Abstract
During the last few years, several new drugs have been introduced for treatment of patients with multiple myeloma, which have significantly improved the treatment outcome. All of these novel substances differ at least in part in their mode of action from similar drugs of the same drug class, or are representatives of new drug classes, and as such present with very specific side effect profiles. In this review, we summarize these adverse events, provide information on their prevention, and give practical guidance for monitoring of patients and for management of adverse events.
Similar content being viewed by others
Introduction
During the last years, options for multiple myeloma have increased substantially with the introduction of several immunomodulatory agents (IMiDs), proteasome inhibitors (PIs), monoclonal antibodies (mAbs), and a histone deacetylase inhibitor (HDACi). Inclusion of novel drugs in myeloma therapy resulted in an increased depth of responses, improved progression-free and overall survival with substantial gains in transplant-eligible patients, and more moderate improvements in elderly patients. The new drugs differ not only in their mode of action, but importantly, also in their toxicity profile from previous standard treatments. Here, we present the most relevant side effects of the novel drugs reported in pivotal clinical studies and discuss strategies for their prevention and management.
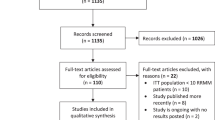
Methods
Pivotal trials leading to drug approval, and references of all regimens recommended by the National Comprehensive Cancer Network (NCCN) clinical practice guidelines on multiple myeloma, version 1.2018 [1], served as a basis for the summaries of treatment-emergent adverse events (AEs). Table S1 of the online supplemental material summarizes the indications approved in the United States (US) and the European Union (EU) valid at the time of writing. Tables 1 and S3 summarize the special warnings and precautions with regard to toxicities of novel agents and common backbone agents as per US prescribing information (USPI) and EU summary of medicinal product characteristics (EU SmPC). These form a patient monitoring guide for complications potentially associated with the approved regimens. All grade ≥3 AEs reported in the pivotal trials leading to US and/or EU approval and published at the time of writing are summarized in Table S2A–D. Where clearly identified in the drug labels, a distinction was made between AEs, defined as “…any untoward medical occurrence in a patient administered a medicinal product and which does not necessarily have to have a causal relationship with this treatment” and adverse drug reactions (ADRs), defined as “…all noxious and unintended responses to a medicinal product related to any dose…” [2]. When a clear classification was not available, the event was listed by the term used in the source document or generally as AE.
The AEs that are discussed in the management section were selected based on their clinical importance rather than their incidence. Management recommendations were taken from available guidelines, such as those developed by the International Myeloma Working Group [3,4,5], the European Myeloma Network [6], the NCCN [1, 7], the British Committee for Standards in Hematology/United Kingdom Myeloma Forum [8], from literature referenced in the respective sections, and from the USPIs and EU SmPCs. These recommendations are subject to the treating physician’s best clinical judgment.
Incidence of adverse events
Multiple myeloma shows a wide range of tumor-related co-morbidities [4, 9] and the majority of patients receive a number of anti-myeloma drugs and medication to ameliorate tumor-associated or other co-morbidities. Thus, it is frequently impossible to clearly attribute a specific side effect to an individual drug. The AEs listed below therefore should be interpreted in the context of complications of the disease, of specific drugs or drug combinations administered, and of supportive or prophylactic measures. Of note, uniform reporting standards for AEs, such as the Medical Dictionary for Regulatory Activities (MedDRA, www.meddra.org) or the Common Terminology Criteria for Adverse Events (CTCAE, https://ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm), are not yet consistently used throughout studies, leading to a substantial variation in the documentation of quality, incidence, and grade of AEs (Table S2A–D).
Warnings and precautions for use of individual drugs as listed in the respective USPIs and EU SmPCs are shown in Table 1 (novel agents) and Table S3 (backbone agents) and provide guidance for patient monitoring during treatment.
Immunomodulatory agents (IMiDs)
The overall incidence of AEs reported in pivotal trials employing IMiD-based regimens is shown in Table S2A. All IMiDs are structural analogs of thalidomide and thus teratogenic. Adequate patient education and contraceptive measures are therefore mandatory for all three drugs of this class [10,11,12,13,14,15].
Thalidomide
In the United States, thalidomide (T)-based therapies are no longer widely used. In Europe, thalidomide is part of the VTD regimen for induction therapy before ASCT and remains an essential element of myeloma therapy in major regions of the world, like South America, parts of Asia, and several Eastern European countries. The incidence and severity of thalidomide-related AEs is dose and treatment duration dependent and influenced by potential comorbidities and toxicities of co-medications. Susceptibility for thalidomide-induced peripheral neuropathy (PNP) has been linked to polymorphism of genes governing repair mechanisms and inflammation in the peripheral nervous system [16]. A systematic review revealed somnolence, constipation, neuropathy, rash, cardiac events, and venous thromboembolism as the most frequent grade 3 or 4 AEs of thalidomide single-agent therapy, particularly with doses >200 mg/day in relapsed/refractory multiple myeloma (RRMM) [17]. In clinical trials using melphalan and prednisone in combination with thalidomide (MPT), hematological events, infections, other neurological toxicities, PNP, deep vein thrombosis, and dermatological toxicity were predominant [18, 19]. In addition, arterial thromboembolism, drowsiness, dizziness, orthostatic hypotension, neutropenia, thrombocytopenia, increased HIV viral load, bradycardia, serious dermatological reactions (Stevens–Johnson syndrome and toxic epidermal necrolysis), seizures, tumor lysis syndrome, and complications that are more frequent while on contraceptives, hypersensitivity, and increased risk for secondary primary malignancies were reported [13].
Patients should be monitored for thromboembolic complications, PNP, rash/skin reactions, bradycardia, arrhythmia, syncope, somnolence, neutropenia, thrombocytopenia, and others (Table 1) [10, 13].
Lenalidomide
The toxicity profile of lenalidomide (R), although structurally very similar to thalidomide, differs remarkably from the originator compound (Table S2A). Notably, neuropathy, constipation, and somnolence are rare, while hematologic AEs are more frequent [20]. Grade ≥3 neutropenia was reported in 26% of patients treated with lenalidomide–dexamethasone (Rd) for 18 cycles and in 28% of those on continuous Rd in the FIRST trial [21]. Grade ≥3 thrombocytopenia occurred in 8% of patients in either arm. The most frequent non-hematological grade ≥3 side effects occurring in the Rd 18 arm in more than 5% were infections (22%), fatigue (9%), cardiac disorders (7%), venous thromboembolism (6%), and asthenia (6%). Long-term lenalidomide therapy may be associated with chronic diarrhea [22]. Side effects observed with MPR and MPR followed by R maintenance in the MM015 trial [23] were similar to those reported for the FIRST trial and are listed in Table S2A. Lenalidomide therapy is associated with an increased risk for second primary malignancies, especially in the post-transplantation setting [24,25,26], or after a melphalan-containing regimen [27], and after an IMiD-based induction therapy [28]. Data from the latter study show a cumulative incidence of 0.7, 2.3, and 3.8% after 1, 2, and 3 years, with the highest incidence in elderly patients. Lenalidomide is to a substantial degree excreted by the kidney and the dose has to be adapted to glomerular filtration rate [29]. Dose modifications are indicated for grade 3 or 4 neutropenia or thrombocytopenia, and for grade 2 to 3 skin rash.
Patients should be monitored for hematological events, thromboembolic complications, PNP, infections, severe skin reactions, diarrhea, secondary malignancies, allergic reactions, cataracts, and others (Table 1) [11, 14].
Pomalidomide
The most frequently reported grade 3 or 4 ADRs reported in heavily pretreated patients receiving pomalidomide were hematological ADRs, including neutropenia, anemia, and thrombocytopenia (Table S2A). Other severe ADRs included infections, fatigue, pyrexia, peripheral edema, and venous thromboembolic events. Cases of PNP were non-serious, although it is of note that patients with ongoing grade ≥2 PNP were excluded from clinical trials with pomalidomide. Modifications of pomalidomide dose are indicated for grade 3 or 4 neutropenia or thrombocytopenia, and for grade 2 to 3 skin rash.
Patients should be monitored for hematological events, thromboembolic complications, skin rash, infections, PNP, diarrhea, secondary malignancies, allergic reactions, dizziness, confusion, and others (Table 1) [12, 15].
Proteasome inhibitors (PIs)
The overall incidence of AEs reported in published pivotal trials employing PI-based regimens is shown in Table S2B.
Bortezomib
The most commonly reported ADRs occurring during treatment with bortezomib were neutropenia, thrombocytopenia, anemia, PNP (including sensory), herpes zoster, nausea, diarrhea, constipation, vomiting, fatigue, pyrexia, headache, paresthesia, decreased appetite, dyspnea, rash, and myalgia (Table S2B). Dose modifications are indicated in response to hematological AEs as well as PNP. Viral prophylaxis is mandatory and will be discussed in the prevention and management section.
Patients should be monitored for viral re-activation, PNP, constipation, diarrhea, progressive multifocal leukoencephalopathy, seizures, hypotension, posterior reversible encephalopathy syndrome, heart failure, pulmonary disorders, and others (Table 1) [30, 31].
Carfilzomib
Carfilzomib is generally very well tolerated. The most commonly reported ADRs were anemia, fatigue, diarrhea, thrombocytopenia, nausea, pyrexia, dyspnea, respiratory tract infection, cough, and peripheral edema (Table S2B). Other, less frequent, but possibly serious ADRs include cardiac toxicity, pulmonary toxicities, pulmonary hypertension, hypertension including hypertensive crises, venous thrombosis, hemorrhage, acute renal failure, tumor lysis syndrome, infusion reactions, hepatic toxicity, posterior reversible encephalopathy syndrome, thrombotic thrombocytopenic purpura and hemolytic uremic syndrome (TTP/HUS), and embryo-fetal risk. Cardiac toxicity and dyspnea typically occurred early in the course of carfilzomib therapy, predominantly in patients with pre-existing cardiac impairment. Dose modifications are warranted in response to hematological AEs or any other severe or life-threatening non-hematologic toxicity, as well as in patients with impaired renal function [32, 33].
Patients should be monitored for pre- and postinfusional hypertension, cardiac, renal and pulmonary toxicities, diarrhea, tumor lysis syndromes, neutropenia, and thrombocytopenia, and others (Table 1) [32, 33].
Ixazomib
Experience with AEs occurring with ixazomib is limited. The most frequent AEs found to be associated with ixazomib include thrombocytopenia, gastrointestinal toxicities, PNP, peripheral edema, cutaneous reactions, and hepatotoxicity (Table S2B). Dose modifications are recommended in response to thrombocytopenia, neutropenia, rash, PNP, and for other non-hematological toxicities at the physician’s discretion when they reach grade 3 or higher [34, 35].
Patients should be monitored for thrombocytopenia, neutropenia, nausea, vomiting, diarrhea, constipation, dry eye, conjunctivitis, and others (Table 1) [34, 35].
Histone deacetylase inhibitors (HDACis)
The overall incidence of AEs reported with panobinostat in combination with bortezomib and dexamethasone (Pano-Vd, PANORAMA trial) is shown in Table S2C. The most frequent hematological AEs included thrombocytopenia, anemia, neutropenia, and lymphopenia. Non-hematological AEs included diarrhea, sometimes with significant impairment of patients’ well-being, electrolyte imbalances, increased creatinine, fatigue, decreased appetite, peripheral edema, pyrexia, nausea, and vomiting. Grade ≥3 PNP was reported relatively frequently in this combination (18% in Pano-Vd versus 15% in placebo-Vd) [36], but the frequency of this complication would be reduced, if bortezomib was given by the subcutaneous route, the present standard of care [36], or if another PI was used. Dose modifications are recommended in response to thrombocytopenia, gastrointestinal toxicities, neutropenia, and hepatic impairment.
Patients should be monitored for diarrhea, nausea, infections, cardiac toxicities, blood cell counts, blood electrolytes, liver and thyroid function, hemorrhage, and others (Table 1) [37, 38].
Monoclonal antibodies (mAbs)
The overall incidence of AEs reported in published pivotal trials for mAb-based regimens is shown in Table S2D. The most frequent AEs are infusion-related reactions (IRR), usually during the first administration, which disappear thereafter and rarely lead to treatment discontinuation.
Elotuzumab
Apart from IRR, which occurred in 10% of patients receiving elotuzumab in combination with lenalidomide and dexamethasone, the most common ADRs were fatigue, pyrexia, constipation, PNP, diarrhea, herpes zoster, nasopharyngitis, cough, pneumonia, upper respiratory tract infections, lymphopenia, decreased appetite, and weight loss. Elotuzumab is a humanized IgGk antibody and interferes with response assessment in patients with IgGk M-component. The most serious ADR was pneumonia.
Patients should be monitored for infusion reactions, infections, diarrhea, fever, cough, constipation, hepatotoxicity, and others (Table 1) [39, 40].
Daratumumab
The most commonly reported ADRs were IRR, which occurred in approximately half of patients (mostly grade 1 or 2); the majority (95%) of IRR occurred at the first infusion. Other commonly reported ADRs were anemia, neutropenia, thrombocytopenia, dyspnea, fatigue, pyrexia, cough, nausea, back pain, pneumonia, and upper respiratory tract infections (Table S2D). Daratumumab interferes with blood group serological testing, as it binds to CD38 on red blood cells and results in a positive indirect antiglobulin test (indirect Coombs test) [41, 42]. Due to its nature as an IgGk antibody, it may interfere with response assessment in patients with an IgGk M-component [43] and also with minimal residual disease assessment, because it binds to CD38-positive residual myeloma cells thus precluding detection of CD38-positive cells by diagnostic anti-CD38 antibodies as recommended by EUROFLOW for conventional flow cytometry [44]. A subcutaneous preparation is in clinical testing and will allow much faster administration with significantly reduced incidence of side effects.
Patients should be monitored for IRR, nausea, fever, cough, upper respiratory tract infection, neutropenia, thrombocytopenia, and others (Table 1) [41, 42].
Backbone agents
Backbone agents frequently used in doublet or triplet combinations with novel agents are dexamethasone, cyclophosphamide, prednisone, doxorubicin, and melphalan. Table S3 shows potentially occurring toxicities of these chemotherapy and corticosteroid backbone agents as per USPI/EU SmPC. The NCCN does no longer consider melphalan-containing regimens as the standard of care to treat patients with multiple myeloma, because of their potential to induce significant cytopenias and subsequently limit the use of novel agents [1], but melphalan continues to be a valuable backbone in non-US countries to which novel agents are added.
Prevention and management of adverse events
In multiple myeloma, it is not always possible to discriminate whether complications occur as a consequence of drug treatment, of the disease itself, or due to a combination of both. Furthermore, a combination of drugs is usually administered. AEs therefore need to be considered in the context of this complex situation. Nevertheless, it is critical to carefully monitor patients regarding possible side effects (Table 1 and Tables S2A–D and S3) to avoid early complications that may compromise therapeutic outcome. Hematological toxicities are commonly observed with most novel agents, but as their prevention and management is quite similar independent of the drugs used, we will not discuss this in detail here [3, 6].
Thromboembolic complications
Treatment-, patient-, and myeloma-specific risk factors for thromboembolic complications, which are quite frequent in multiple myeloma [8, 45], are shown in Table 2. Thromboembolic events occur more frequently during the initial phase of treatment and less commonly during episodes of well-controlled disease, in remission, or at relapse [46]. IMiDs alone and particularly in combination with dexamethasone and other drugs, such as carfilzomib [32, 33], erythropoietin, or adriamycin, are associated with an increased risk of thromboembolic events [10,11,12,13,14,15].
Modifiable risk factors should be minimized if possible. Patients with one patient-specific risk factor for thromboembolism should receive thromboprophylaxis with aspirin at a dose of 81–325 mg [1, 4, 8, 46], while those with two patient-specific or one treatment-specific risk factors should be treated either with low molecular weight heparins (LMWH) or warfarin, (Table 2) [1, 4, 8, 10,11,12,13,14,15, 46]. However, there is currently no robust evidence on the optimal duration of thromboprophylaxis, especially in active uncontrolled disease as well as in lenalidomide maintenance therapy. Concomitant administration of erythropoietic agents or other drugs known to increase the risk of thrombosis, such as hormone replacement therapy, should be used with caution [11]. If a patient experiences thromboembolic complications, anti-myeloma treatment may temporarily be discontinued and anticoagulation therapy started using adjusted dose warfarin or LMWH, and appropriate monitoring should be applied. The appropriate initial therapy in the outpatient setting is therapeutic doses of LMWH. In hospitalized patients, unfractionated heparin for a minimum of 5 days may be preferred [8]. Treatment with LMWH or coumarin should be continued for several months with lower doses of LMWH. In patients started on intravenous heparin, therapy should be resumed until the patient’s partial thromboplastin time (PPT) has increased by 1.5–2.0-fold compared to control for two consecutive days and then switched to oral warfarin or coumarin. Once the acute thromboembolic event has stabilized, anti-myeloma therapy can be restarted depending upon a benefit-risk assessment with continued anticoagulation therapy with warfarin or LMWH. Alternatively, anti-myeloma therapy should be changed to a regimen with lower risk of thromboembolic complications. Renal failure with GFR <30 ml/min limits the use of LMWH, since these drugs depend on renal clearance for drug elimination and increased blood levels increase the risk of bleeding [47].
Whether the occurrence of thromboembolic complications is associated with increased mortality in multiple myeloma is still controversial. Shorter survival was reported in patients with early thrombotic events (within 6 months after start of initial therapy or within the first 2 years) while in another study no difference in mortality was noted, neither in newly diagnosed nor in relapsed/refractory myeloma. New oral anticoagulants (NOACs), which include dabigatran, rivaroxaban, apixaban, and edoxaban, have been shown to be useful for initial and extended VTE treatment [48]. These drugs have not systematically been studied in myeloma as yet, therefore specific recommendations cannot be made at this point in time.
Peripheral neuropathy
PNP is defined as any form of damage, inflammation, or degeneration of peripheral nerves [49] and can be induced by IMiDs, some PIs, and HDACis (Table 1 and Table S2A–C). Thalidomide can cause severe, mostly irreversible PNP, with higher risk in patients with pre-existing PNP [10,11,12,13,14, 50]. Among PIs, bortezomib was shown to induce severe PNP [30, 31]. Bortezomib-induced neurodegeneration occurs via a proteasome-independent mechanism and therefore is not considered a group effect of PIs [51].
The incidence of thalidomide-induced PNP (TiPNP) is dependent on dose, treatment duration, and patient-specific factors, and presents as a sensory neuropathy with prominent symptoms of paresthesia in the hands and feet (glove-and-stocking distribution) [49, 52, 53]. TiPNP also includes numbness, and mild motor involvement with muscle cramps and weakness [49]. Dose reductions are recommended in patients with grade 1 TiPNP with no loss of function, dose reduction, or treatment interruption in patients with grade 2, interfering with function but not with activities of daily living, and treatment discontinuation in patients where lower-grade TiPNP does not resolve upon dose modifications and in patients with grade 3 or 4 TiPNP (Table 3) [10, 13, 54]. Recommendations include patient monitoring at a monthly interval for the first 3 months of treatment to detect early signs of TiPNP and to continue regular monitoring during the entire treatment duration.
Bortezomib-induced PNP (BiPNP) is predominantly sensory, with symptoms of paresthesia and numbness in distal areas, particularly in the lower limbs. BiPNP characteristically shows prominent small fiber involvement, characterized by sharp, burning pain in the toes and soles of the feet. Damage of the autonomic nervous system, including orthostatic hypotension, suppressed heart rate variability, and delayed gastric emptying, may occur. Motor neuropathy is uncommon [53]. There are clear guidelines for the treatment of BiPNP (Table 3) [54]. In case of BiPNP grade 1 with pain or grade 2, the bortezomib dose should be reduced to 1.0 mg/m2 twice weekly or the treatment interval should be extended to 1.3 mg/m2 once per week. In case of grade 2 with pain or grade 3 BiPNP treatment should be withheld until symptoms have resolved, then treatment can be re-initiated at a dose of 0.7 mg/m2 once per week. In the case if BiPNP of grade 4 treatment must be discontinued [30, 31]. Intravenous administration of bortezomib leads to 10-fold higher peak plasma levels and to higher rates of BiPNP than subcutaneous administration. Subcutaneous administration therefore reduces the incidence of BiPNP, particularly BiPNP of grade 3 or 4, without compromising the anti-myeloma effect and thus should be the preferred mode of administration [55].
Treatment of symptoms of PNP and neuropathic pain remains unsatisfactory and includes anti-convulsive agents (gabapentin and pergabalin) and antidepressants [3, 4, 8]. Other agents, such as acetyl-l-carnitine and alphalipoic acid, have shown activity in treatment of chemotherapy-emergent PNP of other cancers [54]. In case of neuropathic pain, the three-step ladder of pain management in cancer patients issued by the World Health Organization (WHO) should be followed [56]. These recommend an escalating analgesic therapy that includes opioids, such as tapentadol for very severe neuropathic pain. Topical pain medications include lidocaine and capsaicin [57]. Both, TiPN and BiPN, can also be associated with autonomic symptoms induced by damage to small fibers. These include orthostatic hypotension, sexual dysfunction, constipation, and bradycardia [49]. In rare cases, the insertion of a pacemaker should be considered [58, 59]. Recommendations for orthostatic dysregulation consist of a combination of vasoconstrictor drugs, volume expansion, compression garments, and postural adjustment, together with reduction or discontinuation of any concomitant blood pressure lowering medication. Drugs such as midodrine, pyridostigmine, and fludrocortisone can be administered, and physical inactivity should be avoided [60].
Muscle cramps and seizures
Several drugs such as lenalidomide, thalidomide, PIs, and dexamethasone can induce subtle perturbations of muscle fibers and/or of neurogenic structures, but the detailed pathogenesis of muscle cramps is still unknown [49]. Presently, specific treatment recommendations are not available. General suggestions include fluid hydration, normalizing magnesium and potassium levels, use of muscle relaxants, and moving and stretching the affected areas. However, the efficacy of these measures has not been ascertained in clinical trials.
Prophylaxis and treatment of infections
Recommendations on antimicrobial prophylaxis and vaccination are summarized in Tables 4 and 5.
Viruses
Almost all people harbor latent virus infections that normally are effectively controlled by the host’s immune surveillance system. Bortezomib, other PIs, high-dose dexamethasone or chemotherapy, and autologous stem cell transplantation inhibit specific T cell functions important for curbing latent virus infections enabling their reactivation, which may result in severe clinical complications [61]. Caregivers and patients should be aware of the increased risks inferred by immunosuppression and install appropriate prophylactic measures, if available.
Vaccination
Patients should be vaccinated against several pathogens (Table 4). The most important are influenza virus, pneumococci, and haemophilus influenzae. A trivalent or quadrivalent influenza vaccine should be used in patients, partners, and caregivers. Vaccination against pneumococci should be started with a 13-valent vaccine (PCV13) and followed at least 8 weeks later by a dose of PCV23 (23 valent polysaccharide conjugate) [62]. A herpes zoster vaccine is currently being studied in patients with multiple myeloma, but results have not been made available to date [63]. Present herpes zoster vaccines are live vaccines and controversy exists whether they can be offered to patients with well-controlled disease. As an alternative to live-attenuated vaccines, which are contraindicated for immunocompromised individuals, heat-inactivated varicella zoster vaccines, and recombinant subunit vaccines have been studied [64,65,66]. Patients and nonimmune close contacts traveling or living in areas of high endemicity of hepatitis B and hepatitis A should receive recombinant hepatitis B and A vaccine. Response to vaccines frequently is suboptimal in multiple myeloma, making it desirable to evaluate the efficacy of the vaccination. An individual report shows that repeated vaccinations with the same influenza vaccine enhances anti-vaccine antibody production [67]. Ideally, patients should already be vaccinated in the premalignant state, namely when presenting with high-risk MGUS or SMM or, when feasible, during periods of optimal disease control.
Hepatitis B and C
Patients living in regions with high prevalence of hepatitis as well as those with increased alanine transaminase should be screened using serologic tests (HBsAg, anti-HBc, and anti-HBs) for previous exposure, or ongoing infection, and/or reactivation. Preemptive antiviral prophylaxis with nucleoside/nucleotide analogs should be considered in patients with latent or previous HBV infection [68]. Formal recommendation for those with a high risk of HCV infection or with previous infections are not available, but it seems reasonable to screen the high-risk group (anti-HCV and/or HCV RNA) and to treat those with evidence of active infection with modern direct-acting antivirals.
Herpes zoster
Pain, scarring, and post-herpetic neuralgia are the most common morbidities associated with herpes zoster reactivation. In pivotal trials, herpes zoster infection occurred in 3–13% of patients receiving bortezomib monotherapy (Table S2B) [30, 31]. Therefore, antiviral prophylaxis during the entire duration of treatment with any of the available PIs, but also during treatment with mAbs, is mandatory [7]. Antiviral agents such as acyclovir, valaciclovir, and penciclovir can be used; valaciclovir and penciclovir have greater bioavailability than acyclovir making them particularly suitable for outpatient treatment [69]. Valaciclovir was shown to significantly reduce the incidence of post-herpetic neuralgia [70], but randomized controlled trials comparing the efficacy of the various agents are not available. In the case of overt viral disease, anti-myeloma therapy should be interrupted and antiviral therapy be intensified. Upon symptom relieve, anti-myeloma therapy can be continued, but a risk of renewed virus reactivation remains [7].
Cytomegalovirus
PIs and high-dose therapy increase the risk for cytomegalovirus (CMV) reactivation or infection. Such infections not rarely remain unrecognized. For diagnosis of CMV infection, polymerase chain reaction (PCR) technology should be used, because antibody testing may fail due to impaired antibody production. CMV prophylaxis is generally not recommended in multiple myeloma [71], but may be considered in selective cases with repeated CMV reactivation. In case of active infection, therapy is typically initiated with intravenous ganciclovir. For second-line treatment or in case of poor tolerance or resistance to ganciclovir, foscarnet and cidofovir can be used [7]. Several new drugs (maribavir, brincidofovir, and letermovir) are undergoing clinical trials. Oral valgancyclovir is convenient, usually well tolerated and an option for initial therapy in very fit patients and for prevention of recurrence of infections during periods of aggressive therapy. Treatment should be continued at minimum until a negative PCR test result.
Bacteria and fungi
The risk for bacterial infections is significantly higher compared to the normal population [72], and particularly high in patients with active disease after start of initial therapy [73], and in those with a history of frequent infections and in elderly frail patients. Grade 3 and 4 infections were noted in 29% of patients treated with continuous lenalidomide–dexamethasone [21] and in 16.5% of relapsed/refractory myeloma exposed to carfilzomib–lenalidomide–dexamethasone [74]. Hence, antibiotic prophylaxis with either trimethoprim–sulfamethoxazole, amoxicillin, or a quinolone should be considered for the first months after start of therapy in selected patients with high risk for bacterial infections such as very elderly patients, those with a history of several previous infections, and those exposed to regimes with a high risk of infectious complications.
Intravenous immunoglobulin is an additional option, but evidence from randomized studies supporting its efficacy is scarce. Chapel et al. showed a significant benefit with fewer infections and no sepsis by administration of 400 mg/kg intravenous immunoglobulin in patients with plateau phase [75]. A meta-analysis including nine small studies on intravenous immunoglobulins in patients with chronic lymphocytic leukemia (CLL) or multiple myeloma revealed a 55% decrease in major infections with active therapy, but no effect on overall survival [76]. Taken together, intravenous immunoglobulin prophylaxis may be considered in selected patients with a history of frequent bacterial infections independent on whether they present with humoral immunoparesis, and in patients with an ongoing severe bacterial infection with no or slow response to standard antibiotic therapy.
Data on the incidence of pneumocystis jirovecii infections during treatment with novel drugs are scarce. The risk increases with severe suppression of T cell immunity. In case of established infection, the treatment of choice is trimethoprim–sulfamethoxazole. Other options are dapsone, atovaquone, or pentamidine [1].
Severe skin reactions
Monitoring patients for severe skin reactions is recommended in patients receiving thalidomide, lenalidomide, pomalidomide, or ixazomib (Table S2A–D). For limited, localized rash, antihistamines or topical steroids are recommended. In case of mild but extensive rash, a short course of low-dose prednisone should be considered [77]. In patients with grade 2 or 3 skin rash, treatment should be interrupted or discontinued and reinstated in case of complete resolution. Rarely, severe skin reactions such as Steven–Johnson syndrome or even toxic dermal necrolysis have been reported [10, 11, 13, 14, 34]. In such severe cases, treatment should be permanently discontinued. For lenalidomide, a desensitization scheme with progressively increased doses and dosing frequencies to reach a target dose of 10 mg/day over the course of 6 weeks has been proposed [78]. Patients having experienced skin reactions during previous courses of thalidomide treatment should not receive lenalidomide [11, 14] or in case of limited alternatives should be started at a low dose and carefully be monitored. For patients developing grade 2 or 3 rash during therapy with ixazomib in combination with lenalidomide, lenalidomide should be withheld until recovery or improvement of rash to grade 1. Lenalidomide treatment can be resumed at the next lower dose. If grade 2 or 3 reappears, withhold both until rash recovers to grade 1 or lower. Following recovery, resume ixazomib at the next lower dose and resume lenalidomide at the last dose. In case of grade 4 toxicity discontinue both drugs [34].
Diarrhea
Diarrhea is a common side effect of novel drugs, and more frequently observed during exposure with bortezomib, lenalidomide, and panobinostat. Diarrhea in general was rare in patients exposed to continuous Rd (4%) or Rd18 (3%) in the FIRST study [22]. However, long-term therapy with lenalidomide may, after a long asymptomatic period, induce a specific form of diarrhea, the so-called bile salt malabsorption syndrome, which seems to result from damage of the intestinal mucosa. Increased accumulation of bile acids in the small bowel may lead to debilitating episodes of diarrhea that may severely impair the patients’ quality of life [22]. The diagnosis can be established by non-invasive selenium homocholic acid taurine (SeHCAT) scanning or is supported when treatment with bile acid binders such as colesevelam results in improvement of symptoms [79]. Following the diagnosis, dietary fat intake should be reduced (to 20% of total calories) and/or colesevelam prescribed. Usually, up to 6 × 625 mg in split doses with food per day lead to rapid improvement in bowel movements and diarrhea if bile acid malabsorption is the underlying cause [79].
Panobinostat was also shown to induce gastrointestinal side effects, particularly diarrhea, which is observed in up to 40% of patients. These events should be managed with liberal use of antidiarrheal medication, proper hydration, and antiemetics, if accompanied by emesis and nausea. The frequency of diarrhea may also be improved through appropriate dose modifications of panobinostat and/or bortezomib [36] or by combining the drug with other PIs.
Pharmacological treatment of diarrhea resulting from anti-myeloma treatment is based primarily on the empirical use of locally active opioids, such as loperamide, deodorized tincture of opium, and a combination of diphenoxylate plus atropine [80, 81]. Octreotide, a long-acting somatostatin analog, is generally reserved for use in complicated cases or as a second-line treatment for persistent diarrhea after loperamide [81]. In addition, existent dehydration and/or mineral loss should be compensated.
Renal toxicity
The renal toxicities that have been reported for lenalidomide, pomalidomide, bortezomib, carfilzomib, and elotuzumab are summarized in Table 6. Presently, there is insufficient data for panobinostat to provide evidence-based information on its renal toxicity and required dose adjustments in patients with pre-existing renal impairment. For lenalidomide and ixazomib dosing, recommendations have been issued for different levels of renal impairment. Lenalidomide should be dosed at 5 mg/day in end stage renal failure, at 15 every other day (or 7.5 mg/day) in patients with GFR <30 ml/min and at 10 mg/day in those with GFR 30–50 ml/min [11, 14]. Ixazomib should be used at a dose of 3 mg/week in patients with creatinine clearance of <30 ml/min [34, 35]. Pomalidomide can be administered without dose reduction to patients with moderate and severe renal impairment [82].
Cardiac and vascular toxicities
Cardiac toxicity has been reported with IMiDs and PIs. Carfilzomib is associated with a higher risk for cardiotoxic adverse events, including hypertension, shortly after drug infusion. The exact mechanism has not yet been clarified, but an effect of carfilzomib on endothelial cells and a common acute rise in NT-proBNP has been reported [83]. A decline in ejection fraction in few patients was shown [83, 84]. In the ENDEAVOR study, events of heart failure and pulmonary hypertension were more frequently reported in Kd versus Vd patients and similar findings were also reported in the CLARION study comparing KMP with VMP [85]. Reported reductions in left ventricular ejection fraction were mostly reversible. The utility of echocardiography as a tool to identify patients at risk of reduced left or right ventricular function was found to be limited in patients receiving carfilzomib [86].
Important cardiopulmonary risk factors and recommendations for patient monitoring, as well as the prevention and management of such events are shown in Table 7. Patients with pre-existing cardiac disease and those aged 75 years or older are at higher risk for carfilzomib-induced cardiac toxicity. They should be subjected to a comprehensive medical assessment prior to carfilzomib initiation [32, 33, 87]. Before administration of carfilzomib, their blood pressure should be tightly controlled and should not exceed systolic levels above 140 mm Hg. In addition, adherence to 30-min infusion time is recommended. Shortening the infusion time to 10 min after 1–2 cycles can be considered, if there were no cardiac or pulmonary symptoms [88]. In case of grade 3 or 4 cardiac events, carfilzomib should be interrupted until recovery. Carfilzomib may be restarted at reduced dose after a thorough benefit/risk assessment [32, 33] and the patient should be assessed for fluid overload [87, 88]. A cardiologist should be involved to address the clinical issue [87, 88]. Currently, a clear dose effect of cardiac toxicity has not been demonstrated, but it seems prudent to start with a lower dose in elderly patients (aged >75 years) and in those with a history of mild cardiac disease. Patients with more severe heart disease have been excluded from clinical studies.
Infusion-related reactions
Both approved monoclonal antibodies, elotuzumab and daratumumab, are of IgG1κ isotype, the former being humanized and the latter being fully human. In spite of their similarity with human IgG, treatment with these antibodies may results in infusion reactions that mostly are seen during the first and less so during following infusions. Lonial et al. reported infusion-related AEs in only 10% of patients receiving 20 mg/kg of elotuzumab, all of grade 1 or 2 [89]. Single-agent daratumumab resulted in higher rates of infusion-related AEs of 45% as reported in a phase II study, with only few being classified as grade 3 [90].
For both drugs, prophylactic measures are recommended. Forty-five to 90 min before start of elotuzumab infusion, dexamethasone (8 mg, IV), diphenhydramine (25–50 mg orally or IV) or equivalent, ranitidine (50 mg IV or 150 mg orally) or equivalent, and paracetamol/acetaminophen (650–1000 mg orally) should be administered. A similar regimen should be used ~1 h before daratumumab infusion, consisting of 100 mg of IV methylprednisolone or equivalent (may be reduced to 60 mg thereafter), oral antipyretic (paracetamol 650–1000 mg), oral or IV antihistamine (diphenhydramine 25–50 mg) or equivalent. All patients should receive post-infusion treatment with 20 mg methylprednisolone or equivalent on each of the 2 days following infusion. Special precautions need to be taken in patients with pre-existing chronic obstructive pulmonary disease (COPD). Premedication with 10 mg montelukast, an oral leukotriene receptor antagonist, 30 min before daratumumab should be considered as well as post-infusion therapy with short- and long-term bronchodilators and inhaled corticosteroids; patients with COPD stage IV disease should be excluded from daratumumab therapy [91]. An early report showed that an SC preparation of daratumumab can be safely administered within 30 min with a significantly lower rate of daratumumab-related IRRs [92]. Details of dilution volume of the drugs, infusion rates, increments in rates, and maximum speed are listed in Table 8.
In case of occurrence of infusion-related AEs of grade ≥2 during elotuzumab infusion, the infusion must be interrupted and can be restarted at lower infusion rate (0.5 ml/min) with gradual increase by 0.5 ml/min every 30 min as tolerated to the rate at which the IRR occurred. If this is well tolerated, escalation of the infusion rate can be resumed. Patients with a grade ≥3 IRR may require emergency treatment and permanent discontinuation. A similar procedure is recommended for daratumumab-induced IRR. The infusion should be interrupted at any grade/severity. If grade 1–2 IRR occurs, the infusion may be resumed at half the rate at which it occurred, provided the patient is stabilized; in case of no recurrence of IRR, escalation can be resumed. If grade 3 IRR occurs, once IRR decreases to grade ≤2, the infusion may be restarted at no more than half the rate at which the IRR occurred. If no recurrence of IRR, escalation can be resumed. Patients have to discontinue daratumumab therapy in case of grade 4 (life threatening) IRRs at first or subsequent infusion.
Teratogenicity
Almost all novel agents and backbone agents showed a certain embryo-fetal risk, especially the thalidomide analogs of the IMiD group (Table 1 and S2A). Pregnancy must be excluded before start of treatment. Women of reproductive potential and their partners should be informed about the embryo-fetal risk of the respective drugs and about adequate contraceptive measures. To prevent pregnancy, continuous abstinence from heterosexual intercourse or two reliable methods of contraception must be used. The respective USPIs and EU SmPCs have detailed instructions suited to the agents used.
Conclusions
A number of novel drugs have recently been introduced in the treatment of multiple myeloma. These drugs differ in their mode of action and their side effect and safety profile. Knowledge of their potential risks and of established measures to prevent occurrence of complications is essential for preventing severe symptoms, dose reductions, and/or treatment discontinuations and in some patients even mortality. In case of emergence of drug reactions, optimal management is key for optimizing treatment outcome.
References
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Multiple Myeloma. Version 1.2018. 2017. https://www.nccn.org/professionals/physician_gls/pdf/myeloma_blocks.pdf. Accessed 03 Oct 2017.
International conference on harmonization of technical requirements for registration of pharmaceuticals for human use. Clinical safety data management: definitions and standards for expedited reporting. E2A. 1994. http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E2A/Step4/E2A_Guideline.pdf. Accessed 5 Dec 2016.
Palumbo A, Rajkumar SV, San Miguel JF, Larocca A, Niesvizky R, Morgan G, et al. International Myeloma Working Group consensus statement for the management, treatment, and supportive care of patients with myeloma not eligible for standard autologous stem-cell transplantation. J Clin Oncol. 2014;32:587–600.
Ludwig H, Miguel JS, Dimopoulos MA, Palumbo A, Garcia Sanz R, Powles R, et al. International Myeloma Working Group recommendations for global myeloma care. Leukemia. 2014;28:981–92.
Cavo M, Rajkumar SV, Palumbo A, Moreau P, Orlowski R, Blade J, et al. International Myeloma Working Group consensus approach to the treatment of multiple myeloma patients who are candidates for autologous stem cell transplantation. Blood. 2011;117:6063–73.
Terpos E, Kleber M, Engelhardt M, Zweegman S, Gay F, Kastritis E, et al. European Myeloma Network guidelines for the management of multiple myeloma-related complications. Haematologica. 2015;100:1254–66.
National Comprehensive Cancer Network. Prevention and treatment of cancer-related infections. Version 1.2018. December 1. 2017. https://www.nccn.org/professionals/physician_gls/pdf/infections.pdf. Accessed 11. February 2018.
Snowden JA, Ahmedzai SH, Ashcroft J, D’Sa S, Littlewood T, Low E, et al. Guidelines for supportive care in multiple myeloma 2011. Br J Haematol. 2011;154:76–103.
Dispenzieri A, Lacy MQ, Greipp PR. Multiple myeloma. In: Gertz MA, Greipp PR, editors. Hematologic malignancies: multiple myeloma and related plasma cell disorders. Berlin Heidelberg: Springer-Verlag; 2004. p. 55–109.
European Medicines Agency. Thalidomide celgene: EPAR - product information. 2015. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000823/WC500037050.pdf. Accessed 10 Nov 2016.
European Medicines Agency. Revlimid: EPAR - product information. 2017. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000717/WC500056018.pdf. Accessed 03 Oct 2017.
European Medicines Agency. Imnovid: EPAR - product information. 2017. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000717/WC500056018.pdf. Accessed 03 Oct 2017.
United States Food and Drug Administration. Thalidomide celgene: label information. 2015. http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/020785s051lbl.pdf. Accessed 10 Nov 2016.
United States Food and Drug Administration. Revlimid: label information. 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/021880s051lbl.pdf. Accessed 03 Oct 2017.
United States Food and Drug Administration. Pomalyst: label information. 2016. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/204026s012s014lbl.pdf. Accessed 03 Oct 2017.
Johnson DC, Corthals SL, Walker BA, Ross FM, Gregory WM, Dickens NJ, et al. Genetic factors underlying the risk of thalidomide-related neuropathy in patients with multiple myeloma. J Clin Oncol. 2011;29:797–804.
Glasmacher A, Hahn C, Hoffmann F, Naumann R, Goldschmidt H, von Lilienfeld-Toal M, et al. A systematic review of phase-II trials of thalidomide monotherapy in patients with relapsed or refractory multiple myeloma. Br J Haematol. 2006;132:584–93.
Kapoor P, Rajkumar SV, Dispenzieri A, Gertz MA, Lacy MQ, Dingli D, et al. Melphalan and prednisone versus melphalan, prednisone and thalidomide for elderly and/or transplant ineligible patients with multiple myeloma: a meta-analysis. Leukemia. 2011;25:689–96.
Palumbo A, Waage A, Hulin C, Beksac M, Zweegman S, Gay F, et al. Safety of thalidomide in newly diagnosed elderly myeloma patients: a meta-analysis of data from individual patients in six randomized trials. Haematologica. 2013;98:87–94.
Mateos MV. Management of treatment-related adverse events in patients with multiple myeloma. Cancer Treat Rev. 2010;36:S24–32.
Benboubker L, Dimopoulos MA, Dispenzieri A, Catalano J, Belch AR, Cavo M, et al. Lenalidomide and dexamethasone in transplant-ineligible patients with myeloma. N Engl J Med. 2014;371:906–17.
Pawlyn C, Khan MS, Muls A, Sriskandarajah P, Kaiser MF, Davies FE, et al. Lenalidomide-induced diarrhea in patients with myeloma is caused by bile acid malabsorption that responds to treatment. Blood. 2014;124:2467–8.
Palumbo A, Hajek R, Delforge M, Kropff M, Petrucci MT, Catalano J, et al. Continuous lenalidomide treatment for newly diagnosed multiple myeloma. N Engl J Med. 2012;366:1759–69.
Attal M, Lauwers-Cances V, Marit G, Caillot D, Moreau P, Facon T, et al. Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. N Engl J Med. 2012;366:1782–91.
McCarthy PL, Owzar K, Hofmeister CC, Hurd DD, Hassoun H, Richardson PG, et al. Lenalidomide after stem-cell transplantation for multiple myeloma. N Engl J Med. 2012;366:1770–81.
Usmani SZ, Sexton R, Hoering A, Heuck CJ, Nair B, Waheed S, et al. Second malignancies in total therapy 2 and 3 for newly diagnosed multiple myeloma: influence of thalidomide and lenalidomide during maintenance. Blood. 2012;120:1597–1600.
Palumbo A, Bringhen S, Kumar SK, Lupparelli G, Usmani S, Waage A, et al. Second primary malignancies with lenalidomide therapy for newly diagnosed myeloma: a meta-analysis of individual patient data. Lancet Oncol. 2014;15:333–42.
Jones JR, Cairns DA, Gregory WM, Collett C, Pawlyn C, Sigsworth R, et al. Second malignancies in the context of lenalidomide treatment: an analysis of 2732 myeloma patients enrolled to the Myeloma XI trial. Blood Cancer J. 2016;6:e506.
Chen N, Zhou S, Palmisano M. Clinical pharmacokinetics and pharmacodynamics of lenalidomide. Clin Pharmacokinet. 2017;56:139–52.
European Medicines Agency. Velcade: EPAR - product information. 2016. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000539/WC500048471.pdf. Accessed 3 Dec 2016.
United States Food and Drug Administration. Velcade: label information. 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/021602s043lbl.pdf. Accessed 03 Oct 2017.
European Medicines Agency. Kyprolis: EPAR - product information. 2017. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003790/WC500197692.pdf. Accessed 03 Oct 2017.
United States Food and Drug Administration. Kyprolis: label information. 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/202714s016lbl.pdf. Accessed 03 Oct 2017.
United States Food and Drug Administration. Ninlaro: label information. 2016. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/208462s001lbl.pdf. Accessed 03 Oct 2017.
European Medicines Agency. Ninlaro: EPAR - product information. 2017. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003844/WC500217620.pdf. Accessed 03 Oct 2017.
San-Miguel JF, Hungria VT, Yoon SS, Beksac M, Dimopoulos MA, Elghandour A, et al. Panobinostat plus bortezomib and dexamethasone versus placebo plus bortezomib and dexamethasone in patients with relapsed or relapsed and refractory multiple myeloma: a multicentre, randomised, double-blind phase 3 trial. Lancet Oncol. 2014;15:1195–206.
European Medicines Agency. Farydak: EPAR - product information. 2017. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003725/WC500193298.pdf. Accessed 03 Oct 2017.
United States Food and Drug Administration. Farydak: label information. 2015. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/205353s000lbl.pdf. Accessed 03 Oct 2017.
European Medicines Agency. Empliciti: EPAR - product information. 2017. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003967/WC500206673.pdf. Accessed 3 Oct 2017.
United States Food and Drug Administration. Empliciti: label information. 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761035s005lbl.pdf. Accessed 03 Oct 2017.
European Medicines Agency. Darzalex: EPAR - product information. 2016. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/004077/WC500207296.pdf. Accessed 5 Dec 2016.
United States Food and Drug Administration. Darzalex: label information. 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761036s005lbl.pdf. Accessed 03 Oct 2017.
van de Donk NW, Otten HG, El Haddad O, Axel A, Sasser AK, Croockewit S, et al. Interference of daratumumab in monitoring multiple myeloma patients using serum immunofixation electrophoresis can be abrogated using the daratumumab IFE reflex assay (DIRA). Clin Chem Lab Med. 2016;54:1105–9.
Flores-Montero J, Sanoja-Flores L, Paiva B, Puig N, Garcia-Sanchez O, Bottcher S, et al. Next generation flow for highly sensitive and standardized detection of minimal residual disease in multiple myeloma. Leukemia. 2017;31:2094–103.
De Stefano V, Za T, Rossi E. Venous thromboembolism in multiple myeloma. Semin Thromb Hemost. 2014;40:338–47.
Palumbo A, Rajkumar SV, Dimopoulos MA, Richardson PG, San Miguel J, Barlogie B, et al. Prevention of thalidomide- and lenalidomide-associated thrombosis in myeloma. Leukemia. 2008;22:414–23.
Nagge J, Crowther M, Hirsh J. Is impaired renal function a contraindication to the use of low-molecular-weight heparin? Arch Intern Med. 2002;162:2605–9.
ten Cate-Hoek AJ, Weitz JI, Gailani D, Meijer K, Philippou H, Bouman AC, et al. Theme 3: Non-invasive management of (recurrent) venous thromboembolism (VTE) and post thrombotic syndrome (PTS). Thromb Res. 2015;136:S13–18.
Delforge M, Blade J, Dimopoulos MA, Facon T, Kropff M, Ludwig H, et al. Treatment-related peripheral neuropathy in multiple myeloma: the challenge continues. Lancet Oncol. 2010;11:1086–95.
Siegel DS, Martin T, Wang M, Vij R, Jakubowiak AJ, Lonial S, et al. A phase 2 study of single-agent carfilzomib (PX-171-003-A1) in patients with relapsed and refractory multiple myeloma. Blood. 2012;120:2817–25.
Arastu-Kapur S, Anderl JL, Kraus M, Parlati F, Shenk KD, Lee SJ, et al. Nonproteasomal targets of the proteasome inhibitors bortezomib and carfilzomib: a link to clinical adverse events. Clin Cancer Res. 2011;17:2734–43.
Kelly JJ. The evaluation of peripheral neuropathy. Part I: clinical and laboratory evidence. Rev Neurol Dis. 2004;1:133–40.
Park SB, Goldstein D, Krishnan AV, Lin CS, Friedlander ML, Cassidy J, et al. Chemotherapy-induced peripheral neurotoxicity: a critical analysis. CA Cancer J Clin. 2013;63:419–37.
Richardson PG, Delforge M, Beksac M, Wen P, Jongen JL, Sezer O, et al. Management of treatment-emergent peripheral neuropathy in multiple myeloma. Leukemia. 2012;26:595–608.
Moreau P, Pylypenko H, Grosicki S, Karamanesht I, Leleu X, Grishunina M, et al. Subcutaneous versus intravenous administration of bortezomib in patients with relapsed multiple myeloma: a randomised, phase 3, non-inferiority study. Lancet Oncol. 2011;12:431–40.
World Health Organization. WHO’s cancer pain ladder for adults. 2016. http://www.who.int/cancer/palliative/painladder/en/. Accessed 20 Dec 2016.
Stacey BR. Management of peripheral neuropathic pain. Am J Phys Med Rehabil. 2005;84:S4–16.
Krone A, Reuther P, Fuhrmeister U. Autonomic dysfunction in polyneuropathies: a report on 106 cases. J Neurol. 1983;230:111–21.
Lee WS, Kim DH, Shin SH, Woo SI, Kwan J, Park KS, et al. Complete atrioventricular block secondary to bortezomib use in multiple myeloma. Yonsei Med J. 2011;52:196–8.
Figueroa JJ, Basford JR, Low PA. Preventing and treating orthostatic hypotension: as easy as A, B, C. Cleve Clin J Med. 2010;77:298–306.
Basler M, Lauer C, Beck U, Groettrup M. The proteasome inhibitor bortezomib enhances the susceptibility to viral infection. J Immunol. 2009;183:6145–50.
Advisory Committee for Immunization Practices. Vaccine-specific recommendations. 2016. https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/. Accessed 30 Dec 2016.
The University of Hong Kong. VZV vaccine for hematopoietic stem cell transplantation (VZIDST). 2015. https://clinicaltrials.gov/ct2/show/study/NCT02329457. Accessed 30 Dec 2016.
Stadtmauer EA, Sullivan KM, Marty FM, Dadwal SS, Papanicolaou GA, Shea TC, et al. A phase 1/2 study of an adjuvanted varicella-zoster virus subunit vaccine in autologous hematopoietic cell transplant recipients. Blood. 2014;124:2921–9.
Hata A, Asanuma H, Rinki M, Sharp M, Wong RM, Blume K, et al. Use of an inactivated varicella vaccine in recipients of hematopoietic-cell transplants. N Engl J Med. 2002;347:26–34.
Redman RL, Nader S, Zerboni L, Liu C, Wong RM, Brown BW, et al. Early reconstitution of immunity and decreased severity of herpes zoster in bone marrow transplant recipients immunized with inactivated varicella vaccine. J Infect Dis. 1997;176:578–85.
Hahn M, Schnitzler P, Schweiger B, Kunz C, Ho AD, Goldschmidt H, et al. Efficacy of single versus boost vaccination against influenza virus in patients with multiple myeloma. Haematologica. 2015;100:e285–288.
Teng CJ, Liu HT, Liu CY, Hsih CH, Pai JT, Gau JP, et al. Chronic hepatitis virus infection in patients with multiple myeloma: clinical characteristics and outcomes. Clinics. 2011;66:2055–61.
Sampathkumar P, Drage LA, Martin DP. Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc. 2009;84:274–80.
MacFarlane LL, Simmons MM, Hunter MH. The use of corticosteroids in the management of herpes zoster. J Am Board Fam Pract. 1998;11:224–8.
Sandherr M, Hentrich M, von Lilienfeld-Toal M, Massenkeil G, Neumann S, Penack O, et al. Antiviral prophylaxis in patients with solid tumours and haematological malignancies--update of the Guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society for Hematology and Medical Oncology (DGHO). Ann Hematol. 2015;94:1441–50.
Blimark C, Holmberg E, Mellqvist UH, Landgren O, Bjorkholm M, Hultcrantz M, et al. Multiple myeloma and infections: a population-based study on 9253 multiple myeloma patients. Haematologica. 2015;100:107–13.
Teh BW, Harrison SJ, Worth LJ, Spelman T, Thursky KA, Slavin MA. Risks, severity and timing of infections in patients with multiple myeloma: a longitudinal cohort study in the era of immunomodulatory drug therapy. Br J Haematol. 2015;171:100–8.
Stewart AK, Rajkumar SV, Dimopoulos MA, Masszi T, Spicka I, Oriol A, et al. Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma. N Engl J Med. 2015;372:142–52.
Chapel HM, Lee M, Hargreaves R, Pamphilon DH, Prentice AG. Randomised trial of intravenous immunoglobulin as prophylaxis against infection in plateau-phase multiple myeloma. The UK Group for immunoglobulin replacement therapy in multiple myeloma. Lancet. 1994;343:1059–63.
Raanani P, Gafter-Gvili A, Paul M, Ben-Bassat I, Leibovici L, Shpilberg O. Immunoglobulin prophylaxis in chronic lymphocytic leukemia and multiple myeloma: systematic review and meta-analysis. Leuk Lymphoma. 2009;50:764–72.
van de Donk NW, Gorgun G, Groen RW, Jakubikova J, Mitsiades CS, Hideshima T, et al. Lenalidomide for the treatment of relapsed and refractory multiple myeloma. Cancer Manag Res. 2012;4:253–68.
Lee MJ, Wickner P, Fanning L, Schlossman R, Richardson P, Laubach J, et al. Lenalidomide desensitization for delayed hypersensitivity reactions in 5 patients with multiple myeloma. Br J Haematol. 2014;167:127–31.
Westergaard H. Bile Acid malabsorption. Curr Treat Options Gastroenterol. 2007;10:28–33.
Andreyev HJ, Davidson SE, Gillespie C, Allum WH, Swarbrick E, British Society of G et al. Practice guidance on the management of acute and chronic gastrointestinal problems arising as a result of treatment for cancer. Gut. 2012;61:179–92.
Benson AB 3rd, Ajani JA, Catalano RB, Engelking C, Kornblau SM, Martenson JA Jr., et al. Recommended guidelines for the treatment of cancer treatment-induced diarrhea. J Clin Oncol. 2004;22:2918–26.
Siegel DS, Weisel KC, Dimopoulos MA, Baz R, Richardson P, Delforge M, et al. Pomalidomide plus low-dose dexamethasone in patients with relapsed/refractory multiple myeloma and moderate renal impairment: a pooled analysis of three clinical trials. Leuk Lymphoma. 2016;57:2833–8.
Rosenthal A, Luthi J, Belohlavek M, Kortum KM, Mookadam F, Mayo A, et al. Carfilzomib and the cardiorenal system in myeloma: an endothelial effect? Blood Cancer J. 2016;6:e384.
Dimopoulos MA, Roussou M, Gavriatopoulou M, Psimenou E, Ziogas D, Eleutherakis-Papaiakovou E, et al. Cardiac and renal complications of carfilzomib in patients with multiple myeloma. Blood Adv. 2017;1:449–54.
Facon T, Lee JH, Moreau P, Niesvizky R, Dimopoulos MA, Hajek R, et al. Phase 3 study (CLARION) of carfilzomib, melphalan, prednisone (KMP) v bortezomib, melphalan, prednisone (VMP) in newly diagnosed multiple myeloma (NDMM). 16th International Myeloma Workshop: New Delhi; 2017. p. OP-044.
Russell SD, Lyon A, Lenihan DJ, Moreau P, Joshua D, Chng W-J, et al. Serial echocardiographic assessment of patients (Pts) with relapsed multiple myeloma (RMM) receiving carfilzomib and dexamethasone (Kd) vs bortezomib and dexamethasone (Vd): a Substudy of the phase 3 Endeavor trial (NCT01568866). Blood. 2015;126: abstract 4250.
Jakubowiak AJ, DeCara JM, Mezzi K. Cardiovascular events during carfilzomib therapy for relapsed myeloma: practical management aspects from two case studies. Hematology. 2017;22:585–91.
Mikhael J. Management of carfilzomib-associated cardiac adverse events. Clin Lymphoma Myeloma Leuk. 2016;16:241–5.
Lonial S, Dimopoulos M, Palumbo A, White D, Grosicki S, Spicka I, et al. Elotuzumab Therapy for Relapsed or Refractory Multiple Myeloma. N Engl J Med. 2015;373:621–31.
Lonial S, Weiss BM, Usmani SZ, Singhal S, Chari A, Bahlis NJ, et al. Daratumumab monotherapy in patients with treatment-refractory multiple myeloma (SIRIUS): an open-label, randomised, phase 2 trial. Lancet. 2016;387:1551–60.
Chari A, Mark TM, Krishnan A, Stockerl-Goldstein K, Usmani SZ, Londhe A, et al. Use of montelukast to reduce infusion reactions in an early access treatment protocol of daratumumab in United States Patients with relapsed or refractory multiple myeloma. ASH: San Diego; 2016. abstract 2142.
Usmani SZ, Nahi H, Mateos M-V, Lokhorst HM, Chari A, Kaufman JL, et al. Open-label, multicenter, dose escalation phase 1b study to assess the subcutaneous delivery of daratumumab in patients (pts) with relapsed or refractory multiple myeloma (PAVO). ASH: San Diego, CA; 2016. abstract 1149.
Tomblyn M, Chiller T, Einsele H, Gress R, Sepkowitz K, Storek J, et al. Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: a global perspective. Biol Blood Marrow Transplant. 2009;15:1143–238.
Cheuk DK, Chiang AK, Lee TL, Chan GC, Ha SY. Vaccines for prophylaxis of viral infections in patients with hematological malignancies. Cochrane Database Syst Rev. 2011; CD006505.
Boehmer LM, Waqar SN, Govindan R. Influenza vaccination in patients with cancer: an overview. Oncology. 2010;24:1167–70.
Chlibek R, Bayas JM, Collins H, de la Pinta ML, Ledent E, Mols JF, et al. Safety and immunogenicity of an AS01-adjuvanted varicella-zoster virus subunit candidate vaccine against herpes zoster in adults>=50 years of age. J Infect Dis. 2013;208:1953–61.
Mallet V, van Bommel F, Doerig C, Pischke S, Hermine O, Locasciulli A, et al. Management of viral hepatitis in patients with haematological malignancy and in patients undergoing haemopoietic stem cell transplantation: recommendations of the 5th European Conference on Infections in Leukaemia (ECIL-5). Lancet Infect Dis. 2016;16: 606–17.
Wanchoo R, Abudayyeh A, Doshi M, Edeani A, Glezerman IG, Monga D, et al. Renal toxicities of novel agents used for treatment of multiple myeloma. Clin J Am Soc Nephrol. 2017;12:176–89.
Acknowledgements
We wish to acknowledge the support of Dr. Margit Hemetsberger in literature search, data collection, and support in the creation of the manuscript, and the Austrian Forum against Cancer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HL has received speakers’ honoraria from Celgene, Amgen, Takeda, Janssen, and Bristol-Myers Squibb, and research funding from Takeda and Amgen, as well as consultancy fees from Amgen, Takeda, and Janssen. MD has received speakers’ honoraria and consultancy fees from Amgen, Takeda, Janssen, Celgene, and Bristol-Myers Squibb, as well as research support from Celgene and Janssen. TF has received speakers’ honoraria and honoraria for participation in advisory boards from Celgene, Janssen, Takeda, Amgen, and PharmaMar. HE has received speakers’ honoraria and honoraria for participation in advisory boards for Celgene, Janssen, Amgen, Bristol-Myers Squibb, and Novartis, and consultancy fees or honoraria from Celgene, Janssen, Bristol-Myers Squibb, and Amgen. FG has received honoraria from Amgen, Bristol-Myers Squibb, Celgene, and Takeda, and honoraria for participation in advisory boards from Janssen, Amgen, Celgene, Roche, and Takeda. PM has received honoraria from Novartis, Janssen, Celgene, Millennium, Onyx, and Bristol-Myers Squibb, and consultancy fees from Novartis, Janssen, Celgene, Millennium, and Onyx. HA-L has received honoraria for participation in advisory boards from Celgene, Janssen, Amgen, and Sanofi, and research funding from Celgene and Sanofi. RH has received consultancy fees, research funding, and honoraria for participation in advisory boards from Amgen, Takeda, Bristol-Myers Squibb, Celgene, Novartis, and Janssen. MM has received honoraria and research funding from Janssen, Celgene, Amgen, Takeda, Novartis, and Bristol-Myers Squibb. MC has received consultancy fees from Janssen, Celgene, Amgen, and Bristol-Myers Squibb, speakers’ honoraria from Janssen, Celgene, Amgen, and Takeda, honoraria for participation in advisory boards from Janssen, Celgene, Takeda, Amgen, and Bristol-Myers Squibb, as well as honoraria from Janssen, Celgene, Bristol-Myers Squibb, Amgen, Novartis, and Takeda. MAD has received consultancy fees and honoraria from Celgene, Onyx, Janssen, Novartis, and Amgen, and honoraria for participation in advisory boards from Amgen, Takeda, Celgene, and Janssen. JS-M has received speaker’s honoraria and consultancy fees from Takeda, Celgene, Novartis, Amgen, Janssen, Bristol-Myers Squibb, Sanofi, and MSD. ET has received honoraria from Janssen, Amgen, Takeda, Abbvie, Bristol-Myers Squibb, PharmaMar, and Celgene, research funding from Amgen, Genesis, Janssen, Novartis, and Takeda, honoraria for participation in advisory boards from Takeda, as well as honoraria for participation in the data monitoring committee from Celgene. SZ has received honoraria for participating in advisory boards and research funding from Janssen, Celgene, Novartis, and Takeda. M-VM has has received personal fees from Janssen, Celgene, BMS, Amgen, and Takeda. GC has received consultancy fees and research funding from Janssen, Celgene, Takeda, Sanofi, Amgen, and Bristol-Myers Squibb. XL has received honoraria for participating in advisory boards and honoraria from Celgene, Janssen, Takeda, Amgen, Novartis, Sanofi, BMS, Merck, Pierre Fabre, and Gilead. HG has received research funding and honoraria from Celgene, Chugai, Novartis, Janssen, and Bristol-Myers Squibb, and honoraria for participating in advisory boards from Janssen, Celgene, Novartis, Amgen, Takeda, and Bristol-Myers Squibb. GJ has received speakers’ honoraria and honoraria for participating in advisory boards from Takeda, Celgene, Janssen, Amgen, and Roche, and research funding from Onyx, Celgene, and CRUK. MK received research funding from Celgene, and honoraria for participating in advisory boards from Takeda, Celgene, Amgen, Janssen, and Bristol-Myers Squibb. KW has received honoraria from Novartis, Janssen, Celgene, Amgen, Onyx, Takeda, and Bristol-Myers Squibb, and consultancy fees from Janssen, Celgene, Amgen, Bristol-Myers Squibb, Takeda, and Onyx. NvdD has received research funding and honoraria for participating in advisory boards from Janssen, Celgene, Bristol-Myers Squibb, and Amgen. AW has received research support from Amgen and Celgene, and honoraria for participation in advisory boards from Amgen, Celgene, and Takeda. MB has received honoraria for participating in advisory boards from Novartis, Amgen, Celgene, and Janssen, and speakers’ honoraria from Amgen, Celgene, and Janssen. U-HM has received honoraria for participating in advisory boards from Amgen and Takeda, and honoraria from Amgen, Celgene, Takeda, Mundipharma, Janssen, and Novartis. PS has received honoraria for participating in advisory boards and honoraria from Celgene, Janssen, Amgen, Karyopharm, and Takeda. MB, JC, CD, ME, and LG declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. If you remix, transform, or build upon this article or a part thereof, you must distribute your contributions under the same license as the original. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/.
About this article
Cite this article
Ludwig, H., Delforge, M., Facon, T. et al. Prevention and management of adverse events of novel agents in multiple myeloma: a consensus of the European Myeloma Network. Leukemia 32, 1542–1560 (2018). https://doi.org/10.1038/s41375-018-0040-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-018-0040-1
This article is cited by
-
Reporting of adverse events of treatment interventions in multiple myeloma: an overview of systematic reviews
Annals of Hematology (2023)
-
Management of herpesvirus reactivations in patients with solid tumours and hematologic malignancies: update of the Guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society for Hematology and Medical Oncology (DGHO) on herpes simplex virus type 1, herpes simplex virus type 2, and varicella zoster virus
Annals of Hematology (2022)
-
Pegfilgrastim for primary prophylaxis of febrile neutropenia in multiple myeloma
Supportive Care in Cancer (2021)
-
Improved survival in multiple myeloma during the 2005–2009 and 2010–2014 periods
Leukemia (2021)
-
COVID-19 in persons with haematological cancers
Leukemia (2020)