematol. 2013;88:359–64.
Ranta S, Nilsson F, Harila-Saari A, Saft L, Tani E, Soderhall S, et al. Detection of central nervous system involvement in childhood acute lymphoblastic leukemia by cytomorphology and flow cytometry of the cerebrospinal fluid. Pediatr Blood Cancer. 2015;62:951–6.
Levinsen M, Marquart HV, Groth-Pedersen L, Abrahamsson J, Albertsen BK, Andersen MK, et al. Leukemic blasts are present at low levels in spinal fluid in one-third of childhood acute lymphoblastic leukemia cases. Pediatr Blood Cancer. 2016;63:1935–42.
Toft N, Birgens H, Abrahamsson J, Griskevicius L, Hallbook H, Heyman M, et al. Results of NOPHO ALL2008 treatment for patients aged 1-45 years with acute lymphoblastic leukemia. Leukemia. 2018;32:606–15.
Berry DA, Zhou S, Higley H, Mukundan L, Fu S, Reaman GH, et al. Association of minimal residual disease with clinical outcome in pediatric and adult acute lymphoblastic leukemia: a meta-analysis. JAMA Oncol. 2017;3:e170580.
Gajjar A, Harrison PL, Sandlund JT, Rivera GK, Ribeiro RC, Rubnitz JE, et al. Traumatic lumbar puncture at diagnosis adversely affects outcome in childhood acute lymphoblastic leukemia. Blood. 2000;96:3381–4.
Dutch Childhood Oncology G, te Loo DM, Kamps WA, van der Does-van den Berg A, van Wering ER, de Graaf SS. Prognostic significance of blasts in the cerebrospinal fluid without pleiocytosis or a traumatic lumbar puncture in children with acute lymphoblastic leukemia: experience of the Dutch Childhood Oncology Group. J Clin Oncol. 2006;24:2332–6.
Pui CH, Campana D, Pei D, Bowman WP, Sandlund JT, Kaste SC, et al. Treating childhood acute lymphoblastic leukemia without cranial irradiation. N Engl J Med. 2009;360:2730–41.
Price RA, Johnson WW. The central nervous system in childhood leukemia. I. The arachnoid. Cancer. 1973;31:520–33.
Williams MT, Yousafzai YM, Elder A, Rehe K, Bomken S, Frishman-Levy L, et al. The ability to cross the blood-cerebrospinal fluid barrier is a generic property of acute lymphoblastic leukemia blasts. Blood. 2016;127:1998–2006.
Munch V, Trentin L, Herzig J, Demir S, Seyfried F, Kraus JM, et al. Central nervous system involvement in acute lymphoblastic leukemia is mediated by vascular endothelial growth factor. Blood. 2017;130:643–54.
Galati D, Di Noto R, Del Vecchio L. Diagnostic strategies to investigate cerebrospinal fluid involvement in haematological malignancies. Leuk Res. 2013;37:231–7.
Acknowledgements
We thank all Nordic and Baltic pediatric oncology centers for providing clinical data and CSF samples for flow cytometric analysis. We are grateful to the staff at the Laboratory of Pediatric Oncology and the Department of Immunology, Rigshospitalet, for their help with sample analysis and data registration. The study was funded by the Danish Childhood Cancer Foundation, Nordic Cancer Union, Rigshospitalet, Swedish Childhood Cancer Foundation, Danish Cancer Research Foundation, Cancer Research Foundation of Elna and Jørgen Fagerholt Pedersen, Axel Muusfeldt’s Foundation, Anders Hasselbalch’s Fight Leukemia Foundation, Otto Christensen’s Foundation, Memorial Foundation of Merchant M. Brogaard and Wife, Research Foundation of Hasselbalch and Lykkegaard Andersen, Memorial Foundation of Eva and Henry Frænkel, Dagmar Marshall’s Foundation, King Christian the Tenth Foundation, Memorial Trust Foundation of Thora and Viggo Grove.
Author information
Authors and Affiliations
Consortia
Contributions
KS, HVM and ML designed the study. All authors contributed to sample collection. MThastrup and ML coordinated the study. MThastrup, HVM, and KG analyzed the data. MThastrup, HVM, KG and KS interpreted the data and wrote the first draft of the manuscript. All authors critically reviewed the manuscript and approved the final draft for submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thastrup, M., Marquart, H.V., Levinsen, M. et al. Flow cytometric detection of leukemic blasts in cerebrospinal fluid predicts risk of relapse in childhood acute lymphoblastic leukemia: a Nordic Society of Pediatric Hematology and Oncology study. Leukemia 34, 336–346 (2020). https://doi.org/10.1038/s41375-019-0570-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-019-0570-1
This article is cited by
-
Mass spectrometry-based proteomics of cerebrospinal fluid in pediatric central nervous system malignancies: a systematic review with meta-analysis of individual patient data
Fluids and Barriers of the CNS (2024)
-
Acute Lymphoblastic Leukemia with Central Nervous System Involvement—Challenges in Management
Indian Journal of Pediatrics (2024)
-
Central nervous system involvement in childhood acute lymphoblastic leukemia: challenges and solutions
Leukemia (2022)
-
Flowcytometric evaluation of cerebrospinal fluid in childhood ALL identifies CNS involvement better then conventional cytomorphology
Leukemia (2021)
-
Involvement of the central nervous system in acute lymphoblastic leukemia: opinions on molecular mechanisms and clinical implications based on recent data
Cancer and Metastasis Reviews (2020)