Abstract
Although inhibition of epidermal growth factor receptor (EGFR)-mediated cell signaling by the EGFR tyrosine kinase inhibitor gefitinib is highly effective against advanced non-small cell lung cancer, this drug might promote severe acute interstitial pneumonia. We previously reported that molecular hydrogen (H2) acts as a therapeutic and preventive anti-oxidant. Here, we show that treatment with H2 effectively protects the lungs of mice from severe damage caused by oral administration of gefitinib after intraperitoneal injection of naphthalene, the toxicity of which is related to oxidative stress. Drinking H2−rich water ad libitum mitigated naphthalene/gefitinib-induced weight loss and significantly improved survival, which was associated with a decrease in lung inflammation and inflammatory cytokines in the bronchoalveolar lavage fluid. Naphthalene decreased glutathione in the lung, increased malondialdehyde in the plasma, and increased 4-hydroxy-2-nonenal production in airway cells, all of which were mitigated by H2-rich water, indicating that the H2-rich water reverses cellular damage to the bronchial wall caused by oxidative stress. Finally, treatment with H2 did not interfere with the anti-tumor effects of gefitinib on a lung cancer cell line in vitro or on tumor-bearing mice in vivo. These results indicate that H2-rich water has the potential to improve quality of life during gefitinib therapy by mitigating lung injury without impairing anti-tumor activity.
Similar content being viewed by others
Introduction
Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors, including gefitinib, display dramatic therapeutic efficacy in non-small cell lung cancer patients that have EGFR-activating mutations, and are recommended as the standard first-line therapy in non-small cell lung cancer [1]. However, despite excellent clinical responses, this drug might promote severe and lethal interstitial lung disease (ILD) that restricts the therapeutic efficacy of this agent. In addition, the incidence of gefitinib-associated ILD appears comparatively higher in Asians than in Caucasians, reported in Japan at 4.5% as compared with that of 0.3% in USA [2, 3]. However, no specific treatment is available for gefitinib-associated ILD, and mortality of the disease is an approximate 30–40%. Thus, acute and innovative treatment strategies are needed to overcome the lethal side-effect of gefitinib. Other risk factors for this side effect of gefitinib include older age, a history of smoking, and pre-existing interstitial pneumonia, suggesting that there is a connection between airway injury and alveolar dysfunction [4].
It was recently reported that administration of gefitinib to mice after treatment with naphthalene worsened their lung injury [5]. Naphthalene, an aromatic hydrocarbon, is metabolized in the lung to reactive intermediates that enhance oxidative stress via glutathione depletion, lipid peroxidation, and production of reactive oxygen species (ROS), including superoxide anion (O2−·) and hydroxyl radical (·OH). Naphthalene selectively injures the non-ciliated epithelial cells of intrapulmonary airways, namely, Clara cells, leading to acute lung injury [6, 7], and increases both EGF and EGFR expression in the epithelial cells of distal bronchioles [8]. Inhibition of EGFR in these repairing epithelial cells with gefitinib prolonged the inflammation in mice [5], indicating that administration of gefitinib after treatment with naphthalene is a useful model for studying oxidative stress-induced lung injury caused by gefitinib.
Molecular hydrogen (H2) specifically quenches detrimental ROS (·OH), while maintaining the metabolic oxidation-reduction reaction and other less potent ROS, such as hydrogen peroxide (H2O2), O2−·, and nitric oxide (NO·). H2 is cell membrane-permeable and can easily target organelles, including mitochondria and nuclei [9]. In fact, H2 suppresses oxidative stress-induced injury in several organs, such as ischemic injury in the brain [9, 10], liver [11], heart [12], and retina [13]. Thus, H2 is a novel anti-oxidant and could be widely used in medical applications as a safe and effective anti-oxidant with minimal toxicity [14, 15].
We reported previously that H2 acts as a radioprotector in the lung. H2 scavenged ·OH and protected against apoptotic damage related to oxidative stress induced by irradiation of cultured lung epithelial cells. In addition, inhalation of H2 gas during irradiation and drinking H2-rich water after irradiation reduced lung tissue damage induced by oxidative stress in mice [16]. Moreover, oral intake of H2 by drinking H2-rich water reduced tissue damage in animal models of cisplatin-induced toxicity in the kidney [17], anti-type II collagen antibody-induced arthritis [18], liver fibrogenesis [19], and lipopolysaccharide-induced sepsis [20]. In clinical studies, oral intake of H2-rich water improved diabetes mellitus type II [21], metabolic syndrome [22], muscle fatigue [23], Parkinson’s disease [24], and Alzheimer’s disease [25] in human patients.
In the current study, we examined the therapeutic effects of H2 against gefitinib-induced lung injury. We found that drinking H2-rich water ameliorated the lung injury induced by administration of naphthalene and gefitinib without affecting the anti-tumor activity of gefitinib.
Materials and methods
Production of H2-rich water
H2-rich water was prepared using a method described previously [16]. Briefly, H2 gas (purity > 99.999%; Iwatani, Tokyo, Japan) was dissolved in reverse-osmosis water under high pressure (0.4 MPa) to a super-saturated level in a stainless steel tank (Unicontrols, Tokyo, Japan). During preparation of H2-rich water, the H2 concentration in the air was carefully monitored using a H2 sensor with an alarm, for safety. The saturated water was poured into 70 mL glass vessels equipped with an outlet line containing two ball bearings, which prevented the water from being degassed, and have a half-life of approximately 1 day. The H2 concentration in the water was measured using a needle-type H2 sensor (Unisense, Aarhus N, Denmark). H2-rich water was approximately 80% saturated (640 μM) at 0.1 MPa at room temperature. Water obtained by degassing H2 from H2-rich water with gentle stirring overnight was used as a control.
Animal model of naphthalene/gefitinib-induced lung injury
C57BL/6 J female mice (7-week-old, specific pathogen-free) were purchased from Japan SLC, Inc. (Hamamatsu, Japan). Mice were housed three to five per cage at 20–22 °C with a 12 h light/dark cycle. All efforts were made to minimize the number of animals used and their suffering during experimental procedures. All protocols for animal use followed the Principles of Laboratory Animal Care [National Institutes of Health (NIH) publication no. 86-23, revised 1985]. All study protocols were reviewed and approved by the Animal Care Committee of the Tokyo Metropolitan Institute of Gerontology. Animals were sacrificed at predetermined endpoints by CO2 asphyxiation followed by exsanguination under deep anesthesia according to a method described previously [26]. In brief, three different anesthetic agents [0.75 mg/kg medetomidine hydrochloride (Domitol; Meiji Seika Pharma, Tokyo, Japan), 4 mg/kg midazolam (Dormicum; Astellas Pharma, Tokyo, Japan), and 5 mg/kg butorphanol (Vetorphale; Meiji Seika Pharma)] were mixed and administered to the mice by intraperitoneal injection.
As previously described [5], naphthalene (Wako Pure Chemical Industries, Osaka, Japan) dissolved in corn oil was injected intraperitoneally at day 0 (200 mg/kg). Gefitinib (AstraZeneca, London, UK) dissolved in 1% Tween 80 (Wako) was given orally daily beginning on day 0 at 200 mg/kg/day, which is the highest dose used in xenograft models of mice (AstraZeneca). Based on the maximum serum concentration, the human standard dose corresponds to a dose in mouse between 20 and 90 mg/kg. However, to evaluate the effect of drinking H2-rich water on lung injury, we prolonged naphthalene-induced severe acute lung injury by administration of the highest dose of gefitinib. Mice were given water freely beginning on day 0, and the water vessel was refilled with fresh H2-rich or control water every day. The effect of administration of gefitinib alone or H2-rich water alone on normal lungs was described previously and no noticeable effect was observed [5, 27]. Then, mice were randomly distributed into five groups as follows: Group 1, corn oil (vehicle) with control water; Group 2, naphthalene with control water; Group 3, naphthalene with H2-rich water; Group 4, naphthalene and gefitinib with control water; and Group 5, naphthalene and gefitinib with H2-rich water. Body weight and survival were monitored daily, and mice were euthanized on selected days after naphthalene injection.
Sample collection from animal model and biochemical assays
At day 14 after naphthalene injection and measurement of body weight and survival, mice (Group 1: n = 8, Group 2: n = 8, Group 3: n = 8, Group 4: n = 11, Group 5: n = 9) were sacrificed for bronchoalveolar lavage fluid (BALF) analysis and lung histopathology. Four sets of BALF and lung tissue (3 in Group 4 and 1 in Group 5) were accidently lost. Furthermore, at day 7 after naphthalene injection, other mice (n = 8 in each group) were sacrificed for BALF analysis including total glutathione assay and lung histopathology. Two BALF samples (one in Group 1 and another in Group 5) were accidently lost. For quantitative PCR analysis, mice (Group 1: n = 10, Group 2: n = 8, Group 3: n = 7, Group 4: n = 6, Group 5: n = 8) were sacrificed at day 3 after naphthalene injection. For measurement of malondialdehyde (MDA) concentration, mice (n = 4 in each group) were sacrificed at day 3 after naphthalene injection. All mice were sacrificed via exsanguination under deep anesthesia with combined anesthetic agents according to the method described above. The trachea was cannulated, and bronchoalveolar lavage was performed with 1 mL of sterile saline, as previously described [28]. The lungs were then removed and fixed for 8 h at 4 °C in 4% paraformaldehyde in 0.1 M phosphate buffer (pH 7.4) under an inflation pressure of 20 cm H2O, after which they were embedded in paraffin.
For measurement of MDA concentration and quantitative PCR, other different sets of mice described above were sacrificed at day 3, and plasma and lung tissues were collected. Plasma concentrations of MDA were measured using assay kits (Northwest Life Science Specialties, Portland, OR) as described previously [20]. The lungs were immediately frozen at −80 °C and used for quantitative PCR analysis.
Bronchoalveolar lavage fluid
Bronchoalveolar lavage fluid (BALF) was analyzed as previously described [28]. Briefly, after centrifugation of BALF samples (1350 rpm, 10 min, 4 °C), supernatants were harvested for measurement of protein, cytokine, and chemokine concentrations, and cell pellets were resuspended in RPMI 1640 medium (ThermoFisher Scientific, Waltham, MA) and collected onto glass slides using a Cytospin 2 (Shandon, Pittsburgh, PA). A modified Giemsa staining protocol (Diff-Quick stain kit; Kokusai Shiyaku, Kobe, Japan) was used to determine differential cell counts. The number of cells (neutrophils, lymphocytes and macrophages) per mm2 was counted in 10 randomly selected fields under high-power magnification (×400). Total protein concentrations in BALF supernatants were measured using the Pierce BCA protein assay kit (ThermoFisher Scientific). The concentrations of tumor necrosis factor (TNF)-α, C–C motif chemokine 2 (CCL2)/monocyte chemotactic protein-1(MCP-1), and interleukin-6 (IL-6) in BALF supernatants were determined using mouse ELISA kits (R&D Systems, Minneapolis, MN). Total glutathione levels in BALF were measured after reducing all disulfide forms using a total glutathione assay kit according to the manufacturer’s protocol (Northwest Life Science Specialties, Vancouver, WA). Eight mice were used per group.
Histopathology of lung tissues
The lung sections were stained with hematoxylin and eosin. Fibrotic scoring was performed by a blinded pathologist according to the scale defined by Ashcroft [29]. The slices were analyzed with a microscope using an ×10 objective. Immunohistochemistry was performed using a previously described protocol (Histofine SAB-PO kit; Nichirei, Tokyo, Japan) [16]. Sections were stained with a rabbit polyclonal anti-CD3 antibody (1:200; Dako, Carpinteria, CA), a rat monoclonal anti-F4/80 antibody (clone CI-A3-1, 1:100; Novus Biologicals, Littleton, CO), a goat polyclonal anti-CCL2/MCP-1 antibody (1:50; Santa Cruz Biotechnology, Santa Cruz, CA), a rabbit polyclonal anti-Clara cell secretory protein (CCSP) antibody (1:500; EMD Millipore, Temecula, CA), a mouse monoclonal anti-IL-6 antibody (1:100; Leica, Wetzlar, Germany), or a mouse monoclonal anti-4-hydroxy-2-nonenal (4-HNE) antibody (1:20; Nikken SEIL, Shizuoka, Japan). For each mouse, 10 terminal bronchi were chosen and the numbers of immune cells and total bronchiolar epithelial cells were counted. At least five mice were used per group.
Quantitative PCR
Total RNA was extracted from the lung using the RNeasy plus mini kit (Qiagen, Valencia, CA) and reverse-transcribed using a first-strand synthesis system (SuperScript II, ThermoFisher Scientific). Quantitative PCR analysis was performed using SYBR Green (Toyobo, Osaka, Japan) on the StepOnePlus real-time PCR system (ThermoFisher Scientific). The primers and probes used are listed in Table 1. The relative gene expression was calculated using the standard curve method after normalizing to the levels of the Rpl4 transcript.
Effects of hydrogen on the cytotoxicity of gefitinib in vitro
The human lung cancer cell lines A549 [American Type Culture Collection (ATCC) CCL-185] and H1975 (ATCC CRL-5908, expressing mutant EGFR [30]) were used to evaluate the effects of hydrogen on the anti-tumor activity of gefitinib in vitro. The cell lines were maintained in phenol red-free Dulbecco’s modified eagle medium (DMEM) containing 10% fetal bovine serum (FBS). We reported previously that pretreatment with H2 suppressed H2O2-induced cell death [31]. Then, to investigate the effects of pretreatment with H2 on gefitinib-induced cell death, we incubated both cell lines with H2 before administration of gefitinib. Furthermore, to investigate the effects of co-treatment with H2 and gefitinib on cell death, we incubated both cell lines with H2 just after administration of gefitinib.
To treat cells with H2, cells grown on culture dishes were set in acrylamide boxes (6.8 × 103/cm3), which were strewn with wet paper to prevent desiccation. The boxes were sealed and filled with the appropriate mixed gas at a flow rate of 1 L/min for 30 min under normal pressure. H2-rich mixed gas was composed of 20% O2, 5% CO2, 25% N2, and 50% H2. N2-rich mixed gas was composed of 20% O2, 5% CO2, and 75% N2. After the boxes were filled, cells were incubated at 37 °C for the indicated amounts of time. Immediately after incubation, the H2 and O2 concentrations in the culture medium were monitored with specific electrodes. Under H2-rich mixed gas, the H2 concentration was maintained at 390 ± 40 μM. Under both H2-rich and N2-rich mixed gases, the O2 concentration was maintained at 120 ± 10 μM.
For pretreatment of cells with H2 before administration of gefitinib, cells were incubated in a box containing the appropriate mixed gas at 37 °C for 3 h. Immediately after exposure to the mixed gas, the culture medium was replaced with DMEM containing 10% FBS with various concentrations of gefitinib (0, 0.5, 5, or 50 μM), and cells were further incubated in a conventional 5% CO2 incubator at 37 °C for 3 days. For co-treatment of cells with H2 and gefitinib, the culture medium was replaced with DMEM containing 10% FBS with various concentrations of gefitinib (0, 5, 10, or 50 μM), and cells were further incubated in a box filled with the appropriate mixed gas at 37 °C for 3 days. After incubation, cell viability was estimated by a modified 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrasodium bromide viability assay according to the manufacturer’s instructions (WST-1 assay; Dojindo Molecular Technologies, Kumamoto, Japan). Three independent experiments were performed, each using eight wells per concentration of gefitinib.
Effects of H2-rich water on the anti-tumor activity of gefitinib in vivo
To evaluate the effects of hydrogen on the anti-tumor activity of gefitinib in vivo, A549 cells were stably transfected with the luciferase-expressing pGL4.50 [luc2/CMV/Hygro] vector (Promega, Madison, WI), to allow tracking of tumor cells (A549-luc2). A549-luc2 cells (6.3 × 106 cells) were suspended in 100 μL of Matrigel (Corning, Tewksbury, MA) and subcutaneously implanted onto the dorsal flank of nude mice (BALB/c-nu, 7 week-old, female; Charles River, Yokohama, Japan) 7 days before gefitinib treatment was initiated. The mice were randomly divided into three groups as follows: corn oil (vehicle) with control water (n = 7), gefitinib with control water (n = 7), and gefitinib with H2-rich water (n = 9). The first group received physiological saline orally as a control, and the second and third groups received gefitinib (200 mg/kg/day) orally for 28 days with or without H2-rich water supplied ad libitum. Body weights and tumor sizes were measured manually with calipers at days 0, 7, 14, 21, and 28 after the start of gefitinib administration. For bioluminescent imaging, mice were given an intraperitoneal injection of 75 mg/kg luciferin (OZ Biosciences, Marseille, France) suspended in saline. After 30 min, mice were anesthetized with isoflurane by inhalation (5% isoflurane at 0.5 L/min air flow) and placed on the heated imaging platform of the optical imaging system (In-Vivo Xtreme; Bruker, Billerica, MA) with isoflurane anesthesia during the imaging procedure (2% with 0.9 L/min air flow). Luciferase-active images were obtained for 10 s.
Statistical analysis
Statistical analyses were performed using SPSS software (SAS, Cary, NC). Survival rates were analyzed by log-rank tests. Statistically significant differences among groups were determined by a nonparametric Kruskal–Wallis test followed by Dunn’s multiple comparisons test. Differences between two independent groups treated with and without H2 were evaluated with Student’s t-test. All values are presented as the mean ± standard error of the mean (SEM). For Results were considered significant at P < 0.05.
Results
H2-rich water reduced mortality and body weight loss induced by naphthalene/gefitinib
Body weight was monitored for 2 weeks in mice treated with naphthalene and gefitinib, because body weight loss is a good marker for the severity of naphthalene toxicity [7]. Treatment with naphthalene alone induced a significant decrease in body weight at day 4 compared with the vehicle control, but by day 7, the naphthalene-treated mice weighed the same as the control mice (Fig. 1a, b). By contrast, the administration of gefitinib after treatment with naphthalene worsened the body weight loss and resulted in 12.5% mortality at day 4. At day 14, the body weights of mice treated with gefitinib after naphthalene were still significantly decreased compared with those of control mice. Noteworthy, drinking H2-rich water ad libitum (H2 treatment) significantly mitigated naphthalene/gefitinib-induced weight loss at day 4 (Fig. 1b) and, by day 7, naphthalene/gefitinib-treated mice drinking H2-rich water weighed the same as the control mice (Fig. 1a) and significantly improved the survival rate, with 0% mortality at day 14. All mice in each group without ones in naphthalene/gefitinib-treated mice drinking control water group survived and only survival curves of naphthalene/gefitinib-treated mice with or without H2-rich water are shown (Fig. 1c).
Suppression of naphthalene/gefitinib-induced body weight loss and mortality by H2-rich water. Changes in body weight during the study period (a) and at day 4 (b) after injection of naphthalene (N) or corn oil (O) (vehicle). Mice were given control water (CW) or H2-rich water (HW) freely, with or without oral administration of gefitinib (G). Data are expressed as the mean ± SEM. Mice were divided into five groups as follows: O with CW (n = 8), N with CW (n = 8), N with HW (n = 8), N + G with CW (n = 11), and N + G with HW (n = 9). **P < 0.01 vs. the control group (O with CW) in a. **P < 0.01 in b. Kaplan-Meier curve representing the survival of mice treated with naphthalene and gefitinib (c). All mice in each group without ones in N + G with CW group survived and only survival curves of N + G with CW and N + G with HW groups are shown. P, log-rank test
H2-rich water decreased lung inflammation and inflammatory cytokines in the BALF
The cellular composition of the BALF was evaluated to determine the effects of H2-rich water on the degree of inflammatory cell infiltration in the lung. At day 7, the numbers of total cells including neutrophils, lymphocytes and macrophages (Fig. 2a), were significantly increased in the BALF of mice administered naphthalene with or without gefitinib, compared with vehicle-treated mice (Fig. 2b). H2 treatment suppressed this increase in lung inflammation in both naphthalene-treated and naphthalene/gefitinib-treated mice. By day 14, the inflammation had resolved in mice administered only naphthalene; however, administration of gefitinib after naphthalene prolonged the inflammation (Fig. 2c). Notably, H2 treatment significantly mitigated the increased inflammation seen in naphthalene/gefitinib-treated mice at day 14.
Suppression of naphthalene/gefitinib-induced inflammation by H2-rich water. Modified Giemsa staining of inflammatory cells in the BALF (a) at day 7 after injection of corn oil (O) or naphthalene (N). Mice were given control water (CW) or H2-rich water (HW) freely, with or without oral administration of gefitinib (G). Numbers of cells in the BALF at days 7 (b) and 14 (c) after injection of O or N. Data are expressed as the mean ± SEM. The numbers inside bars indicate the number of mice used for analysis. *P < 0.05, **P < 0.01, ***P < 0.001
Levels of both CCL2 and IL-6 were increased in the BALF of mice administered naphthalene and gefitinib compared with mice administered vehicle at days 7 and 14 (Fig. 3a–d). H2 treatment significantly suppressed the increase in both CCL2 and IL-6. On the other hand, increased levels of TNF-α were detected in the BALF of mice administrated only naphthalene at day 7, but not at day 14 (Fig. 3e, f). Both H2 treatment and gefitinib administration significantly and independently suppressed the naphthalene-induced increase in TNF-α at day 7.
Suppression of naphthalene/gefitinib-induced inflammatory chemokines and cytokines in the BALF by H2-rich water. CCL2 (a, b), IL-6 (c, d), and TNF-α (e, f) in the BALF were measured at days 7 (a, c, e) and 14 (b, d, f) after injection of naphthalene. Mice were given H2-rich water (HW) freely. Data are expressed as the mean ± SEM. The number of mice used for analysis is shown in Fig. 2. *P < 0.05, **P < 0.01
H2-rich water protected against naphthalene/gefitinib-induced lung damage in mice
Histochemical studies of the lung showed increased numbers of inflammatory cells infiltrating the bronchial wall in naphthalene/gefitinib-treated mice (Fig. 4b, e) compared with vehicle-treated mice (Fig. 4a, d) at day 7. By contrast, H2-treated mice showed reduced numbers of infiltrating inflammatory cells in the bronchial wall (Fig. 4c, f). At day 14, infiltrating inflammatory cells had increased in number and spread into the surrounding alveolar area in naphthalene/gefitinib-treated mice (Fig. 4h, k) compared with vehicle-treated mice (Fig. 4g, j). We also found that H2-treated mice showed reduced numbers of infiltrating inflammatory cells in the bronchial wall at day 14 (Fig. 4i, l). Naphthalene/gefitinib induced a significant increase in Ashcroft scores at days 7 and 14, and H2 treatment suppressed it (Fig. 4m).
Histochemical staining of naphthalene/gefitinib-induced infiltrating inflammatory cells in the bronchial wall. Hematoxylin and eosin staining of the bronchial wall at day 7 (a–f) and day 14 (g–l) after injection of corn oil (O) or naphthalene (N). The right images (d–f and j–l) show a magnified view of the areas marked in the left images (a–c and g–i). Mice were given control water (CW) or H2-rich water (HW) freely, with or without oral administration of gefitinib (G). Scale bar: 100 mm (g–i); 50 mm (a–c, j–l); 20 mm (d–f). Aschcroft scoring (m). Data are expressed as the mean ± SEM. n = 8 in each group. *P < 0.05, **P < 0.01
The immunohistological analysis shown in Fig. 5 revealed that the inflammatory cell infiltrate in naphthalene/gefitinib-treated mice was composed primarily of F4/80 antigen-positive macrophages (Fig. 5b) and CD3-positive T lymphocytes (Fig. 5e). There was also a clear reduction in CCSP-positive Clara cells (Fig. 5h) in the bronchial walls of naphthalene/gefitinib-treated mice (Fig. 5a, d, and g) at day 7. H2-rich water suppressed the accumulation of F4/80-positive and CD3-positive cells (Fig. 5c, f) and partially inhibited the depletion of CCSP-positive cells (Fig. 5i). Both CCL2-positive and IL-6-positive cells increased in the bronchial epithelium of naphthalene/gefitinib-treated mice (Fig. 5k, n) compared with control mice (Fig. 5j and m), which is consistent with the increased levels of these cytokines in the BALF (Fig. 3). As expected, H2 treatment suppressed the naphthalene/gefitinib-induced increases in CCL2-positive and IL-6-positive cells in the lung (Fig. 5l, o).
Immunohistochemical staining of naphthalene/gefitinib-induced infiltrating inflammatory cells and reduction of Clara cells in the bronchial wall. Immunohistochemical staining for F4/80 antigen (a macrophage marker) (a, b, c), CD3 (a T lymphocyte marker) (d, e, f), CCSP (a Clara cell marker) (g, h, i), the chemokine CCL2 (j, k, l), and the cytokine IL-6 (m, n, o) in the bronchial wall at day 7 after injection of corn oil (O) or naphthalene (N). Mice were given control water (CW) or H2-rich water (HW) freely, with or without oral administration of gefitinib (G). Drinking of HW suppressed the increase in infiltrating inflammatory cells, the decrease in Clara cells, and the accumulation of inflammatory chemokines and cytokines
To clarify the protective mechanisms of drinking H2-rich water, we observed early changes of cytokine expression. Quantitative PCR analysis revealed that the administration of naphthalene both with and without gefitinib induced transcriptional expression of the inflammatory cytokines IL-6 and TNF-α in the lung at day 3 (Fig. 6a, b). H2-rich water suppressed this effect, further indicating that drinking H2-rich water can effectively regulate inflammation in the lung during the early stages of drug-induced injury.
Suppression of naphthalene/gefitinib-induced transcription of inflammatory cytokines and enzymes involved in the anti-oxidative defense system by H2-rich water. Transcript levels of inflammatory cytokines [IL-6 (a) and TNF-α (b)] and enzymes involved in the anti-oxidative defense system [heme oxygenase-1 (c), NF-E2-related factor 2 (d), glutathione reductase (e), glutamate-cysteine ligase-catalytic subunit (f), and glutathione peroxidase 1 (g)] were quantified by real-time PCR of total lung RNA at day 3 after administration of corn oil or naphthalene. Mice were given H2-rich water (HW) freely. Transcript levels are expressed relative to the levels in lungs from control mice (not treated with naphthalene, gefitinib, or HW). Mice were divided into six groups as follows: corn oil with control water (control mice, n = 10), corn oil + gefitinib with control water (n = 6), naphthalene with control water (n = 8), naphthalene with HW (n = 7), naphthalene + gefitinib with control water (n = 6), and naphthalene + gefitinib with HW (n = 8). *P < 0.05 vs. vehicle treated mice. #P < 0.05
H2-rich water reduced oxidative stress in the lung
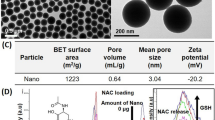
Naphthalene toxicity is related to oxidative stress [32]. Indeed, transcription of heme oxygenase 1 and glutathione reductase was induced by administration of naphthalene and suppressed by H2-rich water (Fig. 6c, e). Combined administration of naphthalene and gefitinib also increased the transcription of enzymes involved in anti-oxidative defense (Fig. 6c-g), and drinking H2-rich water suppressed an increase in the transcription of NF-E2-related factor 2 (Fig. 6d). Administration of naphthalene significantly depleted total glutathione in the BALF; treatment with H2-rich water suppressed this effect (Fig. 7a). Depletion of total glutathione induced by combined treatment with naphthalene and gefitinib was also partially suppressed by H2 treatment. To clarify the protective mechanisms of drinking H2-rich water, we observed early changes of oxidative stress. We then further examined the effect of H2 treatment on oxidative stress as determined by the plasma levels of MDA, an oxidative stress marker derived from lipid peroxides. The MDA level increased at 3 days after combined administration of naphthalene and gefitinib; this increase was significantly inhibited by H2 treatment (Fig. 7b). Furthermore, 4-HNE-positive epithelial cells increased in the bronchial walls of mice administered naphthalene and gefitinib; this was also reduced by H2 treatment (Fig. 7c–e). These results indicate that daily consumption of H2-rich water can reduce naphthalene/gefitinib-induced oxidative stress, which may suppress acute lung injury in mice.
Suppression of naphthalene/gefitinib-induced oxidative stress by H2-rich water. Total glutathione levels in BALF at day 7 (a), MDA concentrations in the plasma at day 3 (n = 4 in each group) (b), and immunohistochemical staining for 4-HNE in the bronchial wall at day 7 (c, d, e) after injection of corn oil (O) or naphthalene (N). The numbers inside bars in a indicate the number of mice used for analysis. Mice were given control water (CW) or H2-rich water (HW) freely, with or without oral administration of gefitinib (G). *P < 0.05
H2-rich water does not impair the anti-cancer activity of gefitinib
To confirm that H2 treatment would not inhibit the anti-cancer activity of gefitinib, lung cancer cell death in response to gefitinib was evaluated in vitro and in vivo. We reported previously that pretreatment with H2 suppressed oxidative stress-induced cell death [31]. First, the lung cancer cell lines A549 and H1975 were pretreated with 50% H2 gas for 3 h, then treated with gefitinib and further incubated for 3 days. The survival rate of both cell lines was reduced by administration of gefitinib in a dose-dependent manner, with no statistical difference between H2-pretreated and untreated cells (Fig. 8a, b). Next, lung cancer cell lines were treated with gefitinib and incubated for 3 days with or without 50% H2 gas. The presence of H2 during gefitinib treatment also had no effect on gefitinib-induced death in either cell line (Fig. 8c, d).
Effect of H2 on the anti-cancer activity of gefitinib. Survival of A549 and H1975 cells treated with (black bars) or without (white bars) H2 was reduced by gefitinib in a dose-dependent manner (a–d). n = 12. However, there were no differences in survival when cells were pretreated (a, b) or co-treated with H2 (c, d). Effect of drinking H2-water (HW) on the anti-cancer activity of gefitinib against lung cancer xenografts (A549-luc) (e–g). Mice were given control water or HW freely. Changes in tumor volume measured with calipers (e) and body weight (f) of mice with or without oral administration of gefitinib during the study period. The numbers in the graphs (e, f) indicate the number of mice used for analysis. Box plots of the tumor volumes expressed as photons in a region of interest (ROI) after 28 days of gefitinib administration, along with representative bioluminescent images (g). ***P < 0.0001 vs. vehicle treated mice
The effect of H2 on the anti-cancer activity of gefitinib against lung cancer xenografts in vivo was evaluated using bioluminescence imaging. Because A549-luc2 cells transplanted into BALB/c nude mice luminesce in the presence of D-luciferin, the number of emitted photons, as measured by a charge-coupled device (CCD) camera, precisely reflects the tumor size. Beginning 1 week after the injection of A549-luc2 cells (6.3 × 106 cells per mouse), when tumors were approximately 0.4 cm3, gefitinib was administered by oral gavage (200 mg/kg) once a day on 5 days per week, for 4 weeks. H2-rich or control water was supplied ad libitum. Tumor volumes were significantly decreased in mice administered gefitinib, with or without H2 treatment (Fig. 8e). Body weights also transiently and significantly decreased in mice administered gefitinib with or without H2 treatment (Fig. 8f). Notably, however, there were no differences in tumor volumes or body weights between gefitinib-treated mice according to H2 treatment. A month after the start of gefitinib administration, the tumor bioluminescence intensity in each mouse was measured (Fig. 8g). This measurement confirmed that tumors were significantly smaller in mice administered gefitinib, and that there were no differences in tumor size in mice treated with H2-rich water.
Discussion
The present study demonstrates that ingestion of H2-rich water ameliorated the lung injury induced by administration of naphthalene and gefitinib in mice, as indicated by a decrease in both inflammation and oxidative stress. Importantly, H2 treatment did not impair the anti-tumor activity of gefitinib.
The administration of naphthalene alone induced an acute body weight loss at day 4, whereas gefitinib alone did not (Fig. 1a, b). Spontaneous recovery of the body weight loss was observed at day 7 (Fig. 1a). Naphthalene alone also induced an increase in infiltrating inflammatory cells (Fig. 2b) and inflammatory chemokines (Fig. 3e, Fig. 6a, b) in the lung. H2 treatment prevented the naphthalene-induced weight loss and lung inflammation. Naphthalene has toxic effects including glutathione depletion, lipid peroxidation, and the production of ROS with Clara cell-selective cytotoxicity, all of which contribute to lung injury [6, 7]. It was reported that naphthalene undergoes stereoselective epoxidation into naphthalene 1 R,2S-oxide in murine Clara cells via cytochrome P450 2F2 (CYP2F2), which explains the cell type-selective cytotoxicity of this chemical [33, 34]. It was also reported that naphthalene-induced pulmonary toxicity was prevented by anti-oxidants such as glutathione prodrugs [7]. In this study, glutathione depletion was seen in the injured lungs of naphthalene-treated mice, and mice were protected against glutathione depletion by drinking H2-rich water (Fig. 7a), indicating that H2 treatment protects against naphthalene toxicity by reducing oxidative stress in Clara cells, thereby reducing inflammation.
Pulmonary stem cells are important in recovery from tissue injury. The progenitor cell populations in the distal airways are Clara cells, pulmonary neuroendocrine cells, and bronchioalveolar stem cells in the bronchoalveolar duct junctions [35]. It is reported that elimination of CCSP-expressing cells results in secondary alveolar inflammation, edema, and depletion of alveolar type II cells, indicating that stem cell abnormalities inhibit regeneration and promote chronic lung injury and lung fibrosis [36]. In this study, we show that administration of gefitinib after naphthalene treatment worsened the naphthalene-induced lung injury in mice, as shown by increased body weight loss (Fig. 1a, b), increased infiltration of the lung by inflammatory cells (Fig. 2a, c), and increased expression of CCL2 and IL-6 in the lung (Fig. 3b, d) compared with mice treated with naphthalene alone. However, administration of gefitinib alone did not induce changes in these parameters. Because EGFR and its ligands play important roles in the regeneration of damaged epithelium, gefitinib may suppress the regeneration of airway epithelial cells such as Clara cells in airway epithelium that is damaged by oxidative stress induced by naphthalene. This phenomenon is noted clinically, in that the patients who are the most prone to developing gefitinib-induced interstitial pneumonia have risk factors for epithelial injury of the distal airways, including older age, smoking history, and pre-existing interstitial pneumonia. These observations suggest a connection between airway injury and alveolar dysfunction [4], confirming the relevance of our mouse model for studying gefitinib-induced acute interstitial pneumonia in humans.
Drinking H2-rich water mitigated naphthalene/gefitinib-induced lung injury, with reduced body weight loss and mortality compared with control mice (Fig. 1). H2-rich water reduced inflammatory cell infiltration of the lung (Fig. 2c), the expression of IL-6 (Fig. 3d) in the BALF, and the accumulation of cells expressing CCL2 and IL-6 in the airway, and prevented the loss of CCSP-positive cells (Fig. 5). Drinking H2-rich water also mitigated naphthalene/gefitinib-induced increases in MDA in the plasma (Fig. 7b) and 4-HNE in the airway cells (Fig. 7c–e), indicating that H2-rich water mitigates the oxidative damage to Clara cells and the accompanying inflammation.
We reported previously that, 3 and 4 min after drinking H2-rich water, micromolar concentrations of H2 was detected in the blood and livers of mice, respectively, and that H2 concentrations returned to the baseline level within 30 min [20, 37]. In humans, drinking H2-rich water rapidly increased the exhaled H2 concentration to its maximal level of approximately 40 ppm by 10 min after ingestion [38]. These observations indicate that H2 is expired via the lung, a metabolic organ with a large pulmonary blood flow. Because of the loose anatomical structure of the lung, H2 can penetrate the lung epithelium and reduce toxic ROS. Even though the precise molecular mechanisms underlying the anti-oxidative effects of H2 remain to be elucidated, many studies have demonstrated that continuous drinking of H2-rich water protects against chronic oxidative damage, such as atherosclerosis in apolipoprotein E knockout mice (6 month treatment) [39], cisplatin-induced renal injury in mice (10 day treatment) [17], and chronic allograft nephropathy in rats (5 month treatment) [40]. Recently, Suzuki et al. reported that drinking H2-rich water attenuated cigarette smoke-induced emphysema in senescence marker protein 30 (SMP30) knockout mice by reducing cigarette smoke-induced oxidative DNA damage and premature cell senescence in the lungs [41]. Interestingly, Ito et al. found that intermittent H2 gas exposure, but not continuous gas exposure, prevented Parkinson’s disease in a rat model [42], suggesting that intermittent exposure to H2 by drinking H2-rich water may be an effective means of protecting against oxidative lung injury. We further demonstrated that administration of H2-rich water to mice before lipopolysaccharide injection prolonged survival and reduced oxidative stress in the liver, with increased expression of heme oxygenase-1 and reduced expression of endothelin-1. H2-rich water is likely to trigger adaptive responses against oxidative stress [20, 31].
We confirmed that treatment with H2 did not inhibit the anti-tumor activity of gefitinib in lung cancer cell lines in vitro or in tumor-bearing mice in vivo (Fig. 8). Since gefitinib acts by inhibiting EGFR signaling in non-small cell lung cancers, thereby reducing cycline-D1 expression and inhibiting proliferation of epithelial tumors [43], it seems that H2 does not interfere with the ability of gefitinib to block EGFR and its downstream signaling pathways.
In conclusion, we show here that H2 effectively protects the lungs of mice from naphthalene/gefitinib-induced toxicity because of the rapid diffusion of H2 across cell membranes in the lung and the resulting reduction in oxidative stress and inflammation. Thus, drinking H2-rich water has the potential to improve quality of life during gefitinib therapy by mitigating the pulmonary toxicity without impairing the anti-tumor activity.
References
Sim EH, Yang IA, Wood-Baker R, et al. Gefitinib for advanced non-small cell lung cancer. Cochrane Database Syst Rev. 2018;1:CD006847.
Nakagawa K, Kudoh S, Ohe Y, et al. Postmarketing surveillance study of erlotinib in Japanese patients with non-small-cell lung cancer (NSCLC): an interim analysis of 3488 patients (POLARSTAR). J Thorac Oncol. 2012;7:1296–303.
Cohen MH, Johnson JR, Chattopadhyay S, et al. Approval summary: erlotinib maintenance therapy of advanced/metastatic non-small cell lung cancer (NSCLC). Oncologist. 2010;15:1344–51.
Kudoh S, Kato H, Nishiwaki Y, et al. Interstitial lung disease in Japanese patients with lung cancer: a cohort and nested case-control study. Am J Respir Crit Care Med. 2008;177:1348–57.
Harada C, Kawaguchi T, Ogata-Suetsugu S, et al. EGFR tyrosine kinase inhibition worsens acute lung injury in mice with repairing airway epithelium. Am J Respir Crit Care Med. 2011;183:743–51.
Stohs SJ, Ohia S, Bagchi D. Naphthalene toxicity and antioxidant nutrients. Toxicology. 2002;180:97–105.
Phimister AJ, Nagasawa HT, Buckpitt AR, et al. Prevention of naphthalene-induced pulmonary toxicity by glutathione prodrugs: roles for glutathione depletion in adduct formation and cell injury. J Biochem Mol Toxicol. 2005;19:42–51.
Van Winkle LS, Isaac JM, Plopper CG. Distribution of epidermal growth factor receptor and ligands during bronchiolar epithelial repair from naphthalene-induced Clara cell injury in the mouse. Am J Pathol. 1997;151:443–59.
Ohsawa I, Ishikawa M, Takahashi K, et al. Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat Med. 2007;13:688–94.
Oláh O, Tóth-Szűki V, Temesvári P, et al. Delayed neurovascular dysfunction is alleviated by hydrogen in asphyxiated newborn pigs. Neonatology. 2013;104:79–86.
Fukuda K, Asoh S, Ishikawa M, et al. Inhalation of hydrogen gas suppresses hepatic injury caused by ischemia/reperfusion through reducing oxidative stress. Biochem Biophys Res Commun. 2007;361:670–4.
Hayashida K, Sano M, Kamimura N, et al. H2 gas improves functional outcome after cardiac arrest to an extent comparable to therapeutic hypothermia in a rat model. J Am Heart Assoc. 2012;1:e003459.
Oharazawa H, Igarashi T, Yokota T, et al. Protection of the retina by rapid diffusion of hydrogen: administration of hydrogen-loaded eye drops in retinal ischemia-reperfusion injury. Invest Ophthalmol Vis Sci. 2010;51:487–92.
Ohta S. Molecular hydrogen as a novel antioxidant: overview of the advantages of hydrogen for medical applications. Methods Enzymol. 2015;555:289–317.
Slezák J, Kura B, Frimmel K, et al. Preventive and therapeutic application of molecular hydrogen in situations with excessive production of free radicals. Physiol Res. 2016;65(Suppl 1):S11–28.
Terasaki Y, Ohsawa I, Terasaki M, et al. Hydrogen therapy attenuates irradiation-induced lung damage by reducing oxidative stress. Am J Physiol Lung Cell Mol Physiol. 2011;301:L415–426.
Nakashima-Kamimura N, Mori T, Ohsawa I, et al. Molecular hydrogen alleviates nephrotoxicity induced by an anti-cancer drug cisplatin without compromising anti-tumor activity in mice. Cancer Chemother Pharmacol. 2009;64:753–61.
Itoh T, Hamada N, Terazawa R, et al. Molecular hydrogen inhibits lipopolysaccharide/interferon γ-induced nitric oxide production through modulation of signal transduction in macrophages. Biochem Biophys Res Commun. 2011;411:143–9.
Koyama Y, Taura K, Hatano E, et al. Effects of oral intake of hydrogen water on liver fibrogenesis in mice. Hepatol Res. 2014;44:663–77.
Iketani M, Ohshiro J, Urushibara T, et al. Preadministration of hydrogen-rich water protects against lipopolysaccharide-induced sepsis and attenuates liver injury. Shock. 2017;48:85–93.
Kajiyama S, Hasegawa G, Asano M, et al. Supplementation of hydrogen-rich water improves lipid and glucose metabolism in patients with type 2 diabetes or impaired glucose tolerance. Nutr Res. 2008;28:137–43.
Nakao A, Toyoda Y, Sharma P, et al. Effectiveness of hydrogen rich water on antioxidant status of subjects with potential metabolic syndrome-an open label pilot study. J Clin Biochem Nutr. 2010;46:140–9.
Aoki K, Nakao A, Adachi T, et al. Pilot study: Effects of drinking hydrogen-rich water on muscle fatigue caused by acute exercise in elite athletes. Med Gas Res. 2012;2:12.
Yoritaka A, Takanashi M, Hirayama M, et al. Pilot study of H2 therapy in Parkinson’s disease: a randomized double-blind placebo-controlled trial. Mov Disord. 2013;28:836–9.
Nishimaki K, Asada T, Ohsawa I, et al. Effects of molecular hydrogen assessed by an animal model and a randomized clinical study on mild cognitive impairment. Curr Alzheimer Res. 2018;15:482–92.
Kawai S, Takagi Y, Kaneko S, et al. Effect of three types of mixed anesthetic agents alternate to ketamine in mice. Exp Anim. 2011;60:481–7.
Wu Q, Zhang J, Wan Y, et al. Hydrogen water alleviates lung injury induced by one-lung ventilation. J Surg Res. 2015;199:664–70.
Okuma T, Terasaki Y, Sakashita N, et al. MCP-1/CCR2 signalling pathway regulates hyperoxia-induced acute lung injury via nitric oxide production. Int J Exp Pathol. 2006;87:475–83.
Ashcroft T, Simpson JM, Timbrell V. Simple method of estimating severity of pulmonary fibrosis on a numerical scale. J Clin Pathol. 1988;41:467–70.
Shimamura T, Lowell AM, Engelman JA, et al. Epidermal growth factor receptors harboring kinase domain mutations associate with the heat shock protein 90 chaperone and are destabilized following exposure to geldanamycins. Cancer Res. 2005;65:6401–8.
Murakami Y, Ito M, Ohsawa I. Molecular hydrogen protects against oxidative stress-induced SH-SY5Y neuroblastoma cell death through the process of mitohormesis. PLoS One. 2017;12:e0176992.
Tozan A, Sehirli O, Omurtag GZ, et al. Ginkgo biloba extract reduces naphthalene-induced oxidative damage in mice. Phytother Res. 2007;21:72–77.
Buckpitt A, Chang AM, Weir A, et al. Relationship of cytochrome P450 activity to Clara cell cytotoxicity. IV. Metabolism of naphthalene and naphthalene oxide in microdissected airways from mice, rats, and hamsters. Mol Pharmacol. 1995;47:74–81.
Shultz MA, Choudary PV, Buckpitt AR. Role of murine cytochrome P-450 2F2 in metabolic activation of naphthalene and metabolism of other xenobiotics. J Pharmacol Exp Ther. 1999;290:281–8.
Wong AP, Keating A, Waddell TK. Airway regeneration: the role of the Clara cell secretory protein and the cells that express it. Cytotherapy. 2009;11:676–87.
Reynolds SD, Giangreco A, Hong KU, et al. Airway injury in lung disease pathophysiology: selective depletion of airway stem and progenitor cell pools potentiates lung inflammation and alveolar dysfunction. Am J Physiol Lung Cell Mol Physiol. 2004;287:L1256–1265.
Nagata K, Nakashima-Kamimura N, Mikami T, et al. Consumption of molecular hydrogen prevents the stress-induced impairments in hippocampus-dependent learning tasks during chronic physical restraint in mice. Neuropsychopharmacology. 2009;34:501–8.
Shimouchi A, Nose K, Shirai M, et al. Estimation of molecular hydrogen consumption in the human whole body after the ingestion of hydrogen-rich water. Adv Exp Med Biol. 2012;737:245–50.
Ohsawa I, Nishimaki K, Yamagata K, et al. Consumption of hydrogen water prevents atherosclerosis in apolipoprotein E knockout mice. Biochem Biophys Res Commun. 2008;377:1195–8.
Cardinal JS, Zhan J, Wang Y, et al. Oral hydrogen water prevents chronic allograft nephropathy in rats. Kidney Int. 2010;77:101–9.
Suzuki Y, Sato T, Sugimoto M, et al. Hydrogen-rich pure water prevents cigarette smoke-induced pulmonary emphysema in SMP30 knockout mice. Biochem Biophys Res Commun. 2017;492:74–81.
Ito M, Hirayama M, Yamai K, et al. Drinking hydrogen water and intermittent hydrogen gas exposure, but not lactulose or continuous hydrogen gas exposure, prevent 6-hydorxydopamine-induced Parkinson’s disease in rats. Med Gas Res. 2012;2:15.
Petty WJ, Dragnev KH, Memoli VA, et al. Epidermal growth factor receptor tyrosine kinase inhibition represses cyclin D1 in aerodigestive tract cancers. Clin Cancer Res. 2004;10:7547–54.
Acknowledgements
We thank Naoki Maruyama for his continuous encouragement and support. This work was supported in part by Grants-in-Aid for Scientific Research (KAKENHI) from the Japan Society for the Promotion of Science (JSPS) (Grant numbers 16K16616 and 16H03267).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Terasaki, Y., Suzuki, T., Tonaki, K. et al. Molecular hydrogen attenuates gefitinib-induced exacerbation of naphthalene-evoked acute lung injury through a reduction in oxidative stress and inflammation. Lab Invest 99, 793–806 (2019). https://doi.org/10.1038/s41374-019-0187-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41374-019-0187-z
This article is cited by
-
Inflation using hydrogen improves donor lung quality by regulating mitochondrial function during cold ischemia phase
BMC Pulmonary Medicine (2023)
-
Molecular hydrogen is a potential protective agent in the management of acute lung injury
Molecular Medicine (2022)










