Abstract
Carfilzomib, a selective proteasome inhibitor (PI), is approved for the treatment of patients with relapsed or refractory multiple myeloma (MM). Combination regimens incorporating a PI and immunomodulatory drug (IMiD) have been associated with deep responses and extended survival in patients with newly diagnosed MM (NDMM). Carfilzomib-based combinations with immunomodulators are being extensively studied in the frontline setting. The objective of this review was to describe efficacy and safety data for carfilzomib-based, PI/immunomodulatory combinations in NDMM. Information sources were articles indexed in PubMed and abstracts from key hematology/oncology congresses published between January 2012 and December 2018. PubMed and congresses were searched for prospective clinical studies assessing the combination of carfilzomib with an IMiD for NDMM treatment. Retrospective and preclinical reports, case reports/series, reviews, and clinical studies not evaluating carfilzomib–immunomodulator combinations in NDMM were excluded based on review of titles and abstracts. A total of nine articles and 72 abstracts were deemed relevant and included in the review. A total of six distinct carfilzomib-based, PI/immunomodulator combination regimens have been evaluated in 12 clinical trials. Overall, treatment with these regimens has resulted in deep responses, including high rates of negativity for minimal residual disease. These deep responses have translated to long progression-free survival and overall survival rates. Efficacy results for these regimens have generally been consistent across subgroups defined by age, transplant eligibility, and cytogenetic risk. The safety profile of carfilzomib in NDMM is consistent with that observed in the relapsed-refractory MM setting. Clinical studies have found that carfilzomib-based combinations with immunomodulators are highly active with a favorable safety profile in NDMM. The carfilzomib, lenalidomide, and dexamethasone (KRd) drug backbone is a promising foundation for treatment strategies aimed at achieving long-term, deep responses (functional cures) in the frontline setting. Several ongoing studies are evaluating KRd, with or without anti-CD38 monoclonal antibodies.
Similar content being viewed by others
Introduction
There were 138,509 new multiple myeloma (MM) cases worldwide in 2016; in the United States, 30,770 projected cases occurred in 2018 [1, 2]. The global incidence has increased sharply in recent decades, in part due to aging populations [1].
For newly diagnosed MM (NDMM) patients, the introduction of proteasome inhibitors (PIs) and immunomodulatory drugs (IMiDs) has improved treatment responses versus older therapies [3]. Several modern combination regimens incorporating a PI–IMiD backbone are considered recommended frontline regimens by the National Comprehensive Care Network and the European Society for Medical Oncology. These clinical regimens build off preclinical evidence showing that PIs and IMiDs have synergistic activity mediated by enhanced proteasome targeting, caspase activation, NF-κB inhibitory activity, and downregulation of CRBN/IRF4/MYC signaling and MCL1 [4,5,6]. These modern combination regimens have been associated with deep responses and improved progression-free survival (PFS) and overall survival (OS) [7].
Carfilzomib is a selective, second-generation PI that irreversibly binds the proteasome [8, 9]. This agent exerts its antimyeloma activity through several actions including unfolded protein stress response induction [10], NF-κB prosurvival activity downregulation [11], modification of bone turnover and the bone marrow microenvironment leading to increased bone strength and compromised microenvironmental support for myeloma cells [12,13,14], and induction of immunogenic myeloma cell death through increased natural kill cell-mediated MM-cell lysis and enhanced antigen presentation (Fig. 1) [12,13,14,15,16,17]. Carfilzomib has a structure (tetrapeptide epoxyketone) differentiated from the first-generation PI bortezomib (dipeptide boronate) [8]. Preclinical studies demonstrated that carfilzomib overcomes bortezomib resistance [9] and that it does not reduce neurite length or inhibit nonproteasomal targets like HtrA2/Omi, effects which were observed with bortezomib [8]. Carfilzomib elicits deeper and more sustained proteasome inhibition versus bortezomib [18].
In MM clinical trials, carfilzomib-based regimens demonstrated robust efficacy and carfilzomib showed single-agent activity; it is approved for treatment of relapsed or refractory MM (RRMM). The approvals of carfilzomib-based combination therapy were based on three randomized phase 3 relapsed and/or refractory MM studies: ASPIRE, ENDEAVOR, and A.R.R.O.W. In ASPIRE and ENDEAVOR, treatment with carfilzomib-based regimens (ASPIRE: carfilzomib–lenalidomide–dexamethasone [KRd]; ENDEAVOR: carfilzomib–dexamethasone [Kd]) resulted in superior PFS, OS, depth of response, and health-related quality of life (QoL) versus recent standards of care in patients with RRMM [19,20,21,22,23,24]. In A.R.R.O.W., treatment with a more convenient once-weekly Kd regimen (carfilzomib 70 mg/m2) improved PFS and health-related QoL compared with twice-weekly Kd (carfilzomib 27 mg/m2) in patients with relapsed and refractory MM [25, 26].
Given the established efficacy of carfilzomib in RRMM and the frontline potency of regimens incorporating a PI–IMiD backbone, recent NDMM clinical trials have evaluated combination regimens using carfilzomib-based, PI–IMiD combinations. This systematic review summarizes the efficacy and safety of these regimens for NDMM.
Methods
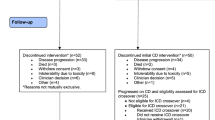
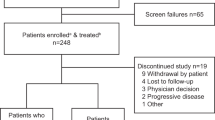
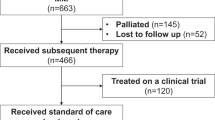
Studies were collected from a search of PubMed and abstracts from key hematology/oncology congresses published between January 2012 and December 2018. The following congresses were systemically searched between January 2012 and December 2018: American Society of Hematology Annual Meeting, American Society of Clinical Oncology Annual Meeting, European Hematology Association Annual Congress, Blood and Marrow Transplantation Tandem Meeting, European Society for Medical Oncology Annual Congress, International Myeloma Workshop, and the Lymphoma & Myeloma Congress. PubMed and congresses were searched for prospective clinical studies that assessed the combination of carfilzomib with an IMiD in NDMM patients. Specific search terms included “carfilzomib,” “Kyprolis,” “MM,” “thalidomide,” “lenalidomide,” “pomalidomide,” “newly diagnosed,” “transplant-eligible,” and “transplant-ineligible.” Three hundred and eighty-four articles were identified and were screened for relevancy to this review based on titles and abstracts. Retrospective and preclinical reports, case reports/series, reviews, and clinical studies not evaluating frontline carfilzomib-immunomodulator combinations were excluded. Nine articles were deemed relevant for inclusion (Fig. 2a). Six hundred and fifty-five abstracts were identified, 72 of which were deemed relevant (Fig. 2b).
Results
Activity of carfilzomib–IMiD combinations in NDMM
To date, six distinct carfilzomib–IMiD combinations have been assessed in 12 NDMM clinical trials [27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51]. Key study information and efficacy data (including minimal residual disease [MRD] and MRD limit of detection) are summarized in Tables 1 and 2 and described below. All studies assessed twice-weekly carfilzomib unless stated otherwise.
Carfilzomib–lenalidomide–dexamethasone
In NDMM, KRd has been examined in six distinct clinical studies. In 2012, the MM Research Consortium (MMRC) reported findings from a phase 1/2 study of KRd (n = 53; transplant-eligible or -ineligible) [27]. Patients received KRd induction until disease progression or unacceptable toxicity for up to eight cycles (carfilzomib 20, 27, or 36 mg/m2 in phase 1; 36 mg/m2 in phase 2). Transplant-eligible patients who achieved ≥partial response (PR) after cycle 4 had stem cell collection (SCC) and the option to proceed with autologous stem cell transplantation (ASCT), but per protocol, were to resume KRd after SCC. After eight cycles, patients received KRd maintenance for a maximum of 24 total KRd cycles. After four cycles, 38% of patients achieved ≥near complete response (nCR; defined as no detectable M protein on electrophoresis independent of immunofixation status, stable bone disease, and normal serum calcium concentration; phase 2 primary endpoint). At a median follow-up of 13 months (median treatment duration, 12 cycles), overall response rate (ORR) was 98% including 42% with a stringent complete response (sCR). Approximately two-thirds of patients who completed ≥8 cycles achieved sCR. Among patients with a complete response (CR/suspected CR), the MRD-negativity rate was 91% (multiparametric flow cytometry [MFC]). Notably, deep responses were obtained with KRd alone as the seven patients who proceeded to ASCT were censored for best response at the time of proceeding to transplant because they did not resume KRd. PFS rates were 97% and 92% at 12 and 24 months, respectively. There were no major efficacy differences between standard- and high-risk cytogenetics subgroups, although numbers were limited (standard risk, n = 34; high risk, n = 17). In a subgroup analysis of the MMRC study evaluating elderly patients (age ≥65 years; n = 23), the ≥very good PR (VGPR) rate was 91%; the sCR rate was 65% [28]. Updated MMRC study results (median follow-up, 4 years) showed that extended KRd treatment increased sCR rates from 42 to 51% [29]. The 2- and 4-year PFS rates were 92% and 69%, respectively [29].
A phase 2 study National Institutes of Health (NIH) Clinical Center study evaluated KRd in transplant-eligible or -ineligible patients with NDMM (n = 45) or smoldering MM (SMM) at high risk of progression (n = 12) [30]. Patients received eight KRd cycles then lenalidomide maintenance. Carfilzomib (36 mg/m2) was administered for the first 3 weeks of a 4-week cycle. Deep responses were observed, with 62% (NDMM) and 100% (SMM) of patients achieving ≥nCR [30]. The 1-year PFS rate in NDMM was 95% and all NDMM patients remained alive [30]. Thirty-four of 45 enrolled NDMM patients (76%) achieved MRD-negative status (MFC). MRD-negativite ≥nCR rates by MFC were 100% (NDMM) and 92% (SMM); MRD-negativity rates by next-generation sequencing (NGS) were 67% and 75%, respectively [30]. MRD negativity was observed In hematopoietic progenitor cell grafts from 29/30 patients [31]. In a 5-year follow-up of the study (NDMM cohort), the MRD-negative CR rate was 62%; median time to progression was 67.3 months and the 6-year OS rate was 84% [32]. Depth of response and PFS were consistent regardless of age (≥65 vs <65 years) or cytogenetic risk [30, 32]. The NIH Clinical Center study was recently reopened for enrollment with expanded sample size. Based on results from the MMRC and NIH Clinical Center studies, KRd is a treatment option for transplant-eligible and -ineligible patients according to the National Comprehensive Care Network guidelines.
Although extended KRd treatment without transplant in the MMRC study showed strong clinical benefit, some patients experienced progression [27]. Therefore, a second phase 2 MMRC study added ASCT to KRd to evaluate if further improvement of outcomes was possible [33, 34]. In this study (n = 76), patients received four 28-day cycles of KRd induction followed by ASCT. Following ASCT, patients received four cycles of KRd consolidation and then KRd maintenance for 10 cycles. Carfilzomib was administered at 20/36 mg/m2. Response rates were 91% ≥VGPR, 78% ≥CR, and 75% sCR (primary endpoint) [33, 34]. Postconsolidation MRD-negative ≥CR rates were 67% (NGS) and 95% (MFC) [34]. High rates of MRD negativity after consolidation were found to be sustained through to cycle 18 and after lenalidomide maintenance; this sustained MRD negativity (cycle 18) correlated with 3-year PFS and OS rates [34]. The 3-year PFS and OS rates for sustained MRD negativity patients by NGS were 94 and 100%, which were higher than those in the overall population (PFS, 86%; OS, 93%) [34]. Similar findings were observed in patients with high-risk disease (n = 27) [34].
The Intergroupe Francophone du Myelome also conducted a phase 2 study evaluating KRd with ASCT [35]. Patients received four KRd induction cycles, ASCT, four KRd consolidation cycles, and 1-year lenalidomide maintenance. Carfilzomib (20/36 mg/m2) was given for 3 weeks of each 4-week cycle. Postconsolidation ORR was 89%, including 85% ≥VGPR and 61% ≥CR. MRD-negativity rate was 70% by flow cytometry. Median PFS was not reached; the 2-year PFS rate was 91%.
The high rates of MRD negativity observed with KRd and integration of MRD assessments into standardized response criteria [3] provided rationale for an ongoing phase 1/2 study that is the first to evaluate MRD status as a guide for KRd treatment duration in NDMM patients [36]. During phase 1, patients receive carfilzomib (45 or 56 mg/m2) with lenalidomide–dexamethasone to determine the maximum tolerated dose (MTD) of carfilzomib. Patients who achieve MRD negativity after any cycle receive two additional KRd cycles before treatment discontinuation, whereas MRD-positive patients continue therapy for ≤12 cycles, or until disease progression or unacceptable toxicity. The phase 2 primary endpoint is MRD negativity at the MTD. Phase 1 results established the carfilzomib MTD at 56 mg/m2. The phase 2 portion of the study is ongoing.
The demonstrated activity of KRd and the promising efficacy of carfilzomib–cyclophosphamide–dexamethasone (KCd) [37] in NDMM patients provided the rationale for the randomized FORTE trial, where NDMM patients were randomized 1:1:1 to four 28-day KCd cycles followed by ASCT and four KCd consolidation cycles; or four 28-day KRd cycles followed by ASCT and four KRd consolidation cycles; or twelve KRd cycles [38]. Patients who complete consolidation are randomized to lenalidomide versus carfilzomib–lenalidomide maintenance. Carfilzomib was administered at 20/36 mg/m2. A total of 474 patients were randomized (KRd + ASCT, n = 158; KCd+ASCT, n = 159; KRd 12 cycles, n = 157). Premaintenance, ≥VGPR and sCR rates were higher in the KRd arms than in the KCd arm (KRd + ASCT, 89 and 44%; KCd + ASCT, 76 and 32%; KRd 12 cycles, 87 and 43%). MRD-negativity rates were also higher with KRd versus KCd (KRd + ASCT, 58%; KCd + ASCT, 42%; KRd 12 cycles, 54%). These benefits for KRd versus KCd were consistent, regardless of the presence of high-risk disease. The sCR rates in the KRd arms also compare favorably with the postconsolidation sCR rate (28.9%) reported for the daratumumab–bortezomib–thalidomide–dexamethasone arm in the phase 3 CASSIOPEIA study of this combination in transplant-eligible NDMM [52].
Inspired by the NIH Clinical Center study, the ongoing phase 2 GEM-CESAR trial is assessing KRd induction and consolidation with ASCT for SMM at high risk of progression. Preliminary post-ASCT efficacy results (69% ≥CR; 58% MRD negative) demonstrate the promise of this approach [39]. An EMN-MSKCC randomized phase 2 study comparing KRd versus Rd in high-risk SMM has recently started.
Overall, the safety profile of KRd in NDMM patients has been consistent with the profile observed in the ASPIRE study. In the FORTE trial, rates of treatment discontinuation due to adverse events (AEs) and fatal AEs were 8 and 1%, whereas in ASPIRE these rates were 15% and 7%, respectively (see Tables 3 and 4 for additional details) [24, 38, 40].
Carfilzomib–thalidomide–dexamethasone
CARTHADEX was a phase 1/2 trial that evaluated carfilzomib–thalidomide–dexamethasone (KTd) as induction and consolidation therapy in transplant-eligible NDMM patients. During KTd induction, patients received four cycles of carfilzomib 20/27, 20/36, 20/45, or 20/56 mg/m2. In the overall population (N = 91), KTd induction resulted in an ORR of 90%, including a CR in 25% of patients and a ≥VGPR (primary endpoint) in 68% of patients [41]. Response rates improved with transplant and KTd consolidation (Table 2). After consolidation, patients with standard- and high-risk disease showed no difference in ≥VGPR rates and had similar CR rates. At a median follow-up of 23 months, the median PFS was not reached and the 3-year PFS rate was 72%. A subsequent update of the CARTHADEX trial assessed the impact of prolonged KTd induction therapy (eight cycles) at carfilzomib 56 mg/m2 on depth of response [42]. Patients treated with prolonged KTd induction (n = 26) had higher ≥VGPR and ≥CR rates at end of induction compared with those treated with four KTd induction cycles at 56 mg/m2 (n = 20). However, depth of response between the two groups was noted to be similar after completion of ASCT and consolidation [42]. Another update of the CARTHADEX trial found that postconsolidation sCR and VGPR rates were numerically higher for the 36–56 versus 27 mg/m2 carfilzomib dose levels, but that PFS/OS were similar between these doses [43].
Carfilzomib–cyclophosphamide–thalidomide–dexamethasone
The phase 1/2 CYKLONE trial (N = 64) examined a four-drug regimen termed CYKLONE (carfilzomib–cyclophosphamide–thalidomide–dexamethasone) for the treatment of transplant-eligible NDMM patients [44]. The MTD of carfilzomib in CYKLONE was 20/36 mg/m2 (phase 1 primary endpoint). The ORR across all treatment cycles and dose levels was 91%. At the MTD, the ≥VGPR rate after four cycles was 59% (phase 2 primary endpoint).
The safety of carfilzomib–thalidomide combinations (KTd and CYKLONE) was consistent with previously reported safety of both agents. Lack of overlapping toxicities (especially neuropathy) between these two agents allowed a favorable safety profile for these regimens.
Carfilzomib–clarithromycin–lenalidomide–dexamethasone
Combination treatment with the antibiotic clarithromycin plus a PI has been found preclinically to induce synergistic cytotoxicity [45, 46]. The phase 2 Car-BiRD study (N = 72) of carfilzomib–clarithromycin–lenalidomide–dexamethasone (Car-BiRD) evaluated carfilzomib as part of a sequential treatment strategy: Kd induction (until maximal response) followed by BiRD consolidation and lenalidomide maintenance for transplant-eligible or -ineligible NDMM patients [47]. Carfilzomib (30-min IV infusion) was given for the first 3 weeks of each 4-week cycle at a dose of 20/45 mg/m2 (first 26 patients) or 20/56 mg/m2 (thereafter). Kd induction resulted in an ORR of 91%, ≥VGPR rate of 71%, and a ≥CR rate of 13%. Following BiRD consolidation, ORR, ≥VGPR, and ≥CR rates improved to 100%, 95%, and 28%, respectively. Lenalidomide maintenance further improved depth of response in 19% of patients.
Carfilzomib–cyclophosphamide–lenalidomide–dexamethasone
In the phase 3 UK NCRI Myeloma XI trial, transplant-eligible patients were randomized to the upfront PI-based quadruplet induction regimen of carfilzomib–cyclophosphamide–lenalidomide–dexamethasone (KCRd), or triplet induction therapy (cyclophosphamide–lenalidomide–dexamethasone [CRd] or cyclophosphamide–thalidomide–dexamethasone [CTd]) [48]. Patients in the triplet induction arms could have received a second induction with bortezomib–cyclophosphamide–dexamethasone (VCd) before ASCT depending on post first induction maximum response (≥VGPR, no second induction; PR or minor response, randomized to VCd or nothing; stable or progressive disease, VCd as second induction). Carfilzomib 20/36 mg/m2 was administered twice weekly for the first 3 weeks of each 4-week cycle. A total of 1056 patients underwent induction randomization (CTd, n = 265; CRd, n = 265; KCRd, n = 526). Deeper responses with carfilzomib-based quadruplet versus IMiD-based triplet treatment were observed at the end of first induction: the ≥VGPR rate at end of initial induction was 82.3% for KCRd versus 52.8 and 64.9% for CTd and CRd, respectively. This difference in depth of response was sustained until ≥100 days post-ASCT.
The quadruplet combination was well tolerated in this large phase 3 trial [48]. Grade ≥3 neutropenia occurred in 16% of KCRd patients, compared with 13% for CTd and 22% for CRd. Grade ≥2 sensory neuropathy rates were lower in the KCRd and CRd arms compared with the CTd arm (~2% vs ~10%). The incidences of any-grade cardiac failure and hypertension in the KCRd arm were both <2%.
Carfilzomib–lenalidomide–dexamethasone plus daratumumab
The phase 1b MMY1001 study evaluated KRd-daratumumab in NDMM patients [49, 50]. Patients were treated with this combination for ≤ 13 treatment cycles or until discontinuation for ASCT. Carfilzomib (20/70 mg/m2) was administered once weekly. This combination (n = 21) resulted in an ORR of 100% with 91 and 57% of patients achieving ≥VGPR and ≥CR, respectively. The 1-year PFS rate was 95%.
An ongoing phase 2 trial is evaluating MRD using blood and bone marrow-based assays after KRd-daratumumab treatment for NDMM. Preliminary results showed the feasibility of longitudinal MRD tracking in three patients who completed the MRD assays [51].
The phase 2 ASCENT trial (NCT03289299) is assessing the feasibility of KRd-daratumumab induction for high-risk SMM.
Safety of carfilzomib–IMiD combinations in NDMM
The safety profile of carfilzomib has been well established in RRMM, where it has shown to have manageable AEs [53] and a favorable benefit-risk profile given the observed PFS/OS advantage. In this setting, the most common grade 3/4 AEs associated with single-agent carfilzomib were primarily hematologic [54]. Cardiovascular events have also been associated with carfilzomib, with hypertension (mainly grades 1 and 2) being the most common type. In a pooled analysis of phases 1–3 RRMM clinical studies (n = 2044 carfilzomib-exposed patients), any-grade and grade ≥3 hypertension rates were 18.5% and 5.9%, respectively, and any-grade and grade ≥3 cardiac failure rates were 6.7% and 4.4%, respectively [55]. Carfilzomib-associated cardiovascular events have been found to be generally reversible and manageable, as reflected by relatively low carfilzomib discontinuation rates across studies [55,56,57]. Furthermore, the efficacy benefit of carfilzomib in terms of reduction in the risk of progression/death has been found to outweigh the risks observed with carfilzomib (including cardiac failure or hypertension) among RRMM patients [55].
Carfilzomib has been associated with low rates of peripheral neuropathy (PN) in RRMM, an AE associated with bortezomib that may impair QoL and limit treatment duration [58]. The low rate of PN with carfilzomib is consistent with preclinical results showing that in contrast to bortezomib, carfilzomib has minimal activity against nonproteasomal proteases, including the stress-induced, prosurvival protease HtrA2/Omi [8]. This selectivity may explain the difference in PN incidence between the carfilzomib and bortezomib arms in ENDEAVOR [19]. In ASPIRE, addition of carfilzomib to Rd did not increase PN rates [24].
The safety profile of carfilzomib–IMiD combination therapy in NDMM patients has been consistent with the known safety profile of carfilzomib. Below, we summarize the above AEs of interest observed in the large, randomized NDMM studies (FORTE and Myeloma XI). General safety and AEs of interest for all NDMM studies are shown in Tables 3 and 4.
Hematologic adverse events
Hematologic events were the most common AEs observed in frontline clinical trials of carfilzomib–IMiD combinations (Table 4). The largest datasets come from the FORTE and Myeloma XI trials. In the FORTE trial, 18–22% of KRd patients had ≥1 grade ≥3 or serious hematologic AE [38]. Hematologic AE rates were comparable for KRd and KCd (18–22% vs 17%). In the KCRd arm of the Myeloma XI trial, rates of grade ≥3 neutropenia and thrombocytopenia were 16.4%, and 8.4%, respectively [48].
Peripheral neuropathy
Consistent with findings in RRMM, carfilzomib-based combination therapy has been associated with a low incidence of grade ≥2 PN in NDMM and a low rate of carfilzomib discontinuation or dose reductions due to PN (Table 4). In the KCRd arm of the Myeloma XI trial, grade ≥2 motor and sensory neuropathy rates were ~3% each [48]. PN rates have not been reported for the FORTE trial.
Cardiovascular events
Cardiovascular events have been reported with carfilzomib–IMiD combinations in the frontline setting (Table 4). In the FORTE trial, the rate of grade 3/4 or serious cardiac events was 2–3% in the KRd arms and 3% in the KCd arm [38]. Hypertension (grade 3/4, or serious in severity) was reported in 8% of patients who received 12 KRd cycles and in 3% patients who received KRd or KCd with ASCT [38]. In the KCRd versus CRd versus CTd arms of the phase 3 Myeloma XI study, any-grade arrhythmia, heart failure, and hypertension were reported in approximately 2.3% versus 1% versus 1.5%, 1% versus 0% versus 0%, and <1% versus <1% versus <1% of patients [48].
Although cardiovascular events have been observed with carfilzomib, they appear to be manageable and reversible in the majority of cases [56]. Importantly, grade ≥3 heart failure rates are relatively low considering carfilzomib efficacy. Clinical experience with carfilzomib has aided development of strategies for managing and mitigating cardiovascular events [56, 57]; clinical guidelines have been developed in collaboration with cardiologists to minimize cardiotoxicity with carfilzomib treatment [59].
Conclusions
Carfilzomib-based, PI–IMiD combination therapies have been shown to be highly efficacious with a favorable safety profile in NDMM, as evidenced by the data from several studies (single-arm and randomized) reviewed above. These regimens elicit deep and durable responses, including MRD negativity, which have translated to high PFS and OS rates. Furthermore, a consistent benefit for these regimens has been observed across patient segments, including in both transplant-eligible and -ineligible patients, across age subgroups, and regardless of cytogenetic risk. To date, results have been reported from only one randomized phase 3 study of carfilzomib-based IMID combination therapy in NDMM, and there are currently no phase 3 data for how these therapies directly compare with the most recent frontline standards of care. Future data from such studies will be important for evaluating the role of carfilzomib-based, PI–IMiD combination therapy in NDMM.
Bortezomib-based, PI–IMiD triplet combinations are considered standards of care in the frontline setting. For example, VRd is considered a preferred regimen by the NCCN for transplant-eligible and -ineligible patients based on data showing that this regimen improved PFS and OS compared with Rd. Despite the absence of controlled and randomized trials, carfilzomib-based, PI–IMiD combinations may offer several advantages relative to this standard of care. For some patients, PN associated with bortezomib may interrupt treatment, resulting in suboptimal response and QoL. These patients may benefit from a carfilzomib-based PI–IMiD regimen. Although there are currently no head-to-head data of carfilzomib- versus bortezomib-based, PI–IMiD therapy in NDMM, KRd (without or without ASCT) is one of the most active frontline regimens observed in NDMM studies [27,28,29,30,31,32,33,34,35,36, 38,39,40, 60]. Preliminary data from the observational CoMMpass study (NCT01454297) suggest that improved response rates and longer event-free survival are associated with KRd versus VRd in NDMM [61], while other preliminary data from CoMMpass and the Flatiron observational study suggest longer treatment duration with VRd [62]. However, these findings need to be validated in a prospective manner. The ongoing, randomized phase 3 ENDURANCE study (NCT01863550; N = 1000+), which is evaluating KRd versus VRd, will provide important head-to-head data regarding the benefit-risk profiles of carfilzomib- versus bortezomib-based PI–IMiD therapy in NDMM, with the limitation of capping carfilzomib treatment duration to nine cycles.
Carfilzomib has been associated with manageable and reversible cardiovascular events in RRMM, and these events merit monitoring in NDMM. In a meta-analysis of NDMM and RRMM patients (N = 2594), any-grade and grade ≥3 congestive heart failure rates were 4.1% and 2.5%, respectively [63].
The introduction of new antimyeloma agents has significantly improved the outlook of MM patients; however, MM remains an incurable disease. To achieve long-term remissions or even functional cure for NDMM patients, the most potent agents need to be used upfront. Based on favorable clinical outcomes of carfilzomib therapies in the relapsed setting, we believe that a carfilzomib–IMiD combination will also benefit NDMM patients. Ongoing frontline studies are evaluating the impact of adding new drugs with novel mechanisms, such as monoclonal antibodies, to the carfilzomib–IMiD combination to achieve functional cures in MM.
References
Cowan AJ, Allen C, Barac A, Basaleem H, Bensenor I, Curado MP, et al. Global burden of multiple myeloma: a systematic analysis for the global burden of disease study 2016. JAMA Oncol. 2018;4:1221–7.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30.
Kumar S, Paiva B, Anderson KC, Durie B, Landgren O, Moreau P, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17:e328–e346.
Chauhan D, Tian Z, Zhou B, Kuhn D, Orlowski R, Raje N, et al. In vitro and in vivo selective antitumor activity of a novel orally bioavailable proteasome inhibitor MLN9708 against multiple myeloma cells. Clin Cancer Res. 2011;17:5311–21.
Das DS, Ray A, Song Y, Richardson P, Trikha M, Chauhan D, et al. Synergistic anti-myeloma activity of the proteasome inhibitor marizomib and the IMiD immunomodulatory drug pomalidomide. Br J Haematol. 2015;171:798–812.
Mitsiades N, Mitsiades CS, Poulaki V, Chauhan D, Richardson PG, Hideshima T, et al. Apoptotic signaling induced by immunomodulatory thalidomide analogs in human multiple myeloma cells: therapeutic implications. Blood. 2002;99:4525–30.
Landgren O, Iskander K. Modern multiple myeloma therapy: deep, sustained treatment response and good clinical outcomes. J Intern Med. 2017;281:365–82.
Arastu-Kapur S, Anderl JL, Kraus M, Parlati F, Shenk KD, Lee SJ, et al. Nonproteasomal targets of the proteasome inhibitors bortezomib and carfilzomib: a link to clinical adverse events. Clin Cancer Res. 2011;17:2734–43.
Kuhn DJ, Chen Q, Voorhees PM, Strader JS, Shenk KD, Sun CM, et al. Potent activity of carfilzomib, a novel, irreversible inhibitor of the ubiquitin-proteasome pathway, against preclinical models of multiple myeloma. Blood. 2007;110:3281–90.
Obeng EA, Carlson LM, Gutman DM, Harrington WJ Jr., Lee KP, Boise LH. Proteasome inhibitors induce a terminal unfolded protein response in multiple myeloma cells. Blood. 2006;107:4907–16.
Hideshima T, Chauhan D, Richardson P, Mitsiades C, Mitsiades N, Hayashi T, et al. NF-kappa B as a therapeutic target in multiple myeloma. J Biol Chem. 2002;277:16639–47.
Chen Y, Usmani SZ, Hu B, Papanikolau X, Heuck C, Epstein J, et al. Carfilzomib induces differentiation of mesenchymal stromal cells toward osteoblast via activation of β-catenin/TCF signaling. Blood. 2012;120:4008–4008.
Hurchla MA, Garcia-Gomez A, Hornick MC, Ocio EM, Li A, Blanco JF, et al. The epoxyketone-based proteasome inhibitors carfilzomib and orally bioavailable oprozomib have anti-resorptive and bone-anabolic activity in addition to anti-myeloma effects. Leukemia. 2013;27:430–40.
Suvannasankha A, Abonour R, Farag S, Silbermann RW, Wongsaengsak S, Cangany MH, et al. Phase 2 study of carfilzomib and bone metabolism in patients with relapsed multiple myeloma. Blood. 2017;130:1826.
Kashiwazaki S, Kobori M, Matsushita M, Hattori Y. Immunogenic cell death against multiple myeloma. Presented at the 15th Annual Meeting of Japan Research Association for Immunotherapeutics in Tokyo. 2018.
Yang G, Gao M, Zhang Y, Kong Y, Gao L, Tao Y, et al. Carfilzomib enhances natural killer cell-mediated lysis of myeloma linked with decreasing expression of HLA class I. Oncotarget. 2015;6:26982–94.
Perel G, Bliss J, Thomas CM. Carfilzomib (Kyprolis): a novel proteasome inhibitor for relapsed and/or refractory multiple myeloma. P T. 2016;41:303–7.
Ludwig H, Spencer A, Kovacsovics T, Gabrail NY, Minuk L, Kimball AS, et al. Comparison of proteasome inhibition activity between carfilzomib and bortezomib in the phase 3 endeavor study. Blood 2017;130:3125.
Dimopoulos MA, Goldschmidt H, Niesvizky R, Joshua D, Chng WJ, Oriol A, et al. Carfilzomib or bortezomib in relapsed or refractory multiple myeloma (ENDEAVOR): an interim overall survival analysis of an open-label, randomised, phase 3 trial. Lancet Oncol. 2017;18:1327–37.
Dimopoulos MA, Moreau P, Palumbo A, Joshua D, Pour L, Hájek R, et al. Carfilzomib and dexamethasone versus bortezomib and dexamethasone for patients with relapsed or refractory multiple myeloma (ENDEAVOR): a randomised, phase 3, open-label, multicentre study. Lancet Oncol. 2016;17:27–38.
Ludwig H, Moreau P, Dimopoulos MA, Mateos M-V, Kaiser MF, Feng S, et al. Health related quality of life results from the open-label, randomized, phase III Endeavor trial evaluating carfilzomib and dexamethasone versus bortezomib and dexamethasone in patients with relapsed or refractory multiple myeloma. Blood. 2016;128:3309.
Siegel DS, Dimopoulos MA, Ludwig H, Facon T, Goldschmidt H, Jakubowiak A, et al. Improvement in overall survival with carfilzomib, lenalidomide, and dexamethasone in patients with relapsed or refractory multiple myeloma. J Clin Oncol. 2018;36:728–34.
Stewart AK, Dimopoulos MA, Masszi T, Špička I, Oriol A, Hájek R, et al. Health-related quality-of-life results from the open-label, randomized, phase III ASPIRE trial evaluating carfilzomib, lenalidomide, and dexamethasone versus lenalidomide and dexamethasone in patients with relapsed multiple myeloma. J Clin Oncol. 2016;34:3921–30.
Stewart AK, Rajkumar SV, Dimopoulos MA, Masszi T, Špička I, Oriol A, et al. Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma. N Engl J Med. 2015;372:142–52.
Moreau P, Mateos MV, Berenson JR, Weisel K, Lazzaro A, Song K, et al. Once weekly versus twice weekly carfilzomib dosing in patients with relapsed and refractory multiple myeloma (A.R.R.O.W.): interim analysis results of a randomised, phase 3 study. Lancet Oncol. 2018;19:953–64.
Moreau P, Kumar S, Boccia R, Iida S, Goldschmidt H, Cocks K, et al. Patient-reported outcomes (PROs) from the phase 3 A.R.R.O.W. Study comparing once-weekly versus twice-weekly carfilzomib dosing in relapsed and refractory multiple myeloma (RRMM). Clin Lymphoma, Myeloma Leuk. 2018;18:S240.
Jakubowiak AJ, Dytfeld D, Griffith KA, Lebovic D, Vesole DH, Jagannath S, et al. A phase 1/2 study of carfilzomib in combination with lenalidomide and low-dose dexamethasone as a frontline treatment for multiple myeloma. Blood. 2012;120:1801–9.
Dytfeld D, Jasielec J, Griffith KA, Lebovic D, Vesole DH, Jagannath S, et al. Carfilzomib, lenalidomide, and low-dose dexamethasone in elderly patients with newly diagnosed multiple myeloma. Haematologica. 2014;99:e162–e164.
Jakubowiak A, Raje N, Vij R, Reece D, Berdeja J, Vesole D, et al. Improved efficacy after incorporating autologous stem cell transplant (ASCT) into KRd treatment with carfilzomib (CFZ), lenalidomide (LEN), and dexamethasone (DEX) in newly diagnosed multiple myeloma. Haematologica. 2016;101(s1):Abstract S101.
Korde N, Roschewski M, Zingone A, Kwok M, Manasanch EE, Bhutani M, et al. Treatment with carfilzomib-lenalidomide-dexamethasone with lenalidomide extension in patients with smoldering or newly diagnosed multiple myeloma. JAMA Oncol. 2015;1:746–54.
Tageja N, Korde N, Kazandjian D, Panch S, Manasanch E, Bhutani M, et al. Combination therapy with carfilzomib, lenalidomide and dexamethasone (KRd) results in an unprecedented purity of the stem cell graft in newly diagnosed patients with myeloma. Bone Marrow Transpl. 2018;53:1445–9.
Kazandjian D, Korde N, Mailankody S, Hill E, Figg WD, Roschewski M, et al. Remission and progression-free survival in patients with newly diagnosed multiple myeloma treated with carfilzomib, lenalidomide, and dexamethasone: five-year follow-up of a phase 2 clinical trial. JAMA Oncol. 2018;4:1781–3.
Zimmerman T, Raje NS, Vij R, Reece D, Berdeja JG, Stephens LA, et al. Final results of a phase 2 trial of extended treatment (tx) with carfilzomib (CFZ), lenalidomide (LEN), and dexamethasone (KRd) plus autologous stem cell transplantation (ASCT) in newly diagnosed multiple myeloma (NDMM). Blood. 2016;128:675.
Jakubowiak AJ, Raje N, Vij R, Reece D, Berdeja JG, Stephens L, et al. High rate of sustained minimal residual disease negativity predicts prolonged survival for the overall patient population in the phase 2 KRd plus autologous stem cell transplantation MMRC trial. Blood. 2017;130:4533.
Roussel M, Lauwers-Cances V, Robillard N, Belhadj K, Facon T, Garderet L, et al. Frontline therapy with carfilzomib, lenalidomide, and dexamethasone (KRd) induction followed by autologous stem cell transplantation, Krd consolidation and lenalidomide maintenance in newly diagnosed multiple myeloma (NDMM) patients: primary results of the Intergroupe Francophone Du MyéLome (IFM) Krd phase II study. Blood. 2016;128:1142. Presented at the ASH 2016 Annual Meeting, San Diego, CA; December 3–6, 2016
Korde N, Mastey D, Mailankody S, Hassoun H, Lesokhin AM, Smith EL, et al. MRD-response driven phase I/II study for newly diagnosed multiple myeloma patients using higher doses of twice-weekly carfilzomib (45 and 56 mg/m2) in combination with lenalidomide and dexamethasone. Blood. 2018;132:1983.
Bringhen S, Petrucci MT, Larocca A, Conticello C, Rossi D, Magarotto V, et al. Carfilzomib, cyclophosphamide, and dexamethasone in patients with newly diagnosed multiple myeloma: a multicenter, phase 2 study. Blood. 2014;124:63–69.
Gay F, Cerrato C, Rota Scalabrini D, Galli M, Belotti A, Zamagni E, et al. Carfilzomib-lenalidomide-dexamethasone (KRd) induction-autologous transplant (ASCT)-Krd consolidation vs KRd 12 cycles vs carfilzomib-cyclophosphamide-dexamethasone (KCd) induction-ASCT-KCd consolidation: analysis of the randomized Forte trial in newly diagnosed multiple myeloma (NDMM). Blood. 2018;132:121. Presented at the ASH 2018 Annual Meeting, San Diego, CA; December 1–4, 2018.
Mateos M-V, Martínez-López J, Rodriguez Otero P, Ocio EM, Gonzalez MS, Oriol A, et al. Curativestategy (GEM-CESAR) for high-risk smoldering myeloma (SMM): carfilzomib, Lenalidomide and dexamethasone (KRd) as induction followed by HDT-ASCT, consolidation with Krd and maintenance with Rd. Blood. 2018;132:2142.
Gay FM, Rota Scalabrini D, Belotti A, Galli M, Zamagni E, Offidani M, et al. A randomized study of carfilzomib-lenalidomide-dexamethasone vs carfilzomib-cyclophosphamide-dexamethasone induction in newly diagnosed myeloma patients eligible for transplant: high efficacy in high- and standard-risk patients. Blood. 2017;130:4541.
Sonneveld P, Asselbergs E, Zweegman S, van der Holt B, Kersten MJ, Vellenga E, et al. Phase 2 study of carfilzomib, thalidomide, and dexamethasone as induction/consolidation therapy for newly diagnosed multiple myeloma. Blood. 2015;125:449–56.
Wester R, van der Holt B, Asselbergs E, Zweegman S, Kersten MJ, Vellenga E, et al. Carfilzomib combined with thalidomide and low-dose dexamethasone for remission induction and consolidation in newly diagnosed, transplant eligible patients with multiple myeloma: the Carthadex trial. Blood. 2017;130:3141.
Wester R, van der Holt B, Asselbergs E, Zweegman S, Kersten MJ, Vellenga E, et al. Update of the phase 2 study of carfilzomib thalidomide and low-dose dexamethasone as induction/consolidation in newly diagnosed transplant eligible patients with multiple myeloma, Carthadex trial. HemaSphere. 2018;2(S1):1–1113.
Mikhael JR, Reeder CB, Libby EN, Costa LJ, Bergsagel PL, Buadi F, et al. Phase Ib/II trial of CYKLONE (cyclophosphamide, carfilzomib, thalidomide and dexamethasone) for newly diagnosed myeloma. Br J Haematol. 2015;169:219–27.
Gregersen H, Do T, Kristensen IB, Frølund UC, Andersen NF, Nielsen LK, et al. A randomized placebo-controlled phase II study of clarithromycin or placebo combined with VCD induction therapy prior to high-dose melphalan with stem cell support in patients with newly diagnosed multiple myeloma. Exp Hematol Oncol. 2018;7:18.
Moriya S, Che XF, Komatsu S, Abe A, Kawaguchi T, Gotoh A, et al. Macrolide antibiotics block autophagy flux and sensitize to bortezomib via endoplasmic reticulum stress-mediated CHOP induction in myeloma cells. Int J Oncol. 2013;42:1541–50.
Forsberg PA, Rossi AC, Pearse RN, Perry A, Pekle K, Jayabalan D, et al. Carfilzomib induction with lenalidomide and clarithromycin consolidation and lenalidomide maintenance (CarBiRD) for multiple myeloma (MM). Blood. 2016;128:4518.
Jackson GH, Davies FE, Pawlyn C, Cairns D, Striha A, Hockaday A, et al. A quadruplet regimen comprising carfilzomib, cyclophosphamide, lenalidomide, dexamethasone (KCRD) vs an immunomodulatory agent containing triplet (CTD/CRD) induction therapy prior to autologous stem cell transplant: results of the Myeloma XI study. Blood. 2018;132:302. Presented at the ASH 2018 Annual Meeting, San Diego, CA; December 1–4, 2018.
Chari A, Usmani SZ, Krishnan A, Krishnan A, Lonial S, Comenzo R, et al. Daratumumab (DARA) in combination with carfilzomib, lenalidomide, and dexamethasone (KRd) in patients with newly diagnosed multiple myeloma (MMY1001): updated results from an open-label, phase 1b study. Blood. 2017;130:3110.
Jakubowiak AJ, Chari A, Lonial S, Weiss BM, Comenzo RL, Wu K, et al. Daratumumab (DARA) in combination with carfilzomib, lenalidomide, and dexamethasone (KRd) in patients (pts) with newly diagnosed multiple myeloma (MMY1001): an open-label, phase 1b study. J Clin Oncol. 2017;35(15_suppl)):8000–8000.
Landgren O, Thoren K, Hultcrantz M, et al. Bone marrow-based and longitudinal blood-based MRD tracking in newly diagnosed multiple myeloma patients treated with daratumumab, carfilzomib, lenalidomide and dexamethasone (DKRd): a correlative and clinical phase II study. Blood. 2018;132:3281.
Genmab announces positive topline results in phase III CASSIOPEIA study of daratumumab in front line multiple myeloma. Genmab. October 21, 2018. https://ir.genmab.com/news-releases/news-release-details/genmab-announces-positive-topline-results-phase-iii-cassiopeia. Accessed May 3, 2019.
Ziogas DC, Terpos E, Kastritis E, Dimopoulos MA. An overview of the role of carfilzomib in the treatment of multiple myeloma. Expert Opin Pharm. 2017;18:1883–97.
Siegel D, Martin T, Nooka A, Harvey RD, Vij R, Niesvizky R, et al. Integrated safety profile of single-agent carfilzomib: experience from 526 patients enrolled in 4 phase II clinical studies. Haematologica. 2013;98:1753–61.
Chari A, Stewart AK, Russell SD, Moreau P, Herrmann J, Banchs J, et al. Analysis of carfilzomib cardiovascular safety profile across relapsed and/or refractory multiple myeloma clinical trials. Blood Adv. 2018;2:1633–44.
Jakubowiak AJ, DeCara JM, Mezzi K. Cardiovascular events during carfilzomib therapy for relapsed myeloma: practical management aspects from two case studies. Hematology 2017;22:585–91.
Mikhael J. Management of carfilzomib-associated cardiac adverse events. Clin Lymphoma Myeloma Leuk. 2016;16:241–5.
Delforge M, Bladé J, Dimopoulos MA, Facon T, Kropff M, Ludwig H, et al. Treatment-related peripheral neuropathy in multiple myeloma: the challenge continues. Lancet Oncol. 2010;11:1086–95.
Lendvai N, Tsakos I, Devlin SM, Schaffer WL, Hassoun H, Lesokhin AM, et al. Predictive biomarkers and practical considerations in the management of carfilzomib-associated cardiotoxicity. Leuk Lymphoma. 2018;59:1981–5.
Mailankody S, Korde N, Lesokhin AM, Lendvai N, Hassoun H, Stetler-Stevenson M, et al. Minimal residual disease in multiple myeloma: bringing the bench to the bedside. Nat Rev Clin Oncol. 2015;12:286–95.
Landgren O, Siegel DS, Auclair D, Chari A, Boedigheimer M, Welliver T, et al. Carfilzomib-lenalidomide-dexamethasone versus bortezomib-lenalidomide-dexamethasone in patients with newly diagnosed multiple myeloma: results from the prospective, longitudinal, observational Commpass study. Blood. 2018;132:799.
Li B, Ren K, Shen L, Hou P, Su Z, Di Bacco A, et al. Comparing bortezomib-lenalidomide-dexamethasone (VRd) with carfilzomib-lenalidomide-dexamethasone (KRd) in the patients with newly diagnosed multiple myeloma (NDMM) in two observational studies. Blood. 2018;132:3298.
Waxman AJ, Clasen S, Hwang WT, Garfall A, Vogl DT, Carver J, et al. Carfilzomib-associated cardiovascular adverse events: a systematic review and meta-analysis. JAMA Oncol. 2018;4:e174519.
Acknowledgements
Medical writing assistance was provided by BlueMomentum, an Ashfield Company, part of UDG Healthcare PLC, and Jacqueline Sayyah, of Amgen, Inc, and funded by Amgen, Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr Landgren has received research funding from the National Institutes of Health, U.S. Food and Drug Administration, Multiple Myeloma Research Foundation, International Myeloma Foundation, Leukemia and Lymphoma Society, Perelman Family Foundation, Rising Tides Foundation, Amgen, Celgene, Janssen, Takeda, Glenmark, Seattle Genetics, and Karyopharm; has served on honoraria/advisory boards for Adaptive, Amgen, Binding Site, BMS, Celgene, Cellectis, Glenmark, Janssen, Juno, Pfizer; and serves on Independent Data Monitoring Committees for clinical trials led by Takeda, Merck, Janssen. Dr Sonneveld received research funding from Janssen, Celgene, Amgen, Karyopharm, SkylineDx, Takeda, and Novartis; and received personal fees from Janssen, Celgene, and Amgen. Dr Jakubowiak repots consultancy, honoraria, and membership on an entity’s Board of Directors or Advisory Committees fees from Amgen, ABBVIE, BMS, Celgene, Janssen, Karyopharm, Millennium, Takeda, Sanofi, and SkylineDx. Dr Mohty has no disclosures to report. Dr Iskander and Dr Mezzi are employees of and own stock in Amgen, Inc. Dr Siegel reports honoraria and consulting or advisory role fees for Celgene, Amgen, Merck, Janssen, BMS, Takeda, and Karyopharm; speakers’ bureau participation for Celgene, Amgen, Merck, Janssen, BMS, and Takeda; and research funding from Celgene.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Landgren, O., Sonneveld, P., Jakubowiak, A. et al. Carfilzomib with immunomodulatory drugs for the treatment of newly diagnosed multiple myeloma. Leukemia 33, 2127–2143 (2019). https://doi.org/10.1038/s41375-019-0517-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-019-0517-6
This article is cited by
-
Global analysis of HBV-mediated host proteome and ubiquitylome change in HepG2.2.15 human hepatoblastoma cell line
Cell & Bioscience (2021)
-
A clinical perspective on plasma cell leukemia; current status and future directions
Blood Cancer Journal (2021)
-
The role of novel agents for consolidation after autologous transplantation in newly diagnosed multiple myeloma: a systematic review
Annals of Hematology (2021)
-
Current Approach to Managing Patients with Newly Diagnosed High-Risk Multiple Myeloma
Current Hematologic Malignancy Reports (2021)
-
Consolidation with carfilzomib, lenalidomide, and dexamethasone (KRd) following ASCT results in high rates of minimal residual disease negativity and improves bone metabolism, in the absence of bisphosphonates, among newly diagnosed patients with multiple myeloma
Blood Cancer Journal (2020)