Abstract
The efficacy of the antibody drug conjugate (ADC) Trastuzumab deruxtecan (T-DXd) in HER2 low breast cancer patients suggests that the historical/conventional assays for HER2 may need revision for optimal patient care. Specifically, the conventional assay is designed to distinguish amplified HER2 from unamplified cases but is not sensitive enough to stratify the lower ranges of HER2 expression. Here we determine the optimal dynamic range for unamplified HER2 detection in breast cancer and then redesign an assay to increase the resolution of the assay to stratify HER2 expression in unamplified cases. We used the AQUA™ method of quantitative immunofluorescence to test a range of antibody concentrations to maximize the sensitivity within the lower range of HER2 expression. Then, using a cell line microarray with HER2 protein measured by mass spectrometry we determined the amount of HER2 protein in units of attomols/mm2. Then by calculation of the limits of detection, quantification, and linearity of this assay we determined that low HER2 range expression in unamplified cell lines is between 2 and 20 attomol/mm2. Finally, application of this assay to a serial collection of 364 breast cancer cases from Yale shows 67% of the population has HER2 expression above the limit of quantification and below the levels seen in HER2 amplified breast cancer. In the future, this assay could be used to determine the levels of HER2 required for response to T-DXd or similar HER2 conjugated ADCs.
Similar content being viewed by others
Introduction
Only about 15 percent of women diagnosed with breast cancer are human epidermal growth factor receptor 2 (HER2) “positive”, or ERBB2 gene amplified, and eligible for anti-HER2 therapy1. Recently, a series of HER2-targeted therapies have been FDA approved, in addition to trastuzumab2, pertuzumab3, and lapatinib4, which have significantly improved clinical outcomes for HER2-positive breast cancer patients5,6,7,8,9. However, all of these HER2 targeting therapies only show efficacy in patients with tumors with HER2 (ERBB2) gene amplification as defined by immunohistochemical (IHC) stain of 3+ or a HER2/chromosome enumeration probe 17 (CEP17) fluorescent in situ hybridization (FISH) amplification ratio ≥2.0 and HER2 copy number signals/cell ≥410. Thus, the majority of breast cancer patients (85%) are considered HER2 “negative” (IHC 0 or IHC 1+ or IHC 2+ and FISH−)11 although they express HER2 at the low levels comparable to that seen in normal breast ductal cells.
The paradigm of HER2 amplification tightly linked to therapy efficacy is changing. Activity of trastuzumab deruxtecan (T-DXd), a novel HER2-targeted antibody drug conjugate (ADC)12, is seen in patients with HERE2 IHC scores of 1+ and 2+ (unamplified)13. However, due to the design of currently used HER2 assays (designed to distinguish HER2 amplified from unamplified tumors) the scoring accuracy for HER2 IHC in the low range (0 and 1+) has been shown to be poor, with less than 70% interrater agreement on 15 of 80 College of American Pathologists Proficiency Testing survey cases14. This is most likely due to the very weak staining of tumors with HER2 protein in the low expression range of normal breast epithelial cells. HER2 has a broad range of expression in tumors from around 1000 molecules to over 1,000,000 molecules/cell in some studies15,16. Very few assays have sufficient dynamic range to span this 3-log difference in expression level. For example, chromogenic IHC generally has less than one log of linear dynamic range. Thus, to accurately assess HER2 protein expression in breast cancer requires either more than one assay with the use of more than one antibody concentration17 or an assay with 3 log dynamic range.
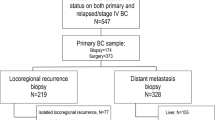
While it might be valuable to have an assay that spans the full dynamic range of HER2 expression, the existing assays for HER2 that distinguish amplified from unamplified HER2 are “fit for purpose” and effective for trastuzumab and other drugs that target amplified HER2. However, since the low range of expression is missed by these assays, we set out to build a new assay with resolution in the low range. While this might be possible with a chromogenic assay, here we use quantitative immunofluorescence coupled with a mass spectrometry standardized HER2 array to generate an assay that can measure absolute amounts of HER2 protein in attomol/mm2 on conventional histology sections. An overview of the assay development is shown in Fig. 1. Our goal was to develop an assay specific to low HER2 expression and then to determine the prevalence of low-level expression in each specimen from a serial, retrospective collection of breast cancer cases.
Cell lines with a range of HER2 expression, as quantified by LC-MS/MS are used to generate a cell microarray (CMA) standard. Determination of the cell area in mm2, allows the transformation of the HER2 expression from amol/ug of total protein to amol/mm2. The CMA is stained using different primary anti-HER2 antibody concentrations and the Limit of Detection (LOD)/ Limit of quantification (LOQ) and Limit of Linearity (LOL) are identified. Linear regression analysis between AQUA Score and amol/mm2 allows for the generation of a standard curve that can be used to calculate HER2 expression in amol/mm2 on a tissue area basis. Breast cancer tissue is stained and analyzed by AQUA. After analysis, HER2 expression/case is quantified by amol/mm2. Liquid Chromatography (LC) with tandem mass spectrometry, LC-MS/MS; Cell MicroArray, CMA; Tissue MicroArray, TMA; Immunofluorescence, IF; Automated Quantitative Analysis, AQUA; Cytokeratin, CK.
Materials and methods
Cell lines and culture conditions
A set of 7 cell lines were obtained from American Type Culture Collection (ATCC, Manassas, VA 20110, USA) including: JURKAT #TIB-152, BT20 #HTB-19, T47D #HTB-133, ZR-75-1 #CRL-1500, BT483 #HTB-121, AU565 #CRL-2351, and BT474 #HTB-20. Each cell line was cultured in accordance with the culture method provided by ATCC. Pellets from these cell lines were produced, frozen, and shipped to Protypia for measurement of the expression of HER2 in attomoles (amol)/µg of total protein.
Liquid chromatography-tandem mass spectrometry (LC-MS/MS)
Protein abundance of HER2 in the 7 cell lines was analyzed by LC-MS/MS at Protypia, Inc, Nashville, TN, USA. Protein was extracted from frozen cell pellets with the M-PERTM reagent (ThermoFisher Scientific, Rockford, IL) supplemented with HALTTM protease inhibitor cocktail (ThermoFisher Scientific) according to the manufacturer’s directions. Protein content was analyzed with the BCA reagent (ThermoFisher Scientific) and 100 μg protein was reduced, alkylated, and digested with trypsin as described previously18. Standards of the HER2 peptides [13C6,15N4-Arg]-DPPFCVAR and [13C6,15N4-Arg]-ELVSEFSR (99.5% isotopic purity; Vivitide, Gardner, MA) were added to the tryptic digest, which was fractionated by high pH reverse phase chromatography with disposable spin columns (ThermoFisher Scientific). Fractions containing the target peptides were analyzed by LC-MS/MS parallel reaction monitoring as described previously19. MS/MS transitions for the labeled standard peptides and the unlabeled HER2 peptides from the samples were analyzed with Skyline20 and HER2 protein abundances were calculated as amol/μg protein from the ratio of summed signals for the three most intense MS/MS transitions for the sequences and the added standard amounts.
HER2 calibration CMA
The HER2 calibration cell microarray (CMA) was built by Array Science LLC (Sausalito, CA). The cell lines were arranged in two rows as shown in Fig. 2, with two-fold redundancy.
HER2 Standardization Yale TMA (YTMA263), Breast Cancer Cohorts (YTMA489, YTMA499) and the mammoplasty derived Breast Tissue cohort (YTMA540)
The HER2 standardization tissue microarray (TMA) was built by extracting 0.6 mm cores from 80 FFPE breast carcinomas seen at Yale Pathology between 1998 and 2011, 10 breast cell lines controls (prepared at Yale), and 10 non-tumor breast tissue cores. Cases were arranged in columns according to their HER2 status, as previously described21. The two breast cancer cohorts (YTMA489 and YTMA499) used in this study were built from 263 and 190 FFPE serial breast carcinomas seen at Yale Pathology between 2011–2012 and 2013–2014, respectively. Results from CLIA-certified IHC and FISH tests were extracted from the pathology reports. Two replicate TMAs for each cohort derived from two independent YTMA489 and YTMA499 blocks, each block containing one non-adjacent tumor core per patient. Basic clinicopathologic characteristics collected from the available tumor cores on the TMAs are shown in Supplementary Table 1. Similarly, YTMA540 was built extracting 0.6 mm cores from FFPE breast tissue samples derived from 16 female patients (age 18–62, median 36.5) without any known breast pathology after reduction mammoplasty (cosmetic surgery) between 2011–2014. Three replicates for each case were used on the TMA.
Antibodies, immunohistochemistry, and quantitative immunofluorescence
Validation of staining and protein expression
For antibody validation two different HER2 antibodies that target the intracellular domain of HER2 were tested; 29D8 (CST #2165; R-IgG) corresponding to residues surrounding tyrosine 1248 of human HER2 protein and PATHWAY anti-HER-2/neu (4B5) (Roche_#107918, R-IgG) corresponding to the TAENPEYLGL epitope (residues 1242–1254) of human HER2 protein22. First, after using the same working concentration, we compared the staining pattern of the two clones in the same tumor spots of YTMA263 using the same staining conditions. HER2 levels measured with 29D8 and 4B5 were highly correlated (rS = 0.87, P < 0.0001) (Fig. 3A). Since 4B5 has been shown to cross-react with ERBB422, we limited our analysis in this study to HER2 levels measured by 29D8. In addition, to account for inter-batch/operator variability, after definition of the optimized conditions for the low range HER2 assay, two independent operators stained the standardized YTMA263 and the Calibration CMA, showing high concordance and reproducibility among batches/operators. (Fig. 3B, C)
Staining protocol (IHC)
Chromogenic staining was performed (Liquid DAB + Substrate Chromogen, Dako), followed by counterstain with Tacha’s hematoxylin (Biocare Medical, Concord, CA, USA) for three minutes and dehydration with ethanol and xylene. Low pH retrieval for 40 min on the Leica Bond III Refine polymer DAB detection and HER2/ErbB2 clone EP3 Epitomics 1:100 was used in the Yale CLIA lab (Fig. 2A). HER2/ErbB2 29D8 (clone 29D8, #2165, Cell Signaling Technology) at 1.28 μg/ml and a pressure boiling container (PT Module, Lab Vision, Thermo Scientific, Waltham, MA) were used in the Rimm Lab (Fig. 2B). Finally, slides were cover-slipped using Cytoseal 60 (Thermo Scientific, Waltham, MA) and were visualized in Aperio ScanScope XT platform.
Digital image analysis (DIA)
The Aperio ScanScope XT platform was used at ×40 to digitize the slides. QuPath (open source software) was used to evaluate the area (mm2)/ cell for each cell line23. Automatic cell segmentation detected individual nuclei or cells and supported the assignment of measurements of the area occupied by each cell. Four independent CMA slides were used, each with two-fold redundancy. The average cell area of 8 measurements per cell line was used to calculate the area (mm2)/cell.
Staining protocol (HER2/CK/DAPI) (QIF)
Briefly, after TMA/CMA sections were deparaffinized, we subjected them to antigen retrieval with EDTA pH 8 buffer at 97 °C for 20 min in a pressure boiling container (PT Module, Lab Vision, Thermo Scientific, Waltham, MA). Next, we incubated the slides with a solution of 0.3% hydrogen peroxide in methanol for 30 min, to block endogenous peroxidase activity, followed by another 30 min incubation with 0.3% bovine serum albumin with 0.05% tween-20 blocking solution. Primary antibody against HER2 (clone 29D8, Cell Signaling), was applied on the tissue for overnight incubation at 4 °C, at seven different concentrations/dilutions (0.000128 μg/ml to 12.8 μg/ml), and with cytokeratin (CK) at 1:100 dilution (monoclonal mouse anti-human cytokeratin, clone AE1/AE3; wide spectrum screening, Dako, Glostrup, Denmark). The secondary antibodies used included anti-rabbit EnVision reagent (Dako) and secondary anti-mouse Alexa Fluor 546 (Invitrogen, 1:100), for HER2 and CK, respectively. Cy5 tyramide (PerkinElmer, 1:50) was used to visualize HER2 positive cells. We used 4′,6-diamidino-2-phenylindole (DAPI) to counterstain and visualize nuclei, and we mounted the slides with ProLong Gold Antifade reagent (Invitrogen).
Additionally, two slides derived from each of two independent YTMA489 and YTMA499 blocks, each block containing one non-adjacent tumor core per patient, were subjected to the same staining procedure at the same days to account for batch variation, using the low HER2 assay.
Image acquisition and quantification
Fluorescent images were acquired using a PM-2000 system (Navigate Biopharma, Carlsbad, CA, USA) and the AQUA™ method of QIF was used to determine levels of expression. An AQUA score was generated by dividing the sum of target pixel intensities by the area of the molecularly designated compartment, as previously described24. To distinguish tumor from tissue stroma and other components, an epithelial tumor “mask” was created by binarizing the CK signal and creating an epithelial compartment. AQUA scores were normalized to the exposure time and bit depth at which the images were captured, to compensate for any variability. All acquired TMA spots were visually assessed and cases with staining artifacts or less than 2% tumor (CK staining) were omitted from the analysis.
Results
Quantitative measurement of HER2 levels in cell lines
To produce a standardization CMA, LC-MS/MS assays were used for HER2 measurements in cell pellets derived from 6 breast cancer cell lines (BT-20, T-47D, ZR-75-1, BT-483, AU565, BT-474) and one non-breast cancer cell line (JURKAT) as a negative control. The linear range of the LC-MS/MS assay was explored via cell mixing experiment with BT-474 (HER2 high expressing) and JURKAT (HER2 null expressing) in serial triplicate dilutions in LC-MS/MS measurements (Supplementary Table 2, Supplementary Fig. 1A).
The DPPFCVAR (extracellular domain of the HER2 protein) and ELVSEFSR peptide (intracellular domain of the HER2 protein) were measured for each of the 7 cell pellets in amol/ug of total protein, by LC-MS/MS at Protypia. Quantification of HER2 in attomole/ug spanned from 25 amol/ug in BT-20, the lowest unamplified line to 1435 amol/ug in the highest amplified line (BT-474). HER2 was not detected in JURKAT cells. HER2 levels measured by both DPPFCVAR and ELVSEFR peptides were highly correlated (Spearman coefficient r = 1.00, P = 0.004) (Supplementary Fig. 1B). Since the HER2 extracellular domain has been found to be enzymatically cleaved from the cell membrane [23] in breast cancer cells and since most of the common clinical assays use cytoplasmic domain antibodies, we used the intracellular ELVSEFSR peptide measurements as our HER2 analyte in this study.
HER2 calibration CMA and DIA
After determining HER2 concentration in amol/µg of total protein for each cell line we constructed a CMA (Array Science, LLC) using the same cell lines (Fig. 2, Table 1) so we could convert amol/ug to amol/mm2. To build an assay that is optimized for low HER2 expression we focused on the non-amplified cell lines of this array (JURKAT, BT-20, T-47D, ZR-75-1, and BT-483)25. To convert amol/µg of total protein in cells to amol/area occupied by cells on the slide, we used QuPath (open-source software) to evaluate the area (mm2)/ cell for each cell line on our CMA. The average value of the measurements in 4 different subsequent slides was used as the reference value for area/ cell in mm2. (Supplementary Tables 3, 4).
Assay development and determination of limits of detection and quantification
As it has been previously described, by Gonzalez and Herrador26, the response function or calibration curve between the analytical signal and the concentration of analyte is a monotonic function27. Several mathematical models, such as mathematical transformations as well as weighted regression techniques, can examine how the response varies as a function of analyte concentration26. The simplest model often found in analytical methodology is the linear regression analysis, leading to predicted responses according to Eq. (1).
where α is the slope and β the intercept, with standard deviations sα and sβ, respectively.
In this study, Y corresponds to the AQUA scores and X to the amol/mm2.
Limit of Detection (LOD) and limit of quantitation (LOQ) are two parameters reciprocally derived from the assay sensitivity and are used to assess performance characteristics. LOD is the lowest concentration of analyte that can be detected and reliably distinguished from the noise level of the system, but not necessarily quantified; the concentration at which a measured value is larger than the uncertainty associated with it. LOD can be expressed in response units (YLOD) and is estimated by using the expression28:
where Yblank and Sblank are the average value of the blank signal and its corresponding standard deviation, respectively, obtained by measuring at least a minimum of 10 independent sample blanks. Blank samples in this case are defined as samples on which primary antibody is omitted from the staining process (see below).
LOQ is the lowest concentration of analyte that can be determined quantitatively with an acceptable level of precision28. The procedure for evaluating LOQs is equivalent to that of LODs, by measuring at least 10 independent sample blanks and using the factor 10 instead of 3 for calculations:
To estimate the Yblank we used the standardized HER2 YTMA263 array, which has more than 10 cases of low HER2. After obtaining the AQUA scores of low HER2 cases (IHC of 0, 1+, 2+/NOT Amplified) when no primary antibody against HER2 was added to the IF protocol, we estimated the Y blank and S blank, as described above. (Supplementary Fig. 3A).
To convert LOD and LOQ expressed in signal units (YLOD, YLOQ) to analyte concentration units (ZLOD, ZLOQ)26 we used the calibration function below:
Using seven dilutions of the primary antibody (HER2/ErbB2 29D8) ranging from 1.28 ng/ml to 12.8 ug/ml we stained the YTMA263 (Supplementary Fig. 2B–H) and the calibration CMA (Supplementary Fig. 3A–G). Linear regression analysis for the signal response (normalized AQUA score) and the analyte concentration (amol/mm2) is shown in Fig. 4 for the standardization CMA. Using the Eqs. 1–4 we were able to identify the LOD and LOQ for each assay. We determined that the optimal assay for low HER2 quantification was at 1.28 ug/ml of 29D8 primary antibody. As shown in supplementary fig. 3D, this concentration of antibody generates the highest level of signal in the unamplified cell line (BT-483) with the lowest level of noise (signal from the Jurkat cells). At 1.28 μg/ml of HER2 29D8 antibody, the calculated LOD was 0 amol/mm2 and the LOQ was 2.8 amol/mm2. In addition, to estimate the limits of assay linearity, described by Huber29, we evaluated the response factors RF for each assay (Supplementary Fig. 4A–G). The linear range of responses corresponds to the analyte concentrations from the point intersecting the line y = 1.05α up to the point that intersects the line y = 0.95α, assuming that the model is linear and without intercept. For the 1.28 μg/ml assay the upper limit of linearity (LOL) was 19 amol/ mm2.
Exploration of the LOQ, LOL of the low HER2 assay in 364 clinical cases characterized by IHC/ISH and in in 11 reduction mammoplasty cases
Having identified the optimal linear low HER2 assay we sought to apply it on a large cohort containing samples from patients with breast cancer collected between 2011–2014 at YNHH. Using TMAs with 364 tumor cores, in two-fold redundancy, we measured levels of expression of HER2. The average value of two cores/ patient was used for the analysis. The transformation of signal response (AQUA scores) to analyte concentration units (amol/mm2) was done based on the regression analysis equation of the optimal assay (Y = 296.4x = 607.9- Fig. 4D). Figure 5 shows a histogram of all of the cases colored by the pathologist score (0 = blue, 1 = red, 2 = black and 3 = green). The Y-axis shows the level of HER2 in amol/mm2 in 364 breast cancer tissue TMA cores. Example images of IHC1+ and 2+ cases are shown in Fig. 6A–D. Using this assay, 61 out of 364 cases (17%) were below the LOQ and 58/264 (16%) were above the LOL. Most of the cases (67%) were within the linear range of the assay. Interestingly, cases with IHC 2+, 1+ and 0 had a broad dynamic range of HER2 expression, consistent with previous observations that accurate scoring of low range cases by pathologists using the conventional IHC assays is challenging or impossible. Also note that the quantitative measurements were on tissue microarray spots while the pathologist scores are from whole tissue sections.
A histogram of the low HER2 assay in 364 breast cancer patients, measured in amol/mm2. Color coding corresponds to the IHC HER2 scoring; green (3+), black (2+), red (1+), blue (0), grey (NA, Not Available). LOQ limit of quantification; LOL limit of linearity; IHC immunohistochemistry. Letters A through D are cases illustrated in Fig. 6.
Representative images of cases from Fig. 5 showing IHC 1+ (A) 3.2 amol/mm2 (B), 15 amol/mm2 and IHC 2+, (C) 2.8 amol/mm2 and (D) 7.8 amol/mm2.
Some pathologists use the term “HER2-normal” rather than “HER2-negative” to reflect the fact that normal breast epithelial cells express HER2. To investigate the dynamic range of HER2 expression in breast tissue without a known pathologic condition we applied the low HER2 assay to 11 available samples of the YTMA540, a cohort built from reduction mammoplasty cases between 2011–2014. We noticed that none of these cases passed the threshold of 10 amol/mm2 (Supplementary Fig. 5). Although more cases will be investigated with this assay in the future, the preliminary data show that normal breast ducts express HER2 across a range of 2.5 and 10 amol/mm2. It will be interesting to see in the future which patients will benefit from ADCs and if their tumor HER2 level will be above the “normal” cutpoint (10 amol/mm2).
Discussion
In this study, we have constructed and validated a new assay for HER2 expression on histologic preparations using quantitative fluorescence and a series of ERBB2 gene unamplified cells lines expressing HER2 protein. The assay is based on mass spectrometry determination of the amount of HER2 protein combined with display in array format for standardization. The expression is measured in attomols/ug total protein in the cell lines, then converted to attomols/mm2 by image analysis and determination of area, supported by the AQUA method of analysis which allows assessment of signal per area rather than per cell. The resultant assay is linear between 2 and 20 attomols/mm2, which is below the levels seen in amplified cell lines or tumors, but within the range of expression seen in normal breast epithelium. We believe this assay will allow measurement of HER2 in the critical range where the HER2 targeting ADC drugs will be effective, but also the range that lacks reproducibility with current assays.
HER2 protein expression spans about 3 orders of magnitude15,16. Previous studies have estimated a functional range for conventional chromogenic stain-based assays between 1 and 1.5 orders of magnitude17. The functional range for fluorescence-based assays is extends to 2+ orders of magnitude (Supplementary Fig. 2) and LC-MS/MS assays to 3.5 log (Supplementary Fig. 1). Although the current assay combination of IHC and ISH can separate amplified from unamplified cases (with sensitivity as high as 95%)1, it is insufficient to identify low levels of HER2 expression. This is because the assay is designed to distinguish gene amplified levels of HER2 from gene unamplified levels. To span the full dynamic range of breast cancer HER2 expression more than one assay is needed. Here we have developed an assay that is complementary to the conventional assay with sensitivity and linearity in the range of HER2 that is largely below the conventional assay usage threshold. We anticipate that this assay can be incorporated in the clinical setting for these low- HER2 unamplified cases allowing more accurate patient stratification for potential benefit from ADC therapy.
This effort has a number of limitations. The most significant is that this work is done with heavy reliance on TMAs that neither replicate the clinical specimens nor suffer the heterogeneity of clinical specimens. However, to some extent, the challenge of heterogeneity is addressed by averaging expression over area rather than per cell. That is, our units are amols/mm2, so heterogeneity can be averaged. We are in the process of determination of the area required for assessment of clinical specimens (core biopsies), but that work is beyond the scope of this initial assay description. A second limitation is the dynamic range. While immunofluorescence-based assays have more linear dynamic range than chromogens, they still use enzyme amplification, and the assay is still limited by other factors common to IHC including sample processing and fixation and stability of protein antigens30,31,32. Finally, a major limitation of the work is that we have been unable to test any tissue from patients treated with HER2 targeting ADCs. While data from the early trials suggest the ADCs are effective in patient whose tumors express HER2 in a low range13,33, the threshold for drug efficacy has not yet been determined. To demonstrate the clinical utility of the assay, it will be necessary to retrospectively quantitatively analyze samples with measured clinical responses to an HER2-targeted ADC therapy, followed by prospective clinical trials.
In summary, we believe this new HER2-V2 assay should allow for objective and quantitative low HER2 assessment and that this tool could improve patient care by optimal selection of patients that will benefit from HER2 targeting of ADC drugs.
References
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, et al. Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. Arch Pathol Lab Med 2018; 142: 1364–1382; e-pub ahead of print 2018/05/31; https://doi.org/10.5858/arpa.2018-0902-SA.
Pegram MD, Lipton A, Hayes DF, Weber BL, Baselga JM, Tripathy D, et al. Phase II study of receptor-enhanced chemosensitivity using recombinant humanized anti-p185HER2/neu monoclonal antibody plus cisplatin in patients with HER2/neu-overexpressing metastatic breast cancer refractory to chemotherapy treatment. J Clin Oncol 1998; 16: 2659–2671; https://doi.org/10.1200/JCO.1998.16.8.2659.
Howie LJ, Scher NS, Amiri-Kordestani L, Zhang L, King-Kallimanis BL, Choudhry Y, et al. FDA Approval summary: Pertuzumab for adjuvant treatment of HER2-positive early breast cancer. Clin Cancer Res 2019; 25: 2949–2955; e-pub ahead of print 2018/12/16; https://doi.org/10.1158/1078-0432.Ccr-18-3003.
Ryan Q, Ibrahim A, Cohen MH, Johnson J, Ko CW, Sridhara R, et al. FDA drug approval summary: lapatinib in combination with capecitabine for previously treated metastatic breast cancer that overexpresses HER-2. Oncologist 2008 13: 1114–1119; e-pub ahead of print 2008/10/14; https://doi.org/10.1634/theoncologist.2008-0816.
Koleva-Kolarova RG, Oktora MP, Robijn AL, Greuter MJW, Reyners AKL, Buskens E, et al. Increased life expectancy as a result of non-hormonal targeted therapies for HER2 or hormone receptor positive metastatic breast cancer: A systematic review and meta-analysis. Cancer Treat Rev 2017; 55: 16–25; https://doi.org/10.1016/j.ctrv.2017.01.001.
von Minckwitz G, Huang C-S, Mano MS, Loibl S, Mamounas EP, Untch M, et al. Trastuzumab Emtansine for residual invasive HER2-positive breast cancer. New Engl J Med 2018; 380: 617–628 https://doi.org/10.1056/NEJMoa1814017.
Saura C, Oliveira M, Feng Y-H, Dai M-S, Chen S-W, Hurvitz SA, et al. Neratinib Plus Capecitabine Versus Lapatinib Plus Capecitabine in HER2-positive metastatic breast cancer previously treated with ≥ 2 HER2-directed regimens: Phase III NALA Trial. J Clin Oncol 2020; 38: 3138–3149 https://doi.org/10.1200/JCO.20.00147.
Murthy RK, Loi S, Okines A, Paplomata E, Hamilton E, Hurvitz SA, et al. Tucatinib, Trastuzumab, and Capecitabine for HER2-positive metastatic breast cancer. New Engl J Med 2019; 382: 597–609 https://doi.org/10.1056/NEJMoa1914609.
Rugo HS, Im S-A, Cardoso F, Cortés J, Curigliano G, Musolino A, et al. Efficacy of Margetuximab vs Trastuzumab in patients with pretreated ERBB2-positive advanced breast cancer: a Phase 3 randomized clinical trial. JAMA Oncol 2021; 7: 573–584 https://doi.org/10.1001/jamaoncol.2020.7932.
Hudis CA. Trastuzumab-mechanism of action and use in clinical practice. N Engl J Med 2007; 357: 39–51.
Tarantino P, Hamilton E, Tolaney SM, Cortes J, Morganti S, Ferraro E, et al. HER2-low breast cancer: pathological and clinical landscape. J Clin Oncol 2020; 38: 1951–1962; e-pub ahead ofprint 2020/04/25 https://doi.org/10.1200/jco.19.02488.
Nakada T, Sugihara K, Jikoh T, Abe Y, Agatsuma T. The latest research and development into the antibody-drug conjugate, [fam-] Trastuzumab Deruxtecan (DS-8201a), for HER2 cancer therapy. Chem Pharm Bull 2019; 67: 173–185; e-pub ahead of print 2019/03/05 https://doi.org/10.1248/cpb.c18-00744.
Modi S, Park H, Murthy RK, Iwata H, Tamura K, Tsurutani J, et al. Antitumor activity and safety of Trastuzumab Deruxtecan in patients With HER2-low–expressing advanced breast cancer: results from a Phase Ib Study. J Clin Oncol 2020; 38: 1887–1896 https://doi.org/10.1200/JCO.19.02318.
Fernandez AI, Liu M, Bellizzi A, Brock J, Fadare O, Hanley K, et al. Examination of low ERBB2 protein expression in breast cancer tissue. JAMA Oncol 2022; https://doi.org/10.1001/jamaoncol.2021.7239.
DeFazio-Eli L, Strommen K, Dao-Pick T, Parry G, Goodman L, Winslow J. Quantitative assays for the measurement of HER1-HER2 heterodimerization and phosphorylation in cell lines and breast tumors: applications for diagnostics and targeted drug mechanism of action. Breast Cancer Res 2011; 13: R44 https://doi.org/10.1186/bcr2866.
Onsum MD, Geretti E, Paragas V, Kudla AJ, Moulis SP, Luus L, et al. Single-cell quantitative HER2 measurement identifies heterogeneity and distinct subgroups within traditionally defined HER2-positive patients. Am J Pathol 2013; 183: 1446–1460; e-pub ahead of print 2013/09/17 https://doi.org/10.1016/j.ajpath.2013.07.015.
McCabe A, Dolled-Filhart M, Camp RL, Rimm DL. Automated quantitative analysis (AQUA) of in situ protein expression, antibody concentration, and prognosis. J Natl Cancer Inst 2005; 97: 1808–1815.
Morales-Betanzos CA, Lee H, Gonzalez Ericsson PI, Balko JM, Johnson DB, Zimmerman LJ, et al. Quantitative Mass Spectrometry Analysis of PD-L1 Protein Expression, N-glycosylation and Expression Stoichiometry with PD-1 and PD-L2 in Human Melanoma. Mol Cell Proteom 2017; 16: 1705–1717; e-pub ahead of print 2017/05/27 https://doi.org/10.1074/mcp.RA117.000037.
Liebler DC, Holzer TR, Haragan A, Morrison RD, O’Neill Reising L, Ackermann BL, et al. Analysis of immune checkpoint drug targets and tumor proteotypes in non-small cell lung cancer. Sci Rep 2020; 10: 9805; e-pub ahead of print 2020/06/20 https://doi.org/10.1038/s41598-020-66902-0.
MacLean B, Tomazela DM, Shulman N, Chambers M, Finney GL, Frewen B, et al. Skyline: an open source document editor for creating and analyzing targeted proteomics experiments. Bioinformatics 2010; 26: 966–968; e-pub ahead of print 2010/02/12 https://doi.org/10.1093/bioinformatics/btq054.
Carvajal-Hausdorf DE, Schalper KA, Neumeister VM, Rimm DL. Quantitative measurement of cancer tissue biomarkers in the lab and in the clinic. Lab Invest 2015; 95: 385–396 https://doi.org/10.1038/labinvest.2014.157.
Schrohl, A-S., Pedersen, HC., Jensen, SS., Nielsen, SL. & Brünner, N. Human epidermal growth factor receptor 2 (HER2) immunoreactivity: specificity of three pharmacodiagnostic antibodies. Histopathology 59, 975–983, https://doi.org/10.1111/j.1365-2559.2011.04034.x (2011).
Bankhead P, Loughrey MB, Fernández JA, Dombrowski Y, McArt DG, Dunne PD, et al. QuPath: Open source software for digital pathology image analysis. Sci Rep 2017; 7: 16878 https://doi.org/10.1038/s41598-017-17204-5.
Camp, R L, Chung, G G & Rimm, D L Automated subcellular localization and quantification of protein expression in tissue microarrays. Nat Med 8, 1323–1327 (2002).
Subik K, Lee JF, Baxter L, Strzepek T, Costello D, Crowley P, et al. The Expression Patterns of ER, PR, HER2, CK5/6, EGFR, Ki-67 and AR by immunohistochemical analysis in breast cancer cell lines. Breast Cancer 2010; 4: 35–41; e-pub ahead of print 2010/08/11.
Gustavo González A, Ángeles Herrador M. A practical guide to analytical method validation, including measurement uncertainty and accuracy profiles. TrAC Trends Anal Chem 2007; 26: 227–238; https://doi.org/10.1016/j.trac.2007.01.009.
Hubert P, Chiap P, Crommen J, Boulanger B, Chapuzet E, Mercier N, et al. The SFSTP guide on the validation of chromatographic methods for drug bioanalysis: from the Washington Conference to the laboratory. Analytica Chimica Acta 1999; 391: 135–148; https://doi.org/10.1016/S0003-2670(99)00106-3.
Inczedy JnLTsUAMIUoP, Applied C. Compendium of analytical nomenclature: definitive rules 1997. Blackwell Science: Osney Mead, Oxford; Malden, MA, 1998.
Huber L. Validation and Qualification in Analytical Laboratories. Interpharm Presss, East Englewood, CO, USA 1998.
Moatamed NA, Nanjangud G, Pucci R, Lowe A, Shintaku IP, Shapourifar-Tehrani S, et al. Effect of ischemic time, fixation time, and fixative type on HER2/neu immunohistochemical and fluorescence in situ hybridization results in breast cancer. Am J Clin Pathol 2011; 136: 754–761 https://doi.org/10.1309/AJCP99WZGBPKCXOQ.
Bai Y, Tolles J, Cheng H, Siddiqui S, Gopinath A, Pectasides E, et al. Quantitative assessment shows loss of antigenic epitopes as a function of pre-analytic variables. Lab Investig 2011; 91: 1253–1261 https://doi.org/10.1038/labinvest.2011.75.
Siddiqui S, Rimm DL. Pre-analytic variables and phospho-specific antibodies: The Achilles heel of immunohistochemistry. Breast Cancer Research (Editorial) 2010; 12; https://doi.org/10.1186/bcr2782.
Modi, S., Saura, C., Yamashita, T., Park, Y H., Kim, S-B. & Tamura, K. et al. Trastuzumab Deruxtecan in previously treated HER2-positive breast cancer. New Engl J Med 382, 610–621, https://doi.org/10.1056/NEJMoa1914510. (2019).
Acknowledgements
We would like to thank Lori Charette, and the team at the Yale Pathology Tissue Service and Developmental Histology Facility for production of the high-quality tissue sections and TMAs. This study was supported by a sponsored research agreement with InviCRO/Konica/Minolta and the Breast Cancer Research Foundation (DLR) and the Yale Cancer Cancer (P30CA016359). Myrto Moutafi was supported by a scholarship from the Hellenic Society of Medical Oncologists (HESMO).
Author information
Authors and Affiliations
Contributions
MM: Data collection, formal analysis, investigation, visualization, methodology, writing including the original draft, and review and editing of the manuscript. CR: Data collection and curation, formal analysis, validation, and review and editing of the manuscript. VY: Data collection and curation and review and editing of the manuscript. SM-M: Data collection and curation and review and editing of the manuscript. VX: Data collection and curation and review and editing of the manuscript. YB; Data collection and curation and review and editing of the manuscript. YS: Data collection and curation and review and editing of the manuscript. PG: Data collection and curation and review and editing of the manuscript. JK: Data collection and curation, project administration and supervision, and review and editing of the manuscript. KB: Data collection and curation, project administration and supervision, and review and editing of the manuscript. SH: Data collection and curation and review and editing of the manuscript. D: Data collection and curation and review and editing of the manuscript. RF: Data collection and curation, resource provision, and review and editing of the manuscript DLR: Conceptualization, resources, formal analysis, supervision, funding acquisition, writing including the original draft, project administration, writing, review, and editing of the final draft.
Corresponding author
Ethics declarations
Competing interests
DLR has served as an advisor for AstraZeneca, Agendia, Amgen, BMS, Cell Signaling Technology, Cepheid, Danaher, Daiichi Sankyo, Novartis, GSK, Konica Minolta, Merck, NanoString, PAIGE.AI, Perkin Elmer, Regeneron, Roche, Sanofi, Ventana, and Ultivue. Amgen, Cepheid, Konica Minolta, NavigateBP, NextCure, and Lilly have funded research in his lab. JK and KB are employees of Invicro, a division of Konica/Minolta. DCL and SH are employees of Protypia, Inc. Regan Fulton is the majority owner of Array Science, LLC and serves as a consultant to Leica Biosystems, Personalis, Inc., and Konica/Minolta (Invicro). All other authors declare no conflict of interest.
Ethics approval and consent to participate
All tissue samples were collected with the approval from the Yale Human Investigation Committee protocol #9505008219. Written informed consent, or waiver of consent, was obtained from all patients with the approval of the Yale Human Investigation Committee.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Moutafi, M., Robbins, C.J., Yaghoobi, V. et al. Quantitative measurement of HER2 expression to subclassify ERBB2 unamplified breast cancer. Lab Invest 102, 1101–1108 (2022). https://doi.org/10.1038/s41374-022-00804-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41374-022-00804-9
This article is cited by
-
Quantitative proteomic analysis of HER2 protein expression in PDAC tumors
Clinical Proteomics (2024)
-
Immunohistochemical assessment of HER2 low breast cancer: interobserver reproducibility and correlation with digital image analysis
Breast Cancer Research and Treatment (2024)
-
High inter-laboratory variability in the assessment of HER2-low breast cancer: a national registry study on 50,714 Danish patients
Breast Cancer Research (2023)
-
NFIB facilitates replication licensing by acting as a genome organizer
Nature Communications (2023)
-
Targeting HER2-positive breast cancer: advances and future directions
Nature Reviews Drug Discovery (2023)