Abstract
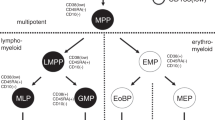
CD69 regulates lymphocyte egress from the thymus and lymph nodes through cis-interactions and the downregulation of surface sphingosine-1-phosphate (S1P) receptor-1 (S1P1). However, its role in the regulation of cell egress from bone marrow has not been extensively studied. We show here that CD69 targeting induced rapid and massive mobilization of BM leukocytes, which was inhibited by desensitization to S1P with FTY720. This mobilization was reproduced with anti-human CD69 mAb treatment of mice expressing human CD69. In this strain, the mobilization occurred to the same extent as that induced by AMD3100. The anti-human CD69 treatment highly increased LSK and CLP cell proliferation and numbers, both in the periphery and in the BM, and also augmented S1P1 and CXCR4 expression. Additionally, increased mTOR, p70S6K, S6, and 4E-BP1 phosphorylation was detected after in vivo anti-CD69 treatment in the bone marrow. Importantly, mTOR inhibition with rapamycin inhibited anti-huCD69-induced mobilization of hematopoietic stem and progenitor cells (HSPCs). Together, our results indicated that CD69 targeting induces not only mobilization but also high proliferation of HSPCs, and thus is crucial for precursor cell replenishment over time. These results suggest that anti-CD69 mAbs are putative novel candidates for mobilization strategies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Broxmeyer HE, Orschell CM, Clapp DW, Hangoc G, Cooper S, Plett PA., et al. Rapid mobilization of murine and human hematopoietic stem and progenitor cells with AMD3100, a CXCR4 antagonist. J Exp Med. 2005;201:1307–18. https://doi.org/10.1084/jem.20041385.
Ponomaryov T, Peled A, Petit I, Taichman RS, Habler L, Sandbank J., et al. Induction of the chemokine stromal-derived factor-1 following DNA damage improves human stem cell function. J Clin Invest. 2000;106:1331–9. https://doi.org/10.1172/JCI10329.
Dar A, Schajnovitz A, Lapid K, Kalinkovich A, Itkin T, Ludin A, et al. Rapid mobilization of hematopoietic progenitors by AMD3100 and catecholamines is mediated by CXCR4-dependent SDF-1 release from bone marrow stromal cells. Leukemia. 2011;25:1286–96. https://doi.org/10.1038/leu.2011.62.
Petit I, Szyper-Kravitz M, Nagler A, Lahav M, Peled A, Habler L., et al. G-CSF induces stem cell mobilization by decreasing bone marrow SDF-1 and up-regulating CXCR4. Nat Immunol. 2002;3:687–94.10.1038/ni813.
Metcalf D, Nicola NA. Proliferative effects of purified granulocyte colony-stimulating factor (G-CSF) on normal mouse hemopoietic cells. J Cell Physiol. 1983;116:198–206. https://doi.org/10.1002/jcp.1041160211.
Karpova D, Ritchey J, Holt M, Abou-Ezzi G, Monlish D, Batoon L, et al. Continuous blockade of CXCR4 results in dramatic mobilization and expansion of hematopoietic stem and progenitor cells. Blood. 2017. https://doi.org/10.1182/blood-2016-10-746909.
Takabe K, Paugh SW, Milstien S, Spiegel S. “Inside-out” signaling of sphingosine-1-phosphate: therapeutic targets. Pharmacol Rev. 2008;60:181–95. https://doi.org/10.1124/pr.107.07113.
Golan K, Vagima Y, Ludin A, Itkin T, Cohen-Gur S, Kalinkovich A, et al. S1P promotes murine progenitor cell egress and mobilization via S1P1-mediated ROS signaling and SDF-1 release. Blood. 2012;119:2478–88. https://doi.org/10.1182/blood-2011-06-358614.
Juarez JG, Harun N, Thien M, Welschinger R, Baraz R, Pena AD, et al. Sphingosine-1-phosphate facilitates trafficking of hematopoietic stem cells and their mobilization by CXCR4 antagonists in mice. Blood. 2012;119:707–16. https://doi.org/10.1182/blood-2011-04-348904.
Pereira JP, Xu Y, Cyster JG. A role for S1P and S1P1 in immature-B cell egress from mouse bone marrow. PloS ONE. 2010;5:e9277. https://doi.org/10.1371/journal.pone.0009277.
Maeurer C, Holland S, Pierre S, Potstada W, Scholich K. Sphingosine-1-phosphate induced mTOR-activation is mediated by the E3-ubiquitin ligase PAM. Cell Signal. 2009;21:293–300. https://doi.org/10.1016/j.cellsig.2008.10.016.
Tesio M, Golan K, Corso S, Giordano S, Schajnovitz A, Vagima Y, et al. Enhanced c-Met activity promotes G-CSF-induced mobilization of hematopoietic progenitor cells via ROS signaling. Blood. 2011;117:419–28. https://doi.org/10.1182/blood-2009-06-230359.
Vagima Y, Avigdor A, Goichberg P, Shivtiel S, Tesio M, Kalinkovich A, et al. MT1-MMP and RECK are involved in human CD34+ progenitor cell retention, egress, and mobilization. J Clin Invest. 2009;119:492–503. https://doi.org/10.1172/JCI36541.
Cibrian D, Sanchez-Madrid F. CD69: from activation marker to metabolic gatekeeper. Eur J Immunol. 2017;47:946–53. https://doi.org/10.1002/eji.201646837.
Notario L, Alari-Pahissa E, de Molina A, Lauzurica P. CD69 Deficiency Enhances the Host Response to Vaccinia Virus Infection through Altered NK Cell Homeostasis. J Virol. 2016;90:6464–74. https://doi.org/10.1128/JVI.00550-16.
Esplugues E, Vega-Ramos J, Cartoixa D, Vazquez BN, Salaet I, Engel P, et al. Induction of tumor NK-cell immunity by anti-CD69 antibody therapy. Blood. 2005;105:4399–406. https://doi.org/10.1182/blood-2004-10-3854.
Sancho D, Gomez M, Martinez Del Hoyo G, Lamana A, Esplugues E, Lauzurica P, et al. CD69 targeting differentially affects the course of collagen-induced arthritis. J Leukoc Biol. 2006;80:1233–41. https://doi.org/10.1189/jlb.1205749.
Matloubian M, Lo CG, Cinamon G, Lesneski MJ, Xu Y, Brinkmann V, et al. Lymphocyte egress from thymus and peripheral lymphoid organs is dependent on S1P receptor 1. Nature. 2004;427:355–60. https://doi.org/10.1038/nature02284.
Shiow LR, Rosen DB, Brdickova N, Xu Y, An J, Lanier LL, et al. CD69 acts downstream of interferon-alpha/beta to inhibit S1P1 and lymphocyte egress from lymphoid organs. Nature. 2006;440:540–4. https://doi.org/10.1038/nature04606.
Mackay LK, Rahimpour A, Ma JZ, Collins N, Stock AT, Hafon ML, et al. The developmental pathway for CD103(+)CD8 + tissue-resident memory T cells of skin. Nat Immunol. 2013;14:1294–301. https://doi.org/10.1038/ni.2744.
Shinoda K, Tokoyoda K, Hanazawa A, Hayashizaki K, Zehentmeier S, Hosokawa H, et al. Type II membrane protein CD69 regulates the formation of resting T-helper memory. Proc Natl Acad Sci USA. 2012;109:7409–14. https://doi.org/10.1073/pnas.1118539109.
Alari-Pahissa E, Vega-Ramos J, Zhang JG, Castano AR, Turley SJ, Villadangos JA, et al. Differential effect of CD69 targeting on bystander and antigen-specific T cell proliferation. J Leukoc Biol. 2012;92:145–58. https://doi.org/10.1189/jlb.1011499.
Yang Q, Wang J, Liu R, Wang Z, Li Y, Zhang Y, et al. Amelioration of concanavalin A-induced autoimmune hepatitis by magnesium isoglycyrrhizinate through inhibition of CD4(+)CD25(-)CD69(+) subset proliferation. Drug Des Devel Ther. 2016;10:443–53. https://doi.org/10.2147/DDDT.S92440.
Esplugues E, Sancho D, Vega-Ramos J, Martinez C, Syrbe U, Hamann A, et al. Enhanced antitumor immunity in mice deficient in CD69. J Exp Med. 2003;197:1093–106. https://doi.org/10.1084/jem.20021337.
Cyster JG, Schwab SR. Sphingosine-1-phosphate and lymphocyte egress from lymphoid organs. Annu Rev Immunol. 2012;30:69–94. https://doi.org/10.1146/annurev-immunol-020711-075011.
Edwards LE, Haluszczak C, Kedl RM. Phenotype and function of protective, CD4-independent CD8 T cell memory. Immunol Res. 2013;55:135–45. https://doi.org/10.1007/s12026-012-8356-9.
Madan VMB, Brykczynska U, Zilbermann F, Hogeveen K, Döhner K, Döhner H, et al. Impaired function of primitive hematopoietic cells in mice lacking the Mixed-Lineage-Leukemia homolog MLL5. Blood. 2009;113:1444–54. https://doi.org/10.1182/blood-2008-02-142638.
Merchant A, Joseph G, Wang Q, Brennan S, Matsui W. Gli1 regulates the proliferation and differentiation of HSCs and myeloid progenitors. Blood. 2010;115:2391–6. https://doi.org/10.1182/blood-2009-09-241703.
Tassone P, Turco MC, Tuccillo F, Bonelli P, Morrone G, Cecco L, et al. CD69 expression on primitive progenitor cells and hematopoietic malignancies. Tissue Antigens. 1996;48:65–68.
Sancho D, Gomez M, Sanchez-Madrid F. CD69 is an immunoregulatory molecule induced following activation. Trends Immunol. 2005;26:136–40. https://doi.org/10.1016/j.it.2004.12.006.
Martin P, Gomez M, Lamana A, Cruz-Adalia A, Ramirez-Huesca M, Ursa MA, et al. CD69 association with Jak3/Stat5 proteins regulates Th17 cell differentiation. Mol Cell Biol. 2010;30:4877–89. https://doi.org/10.1128/MCB.00456-10.
Allende ML, Tuymetova G, Lee BG, Bonifacino E, Wu YP, Proia RL. S1P1 receptor directs the release of immature B cells from bone marrow into blood. J Exp Med. 2010;207:1113–24. https://doi.org/10.1084/jem.20092210.
Ratajczak MZ, Lee H, Wysoczynski M, Wan W, Marlicz W, Laughlin MJ, et al. Novel insight into stem cell mobilization-plasma sphingosine-1-phosphate is a major chemoattractant that directs the egress of hematopoietic stem progenitor cells from the bone marrow and its level in peripheral blood increases during mobilization due to activation of complement cascade/membrane attack complex. Leukemia. 2010;24:976–85. https://doi.org/10.1038/leu.2010.53.
Acknowledgements
The study was supported by the Instituto de Salud Carlos III MPY 1366/13 and MPY 1346/16. ML was supported by SAF2015-74112-JIN from MINECO. GS was supported by ERC 260464, EFSD 2030, MINECO-FEDER SAF2016-79126-R, and Comunidad de Madrid S2010/BMD-2326. The CNIC is supported by the Ministerio de Economía y Competitividad and the Pro-CNIC Foundation. The Pro-CNIC Foundation is a Severo Ochoa Center of Excellence (MINECO award SEV-2015-0505). We are grateful to Dra Ana Justel, of UAM, for help in statistical analysis. We thank Daniel Baizan, Cristina Pintos, and Maria Clemente for mouse husbandry.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Notario, L., Alari-Pahissa, E., Albentosa, A. et al. Anti-CD69 therapy induces rapid mobilization and high proliferation of HSPCs through S1P and mTOR. Leukemia 32, 1445–1457 (2018). https://doi.org/10.1038/s41375-018-0052-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-018-0052-x
This article is cited by
-
Single-cell transcriptomics reveals multiple chemoresistant properties in leukemic stem and progenitor cells in pediatric AML
Genome Biology (2023)
-
Rapid activation of hematopoietic stem cells
Stem Cell Research & Therapy (2023)
-
The role of sphingosine-1-phosphate in autophagy and related disorders
Cell Death Discovery (2023)
-
SphK-produced S1P in somatic cells is indispensable for LH-EGFR signaling-induced mouse oocyte maturation
Cell Death & Disease (2022)
-
Comparison of the efficacy of hematopoietic stem cell mobilization regimens: a systematic review and network meta-analysis of preclinical studies
Stem Cell Research & Therapy (2021)