Abstract
Tumor-associated macrophages (TAMs) constitute a large population of glioblastoma and facilitate tumor growth and invasion of tumor cells, but the underlying mechanism remains undefined. In this study, we demonstrate that chemokine (C-C motif) ligand 8 (CCL8) is highly expressed by TAMs and contributes to pseudopodia formation by GBM cells. The presence of CCL8 in the glioma microenvironment promotes progression of tumor cells. Moreover, CCL8 induces invasion and stem-like traits of GBM cells, and CCR1 and CCR5 are the main receptors that mediate CCL8-induced biological behavior. Finally, CCL8 dramatically activates ERK1/2 phosphorylation in GBM cells, and blocking TAM-secreted CCL8 by neutralized antibody significantly decreases invasion of glioma cells. Taken together, our data reveal that CCL8 is a TAM-associated factor to mediate invasion and stemness of GBM, and targeting CCL8 may provide an insight strategy for GBM treatment.
Similar content being viewed by others
Introduction
Glioblastoma (GBM) is the most frequent and fatal primary brain cancer of the adult [1, 2]. GBM patients are suffered from dismal prognoses despite treatment with multimodal therapies [3, 4]. The invasiveness and dissemination of GBM limit complete resection of tumor tissues and lead to high recurrence rates [5]. Evidence has showed that glioma stem-like cells (GSCs) facilitate tumor initiation, invasion and recurrence, and are a potential target for GBM treatment [6, 7]. GSCs represent a subpopulation of cancer cells that possess stem-like characteristics including self-renewal and tumor initiation [8, 9]. Recent studies show that cancer cells with stem-like phenotype exhibit higher invasive capabilities and contribute to poorer outcomes of patients [10, 11], but the mechanism is still unclear.
It has been confirmed that the biological behavior of GBM cells is influenced by the tumor microenvironment [12,13,14]. Infiltrating tumor-associated macrophages (TAMs) are abundant in the GBM niche, and are thought to promote the progression of GBM by increasing invasion and suppressing the immune response [15, 16]. Several studies also show that TAMs plays a critical role in GSCs-mediated tumor development [17,18,19,20], and disrupting the interaction between TAM and GSC has therapeutic potential for glioma patients [21]. However, the multilevel relationship between TAMs and CSCs is intricate [22], and how TAMs promote invasion and stem-like traits of GBM cells has not been fully defined.
Chemokine (C-C motif) ligand 8 (CCL8), also known as MCP-2, was first identified in human osteosarcoma cells [23, 24], and functions in a wide variety of inflammatory cells as a chemotactic factor [25,26,27,28,29,30]. Recently, the relationship between CCL8 and tumor cells has been explored, but its effect on different tumors is disputed. CCL8 contributes to the dissemination of breast cancer [31], and promotes the migration and invasion of esophageal squamous cell carcinoma [32]. On the other hand, it has also been reported that CCL8 inhibits growth of cervical carcinoma tumors [33] and exhibits an antitumor metastatic effect in melanoma [34]. Therefore, CCL8 may have distinct functions in different tumors, and its function on GBM has yet to be determined.
In this study, we reveal that CCL8 was highly expressed by TAMs and exhibited functional significance by increasing invasion and stem-like characteristics of GBM cells. We further identified the downstream signaling of CCL8 to mediate its biological function, and explored whether interruption of the CCL8 axis would be conducive to GBM therapy.
Materials and methods
GBM tumor specimens
Human GBM surgical specimens were obtained from the Xinqiao hospital, Army Medical University in Chongqing (China), with informed consents from patients or their guardians under an approved institutional review board protocol. The fresh GBM specimens were dissociated through collagenase I/IV, and then followed by fluorescence-activated cell sorter (FACS) to isolate TAMs by the surface marker CD14 and CD163. All procedures were performed in accordance with the principles of the Helsinki Declaration and approved by the institutional ethics committees of Southwest hospital.
Cell culture
GBM1 and GBM2 cell lines were isolated from two patients of primary GBMs (Southwest Hospital) through FACS as previously described [35]. Cells were cultured (5 × 106 cells/ml) in DMEM supplemented with 10% fetal bovine serum (FBS, HyClone), 100 U/ml penicillin-G, 100 μg/ml streptomycin, 2 mmol/l l-glutamine (Life Technologies) and incubated at 37 °C with 5% CO2.
Microscopic observation of pseudopodia formation in 3D cell culture
For 3D cell culture, hydromatrix (Sigma) was dissolved in sterile water to achieve 1% w/v stock solution (10 mg/ml). The stock solution was then diluted with DMEM (FBS-free) at a ratio of 1:2 as work solution, and added in plates at 37 °C for 30 min to form the gel. GBM cells with 2D culture were digested with 0.25% trypsin and washed with ice-cold PBS 2 times. Cells were then re-suspended with work solution of hydromatrix with CCL8 (5 ng/mL) or PBS, and seeded on the gel at a density of 5 × 104 cells/ml. After 30 min incubation at 37 °C, cells were put into live-cell imaging system (Zeiss) for 30 min at 37 °C, 5% CO2. Photomicrograph at 400X was taken immediately (time 0 h) and with an inverted of 3 min. The pseudopodia were defined as dynamical protrusions stretched from the edge of cell bodies, and the frequency of pseudopodia formation were counted during 30-min observation.
Animal experiments
C57BL/6 and NOD-SCID mice were provided by the laboratory animal centre of Army Medical University (AMU). Mice were housed in a specific-pathogen-free facility in individually ventilated cages under positive pressure and accessed to food and water ad libitum. All animal experiments were performed by the guidelines of the Hessian animal care and use committee Mice at an age between 4 and 6 weeks were chosen for allograft model. For subcutaneous tumor model, GBM1 cells (2 × 105) was coinjected with CCL8 (5 ng /mL) on the right side of the hip, and with PBS on the left side (n = 6). Same amount of CCL8 or PBS was then intratumorally injected at day 7th and 14th post transplantation. The maximum diameter (a) and minimum diameter (b) of each tumor were measured by vernier caliper and tumor volume was calculated as V = ab2/2. At 28th day, mice were sacrificed and tumors were weighted.
For orthotopical tumor model, mice were anesthetized and fixed in a stereotaxic frame and the injection site (1 mm anterior, 2.5 mm lateral right to the bregma) was exposed and sterilized. A suspension of 2 × 104 GL261 cells or 1 × 105 GBM1 in 10 μL PBS or 10 μL CCL8 (dissolved in PBS at concentration of 5 ng/μL) was injected at the depth of 3.5 mm and at a rate of 1 μL/min by a microsyringe (GAOGE Industrial, Shanghai, China). After injection, the microsyringe was immobilized for 30 s before driven out in order to prevent the outflow of tumor cells. At the 12th day, mice were sacrificed and whole brains were isolated. Tumor-bearing brains were cut into 5–10 slices, and the invasive sites were counted at a view of 100X field. All in vivo experiments were carried out in accordance with the Guide for the Care and Use of Laboratory Animals and approved by the Institutional Animal Care and Use Committee of Southwest hospital.
Flow cytometry
Cell suspensions were processed for staining of cell surface markers, including cd163 (563887, BD), CD14 (clone 61D3, 11-0149-41, ebioscience). Protocol for intracellular staining was performed by the manufacturer’s recommendations. Briefly, harvested cells were cultured with GolgiPlug (1 µL/mL, BD) for 6 h, followed by fixation and permeabilization (554714, BD). Cells were then resuspended with 50 µL of Perm/Wash™ buffer containing a predetermined optimal concentration of a fluorochrome-conjugated anti-CCL8 antibody (50-9789-42, ebioscience) or appropriate IgG control, and incubated at 4 °C for 30 min in the dark followed by three times washes. Data were collected using the BD FACSCanto II (BD) and analyzed using the FlowJo software (Tree Star Inc).
Quantitative real-time PCR
qRT–PCR was performed on a CFX96 Real-Time PCR Detection System (Bio-Rad). The sequences of primers for mouse ccl8 were used as described [28]. Primers for mouse β-actin were 5’-CAGCTTCTTTGCAGCTCCTT-3’ and reverse 5’-CACGATGGAGGGGAATACAG-3’.
Generation of human PBMC-derived macrophages
Peripheral Blood Mononuclear Cells were isolated by a density gradient using Ficoll-Paque Plus (GE Healthcare Bio-sciences) in accordance with the manufacturer’s recommendations. Monocytes were then sorted using CD14 antibody (clone 61D3, 11-0149-41,ebioscience) by FACS and immediately cultured (5 × 106 cells/ml) in RPMI 1640 supplemented with 10% FBS, 100 U/ml penicillin-G, 100 μg/ml streptomycin, 2 mmol/l l-glutamine (Life Technologies) and incubated at 37 °C with 5% CO2. To obtain macrophages, M-CSF (20 ng/ml, 216-MC, R&D) was added during 7 days culture.
Collection and generation of bone marrow-derived macrophages
BMDMs were generated by the protocol as previously described [20]. Briefly, mice were euthanized by rapid cervical dislocation. By aseptic technique, each hind leg was cut off at the hip joint with scissors, leaving the femur intact. After removing excess muscle, insert needle with cold PBS into bone marrow cavity of femur and flush bone cavity until bone cavity appears white. Cells from bone marrow were harvested and cultured with rmM-CSF (20 ng/mL, 416-ML, R&D) for 7 days at 37 °C, 5% CO2. Macrophages were then identified with anti-CD11b and anti-F4/80 antibodies by FACS, and the double-positive population was used for the next experiments.
Immunoblotting
Western analysis was performed as described [17]. Antibodies against human N-Cadherin, E-Cadherin (9782 kit, Cell signaling Technology), CD44 (3570, Cell signaling Technology), and MMP-13 (94808, Cell signaling Technology) were used to detect the expression of invasion-related proteins after treating with CCL8 (5 ng/mL) for 48 h. ERK1/2 antibody (9102, Cell Signaling Technology) and Phospho-ERK1/2 antibody (9101, Cell Signaling Technology) were used to investigate CCL8-induced ERK1/2 activation in GBM cells. Antibody against β-actin (1:2000, Santa Cruz Biotech) or Vinculin (Cell Signaling Technology) was used as internal reference. Corresponding bands were detected using Odyssey infrared imaging system (Li-COR Biosciences) and densitometric analysis was performed using ImageJ software.
Microarray analysis from the TCGA database
The gene expression in human GBMs and the information of patient survivals were analyzed using gene-profiling data from TCGA database (https://tcga-data.nci.nih.gov/tcga).
In vitro limiting dilution assay and sphere-forming assay
In vitro limiting dilution assay was performed as previously described [36] and the analysis was performed using online tool (http://bioinf.wehi.edu.au/software/elda/). Spheres with diameter >50 mm were counted.
In vitro Matrigel™ invasion assay
The invasion of the cells was assayed in BD BioCoat Matrigel™ invasion chambers (24 wells, polycarbonate filters membrane surface area 0.3 cm2, 8 µm pore size, BD) using 10% FBS as chemoattractant. Briefly, after starved with serum-free medium for 6 h, cells were counted and added to the upper chamber. CCL8 (5 ng/ml) or PBS was added to the upper chamber in a final volume of 200 μL. Lower chamber contained media with 10% FBS. After 24 h at 37 °C, noninvasive cells were mechanically removed from the upper membrane surface and the traversed cells on the lower surface were fixed with methanol and stained with 0.1% crystal violet. The migrated cells were counted with an inverted microscope. Each data point is the average number of cells in five random fields, and the mean and standard deviation (SD) of three individual wells were calculated.
Wound healing migration assay
Migration of GBM cells was investigated by wound healing migration assay. Cells were plated in 24-well culture plates using growth media containing 10% FBS. After the cells had reached confluence, in vitro scratch wounds were created by scraping the cell monolayers with a 200 μL sterile pipette tip. After washing away suspended cells with PBS, the cells were treated with PBS or CCL8 (0, 1, 5, and 10 ng/mL) and put into live-cell imaging system (Zeiss) for 24 h at 37 °C, 5% CO2. Photomicrograph was taken immediately (time 0 h) with an inverted of 3 h. Migration was quantified by counting distances from the wound edge. The experiments were performed in triplicates within each assay.
Inhibitor treatments
Bx471 (MCE), maraviroc (MCE), and SCH772984 (Selleck Chemicals) were dissolved in DMSO for in vitro studies. The concentration of inhibitors used for GBM cells was depended on reference [37,38,39,40,41] and our additional experiments.
Statistical analyses
Data are presented as means ± SEM. No statistical method was used to predetermine sample size. All data were included for statistical analyses using PASW Statistics 18 or GraphPad Prism 6.0. Statistical comparisons between groups were performed with paired or unpaired two-tailed Student’s t test. Bar graphs were presented as means ± SD. or means ± SEM., with statistical significance at *P < 0.05 or **P < 0.01.
Results
CCL8 secreted by TAMs promotes the formation of pseudopodia in glioblastoma cells
TAMs constitute up to 30% of the tumor mass and display a wide spectrum of secretions that modify tumor cells’ behavior [42, 43], but the mechanism is not fully understood. To find possible secreted factors of TAMs, we analyzed microarray data of the tumor-infiltrating myeloid cells (TIMs) and the blood monocytes from human GBM patients (Gene Expression Omnibus (GEO) database, GSE77043), and found that CCL8 was unregulated by TIMs in GBM (Fig. 1a). Although it was first identified from human osteosarcoma cells [23, 24], CCL8 can be found on human monocytes (Supplementary Fig. S1a). To explore whether CCL8 is highly expressed by TAMs, we performed FACS analysis on human specimens from five GBM patients, and found that TAMs expressed higher level of CCL8 than PBMC-derived macrophages from the corresponding patient (Fig. 1b). The Kaplan–Meier analyses of GBM patients from TCGA database showed that high expression of CCL8 is strongly related to macrophage markers CD68 and CD163 (Supplementary Fig. S1b), and predicts poorer survivals (Fig. 1c). We also performed a microarray on mouse bone marrow-derived macrophages (BMDMs) and found that CCL8 was highly expressed by M(IL-4) macrophages as compared with naïve ones (Supplementary Fig. S1c). To further explore the expression of CCL8 in glioma cells and macrophages, we employed western blot assay to detect CCL8 on two primary glioma cells, GBM1 and GBM2, as well as TAMs from a GBM patient, and found that TAMs, but not glioma cells, possessed CCL8 (Fig. 1d). In addition, we sorted tumor cells, TAMs, spleen resident macrophages and BMDMs from GL-261 orthotopical mice model, and found that the mRNA level of CCL8 was significantly lifted in TAMs as compared with tumor cells and other types of macrophage (Supplementary Fig. S1d). These data suggest that CCL8 is secreted by TAMs in GBM and may be related to glioma progression.
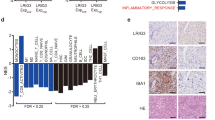
CCL8 is highly expressed by TAMs and facilitates the formation of pseudopodia in GBM cells. a Expression heatmap of the upregulated genes in human GBM infiltrating myeloid cells and blood monocytes from GEO dataset (GSE77043). b TAMs were separated from five GBM specimens and MIF of CCL8 expression was analyzed by FACS, PBMC-derived macrophages from each patient were used as comparison. P value was calculated by paired student’s t test. c Kaplan–Meier survival analysis of CCL8 expression and the overall survival of GBM patients from TCGA database. d Western blotting of CCL8 expression on primary GBM cells (GBM1 and GBM2 cells) and TAMs from GBM patient. e–g GBM cells were seeded in 3D cell culture medium with or without CCL8 (5 ng/mL), and the pseudopodia formation was dynamically observed by live-cell imaging system. Representative images of pseudopodia (white arrow) in GBM1 cells were showed (e). The numbers of pseudopodia in GBM1 (f) and GBM2 (g) cells were counted during 30-min observation. h. GBM cells were stained with rhodamine-labeled phalloidin to observe the morphology of pseudopodia under laser confocal canning microscopy. Representative images of two independent experiments were showed
One of the characteristic behaviors of GBM cells is strong locomotivity and high invasiveness [44,45,46], and the mobility of cells is proved to be supported by pseudopodia, which is F-actin-filled protrusion stretching out of the cell surface [47,48,49,50]. By using living cell station to dynamically evaluate the pseudopodia formation in Hydromatrix 3D cell culture model, we found that in the presence of CCL8 (5 ng/mL), GBM1 cells outstretched more pseudopodia than the cells in the absence of CCL8 (Fig. 1e, f and Supplementary video 1, 2). Same results were also confirmed by using another primary glioblastoma cell line (GBM2) (Fig. 1g and Supplementary Fig. S1e). The morphology of pseudopodia was further observed under a fluorescence confocal microscopy by staining F-actin (Fig. 1h). Taken together, the results prompt us to realize that CCL8 in the tumor microenvironment contributes to the migratory and invasive behavior of GBM.
CCL8 facilitates progression of glioblastoma in vivo
To determine whether CCL8 increases the development of GBM in vivo, we explored the effect of CCL8 on tumor growth by subcutaneous tumor model and found that CCL8 significantly increased the tumor volume (Fig. 2a, p < 0.001, two-way anova test) and tumor weight (Fig. 2b), suggesting that CCL8 promotes growth of GBM cells. To further investigate the pro-invasiveness function of CCL8 in GBM microenvironment, we coinjected GL-261 cells with recombinant mouse CCL8 (rmCCL8) or PBS orthotopically into the brain of C57/B6 mice, and found that the presence of CCL8 in the tumor microenvironment decreased the survival time of mice (Fig. 2c). We then evaluated aggressive status at the 12th day post implantation of tumor cells, and demonstrated that in the presence of CCL8, more tumor cells stretched from the tumor-brain frontier and formed more invasive sites beyond the tumor-brain barrier (Fig. 2d). Of notes, even though GL-261 can also express CCL8 mRNA (Supplementary Fig. S1d), knocking down CCL8 in GL-261 cells did not affect the invasion and migration abilities (Supplementary Fig. S2a–c). On the other hand, exogenous CCL8 significantly increased the invasion and migration in GL-261 cells (Supplementary Fig. S2d, e), which was consistent with the findings of in vivo experiments (Fig. 2c, d). To verify whether CCL8 can influence the in vivo behaviors of human GBM cells, we repeated the experiment by using a NOD-SCID mouse model with orthotopical transplantation of primary GBM cells, and revealed that tumor cells coinjected with recombinant human CCL8 showed more aggressive capabilities as well (Fig. 2e). In conclusion, these data indicate that CCL8 enhances GBM progression in vivo.
CCL8 promotes growth and invasion of glioma in vivo. a, b GBM1 cells with or without CCL8 were transplanted subcutaneously into the hips of NOD-SCID mice. CCL8 or PBS was then intratumorally injected at the day 7th and 14th post transplantation, and tumor volume was measured (a). b mice were sacrificed at the 28th day and tumors were weighted. c, d CCL8 shorts the survival time and increases tumor invasion in GL-261 orthotopical mice model. GL-261 cells with CCL8 (5 ng/μL) or PBS were coinjected into C57/B6 mice, and the survival time of mice were analyzed by Kaplan–Meier survival analysis (c). d At the day 12th mice were sacrificed and the invasive sites of tumor were microscopically observed and calculated. e GBM1 cells were orthotopically transplanted into NOD-SCID mice and tumor morphology was observed at day 12th
CCL8 promotes migration and invasion of glioblastoma cells
To further confirm that CCL8 impact the biological behavior of GBM cells, we performed both wound healing assay and invasive one on two primary GBM cell lines with different concentrations of CCL8 (Supplementary Fig. S3), and found that CCL8 (5 ng/mL) not only significantly increased the tumor cell migration (Fig. 3a), but also promoted the invasiveness (Fig. 3b) of GBM cells. Furthermore, recent evidence has supported the hypothesis that epithelial–mesenchymal transition (EMT) play a crucial role in the invasiveness of glioma [51, 52], and an E-cadherin to N-cadherin shift can represent the EMT status [53, 54]. By western blot, we discovered that CCL8 increased N-cadherin expression and decreased E-cadherin in glioma cells, and that tumor invasive makers (CD44 and MMP-13) were also lifted by CCL8 as well (Fig. 3c). In conclusion, the results suggest that CCL8 contribute to more invasive phenotype of GBM cells.
CCL8 increases migration, invasion, and EMT of GBM cells in vitro. a GBM cells were treated with CCL8 (5 ng/mL) or PBS, and the migration distance was calculated by wound healing assay. b GBM cells with incremental doses of CCL8 were seeded in MatrigelTM-coated transwell chambers, and the invasive cells were counted after 24 h. c CCL8 (5 ng/mL) or PBS was added into GBM cells. After 48 h, cells were harvested and the invasive markers for EMT and invasion were detected by western blot. Statistics of three independent experiments are shown. *p < 0.05; **p < 0.01; ***p < 0.001
CCL8 augments stemness of glioblastoma cells
GSCs compose a small proportion of cancer cells that exhibit potential of tumor initiation, angiogenesis, and chemotherapy resistance [7,8,9]. Accumulating evidence has also been suggesting that cancer cells with a stem-like phenotype have functional invasion capacities [10, 55,56,57]. Therefore, we assume that CCL8 facilities invasion via enhancing the stemness of GBM cells as well. By western blot, we found that the GSC markers, CD133 and SOX2, were both highly lifted after treated by CCL8 (Fig. 4a), and the addition of CCL8 in GBM cells could enhance the sphere-forming efficiency (Fig. 4b) and colony-forming capability (Fig. 4c). Of note, we observed that spheres derived from GBM cells possessed less or none CCL8 (Supplementary Fig. S4a). Thus, these data indicate that exogenous CCL8 can increase stem-like traits of GBM cells.
CCL8 augments the stem-like traits of GBM cells. a GBM cells were treated with or without CCL8 and the expression of CD133 and SOX2 were detected by Western blot. b, c CCL8 enhances clone formation of GBM cells. Cells were cultured in stem-cell medium, and sphere-forming efficiency (b) was calculated and sphere morphology (c) was detected. d, e CCR1 and CCR5 were highly expressed by GSCs. mRNA expression (d) and protein level (e) in tumor-sphere or non-sphere cells was detected by RT-PCR and FACS, respectively. f. Kaplan–Meier survival analysis of CCR1 and CCR5 expression and the overall survival of GBM patients from TCGA database. g, h The inhibitor of CCR1 or CCR5 attenuates clone-formation abilities and invasion of GBM cells. g CCL8 (5 ng/mL) was added into GBM cells together with BX471 (CCR1 inhibitor) or (and) maraviroc (CCR5 inhibitor), cells were then cultured for 14 days, and the clone numbers were calculated. h Cells were pretreated with BX471 or (and) maraviroc for 2 h, and the invasive assay were then performed. *p < 0.05; **p < 0.01; ***p < 0.001. i Western blot of CCL8 expression showed that CCR1 and CCR5 were significantly knocked down on GBM2 cells. j CCR1 or CCR5 knockdown attenuates the invasion of GBM2 cells
Similar to other Chemokine (C-C motif) ligands, CCL8 can bind to several receptors such as CCR1, CCR2B, CCR3, and CCR5 [25, 26, 30, 33, 58, 59], but which receptor responses to CCL8 in GSCs is still unclear. As shown in Fig. 4d, the mRNA level of CCR1 and CCR5 was lifted in GSCs as compared with non-GSCs, and FACS analysis also showed that GSCs possessed more protein abundances of CCR1 and CCR5 than non-GSCs (Fig. 4e). Furthermore, analysis of TCGA database demonstrated that expression of these two receptors was correlated to the expression of CCL8 (Supplementary Fig. S4b) and stem cell marker Prom1 (CD133) (Supplementary Fig. S4c). In addition, the high expression level of CCR1 or CCR5 predicted poorer survivals of glioma patients (Fig. 4f). Thus, CCR1 and CCR5 cooperated with CCL8 may play critical functions in glioma cells. To investigate the effect of CCR1 and CCR5 on the stemness and invasiveness of glioma cells, we performed clone formation analysis and invasive assays with an inhibitor specific for CCR1 (BX471) or CCR5 (maraviroc), and found that the inhibition of each receptor could attenuate the strong clone-formation ability (Fig. 4g and Supplementary Fig. S4d) and high invasiveness (Fig. 4h) caused by CCL8 in GBM cells. We further knocked down CCR1, or CCR5 or both, and found that with the addition of CCL8, cells with the knockdown of the receptor or receptors had decreased invasion abilities as compared with control, which is consistent with the inhibitor study (Fig. 4i, j). It indicates that CCR1 and CCR5 are two key receptors of CCL8 in GSCs and trigger CCL8-induced invasion of GBM cells.
CCL8 activates ERK1/2 signaling in glioblastoma cells
Several studies have been focused on the function of chemokine (C-C motif) ligands on immune cells, but the underlying mechanisms of CCL8 in tumor cells are still unclear. As showed in Fig. 5a, markedly enhanced phosphorylation of ERK1/2 by CCL8 was confirmed by immunoblotting. We also found that CCL8-induced ERK1/2 activation could be dramatically interrupted by BX471 or maraviroc (Supplementary Fig. S5). Treatment with SCH772984, an ERK1/2 inhibitor, significantly impaired CCL8-induced invasion capability (Fig. 5b) and sphere-forming efficiency of GBM cells (Fig. 5c). Furthermore, dynamical observation in 3D cell culture model showed that SCH772984 also attenuated CCL8-induced pseudopodia formation (Fig. 5d). These results suggest that ERK1/2 signal is the pivotal downstream pathway for CCL8 to mediate the invasion and stemness of glioblastoma cells. Moreover, anti-CCL8 blocking antibody significantly decreased both glioma cells migration (Fig. 5e) and ERK1/2 activation (Fig. 5f) which were mediated by supernatant of TAMs, implying that targeting TAMs-derived CCL8 secretion may provide new prospect for glioma therapy.
The activation of ERK1/2 is the pivotal downstream pathway of CCL8 to mediate biological functions in GBM cells. a Western blots show ERK1/2 expression and phosphorylation in GBM cells activated by CCL8 at different time points. Densitometry analysis was performed by ImageJ software. b Cells were pretreated with ERK1/2 inhibitor (SCH772984) for 2 h, and the invasive assay of GBM cells was performed. SCH772984 attenuates CCL8-induced sphere-formation efficiency (c) and pseudopodia formation (d) of GBM cells. e, f Blocking TAM-secreted CCL8 decreases invasion and ERK1/2 phosphorylation. The conditional medium of TAMs or naïve macrophages was added into GBM cells with or without α-CCL8 neutralizing antibody. The invasive ability of GBM cells were performed by invasive assay (e), and the phosphorylation of ERK1/2 was detected by western blot (f). *p < 0.05; **p < 0.01; ***p < 0.001
Discussion
TAMs constitute the largest population of infiltrating immunocytes in GBM microenvironment, and support malignant progression [14, 15]. Abundant infiltration of TAMs predicts poor prognosis of GBM patients [16, 17]. Our previous work has demonstrated that TGF-β and PTN secreted by TAMs participate in the initiation and progression of GBM [17, 20]. However, the multiple effects of TAMs on the invasion and stemness of GBM cells are still unknown. In this study, we found that TAMs secrete CCL8 to promote the formation of pseudopodia in GBM cells. The presence of CCL8 in the tumor microenvironment contributes to more aggressive tumor development and faster tumor growth in vivo. Furthermore, CCL8 can augment the stem-like traits of GBM cells via CCR1 and CCR5, which is the novel bond between TAMs and GSCs. In addition, we found that ERK1/2 activation is the downstream mechanism that mediates CCL8-induced invasion and stemness of GBM cells. Our study provides an insight into understanding the function of TAMs on GBM invasiveness and stemness. Blocking TAMs-derived CCL8 may be a potential therapeutic approach for GBM in the future.
The formation of pseudopodia is a temporary and spontaneous event triggered by chemical (chemotaxis) or temperature (thermotaxis) gradients or electric fields [49, 50]. The observation of pseudopodia in a three-dimensional (3D) cell culture model is superior to a 2D system because it better mimics the in vivo microenvironments and exhibits more of the behaviors of cancer cells [47]. Herein, we observed pseudopodia in a Matirx™ 3D cell culture model and discovered the effects of CCL8 on pseudopodia formation. In the presence of CCL8, tumor cells exhibited more aggressiveness by marching deeper into normal brain tissue and forming more invasive sites. Furthermore, treatment with CCL8 enhanced the expression of N-cadherin and E-cadherin in GBM cells were shifted, as well as the invasive markers (CD44 and MMP13), indicating that the CCL8 induces GBM invasion in an EMT manner.
GSCs are believed to be key to glioma cells’ invasion and recurrence [9]. It also been demonstrated that cancer cells exhibit stronger invasive abilities after turning into a stem-like phenotype [9, 10, 36, 55]. In this study, we found that the stem-like traits of GBM cells were obtained by treatment with CCL8, including the deregulation of cancer stem cell markers and the enhancement of clone-formation, indicating that CCL8 contributes to an aggressive stem-like cells of GBM. In fact, the concept of metastatic CSCs or invasive CSCs has previously been proposed [56], and our data help explain the heterogeneity of CSCs and point to a possible target for tumor therapy. Moreover, the receptors for CCL8, CCR1, CCR2B, CCR3 as well as CCR5 have been identified in various cell types [25, 31, 33, 58, 59], but it has not yet been defined which receptor(s) contribute(s) to the function of CCL8 in GSCs. We observed that among the four possible receptors for CCL8, CCR1 and CCR5 significantly unregulated in GSCs, and solely blocking each receptor could dramatically attenuate CCL8-induced invasion and clone formation. Thus, our data suggest that CCR1 and CCR5 are key receptors of CCL8 in GSCs, and simultaneously disrupting these two receptors will exhibit better effects for GBM treatment. Once secreted into the tumor microenvironment by TAMs/microglia, CCL8 can bind to its receptors CCR1/CCR5 on glioma cells. Then CCL8 can be taken up by glioma cells together with its receptor through internalization, or trigger the signal transduction in glioma cells. Due to the shared receptors of chemokine (C-C motif) ligands [59], the signal pathway of CCL8 is still undetermined. We found that CCL8 triggered the activation of ERK1/2 in GBM cells and blocking ERK1/2 signal by inhibitor weakened CCL8-induced invasion and stemness. Though ERK1/2 has been well studied in tumor initiation and development [60, 61], our data provide an option that blocking TAM-secreted CCL8 can decrease the activation of ERK1/2 in GBM.
Taken together, our data show that CCL8 is highly expressed by glioma-associated macrophages, and triggers the invasion and stemness of GBM cells through CCR1 or CCR5. The activation of ERK1/2 the downstream mechanism of CCL8 in GBM cells and blocking TAM-secreted CCL8 may therefore be a target for GBM therapy.
References
Ricard D, Idbaih A, Ducray F, Lahutte M, Hoang-Xuan K, Delattre JY. Primary brain tumours in adults. Lancet. 2012;379:1984–96.
Graeber MB, Scheithauer BW, Kreutzberg GW. Microglia in brain tumors. Glia. 2002;40:252–9.
Johnson DR, O’Neill BP. Glioblastoma survival in the United States before and during the temozolomide era. J Neurooncol. 2012;107:359–64.
Van Meir EG, Hadjipanayis CG, Norden AD, Shu HK, Wen PY, Olson JJ. Exciting new advances in neuro-oncology: the avenue to a cure for malignant glioma. CA Cancer J Clin. 2010;60:166–93.
Li XZ, Li YB, Cao Y, Li PL, Liang B, Sun JD, et al. Prognostic implications of resection extent for patients with glioblastoma multiforme: a meta-analysis. J Neurosurg Sci. 2017;61:631–9.
Park NI, Guilhamon P, Desai K, McAdam RF, Langille E, O’Connor M, et al. ASCL1 reorganizes chromatin to direct neuronal fate and suppress tumorigenicity of glioblastoma stem cells. Cell Stem Cell. 2017;21:209–24.
Fang X, Zhou W, Wu Q, Huang Z, Shi Y, Yang K, et al. Deubiquitinase USP13 maintains glioblastoma stem cells by antagonizing FBXL14-mediated Myc ubiquitination. J Exp Med. 2017;214:245–67.
Spencer DA, Auffinger BM, Murphy JP, Muroski ME, Qiao J, Gorind Y, et al. Hitting a moving target: glioma stem cells demand new approaches in glioblastoma therapy. Curr Cancer Drug Targets. 2017;17:236–54.
Lathia JD, Mack SC, Mulkearns-Hubert EE, Valentim CL, Rich JN. Cancer stem cells in glioblastoma. Genes Dev. 2015;29:1203–17.
Ji C, Yang L, Yi W, Xiang D, Wang Y, Zhou Z, et al. Capillary morphogenesis gene 2 maintains gastric cancer stem-like cell phenotype by activating a Wnt/beta-catenin pathway. Oncogene. 2018;37:3953–66.
Sengupta S, Nagalingam A, Muniraj N, Bonner MY, Mistriotis P, Afthinos A, et al. Activation of tumor suppressor LKB1 by honokiol abrogates cancer stem-like phenotype in breast cancer via inhibition of oncogenic Stat3. Oncogene. 2017;36:5709–21.
Mirzaei R, Sarkar S, Yong VW. T cell exhaustion in glioblastoma: intricacies of immune checkpoints. Trends Immunol. 2017;38:104–15.
Prionisti I, Bühler LH, Walker PR, Jolivet RB. Harnessing microglia and macrophages for the treatment of glioblastoma. Front Pharmacol. 2019;10:506
Quail DF, Joyce JA. The microenvironmental landscape of brain tumors. Cancer Cell. 2017;31:326–41.
Roesch S, Rapp C, Dettling S, Herold-Mende C. When immune cells turn bad-tumor-associated microglia/macrophages in glioma. Int J Mol Sci. 2018;19:436.
Noy R, Pollard JW. Tumor-associated macrophages: from mechanisms to therapy. Immunity. 2014;41:49–61.
Shi Y, Ping YF, Zhou W, He ZC, Chen C, Bian BS, et al. Tumour-associated macrophages secrete pleiotrophin to promote PTPRZ1 signalling in glioblastoma stem cells for tumour growth. Nat Commun. 2017;8:15080.
Otvos B, Silver DJ, Mulkearns-Hubert EE, Alvarado AG, Turaga SM, Sorensen MD, et al. Cancer stem cell-secreted macrophage migration inhibitory factor stimulates myeloid derived suppressor cell function and facilitates glioblastoma immune evasion. Stem Cells. 2016;34:2026–39.
Zhou W, Ke SQ, Huang Z, Flavahan W, Fang X, Paul J, et al. Periostin secreted by glioblastoma stem cells recruits M2 tumour-associated macrophages and promotes malignant growth. Nat Cell Biol. 2015;17:170–82.
Ye XZ, Xu SL, Xin YH, Yu SC, Ping YF, Chen L, et al. Tumor-associated microglia/macrophages enhance the invasion of glioma stem-like cells via TGF-beta1 signaling pathway. J Immunol. 2012;189:444–53.
Sarkar S, Doring A, Zemp FJ, Silva C, Lun X, Wang X, et al. Therapeutic activation of macrophages and microglia to suppress brain tumor-initiating cells. Nat Neurosci. 2014;17:46–55.
Raggi C, Mousa HS, Correnti M, Sica A, Invernizzi P. Cancer stem cells and tumor-associated macrophages: a roadmap for multitargeting strategies. Oncogene. 2016;35:671–82.
Van Damme J, Proost P, Lenaerts JP, Opdenakker G. Structural and functional identification of two human, tumor-derived monocyte chemotactic proteins (MCP-2 and MCP-3) belonging to the chemokine family. J Exp Med. 1992;176:59–65.
Decock B, Conings R, Lenaerts JP, Billiau A, Van Damme J. Identification of the monocyte chemotactic protein from human osteosarcoma cells and monocytes: detection of a novel n-terminally processed form. Biophys Res Commun. 1990;167:904–9.
Halvorsen EC, Hamilton MJ, Young A, Wadsworth BJ, LePard NE, Lee HN. et al. Maraviroc decreases CCL8-mediated migration of CCR5(+) regulatory T cells and reduces metastatic tumor growth in the lungs. Oncoimmunology. 2016;5:e1150398.
Asano K, Takahashi N, Ushiki M, Monya M, Aihara F, Kuboki E, et al. Intestinal CD169(+) macrophages initiate mucosal inflammation by secreting CCL8 that recruits inflammatory monocytes. Nat Commun. 2015;6:7802.
Severa M, Islam SA, Waggoner SN, Jiang Z, Kim ND, Ryan G, et al. The transcriptional repressor BLIMP1 curbs host defenses by suppressing expression of the chemokine CCL8. J Immunol. 2014;192:2291–304.
Islam SA, Chang DS, Colvin RA, Byrne MH, McCully ML, Moser B, et al. Mouse CCL8, a CCR8 agonist, promotes atopic dermatitis by recruiting IL-5+ T(H)2 cells. Nat Immunol. 2011;12:167–77.
Debes GF, Diehl MC. CCL8 and skin T cells-an allergic attraction. Nat Immunol. 2011;12:111–2.
Ota A, Yamamoto M, Hori T, Miyai S, Naishiro Y, Sohma H, et al. Upregulation of plasma CCL8 in mouse model of graft-vs-host disease. Exp Hematol. 2009;37:525–31.
Farmaki E, Chatzistamou I, Kaza V, Kiaris H. A CCL8 gradient drives breast cancer cell dissemination. Oncogene. 2016;35:6309–18.
Zhou J, Zheng S, Liu T, Liu Q, Chen Y, Tan D, et al. MCP2 activates NF-kappaB signaling pathway promoting the migration and invasion of ESCC cells. Cell Biol Int. 2018;42:365–72.
Struyf S, Proost P, Vandercappellen J, Dempe S, Noyens B, Nelissen S, et al. Synergistic up-regulation of MCP-2/CCL8 activity is counteracted by chemokine cleavage, limiting its inflammatory and anti-tumoral effects. Eur J Immunol. 2009;39:843–57.
Hiwatashi K, Tamiya T, Hasegawa E, Fukaya T, Hashimoto M, Kakoi K, et al. Suppression of SOCS3 in macrophages prevents cancer metastasis by modifying macrophage phase and MCP2/CCL8 induction. Cancer Lett. 2011;308:172–80.
Wang Z, Wang B, Shi Y, Xu C, Xiao HL, Ma LN. et al. Oncogenic miR-20a and miR-106a enhance the invasiveness of human glioma stem cells by directly targeting TIMP-2. Oncogene. 2015;34:1407–19.
Shi Y, Zhou W, Cheng L, Chen C, Huang Z, Fang X, et al. Tetraspanin CD9 stabilizes Gp130 by preventing its ubiquitin-dependent lysosomal degradation to promote STAT3 activation in glioma stem cells. Cell Death Differ. 2017;24:167–80.
Abravanel DL, Belka GK, Pan TC, Pant DK, Collins MA, Sterner CJ, et al. Notch promotes recurrence of dormant tumor cells following HER2/neu-targeted therapy. J Clin Invest. 2015;125:2484–96.
Lee SH, Hu W, Matulay JT, Silva MV, Owczarek TB, Kim K, et al. Tumor evolution and drug response in patient-derived organoid models of bladder. Cell. 2018;173:515–28.
Zhang C, Yi W, Li F, Du X, Wang H, Wu P. et al. Eosinophil-derived CCL-6 impairs hematopoietic stem cell homeostasis. Cell Res. 2018;28:323–35.
Liu K, Xiao C, Wang F, Xiang X, Ou A, Wei J, et al. Chemokine receptor antagonist block inflammation and therapy japanese encephalitis virus infection in mouse model. Cytokine. 2018;110:70–77.
Guo Q, Zheng K, Fan D, Zhao Y, Li L, Bian Y. et al. Wu-Tou decoction in rheumatoid arthritis: integrating network pharmacology and in vivo pharmacological evaluation. Front Pharmacol. 2017;8:230.
Chen Z, Feng X, Herting CJ, Garcia VA, Nie K, Pong WW, et al. Cellular and molecular identity of tumor-associated macrophages in glioblastoma. Cancer Res. 2017;77:2266–78.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74.
Ding AS, Routkevitch D, Jackson C, Lim M. Targeting myeloid cells in combination treatments for glioma and other tumors. Front Immunol. 2019;10:1715.
de Gooijer MC, Guillen NM, Bernards R, Wurdinger T, van Tellingen O. An experimenter’s guide to glioblastoma invasion pathways. Trends Mol Med. 2018;24:763–80.
Vehlow A, Cordes N. Invasion as target for therapy of glioblastoma multiforme. Biochim Biophys Acta. 2013;1836:236–44.
Jacquemet G, Hamidi H, Ivaska J. Filopodia in cell adhesion, 3D migration and cancer cell invasion. Curr Opin Cell Biol. 2015;36:23–31.
Klemke RL. Trespassing cancer cells: ‘fingerprinting’ invasive protrusions reveals metastatic culprits. Curr Opin Cell Biol. 2012;24:662–9.
Paul NR, Allen JL, Chapman A, Morlan-Mairal M, Zindy E, Jacquemet G, et al. Alpha5beta1 integrin recycling promotes Arp2/3-independent cancer cell invasion via the formin FHOD3. J Cell Biol. 2015;210:1013–31.
Yu X, Zech T, McDonald L, Gonzalez EG, Li A, Macpherson I, et al. N-WASP coordinates the delivery and F-actin-mediated capture of MT1-MMP at invasive pseudopods. J Cell Biol. 2012;199:527–44.
Lu Y, Xiao L, Liu Y, Wang H, Li H, Zhou Q, et al. MIR517C inhibits autophagy and the epithelial-to-mesenchymal (-like) transition phenotype in human glioblastoma through KPNA2-dependent disruption of TP53 nuclear translocation. Autophagy. 2015;11:2213–32.
Iser IC, Pereira MB, Lenz G, Wink MR. The epithelial-to-mesenchymal transition-like process in glioblastoma: an updated systematic review and in silico investigation. Med Res Rev. 2017;37:271–313.
Lv B, Yang X, Lv S, Wang L, Fan K, Shi R. et al. CXCR4 signaling induced epithelial-mesenchymal transition by PI3K/AKT and ERK pathways in glioblastoma. Mol Neurobiol. 2015;52:1263–8.
Srivastava C, Irshad K, Dikshit B, Chattopadhyay P, Sarkar C, Gupta DK, et al. FAT1 modulates EMT and stemness genes expression in hypoxic glioblastoma. Int J Cancer. 2018;142:805–12.
Tan J, Liu M, Zhang JY, Yao YL, Wang YX, Lin Y, et al. Capillary morphogenesis protein 2 is a novel prognostic biomarker and plays oncogenic roles in glioma. J Pathol. 2018;245:160–71.
Liao WT, Ye YP, Deng YJ, Bian XW, Ding YQ. Metastatic cancer stem cells: from the concept to therapeutics. Am J Stem Cells. 2014;3:46–62.
Louhichi T, Saad H, Dhiab MB, Ziadi S, Trimeche M. Stromal CD10 expression in breast cancer correlates with tumor invasion and cancer stem cell phenotype. BMC Cancer. 2018;18:49.
Ge B, Li J, Wei Z, Sun T, Song Y, Khan NU. Functional expression of CCL8 and its interaction with chemokine receptor CCR3. BMC Immunol. 2017;18:54.
Blaszczyk J, Coillie EV, Proost P, Damme JV, Opdenakker G, Bujacz GD, et al. Complete crystal structure of monocyte chemotactic protein-2, a CC chemokine that interacts with multiple receptors. Biochemistry. 2000;39:14075–81.
Samatar AA, Poulikakos PI. Targeting RAS-ERK signalling in cancer: promises and challenges. Nat Rev Drug Discov. 2014;13:928–42.
Deschenes-Simard X, Kottakis F, Meloche S, Ferbeyre G. ERKs in cancer: friends or foes? Cancer Res. 2014;74:412–9.
Acknowledgements
This work was supported by the grants from the National Science Foundation of China (81773145 and 81372273) to XZ, the National Key Research and Development Program of China (2017YFC1309004 to XZ and 2016YFA0101203 to XWB) and the Basic and Applied Fund of First Affiliated Hospital of Army Military Medical University (SWH2016JCZD-04) to XZ.
Author information
Authors and Affiliations
Contributions
Conceptualization: X(xia)Z and XWB; methodology: XZ, WQD, LC, HML, JYM, MFC, JFX and XDL; formal analysis: XZ, X(xia)Z; resources: XHY, SCY, YFP, YHC, WJJ, YW, X(xia)Z and SQL; writing of original draft: XZ; manuscript review and editing: all authors; supervision: X(xia)Z, and XWB.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, X., Chen, L., Dang, Wq. et al. CCL8 secreted by tumor-associated macrophages promotes invasion and stemness of glioblastoma cells via ERK1/2 signaling. Lab Invest 100, 619–629 (2020). https://doi.org/10.1038/s41374-019-0345-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41374-019-0345-3
This article is cited by
-
Single-cell RNA sequencing reveals recruitment of the M2-like CCL8high macrophages in Lewis lung carcinoma-bearing mice following hypofractionated radiotherapy
Journal of Translational Medicine (2024)
-
From complexity to clarity: unravelling tumor heterogeneity through the lens of tumor microenvironment for innovative cancer therapy
Histochemistry and Cell Biology (2024)
-
Fasting mimicking diet inhibits tumor-associated macrophage survival and pro-tumor function in hypoxia: implications for combination therapy with anti-angiogenic agent
Journal of Translational Medicine (2023)
-
Macrophage’s role in solid tumors: two edges of a sword
Cancer Cell International (2023)
-
Macrophages in immunoregulation and therapeutics
Signal Transduction and Targeted Therapy (2023)