Abstract
Glioblastoma (GBM) is still one of the most commonly diagnosed advanced stage primary brain tumors. Current treatments for patients with primary GBM (pGBM) are often not effective and a significant proportion of the patients with pGBM recur. The effective treatment options for recurrent GBM (rGBM) are limited and survival outcomes are poor. This retrospective multicenter pilot study aims to determine potential cell-free microRNAs (cfmiRs) that identify patients with pGBM and rGBM tumors. 2,083 miRs were assessed using the HTG miRNA whole transcriptome assay (WTA). CfmiRs detection was compared in pre-operative plasma samples from patients with pGBM (n = 32) and rGBM (n = 13) to control plasma samples from normal healthy donors (n = 73). 265 cfmiRs were found differentially expressed in plasma samples from pGBM patients compared to normal healthy donors (FDR < 0.05). Of those 193 miRs were also detected in pGBM tumor tissues (n = 15). Additionally, we found 179 cfmiRs differentially expressed in rGBM, of which 68 cfmiRs were commonly differentially expressed in pGBM. Using Random Forest algorithm, specific cfmiR classifiers were found in the plasma of pGBM, rGBM, and both pGBM and rGBM combined. Two common cfmiR classifiers, miR-3180-3p and miR-5739, were found in all the comparisons. In receiving operating characteristic (ROC) curves analysis for rGBM miR-3180-3p showed a specificity of 87.7% and a sensitivity of 100% (AUC = 98.5%); while miR-5739 had a specificity of 79.5% and sensitivity of 92.3% (AUC = 90.2%). This study demonstrated that plasma samples from pGBM and rGBM patients have specific miR signatures. CfmiR-3180-3p and cfmiR-5739 have potential utility in diagnosing patients with pGBM and rGBM tumors using a minimally invasive blood assay.
Similar content being viewed by others
Introduction
Glioblastoma (GBM) is a devastating advanced stage primary brain tumor with a poor survival rate after initial diagnosis1,2. The poor disease outcome is due to the high rate of recurrence typically seen shortly after surgery and the limited effective treatment options1,2. Magnetic resonance imaging (MRI) is used to diagnose, monitor therapeutic response, and determine disease progression in GBM patients2. The major limitation is that GBM patients need to be scanned frequently to monitor disease progression; however, this is costly and can logistically be a problem. The other limitation is that MRI cannot distinguish GBM tumor pseudo-progression or radionecrosis on patients receiving treatment. Thus, there is an urgent need to develop a robust and reproducible minimally invasive blood molecular biomarker assay that allows for repetitive monitoring. Blood biomarkers for GBM should allow for the identification of early stages of the disease and provide a minimally invasive method for monitoring tumor recurrence. Our group has been working to develop novel approaches to identify blood biomarkers in different forms of cell-free DNA (cfDNA)3, circulating tumor cells (CTCs)4, and more recently, cell-free microRNAs (cfmiRs)5,6,7,8 in patients with solid tumors. Unfortunately, CTC detection of GBM patients is restricted due to a limited amount of shedding in the peripheral blood9. The brain tumor cfDNA detection is also inefficient due to the size of the cfDNA and short half-life once released into the peripheral blood10,11,12.
MicroRNAs (miRs) are non-coding small RNA molecules that bind to the coding mRNA to either promote mRNA degradation or stop mRNA translation and consequently, block gene expression12,13,14. Thus, miRs represent major regulators of the cellular transcriptome, including the regulation of tumor suppressor and oncogenic genes14. The dysregulation of miRs expression has been linked to cancer development and progression of brain tumors as we and other groups have shown8,12,15. Changes in the expression of specifics miRs in GBM tissue samples have potential as diagnostic and prognostic factors in GBM patients8,12,15. The primary challenge with using miRs detected in tissues as potential biomarkers is that repetitive tissue biopsies to monitor GBM patients are not feasible.
The miRs can be released by the tumor cells into the blood in the form of cfmiRs or exosomal-miRs12. In comparison to cfDNA released by the tumor cells, cfmiRs are more stable in the blood16. CfmiRs detected in the blood represent one of the most promising areas to identify new biomarkers for GBM patients, as miRs can cross the blood-brain barrier due to their small size12. MiRs have been found in the plasma and serum of GBM patients using different technologies, although most of the studies rely on qRT-PCR and microarray assays13,17. Specific miRs are upregulated in plasma or serum samples and have diagnostic and/or prognostic value for GBM patients, as previously discussed12,13. A previous study has shown that miR-21, miR-128, and miR-342-3p distinguish GBM patients from normal healthy donors and other types of brain metastases and have been proposed as diagnostic markers for GBM18. Additionally, miR-21 has been shown to have clinical utility to monitor GBM treatment effectiveness19,20. In another study, an 11-cfmiR signature has been suggested as a biomarker for GBM recurrence13,21. The major limitation in these studies is that single or combined miR biomarkers often are devoid of specificity as they have also been related to other types of tumors or benign diseases22. The other limitation is that there is still no validation in defined clinical trials that have determined whether the proposed cfmiRs represent reliable biomarkers to assess for GBM tumors and monitor recurrence. Despite the limitations observed in previous studies, cfmiRs have advantages over other blood-based assays for detecting GBM tumors.
Our group has previously demonstrated the utility of High Throughput Genomics (HTG) miR Whole Transcriptome Assay (WTA) in detecting miRs5,6,7,8. The HTG miR WTA assessed 2,083 miRs, where most of the probes are designed to capture the mature forms of the miRs. This assay is extraction-free and requires minimal amounts of plasma and tissue samples5,6,7. This retrospective pilot study aims to demonstrate that cfmiRs found in the plasma of patients with primary GBM (pGBM) may represent potential molecular biomarkers to (1) identify tumor presence in patients with pGBM, and (2) patients with recurrent GBM (rGBM). To accomplish the proposed aims, we compared the cfmiRs profiles of pre-operative plasma samples from patients diagnosed with pGBM (n = 32) or rGBM (n = 13) in a multicenter accrual to normal healthy donors (n = 73) plasma samples. Using Random Forest (RF) machine learning, we identified cfmiR classifiers in plasma samples that distinguish pGBM and rGBM patients from normal healthy donors, and common cfmiRs in the plasma of pGBM and rGBM. CfmiR-3180-3p and miR-5739 showed to be good classifiers for pGBM and rGBM patients. In receiver operating characteristic (ROC) curve analysis, both cfmiR-3180-3p and miR-5739 showed potential utility in detecting pGBM and rGBM tumors.
Materials and methods
Blood collection and tissue analysis
Please refer to the below section “Ethics Approval and Consent to Participate”. Blood samples from normal healthy donors and cancer patients were obtained at SJHC/SJCI and Swedish Medical Center. All blood samples were collected in Streck tubes (Streck, La Vista, NE, USA) or EDTA tubes (BD vacutainers®, USA). Briefly, all blood samples from SJCI and Swedish Medical Center were processed, aliquoted, barcoded, and cryopreserved −80 °C, as previously described5,6. Aliquots of plasma were thawed once and mixed. Plasma samples were collected from normal healthy donors (n = 73) ranging in age from 21-65 years old at SJHC/SJCI. Single pre-operative plasma samples were collected from pGBM (n = 16 at SJHC and n = 16 at Swedish Medical Center) and rGBM patients (n = 13 at SJHC/SJCI). Single pre-operative plasma samples were collected from LGG (n = 9 at Swedish Medical Center). All plasma samples were analyzed by the HTG miR WTA. Patients’ demographics and clinical data are summarized in Table 1. The clinical information for each case is described in Supplementary Table 1.
Formalin-fixed paraffin-embedded (FFPE) surgically resected tissue samples were taken from patients diagnosed with pGBM (n = 15). These patients received a craniotomy at Swedish Medical Center and had pre-operatively paired plasma samples collected. The 15 FFPE samples were analyzed using HTG miR WTA as previously described6,7.
Relevant diagnostic factors were included in the study for all the patients pGBM (n = 32), rGBM (n = 13), and LGG (n = 9) such as: the O[6]-methylguanine-DNA methyltransferase (MGMT) promoter methylation status, age at diagnosis, recurrence status, and Isocitrate Dehydrogenase 1 (IDH1) R132H mutation status. The pathological evaluation of the tumor was performed at the Department of Pathology at SJHC or at Swedish Medical Center. The MGMT promoter methylation status was determined by methylation-specific PCR (MSP). The IDH1 R132H mutation status was determined by immunohistochemistry. All the GBM tumors were categorized using the World Health Organization (WHO) classification of central nervous system tumors of 201623.
Sample processing and profiling for HTG miR WTA
Normal healthy donors, pGBM, rGBM, and LGG plasma samples processing, library preparation, Next Generation Sequencing (NGS) library quality control, and NGS library normalization and pooling were performed as previously described5,6,7. pGBM tissue samples processing, library preparation, NGS library quality control, and NGS library normalization and pooling were done as previously described5,6,7. The NGS was performed with Illumina NextSeq 550 or MiSeq platforms following HTG instructions. Sequences were assessed with a read length of 1 × 50 base pairs. FASTQ files were generated from raw sequencing data using Illumina BaseSpace bcl2fastq software version 2.2.0 and Illumina Local Run Manager Software version 2.0.0. FASTQ files were analyzed with HTG EdgeSeq Parser software version v5.3.0.7184 to generate raw counts for 2,083 miRs per sample5,6,7. All of the samples included in this study passed quality control checks. Each HTG miR WTA includes negative (CTRL_ANT1, CTRL_ANT2, CTRL_ANT3, CTRL_ANT4, CTRL_ANT5), positive (CTRL_miR_POS) miR controls, and 13 mRNA housekeeping genes. All these controls are included in addition to the 2,083 total miR panel. In all runs, Human Brain Total RNA (Ambion, Inc., Austin, TX, USA) was used as a control for library preparation but was not sequenced5,6,7.
Bioinformatic analysis
The DESeq2 data normalization, analyses, and statistical comparisons between normal healthy donors, pGBM, rGBM, and LGG plasma samples, as well as paired pGBM plasma and tissues, were performed using the HTG REVEAL software version: 4.0.0. DESeq2 normalized data were logarithmically scaled for data visualization5,6. ROC curves and the area under the curve (AUC) were evaluated with R 4.0.2, using pROC package version 1.17.0.1 and cutpointr package version 1.1.1. Box plots were created using GraphPad prism 8 (GraphPad software Inc., La Jolla, CA). Principal component analysis (PCA) was performed using ClustVis software (https://bit.cs.ut.ee/clustvis/). RNA-Seq expression data for normal tissues and organs were obtained from the Genotype-Tissue Expression (GTEx) project (https://gtexportal.org/home/). TCGA RNA-Seq expression data for pGBM and normal adjacent brain tissues were obtained from http://tcga-data.nci.nih.gov and http://gdac.broadinstitute.org/ in May 2021. Predicted targets for miR-3180-3p and miR-5739 were obtained from the TargetScan database (http://www.targetscan.org/vert_71/). Only predictive targets that have a total context score <−0.5 were included in the analysis.
Biostatistical analysis
Differential expression was calculated using DESeq2 and differentially expressed miRs with a false-discovery rate (FDR) < 0.05 were only included. DESeq2 was performed using HTG REVEAL software as described in Bioinformatic analysis. T-test analysis and One-Way ANOVA were performed with GraphPad prism 8. A two-sided p value < 0.05 was considered statistically significant. All the figures were unified using CorelDraw graphics suite 8X (Corel Corporation, Ottawa, Canada) and/or Adobe Illustrator CC (Adobe Inc., Los Angeles).
Results
Study design and patients’ demographics
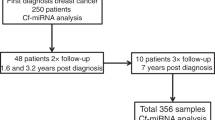
This is a retrospective multicenter (two centers highly experienced in GBM neurosurgery; D.F.K., G.B., and C.C.) pilot study analyzing 45 pre-operative plasma samples from 42 patients diagnosed with pGBM and/or rGBM. All the patients underwent a craniotomy for pGBM or rGBM tumors. The clinical information for the patients was retrospectively collected at each center (Table 1 and Supplementary Table 1). The pre-operative plasma samples were from patients with pGBM (n = 32) and rGBM (n = 13) (Fig. 1a). Paired pre-operative plasma samples were collected from three patients who were diagnosed with pGBM and rGBM. In addition, 15 patients with pGBM had both plasma and FFPE tissue samples analyzed. The median age at diagnosis was 58.6 years (range = 27–77 years) in the pGBM group and 56.3 years (range = 44–75 years) in the rGBM group (Table 1 and Supplementary Table 1). 68.75% (22 of 32) of the patients were male in the pGBM group; meanwhile, 76.9% (10 of 13) of the patients were male in the rGBM group (Table 1 and Supplementary Table 1).
MiRs detected in plasma and tumor tissue of pGBM patients
The first objective of this study is to identify significant cfmiRs in pre-operative plasma samples obtained from pGBM patients. To accomplish this, the pre-operative plasma samples were assessed using HTG miR WTA for 2,083 miRs. Although the HTG miR WTA works for both plasma and serum samples, our focus was on plasma samples because we have previously shown better efficacy and accuracy6. The cfmiR profiles from pGBM patients (n = 32) were compared to the cfmiR profiles obtained from the normal healthy donors (n = 73) using HTG REVEAL software. After applying DESeq2 and FDR < 0.05, 265 cfmiRs were found differentially expressed in plasma obtained from pGBM patients; where 141 were upregulated and 124 were downregulated (Supplementary Fig. 1a). In order to determine cfmiRs with potential utility as blood biomarkers, we focused on the most detectable cfmiRs (top 100), the most upregulated cfmiRs (top 100), and most significantly changing cfmiRs (top 100) within the 265 differentially expressed cfmiRs. The results showed 28 cfmiRs in the plasma of pGBM patients meeting these criteria that may represent potential biomarkers associated with pGBM tumor presence (Fig. 2a and Supplementary Table 1). Several studies have proposed cfmiR-21 detection in the plasma or serum as a potential diagnostic, prognostic, treatment monitoring utility in GBM patients19,20. However, miR-21-3p or miR-21-5p were not found among these 28 cfmiRs. Of note, miR-21-5p was observed in the top 100 most upregulated and detected cfmiRs, but it was not observed among the top 100 most significantly changing cfmiRs (Fig. 2a and Supplementary Table 2). Similar results were observed for miR-16-5p, miR-29b-3p, and miR-29c-3p in plasma samples from GBM patients (Fig. 2a and Supplementary Table 2). We also searched for miR-124-3p, which has been reported to be detected in exosomes purified from serum samples from high-grade glioma patients24. Our results showed that miR-124-3p is found in the top 100 most upregulated and most significant changing cfmiRs, but it was not observed among the top 100 most detected cfmiRs (Fig. 2a).
a Venn diagram showing the common cfmiRs found considering the top 100 cfmiRs most detected, most significant changing, and most upregulated that were identified for pGBM vs normal healthy donors (NHD). 28 cfmiRs were commonly identified as the most significantly changing, upregulated, and detected in pGBM. b, c Correlation matrices showing the correlation values across the 15 plasma (b) or the 15 tissue (c) samples from pGBM. The color scale bar indicates the correlation values from 0–1. d Plot showing the correlation values between the miR detection (Log2 mean CPM + 1) in 15 paired plasma and tissue samples obtained from pGBM patients. e Venn diagram showing the cfmiRs differentially expressed detected in plasma pGBM that were also detected in tissue samples from pGBM patients (normalized counts >30). f PCA comparing NHD (red) and pGBM (blue). Shown are the principal components (PC) 3 and PC2.
Next, our focus was to determine whether the cfmiRs found differentially expressed in the plasma samples of pGBM patients were also detected in pGBM tumor samples. To do that, we analyzed the miR expression in FFPE surgically resected tumors (n = 15) with paired plasma samples (n = 15). All the pGBM FFPE tumor tissues were micro-dissected to obtain the tumor section before being analyzed with HTG miR WTA. The 2,083 miRs detected by the HTG miR WTA were correlated among the 15 pGBM tissue samples analyzed. We observed positive correlation values >0.94 for all the tissue samples compared (Fig. 2b); indicating that miR detection was consistent across the pGBM tissue samples. As determined by the correlation values (0.26–0.94) for miR detection, the 15 pGBM plasma samples showed higher variability in miR detection than the pGBM tissue samples (Fig. 2c). The detection values for all the 2,083 miRs analyzed in the plasma and paired tissue samples showed a significant positive correlation (r = 0.69, p < 0.001; Fig. 2d); indicating that the miR detection in plasma and tissue samples overlaped. To summarize, paired plasma and tissue samples obtained from pGBM patients showed a positive correlation in miR detection. The miRs detected in the tissues are consistently detected in the plasma samples of pGBM patients and may represent potential biomarkers for tumor detection assessment.
Then, miRs detected in the pGBM tissues were compared to the cfmiRs differentially expressed in paired plasma samples obtained from pGBM patients, using normal healthy donors as a baseline. 72.8% (193 of 265) of the miRs found differentially expressed in the plasma of pGBM patients were commonly detected in pGBM tissues (total 1,005 miRs detected with >30 normalized counts, Fig. 2e). These results indicate that a significant amount of cfmiRs found in the blood is also detected in the pGBM tumor. On the other hand, 27.2% (72 of 265) of the miRs differentially expressed in the plasma of pGBM patients were not detected in the pGBM tumor tissues (Fig. 2e). These miRs may have been released by the tumor microenvironment and may have not been detected due to the pGBM tissue microdissection. To further refine the cfmiR signature and find the best cfmiR classifiers for pGBM, the 193 miRs were analyzed by the RF algorithm. A total of 18 miRs were found using RF (inclusion criteria: Feature Importance Scores >0.01) in pGBM patients compared to normal healthy donors (Table 2). The top five cfmiRs found in the RF analysis separated pGBM patients from normal healthy donors in a PCA (Fig. 2f). The first three components of the PCA showed a cumulative variance of 88%. These results demonstrated that specific miRs detected in the pGBM tumor tissues are released into the systemic blood system. This 5-cfmiR signature determined by using RF may have potential utility to be applied as a cfmiR biomarker in blood assays for pGBM patients.
Distinctive cfmiRs signature in the plasma of rGBM patients
Our focus was to determine whether the cfmiRs found in the plasma of patients diagnosed with rGBM significantly differ from those found in normal healthy donors. Thus, plasma samples from rGBM patients and normal healthy donors were assessed and compared to determine differentially expressed cfmiRs. Using DESeq2 and FDR < 0.05, 179 cfmiRs were found differentially expressed in the plasma of rGBM compared to normal healthy donors (Supplementary Fig. 2a). Of those 179 cfmiRs, 66 were upregulated, while 113 were downregulated (Supplementary Fig. 2a). To determine potential cfmiR biomarkers, we compared the most detectable miRs (top 100), the most upregulated miRs (top100), and the most significantly changing miRs (top 100) in rGBM versus normal healthy donors (Fig. 3a). A total of 23 cfmiRs met these criteria and it may represent potential biomarkers for rGBM (Fig. 3a and Supplementary Table 3). Ten cfmiRs were consistently detected in both comparisons considering the top 100 ranking in pGBM and rGBM plasma samples (Fig. 3b). To define the best cfmiR classifiers for rGBM, we applied RF to the 179 differentially expressed cfmiRs. A 23-cfmiR signature was identified in the plasma of rGBM patients (Table 2).
a Venn diagram showing the common cfmiRs considering the top 100 cfmiRs most detected, most significantly changing, most upregulated that were identified for rGBM vs normal healthy donors (NHD). A total of 23 cfmiRs were commonly identified as the most significantly changing, most upregulated, and most detected in rGBM. b The 23 cfmiRs were commonly identified as the most significantly changing, upregulated, and detected in NHD vs rGBM were then compared to the 28 cfmiRs identified in NHD vs pGBM. c 68 cfmiRs were commonly found as differentially expressed in the two comparisons NHD vs pGBM and NHD vs rGBM. d PCA plot comparing NHD (red), pGBM (blue), and rGBM (green). Shown are the principal components (PC) 4 and 2.
Another aim of this pilot study was to demonstrate whether plasma samples from rGBM and pGBM patients have overlapping miR profiles. To address this aim, we compared the 193 miRs commonly found in pGBM plasma and tissues to the 179 miRs differentially expressed in rGBM. 35.2% (68 of 193) of the cfmiRs were differentially expressed in pGBM and rGBM (Fig. 3c). This indicates that similar miRs may be released by both pGBM and rGBM tumors. The 68 miRs commonly detected were subjected to an RF machine learning algorithm to determine the best classifiers for normal healthy donors and GBM patients (both pGBM and rGBM). A 33-miR signature was developed using RF in GBM patients compared to normal healthy donors (Table 2). Using PCA, we observed that the 33-miR signature distinguished normal healthy donors from GBM patients. The first five components of the PCA showed a cumulative variance of 80.7% (Fig. 3d). Based on these results the 33-miR signature has potential utility in detecting rGBM tumors.
MiR-3180-3p and miR-5739 have utility to identify patients with rGBM
We compared the miR classifiers identified in each of the RF analyses for the three comparisons: normal healthy donors vs pGBM, rGBM, and GBM. MiR-3180-3p and miR-5739 were commonly detected as cfmiR classifiers in the three comparisons (Fig. 4a). Next, we compared the detection of both cfmiRs in plasma samples obtained from normal healthy donors, pGBM, and rGBM patients. Both miR-3180-3p and miR-5739 were significantly increased in pGBM and rGBM when compared to normal healthy donors (Fig. 4b, c).
a Venn diagram showing the two common cfmiRs and the three different RF analysis performed: the 18 cfmiR classifiers identified for pGBM, the 23 cfmiR classifiers identified for rGBM, and the 33 classifiers identified for GBM (pGBM and rGBM). MiR-3180-3p and miR-5739 were commonly identified as cfmiR classifiers. b Detection of miR-3180-3p in normal healthy donors (NHD), pGBM, rGBM, and LGG plasma samples. c Detection of miR-5739 in NHD, pGBM, rGBM, and LGG plasma samples. d–i ROC curves for miR-3180-3p comparing NHD and pGBM (d), NHD and rGBM (f), NHD and GBM (h); or for miR-5739 comparing NHD and pGBM (e), NHD and rGBM (g), NHD and GBM (i). Data represent the mean ± SD. *p < 0.05, **p < 0.01, ***p < 0.001, and NS non-significant.
To demonstrate that miR-3180-3p and miR-5739 had higher detection in patients with pGBM and rGBM, additional plasma samples from LGG patients (n = 9) were profiled using HTG miR WTA. Consistently, miR-3180-3p and miR-5739 were significantly increased in the plasma of pGBM and rGBM compared to LGG patients (Fig. 4b, c).
Using ROC curves, both miR-3180-3p and miR-5739 were assessed for their specificity and sensitivity to distinguish pGBM, rGBM, or GBM from normal healthy donors. MiR-3180-3p showed a specificity of 93.2% and a sensitivity of 78.1% (AUC 83.8%, Fig. 4d) in pGBM plasma samples; while miR-5739 showed a specificity of 95.9% and a sensitivity of 59.4% (AUC 82.7%, Fig. 4e). In identifying rGBM from normal healthy donors, miR-3180-3p showed a specificity of 87.7% and a sensitivity of 100% (AUC 98.5%, Fig. 4f); while miR-5739 showed a specificity of 79.5% and sensitivity of 92.3% (AUC 90.2%, Fig. 4g). Then, both miRs were assessed in GBMs (pGBM and rGBM). MiR-3180-3p had a specificity of 93.2% and sensitivity of 83.2% (AUC 88.1%, Fig. 4h); while miR-5739 showed a specificity of 95.9% and sensitivity of 62.2% (AUC 84.8%, Fig. 4i). To summarize, miR-5739 and miR-3180-3p represent potential cfmiR blood biomarkers to identify patients with pGBM and rGBM tumors.
We then looked at specific genes, which may have biological implications for GBM tumors, whose mRNAs can be targeted and downregulated by miR-3180-3p and miR-5739. Thus, we searched for specific mRNA targets in the miR database TargetScan. All predictive targets with a total context score <−0.5 were included in the comparison for both miRs (Supplementary Tables 4 and 5). Potential genes related to neuronal and brain functions included SCRT1 (Scratch Family Transcriptional Repressor 1), NPTX2 (Neuronal Pentraxin 2), STX1A (Syntaxin-1) were predicted as targets for miR-3180-3p and DDN (Dendrin) was specific for miR-5739 (Supplementary Table 4 and 5). Seven genes were commonly predicted as targets for both miRs (Fig. 5a). Four of the seven (CPLX1 (complexin-1), DLGAP3 (DLG associated protein-3), ATP6V0C (ATPase V0 subunit), and TTBK1 (Tau tubulin kinase-1) mRNA target genes were expressed specifically in normal brain tissues (Fig. 5b-e). The sequence in the CPLX1 gene targeted by miR-3180-3p and miR-5739 is shown as an example (Fig. 5f, g). Moreover, the four genes were consistently downregulated in pGBM (n = 156) tumors compared to normal adjacent brain tissues (n = 5) using the TCGA GBM RNA-Seq dataset (Fig. 6a–d). These results show that CPLX1, DLGAP3, ATP6V0C, and TTBK1 genes are commonly predicted targets for both miR-3180-3p and miR-5739. CPLX1, DLGAP3, ATP6V0C, and TTBK1 genes are specifically expressed in normal brain tissues. Supporting these findings, all four potential target genes of miR-3180-3p and miR-5739 are downregulated in pGBM tumors, suggesting that mRNA downregulation on the predicted target genes may have biological functions in promoting pGBM tumor development.
a Seven genes were commonly identified as predictive targets for miR-3180-3p and miR-5739 using the TargetScan database. Four of the seven predicted targets were identified as brain-specific genes: CPLX1, DLGAP3, ATP6V0C, and TTBK1. b–e The mRNA expression levels of CPLX1 (b), DLGAP3 (c), ATP6V0C (d), and TTBK1 (e) in normal tissues were evaluated in the GTEx database. f Schematic representation showing one of the four predicted binding sites for miR-3180-3p in the CPLX1 gene. g Schematic representation showing one of the four predicted binding sites for miR-5739 in the CPLX1 gene.
a–d The mRNA expression levels of CPLX1 (a), DLGAP3 (b), ATP6V0C (c), and TTBK1 (d) were evaluated using the TCGA GBM RNA-Seq database. In all the comparisons normal adjacent brain tissues (Normal, n = 5) and pGBM (n = 156) were included in the analysis. Data represent the mean ± SD. *p < 0.05, ****p < 0.0001.
Discussion
During the last years, several efforts have been made to address three separate challenges in the clinical management of GBM patients: diagnosis, prognosis, and monitoring of adjuvant treatment and recurrence. CfmiRs have surged as promising molecular blood biomarkers to also address the clinical management problems of patients with GBM. The majority of previous studies have focused on single or a few miRs, which limits the landscape understanding of miR regulation and validation across different specimen cohorts. Thus, there is a critical and unmet need to find cfmiR biomarkers that aid in the identification of patients with pGBM and rGBM tumors. Early, accurate diagnosis, and early intervention have the potential to improve patient outcomes.
To meet this need, we developed a pilot study to identify potential cfmiR biomarkers in the peripheral blood of patients diagnosed with pGBM and rGBM using the HTG miR WTA. Our results found specific cfmiR signatures of differentially expressed cfmiRs in the plasma samples of patients with pGBM and rGBM in comparison to normal healthy donors. Additionally, these miRs were also detected in tumor tissues from pGBM patients. We observed the highest correlation values in miR detection in tumor tissue samples. Nonetheless, we observed a significant positive correlation between paired plasma and tumor samples obtained from pGBM patients for the comprehensive panel of the miRs assessed, suggesting that specific cfmiRs detected in the plasma may have been released by pGBM tumors. Thus, HTG miR WTA assay may complement other techniques apply to the diagnose of brain tumors such as conventional MRI and magnetic resonance spectroscopy (MRS)25. MRS is a non-invasive and innovative technique that analyzes specific metabolites and allows for the identification of GBM tumors from other types of brain tumors. Many applications of MRS have been proposed, however, some reached clinical stages while others are confined to research purposes25. Complement assessment of GBM patients with these technologies and blood biomarkers will provide better clinical decisions and healthcare for patients.
Previous studies have proposed miR-21 as a potential diagnostic, prognostic, and treatment monitoring biomarker for GBM patients13. Our results showed a significant upregulation in miR-21-5p in plasma samples from pGBM patients. Additionally, miR-21-5p is highly expressed in pGBM tumor samples. However, miR-21-5p detection levels are variable from patient to patient. Thus, the values observed in plasma may not necessarily represent changes in the pGBM tumors. In addition, miR-21-5p has been associated with various benign diseases and inflammation events, thus specificity is an issue as previously discussed by Jenike et al22.
MiR-124-3p is expressed in normal brain-specific tissue26. Our results showed that miR-124-3p is upregulated in the plasma of pGBM patients. MiR-124-3p was also detected in the tissues of pGBM patients, although, in lower quantities in comparison to other miRs. Further studies are needed to determine whether miR-124-3p has biological implications in pGBM development, or on the contrary, it is released by normal brain cells that have undergone damage or destruction due to the pGBM tumor growth.
Finding specific miRs with high sensitivity and specificity is challenging, especially for heterogeneous tumors such as pGBM. Different studies have selected miRs and then assessed them by qRT-PCR in tissues, plasma, serum, and CSF13,27. This random miR selection is biased as the miRs may not represent specific miRs released into the blood by pGBM and rGBM tumors. Our results show that specific miRs such as miR-3180-3p and miR-5739 are potential biomarkers to identify patients with rGBM. However, the sensitivity for miR-5739 was decreased in pGBM. The main reason for this observation could be due to the heterogeneity observed in pGBM, the size of the lesions, and other clinical variables that will need to be considered in a larger validation cohort.
Previous studies in non-small cell lung carcinoma have identified exosomal-miR-3180 and miR-3180-3p as regulators of cell proliferation that downregulate FOXP4 mRNA expression in gastric cancer28. In addition, miR-3180 was shown to be upregulated in cisplatin resistance gastric cancer serum samples and was able to distinguish cisplatin chemoresistance from chemosensitive patients29. MiR-5739 has been shown to play a role in embryonic stem cells regulating ENG (endoglin a major glycoprotein of the vascular endothelium) mRNA expression30. In another study, miR-5739 was proposed as part of the 4-miR signature in serum samples to predict early gastric cancer. A 4-miR signature, including miR-5739, had a sensitivity of 0.983 and a specificity of 0.977, suggesting its potential utility as a blood biomarker31. Our results suggest that miR-3180-3p and miR-5739 together or separate may help to determine pGBM or rGBM patients. However, future analysis using longitudinal bleeds would help to determine whether these cfmiRs are specific to monitor patients who had surgery for GBM tumors and are on adjuvant chemo and/or radiotherapy treatments.
Using in-silico analysis, we have identified four potential and common brain-specific target genes for miR-3180-3p and miR-5739. These four genes (CPLX1, DLGAP3, ATP6V0C, and TTBK1), predicted as miR-3180-3p and miR-5739 targets, are expressed in normal brain tissues. Surprisingly, the four genes were downregulated in pGBM tumors compared to normal adjacent brain tissues. CPLX1 codifies for complexin-1 protein, which is a component of the presynaptic compartment involved in controlling a specific process during synaptic vesicles exocytosis that mediates neurotransmitter release32. ATP6V0C gene encodes a component of vacuolar ATPase (V-ATPase). The V-ATPase is a multi-subunit enzyme that mediates organelles acidification, which is required for intracellular functions such as receptor-mediated endocytosis, the sorting of specific proteins, and the generation of synaptic vesicles proton gradients. In prostate cancer, the knockdown of ATP6V0C reduced invasion rates by decreasing the activation of MMP933, while in colorectal cancer cells ATP6V0C overexpression promotes metastasis by inducing epithelial–mesenchymal transition34. The role and function of DLGAP3 (Discs Large Homolog Associated Protein 3) are less understood and it may participate in synapses organization and neuronal cell signaling35. TTBK1 encodes for Tau-tubulin kinase-1, a kinase that is associated with Tau aggregation and phosphorylation, but also linked to Alzheimer’s Disease36. To our knowledge, there is no report for the four target genes identified in relation to GBM. Further studies are required to determine whether the downregulation of any of the four genes identified in this study is related to pGBM tumor growth; or on the contrary, these genes represent markers of neuronal de-differentiation during pGBM tumor growth because of miR-3180-3p and miR-5739 upregulation.
In conclusion, this study reports specific cfmiR signatures that allow for the identification of patients with pGBM and rGBM. MiR-3180-3p and miR-5739 were proposed as potential biomarkers for the identification of patients with pGBM and rGBM. The cfmiR signatures as well as the two miRs proposed require further validation in a larger patient multicenter study to determine their accuracy and clinical utility to assist with making clinical decisions.
Data availability
The data generated and discussed in this study have been deposited in the National Center for Biotechnology Information (NCBI) Gene Expression Omnibus (GEO) and is accessible through the GEO Series accession number GSE184472. The TCGA RNA-seq GBM dataset for mRNA was obtained from http://tcga-data.nci.nih.gov and http://gdac.broadinstitute.org/).
References
King, J. L. & Benhabbour, S. R. Glioblastoma multiforme-a look at the past and a glance at the future. Pharmaceutics 13, 1053–1064 (2021).
McKinnon, C., Nandhabalan, M., Murray, S. A. & Plaha, P. Glioblastoma: clinical presentation, diagnosis, and management. Bmj 374, 1560–1569 (2021).
Lin, S. Y., et al. Multiplex gene profiling of cell-free DNA in patients with metastatic melanoma for monitoring disease. JCO Precision Oncology https://doi.org/10.1200/po.17.00225, 1–30 (2018).
Lin, S. Y. et al. Prospective molecular profiling of circulating tumor cells from patients with melanoma receiving combinatorial immunotherapy. Clinical chemistry 66, 169–177 (2020).
Bustos, M. A. et al. A pilot study comparing the efficacy of lactate dehydrogenase levels versus circulating cell-free micrornas in monitoring responses to checkpoint inhibitor immunotherapy in metastatic melanoma patients. Cancers 12, 3361–3379 (2020).
Bustos, M. A. et al. Integrated assessment of circulating cell-free MicroRNA signatures in plasma of patients with melanoma brain metastasis. Cancers 12, 1692–1718 (2020).
Tran, K. D. et al. Assessment of cell-free microRNA by NGS whole-transcriptome analysis in cutaneous melanoma patients’ blood. Methods in molecular biology 2265, 475–486 (2021).
Wang, X. et al. Downregulation of the ubiquitin-E3 ligase RNF123 promotes upregulation of the NF-κB1 target serpinE1 in aggressive glioblastoma tumors. Cancers 12, 1081–1101 (2020).
Zhang, H., Yuan, F., Qi, Y., Liu, B. & Chen, Q. Circulating tumor cells for glioma. Frontiers in oncology 11, 607150–607159 (2021).
Bagley, S. J. et al. Clinical utility of plasma cell-free dna in adult patients with newly diagnosed glioblastoma: a pilot prospective study. Clinical cancer research: an official journal of the American Association for Cancer Research 26, 397–407 (2020).
Jelski, W. & Mroczko, B. Molecular and circulating biomarkers of brain tumors. International journal of molecular sciences 22, 7039–7050 (2021).
Aili, Y. et al. Liquid biopsy in central nervous system tumors: the potential roles of circulating miRNA and exosomes. American journal of cancer research 10, 4134–4150 (2020).
Jones, J., Nguyen, H., Drummond, K. & Morokoff, A. Circulating biomarkers for glioma: a review. Neurosurgery 88, 221–230 (2021).
Reda El Sayed, S. et al. MicroRNA therapeutics in cancer: current advances and challenges. Cancers 13, 02680–02708 (2021).
Balachandran, A. A., Larcher, L. M., Chen, S. & Veedu, R. N. Therapeutically significant microRNAs in primary and metastatic brain malignancies. Cancers 12, 2534–2563 (2020).
Arroyo, J. D. et al. Argonaute2 complexes carry a population of circulating microRNAs independent of vesicles in human plasma. Proceedings of the National Academy of Sciences of the United States of America 108, 5003–5008 (2011).
Dong, H. et al. Investigation gene and microRNA expression in glioblastoma. BMC Genomics 11, 1–10 (2010).
Wang, Q. et al. Plasma specific miRNAs as predictive biomarkers for diagnosis and prognosis of glioma. Journal of experimental & clinical cancer research: CR 31, 1–10 (2012).
Morokoff, A. et al. Serum microRNA is a biomarker for post-operative monitoring in glioma. Journal of neuro-oncology 149, 391–400 (2020).
Siegal, T. et al. Dynamics of circulating hypoxia-mediated miRNAs and tumor response in patients with high-grade glioma treated with bevacizumab. Journal of neurosurgery 125, 1008–1015 (2016).
Matos, B., Bostjancic, E., Matjasic, A., Popovic, M. & Glavac, D. Dynamic expression of 11 miRNAs in 83 consecutive primary and corresponding recurrent glioblastoma: correlation to treatment, time to recurrence, overall survival and MGMT methylation status. Radiol Oncol 52, 422–432 (2018).
Jenike, A. E. & Halushka, M. K. miR-21: a non-specific biomarker of all maladies. Biomark Res 9, 1–7 (2021).
Louis, D. N. et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta neuropathologica 131, 803–820 (2016).
Olioso, D. et al. Serum exosomal microRNA-21, 222 and 124-3p as noninvasive predictive biomarkers in newly diagnosed high-grade gliomas: a prospective study. Cancers 13, 3006–3017 (2021).
Weinberg, B. D., Kuruva, M., Shim, H. & Mullins, M. E. Clinical applications of magnetic resonance spectroscopy in brain tumors: from diagnosis to treatment. Radiol Clin North Am 59, 349–362 (2021).
Ludwig, N. et al. Distribution of miRNA expression across human tissues. Nucleic acids research 44, 3865–3877 (2016).
Kopkova, A. et al. Cerebrospinal fluid MicroRNA signatures as diagnostic biomarkers in brain tumors. Cancers 11, 1546–1558 (2019).
Chen, T. et al. Exosomal miR-3180-3p inhibits proliferation and metastasis of non-small cell lung cancer by downregulating FOXP4. Thorac Cancer 12, 372–381 (2021).
Jin, L. & Zhang, Z. Serum miR-3180-3p and miR-124-3p may function as noninvasive biomarkers of cisplatin resistance in gastric cancer. Clin Lab 66, 200302–200315 (2020).
Yoo, J. K. et al. The hsa-miR-5739 modulates the endoglin network in endothelial cells derived from human embryonic stem cells. Biochemical and biophysical research communications 415, 258–262 (2011).
Abe, S. et al. A novel combination of serum microRNAs for the detection of early gastric cancer. Gastric Cancer 24, 835–843 (2021).
Melland, H., Carr, E. M. & Gordon, S. L. Disorders of synaptic vesicle fusion machinery. J Neurochem 157, 130–164 (2021).
Zou, P. et al. Silencing of vacuolar ATPase c subunit ATP6V0C inhibits the invasion of prostate cancer cells through a LASS2/TMSG1-independent manner. Oncology reports 39, 298–306 (2018).
Wang, J. et al. ATP6L promotes metastasis of colorectal cancer by inducing epithelial-mesenchymal transition. Cancer Sci 111, 477–488 (2020).
Rasmussen, A. H., Rasmussen, H. B. & Silahtaroglu, A. The DLGAP family: neuronal expression, function and role in brain disorders. Mol Brain 10, 1–33 (2017).
Sato, S., Cerny, R. L., Buescher, J. L. & Ikezu, T. Tau-tubulin kinase 1 (TTBK1), a neuron-specific tau kinase candidate, is involved in tau phosphorylation and aggregation. J Neurochem 98, 1573–1584 (2006).
Acknowledgements
The authors thank the Department of Translational Molecular Medicine staff at SJCI, the Cancer Clinic, the Department of Pathology, PNI staff at SJHC, and Ivy Center research staff at Swedish Medical Center for their kind advisory and technical assistance.
Funding
This research was funded by the Gonda Foundation to D.S.B.H. The work performed at Swedish Medical Center was supported by the Ivy Center’s Philanthropic Research Fund.
Author information
Authors and Affiliations
Contributions
M.A.B.: conceptualization and design, methodology, data analysis and interpretation, writing original draft preparation; N.R.: bioinformatic analysis; R.I.R.: data analysis; S.R.; V.R.L.; and L.T.: performed HTG miR WTA and sequencing; R.G. FFPE tissue microdissection, plasma sample retrieval, and preparation. A.E.: clinical data retrieval; S.K..: conceptualization. Y.T.: GBM tissue pathologist review and GBM tumor identification; H.P.: clinical data retrieval; G.B.: GBM tumor surgery, clinical data, and blood collection; C.C.: GBM tumor surgery, clinical data, and blood collection; D.F.K.: GBM tumor surgery, clinical data, and blood collection; D.S.B.H.: conceptualization and design, supervision, funding, writing. All the authors reviewed, edited, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This pilot study followed the principles in the Declaration of Helsinki. Informed consent was obtained from all participants. All the human samples were de-identified and barcoded. Human samples and clinical information for this study were obtained according to the protocol guidelines approved by the SJHC/SJCI (formerly John Wayne Cancer Institute) Joint Institutional Review Board (IRB): JWCI Universal Consent (Providence Health System Portland IRB: JWCI-18-0401) and Western IRB: MORD-RTPCR-0995. Human samples and de-identified clinical information from Swedish Medical Center were obtained in accordance with Western Institutional Review Board (WIRB) approved protocols (# 20062252 and # 20091563). Tumors and plasma samples were obtained from surgeries performed at the Swedish Medical Center (Seattle, WA) according to IRB guidelines. All participants provided written informed consent according to IRB guidelines prior to participation in this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bustos, M.A., Rahimzadeh, N., Ryu, S. et al. Cell-free plasma microRNAs that identify patients with glioblastoma. Lab Invest 102, 711–721 (2022). https://doi.org/10.1038/s41374-021-00720-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41374-021-00720-4
This article is cited by
-
MiR-3180 inhibits hepatocellular carcinoma growth and metastasis by targeting lipid synthesis and uptake
Cancer Cell International (2023)
-
Recent Developments in Blood Biomarkers in Neuro-oncology
Current Neurology and Neuroscience Reports (2023)