Abstract
Systemic inflammatory diseases enhance circulating oxidative stress levels, which results in the oxidation of circulating high-density lipoprotein (oxHDL). Endothelial cell function can be negatively impacted by oxHDL, but the underlying mechanisms for this remain unclear. Some reports indicate that the lectin-like oxidized low-density lipoprotein receptor-1 (LOX-1) is also a receptor for oxHDL. However, it is unknown if oxHDL induces increased LOX-1 expression at the plasma membrane, as an event that supports endothelial dysfunction. Therefore, the aims of this study were to determine if oxHDL induces plasma-membrane level changes in LOX-1 and, if so, to describe the underlying mechanisms in endothelial cells. Our results demonstrate that the incubation of arterial or vein endothelial cells with oxHDL (and not HDL) induces the increase of LOX-1 expression at the plasma membrane; effect prevented by LOX-1 inhibition. Importantly, same results were observed in endothelial cells from oxHDL-treated rats. Furthermore, the observed oxHDL-induced LOX-1 expression is abolished by the down-regulation of NOX-2 expression with siRNA (and no others NOX isoforms), by the pharmacological inhibition of NAD(P)H oxidase (with DPI or apocynin) or by the inhibition of NF-κB transcription factor. Coherently, LOX-1 expression is augmented by the incubation of endothelial cells with H2O2 or GSSG even in absence of oxHDL, indicating that the NOX-2/ROS/ NF-κB axis is involved. Interestingly, oxHDL incubation also increases TNF-α expression, cytokine that induces LOX-1 expression. Thus, our results suggest a positive feedback mechanism for LOX-1 receptor during inflammatory condition where an oxidative burst will generate oxHDL from native HDL, activating LOX-1 receptor which in turn will increase the expression of NOX-2, TNF-α and LOX-1 receptor at the plasma membrane. In conclusion, oxHDL-induced translocation of LOX-1 to the plasma membrane could constitute an induction mechanism of endothelial dysfunction in systemic inflammatory diseases.
Similar content being viewed by others
Introduction
Cholesterol is distributed by various circulating lipoproteins that have varying effects on health. Two major members of the circulating lipoprotein group are low-density lipoprotein (LDL) and high-density lipoprotein (HDL) [1, 2]. LDL is correlated with adverse clinical outcomes and an increased risk of several vascular diseases. By contrast, HDL is well established as a protective factor to prevent the development of several vascular diseases, including atherosclerosis and coronary artery disease [3, 4]. HDL improves endothelial function, preserves the integrity of vascular endothelium and enhances the production of vasodilators, such as prostacyclin by the endothelium. Additionally, HDL exhibits antithrombotic activity, improves fibrinolytic capacity, and plays a significant role in promoting antioxidant and anti-inflammatory activities [2, 5, 6].
Several systemic inflammatory diseases, such as hypertension, diabetes, arthritis, atherosclerosis, obesity, and sepsis, are characterized by an over-activation of the immune system, which triggers the activation of macrophages and neutrophils and consequently increases the secretion of inflammatory mediators, such as tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), IL-6, as well as reactive oxygen species (ROS), generating pro-inflammatory and pro-oxidative reactions into the bloodstream [7,8,9,10]. Congruently, systemic inflammatory diseases are associated with severe alterations in circulatory system function because circulating inflammatory mediators act on vascular tissue. In fact, during systemic inflammatory disease, interaction between inflammatory mediators and vascular endothelial cells (ECs) is unavoidable and triggers severe endothelial dysfunction [11, 12].
Thus, a highly oxidative environment is established during systemic inflammatory disease which promotes oxidative modifications to several macromolecules [13,14,15]. As a result, lipoproteins are oxidized through the action of oxidative enzymes, and by non-enzymatic attacks by ROS as well [16, 17]. Specifically, native HDL is extensively converted into its oxidized form (oxHDL), which promotes several detrimental effects on EC function [18, 19].
Lectin-like oxidized low-density lipoprotein receptor-1 (LOX-1) is the principal endothelial receptor for oxidized low-density lipoprotein (oxLDL) [20, 21]. When LOX-1 is translocated to the plasma membrane, it can bind oxLDL to initiate multiple intracellular signaling cascades that induce endothelial dysfunction [22, 23]. Additionally, it has been shown that LOX-1 is the receptor for oxHDL, mediating its actions on ECs [24, 25].
Interestingly, several factors can upregulate the expression of LOX-1, including TGF-β1 and pro-inflammatory cytokines, such as TNF-α, IL-1β, and HDL3 modified by 15-lipoxygenase (15LO-modified HDL3) [25, 26]. The 15LO-modified HDL3 is able to increase LOX-1 expression and binds LOX-1 with higher affinity when compared to HDL3 in ECs [25]. These observations suggest that oxHDL is able to bind LOX-1 and increases LOX-1 expression by means of positive feedback.
However, it has not been determined whether such an increase LOX-1 expression also promotes LOX-1 localization to the plasma membrane, thereby increasing functional LOX-1. Additionally, the cellular mechanism by which oxHDL induces LOX-1 expression has not been well described. Therefore, the aim of this study was to determine whether oxHDL induces changes in LOX-1 expression at the plasma membrane and the underlying mechanism in ECs.
Our results showed that oxHDL, but not HDL, increases LOX-1 expression. More importantly, the intracellular distribution of LOX-1 was modified by oxHDL, which promoted a cellular distribution of LOX-1 to the plasma membrane. In contrast, native HDL did not change distribution of LOX-1 in ECs. Moreover, our results suggest that the mechanism by which oxHDL induces expression of LOX-1 to the membrane is dependent on interaction with LOX-1, and NOX-2/ROS/NF-κB pathway but independent of cytokine receptor activation.
These results will be useful in understanding the cellular effects of oxHDL on LOX-1 expression in ECs and have implications for several systemic inflammatory diseases.
Materials and methods
Artery and vein endothelial cell culture
HUVEC-derived endothelial cell line: Endothelial cell line EA hy926 (named here as HUVEC, ATCC, Manassas, VA, USA), was cultured at 37 °C in a 5%:95% CO2:air atmosphere in DMEM-low glucose (GIBCO, USA) supplemented with 10% FBS, 2 mM glutamine, and 50 U/ml penicillin–streptomycin (Sigma-Aldrich) [27]. Human aortic ECs (named here as HAEC, Lonza, Chicago, IL) were cultured in EGM-2 medium supplemented with 2% FBS. On the day before the study, the FBS concentration was reduced to 1%.
Animals, lipoprotein administration, and primary endothelial cell isolation
Male Sprague-Dawley rats weighing 100–120 g were used. The experimental protocols were approved by the Commission of Bioethics and Biosafety of the Universidad Andres Bello. Rats were treated with saline solution (vehicle), HDL (8 mg/kg), and oxHDL (8 mg/kg) by intraperitoneal (I.P.) injection (200 µL) for 24 h. Rats were housed in individual cages with water and food ad libitum. Rat mesenteric endothelial cells (RMECs) were isolated as follows: after surgery, the mesenteric artery was occluded on its distal end and cannulated from its proximal end with a polyethylene tubing connected to a 21-gauge syringe. The mesentery was surgically removed and washed with sterile PBS. For the enzymatic isolation of RMECs, each mesenteric artery was slowly perfused in a culture hood for 5 min with 5 ml M-199 medium supplemented with 40 μl Pen/Strep (10,000 U/ml/10,000 μg/ml), 20 μl fungizone (250 μg/ml), and 12.5 mg collagenase type II. The cell suspension was centrifuged at 3000 rpm for 7 min; the pellet was reconstituted in 3 ml M-199 medium supplemented with 8 ml/l of Pen/Strep (10,000 U/ml/10,000 μg/ml), 4 ml/l of fungizone (250 μg/ml), 10% FBS, and 10% CCS. Thereafter, the cells were subjected immediately to experiments.
Oxidization of HDL
Native HDL was obtained commercially from Sigma-Aldrich Inc. (St. Louis, MO, USA) and oxidized as previously described [24] with modifications. Briefly, HDL at a final concentration of 0.5 mg/ml was incubated at 37 °C for 16 h in the presence of 50 μM CuSO4 in PBS. The reaction was stopped by storing the oxHDL at 4 °C to prevent further oxidation. The extent of lipoprotein oxidation was monitored by measuring the thiobarbituric acid reactive substances (TBARS) formation [28] with the TBARS assay kit (Cayman Chemical Company, Ann Arbor, MI USA) as recommended by the supplier. For oxHDL, a total of 12.13 ± 1.04 μM MDA was obtained vs. 2.46 ± 0.65 μM from native HDL, in a total of seven independent experiments (P ≤ 0.001). To chelate copper from the reaction, oxHDL was incubated for 5 min with 100 mg/ml CHELEX-100 (Bio-Rad Laboratories Inc., Hercules, CA USA), centrifuged at 4 °C for 1 min at 500 × g, and the pellet was discarded [29].
Cytosol-rich and plasma membrane-rich fractions
Cells were cultured to 80% confluence and then subjected to treatment. Cells were lysed in cold lysis buffer containing protease inhibitors and subjected to centrifugation at 40 × g for 5 min to remove whole cells. Supernatants were collected and used to generate the plasma membrane-rich fraction. Briefly, cells were collected, washed with ice-cold PBS, and then suspended in buffer I (2 mM ethylenediaminetetraacetic acid (EDTA), 10 mM Tris–HCl, pH 7.5). After incubation on ice for 10 min, an equal volume of buffer II (0.5 M sucrose, 0.1 M KCl, 10 mM MgCl2, 2 mM CaCl2, 2 mM EDTA, 10 mM Tris–HCl, pH 7.5) was added, and cells were lysed. Cell lysate was transferred to an ice-cold tube and subjected to centrifugation (1300 × g for 10 min) at 4 °C. The resulting pellet contained the nuclear-rich fraction. The supernatant was then subjected to centrifugation (17,000 × g for 15 min) at 4 °C. The resulting pellet contained the mitochondria-rich fraction. The supernatant was again subjected to centrifugation (80,000 × g for 60 min) at 4 °C. The resulting pellet contained the plasma membrane-rich fraction. The supernatant was subjected to a final centrifugation (150,000 × g for 3 h) at 4 °C. The resulting pellet contained the ER/Golgi-rich fraction, and the resulting supernatant contained the cytosol-rich fraction. Enrichment control and contamination evaluation were performed using specific markers for each fraction: Actin for cytosol, Na+-pump for plasma membrane, UCP2 for mitochondria, the chaperone BiP for ER-Golgi, and the Histone H1 for nuclear-rich fraction.
Western blot procedures
HAEC and HUVEC treated with vehicle, HDL, and oxHDL were lysed in cold lysis buffer, and then, proteins were extracted. Supernatants were collected and stored in the same lysis buffer. Protein extract and supernatant were subjected to SDS–PAGE, and resolved proteins were transferred to a nitrocellulose or PVDF membrane. The blocked membrane was incubated with the primary antibody against LOX-1, washed twice, and incubated with a secondary antibody. Bands were revealed using a peroxidase-conjugated IgG antibody. Tubulin and Na+-pump were used as a loading controls. Peroxidase activity was detected through enhanced chemiluminescence (Bio-Rad, CA) and images were acquired using Fotodyne FOTO/Analyst Luminary Workstations Systems (Fotodyne, Inc., Hartland, WI). Protein content was determined by densitometric scanning of immunoreactive bands, and intensity values were obtained by densitometry of individual bands normalized against tubulin or Na+-pump.
Fluorescent immunohistochemistry in fresh rat blood vessels
Fluorescent immunohistochemistry was performed to blood vessels (aorta, renal artery, renal vein, and hepatic vein) obtained from rats treated with vehicle, HDL, and oxHDL. Vessels were extracted, fixed with PFA 1% for 30 min at room temperature (RT) to avoid permeabilization and then blocked for 3 h at RT with 3% BSA in PBS. Samples were subsequently washed and incubated with a primary antibody against LOX-1. Additionally, a primary antibody against endothelial protein VE-Cadherin was used as an endothelial marker. Then, cells were washed twice and incubated with secondary antibodies. Nuclei were stained with Hoechst (Sigma).
Small interfering RNA and transfection
SiGENOME SMARTpool siRNA (four separated siRNAs per NOX-1, NOX-2, and NOX-4) were purchased from Dharmacon (Dharmacon, Lafayette, CO). In brief, HUVEC were plated overnight in 24-well plate and then transfected with 5 nmol/L siRNA using DharmaFECT 4 transfection reagent (Dharmacon) according to the manufacturer’s protocols in serum-free medium for 6 h. After 24–48 transfection, experiments were performed.
RNA isolation and RT-qPCR
RT-qPCR experiments were performed to measure LOX-1, NOX-1, NOX-2, NOX-4, and TNF-α in HAEC and HUVEC, and Oct-1 and NF-κB-p50 mRNA levels in RMEC. Total RNA was extracted with Trizol according to the manufacturer’s protocol (Invitrogen, Carlsbad, CA). DNAse I-treated RNA was used for reverse transcription using the Super Script II Kit (Invitrogen, Carlsbad, CA). Equal amounts of RNA were used as templates in each reaction. Quantitative-PCR was performed using the SYBR Green PCR Master Mix (AB Applied Biosystems, Foster City, CA). Assays were run using a Rotor-gene system (Corbet Research) instrument. Data are presented as relative mRNA levels of the gene of interest normalized to relative levels of 28S mRNA.
ROS measurements
ROS production was measured in cells treated with HDL and oxHDL for 6, 12, 18, and 12 h in the absence or presence of κ-carrageenan, DPI and apocynin, or with siRNA against NOX-1, NOX-2, and NOX-4, using DCF, Amplex Red, and DHE/HPLC methods. For DCF studies: Cells were harvested with trypsin/EDTA, washed twice in ice-cold PBS, resuspended and loaded with the cell permeant ROS-sensitive dye 2′,7′-dichlorodihydrofluorescein diacetate (DCF, 5 μM) for 15–30 min at room temperature in the dark. The labeled cells were then analyzed immediately by flow cytometry (FACSCanto, BD Biosciences, San Jose, CA). Fluorescence was measured in a microplate reader (488/610 nm excitation/emission). A minimum of 10,000 cells/sample were analyzed. Cellular dye intensity analysis was performed using FACSDiva software v4.1.1 (BD Biosciences). For Amplex Red determination: intracellular ROS was measured using the Amplex Red (Thermo Fisher Scientific, Waltham, MA, USA)/HRP method according to manufacturer’s protocol. ECs were lysed in 100 μM Amplex Red solution supplemented with 2 mUnits/ml horseradish peroxidase (HRP) and 200 mUnits/ml superoxide dismutase (SOD) and incubated in the dark for 30 min. Fluorescence was measured in a microplate reader with 540/590 nm excitation/emission. For DHE/HPLC assays: superoxide was measured using dihydroethidium (DHE) and an HPLC-based (DHE/HPLC) assay according to manufacturer’s protocol. ECs were incubated with 50 μM DHE for 30 min. DHE oxidation was then assessed by HPLC as described previously [30]. Data were normalized relative to vehicle condition at 0 time.
Reagents and inhibitors
The following reagents and inhibitors were used: NF-κB inhibitor (SC3060, 5 μM, Santa Cruz Biotechnology), TNF-α receptor inhibitor (R7050, 5 μM, Tocris), LOX-1 inhibitor κ-carrageenan (250 μg/ml, Sigma-Aldrich), neutralizing anti-LOX antibody (1:50, Abcam), NAD(P)H oxidase inhibitor, diphenyleneiodonium (DPI, 10 μM, Sigma-Aldrich), NAD(P)H oxidase inhibitor, apocynin (Apo, 10 mM, Sigma-Aldrich), cell permeable antioxidant N-Acetylcysteine (NAC, 5 mM, Tocris), and the reduced (GSH, 1 mM) and oxidizing (GSSG, 2 mM) form of glutathione (Sigma-Aldrich). All inhibitors were added 1 h before and maintained throughout the treatment. Buffers and salts were purchased from Merck Biosciences.
Data analysis
All results are presented as mean ± SD. Statistical differences were assessed by one-way analysis of variance (one-way ANOVA) (or non-parametric method Kruskal–Wallis) followed by Dunn’s post hoc test or two-way analysis of variance (two-way ANOVA) followed by Tukey post hoc test; differences were considered significant at p < 0.05. See the figure legends for the specific test used.
Results
OxHDL increases LOX-1 expression at the cellular plasma membrane through the activation of LOX-1 and NF-κB
First, we tested whether LOX-1 protein expression in vein-derived and artery-derived ECs (HUVEC-derived EAhy926 and HAEC, respectively) is modulated by oxHDL exposure. HAEC and HUVEC were treated with oxHDL (Fig. 1a, b) and HDL (Fig. 1c, d) for 12 and 24 h, and LOX-1 expression was measured (Fig. 1a–d). OxHDL-treated HAEC and HUVEC showed a significant increase in LOX-1 expression after 12 and 24 h of oxHDL exposure, respectively (Fig. 1a, b), whereas HAEC and HUVEC treated with the native form of the lipoprotein, HDL, show no modification in LOX-1 expression (Fig. 1c, d). These results suggest that oxidized HDL, but not the native form, participates in the control of LOX-1 expression. These findings are concordant with results shown previously using 15LO-modified HDL3 [30].
OxHDL increases LOX-1 expression at the cellular plasma membrane through the activation of LOX-1 and NF-κB in EC. a–d HAEC and HUVEC were exposed to oxHDL (a, b) and HDL (c, d) for 12 and 24 h, and LOX-1 expression was analyzed. Representative images from western blot experiments for detection of LOX-1 in the presence of oxHDL (50 μg/ml) (a) or HDL (50 μg/ml) (c). b and d Densitometric analyses of the experiments shown in a and c, respectively. Protein levels were normalized against tubulin, and data are expressed normalized to 0 time (N = 5). Statistical differences for HAEC and HUVEC samples were assessed by a one-way analysis of variance (ANOVA) (Kruskal–Wallis) followed by Dunn’s post hoc test. *P < 0.05, **P < 0.01, NS: non-significant. Graph bars show the mean ± SD. LOX-1 expression was measured in HAEC and HUVEC in the plasma membrane-rich (e, f) or cytosol-rich (g, h) fractions from ECs exposed to oxHDL (50 μg/ml) and HDL (50 μg/ml) for 24 h. Representative images from western blot experiments performed for detection of LOX-1 in the EC membrane-rich (e) or cytosol-rich (g) fractions, and densitometric analyses of (e) and (g) are shown in (f) and (h), respectively. Protein levels were normalized against Na+ pump in the membrane-rich fraction and against tubulin in cytosol-rich fraction. Data are expressed normalized to vehicle condition (N = 3). Statistical differences for HAEC and HUVEC samples were assessed by a one-way analysis of variance (ANOVA) (Kruskal–Wallis) followed by Dunn’s post hoc test. *P < 0.05, **P < 0.01, NS: non-significant. Graphs show the mean ± SD. Ox-HDL-induced LOX-1 mRNA expression was determined by RT-qPCR in HAEC (i) and HUVEC (j). Data are expressed normalized to 0 time (N = 3). Statistical differences for HAEC and HUVEC samples were assessed by a one-way analysis of variance (ANOVA) (Kruskal–Wallis) followed by Dunn’s post hoc test. *P < 0.05, **P < 0.01. Graph bars show the mean ± SD. LOX-1 expression was measured in ECs in the absence (–) or presence (+) of LOX-1 inhibitor κ-carrageenan (250 μg/ml) (k, l), LOX-1 neutralizing anti-LOX (1:50) (m, n), or the NF-κB inhibitor SC-3060 (5 μM) (o, p) (N = 4). All inhibitors were added 1 h before and maintained throughout the treatment. Protein levels were normalized against Na+ pump, and data are expressed normalized to vehicle condition. Statistical differences were assessed by a two-way analysis of variance (ANOVA) followed by Tukey post hoc test. **P < 0.01. Graph bars show the mean ± SD
Taking into account that plasma membrane localization is required for LOX-1 receptor to be functional, we were prompted to study whether oxHDL promotes the distribution of LOX-1 to the plasma membrane in HAEC and HUVEC. After oxHDL and HDL treatment, ECs were separated into cytosol-rich and plasma membrane-rich fractions. Fraction enrichment and purity were evaluated by measuring fraction-specific proteins, showing a strong enrichment and purity of both fractions (Supplementary Figure S1). Plasma membrane-rich fraction showed a strong accumulation of LOX-1 expression (Fig. 1e, f), whereas the cytosol-rich fraction exhibited a weak but significant decrease in LOX-1 expression at 24 h after oxHDL treatment in HUVEC, while HAEC showed no differences (Fig. 1g, h). To assess whether oxHDL increases LOX-1 at the mRNA level, we performed real-time PCR experiments. OxHDL treatment increased LOX-1 mRNA expression as early as 6 and 12 h after oxHDL induction in HAEC and HUVEC, respectively (Fig. 1i, j).
Because LOX-1 acts as a receptor for oxLDL, we wondered whether the oxHDL-induced LOX-1 expression increase at the plasma membrane is also mediated by LOX-1. To that end, HUVEC-derived ECs were exposed to oxHDL and HDL in the presence of κ-carrageenan and LOX-1 expression was measured in the plasma membrane-rich fraction. Treatment with κ-carrageenan completely abolished the increase in LOX-1 expression induced by oxHDL (Fig. 1k, l). Similar results were obtained using anti-LOX-1 as a neutralizing antibody (Fig. 1m, n). These results confirmed that oxHDL-induced LOX-1 plasma membrane accumulation is mediated by LOX-1 receptor activity.
Considering that LOX-1 receptor signaling is mediated by NF-κB activation, we tested whether NF-κB participates in the LOX-1 plasma membrane accumulation induced by oxHDL. The plasma membrane fraction obtained from oxHDL-treated HUVEC-derived ECs in the presence of the NF-κB inhibitor, SC3060, showed no significant increase of LOX-1 expression (Fig. 1o, p), suggesting that NF-κB activation is required for LOX-1 accumulation at the plasma membrane induced by oxHDL.
The cytosol-rich fraction exhibited no detectable change in LOX-1 level when HUVEC-derived ECs were exposed to κ-carrageenan, anti-LOX-1, and SC3060 (data not shown).
In vivo oxHDL administration increases LOX-1 expression at the endothelial cellular plasma membrane
To demonstrate that oxHDL increases LOX-1 expression in vivo, rats were treated with oxHDL, native HDL, and saline solution (vehicle) for 24 h. After treatment, aorta, renal artery, renal vein, and hepatic vein were extracted to perform fluorescence immunohistochemistry to determine LOX-1 expression in freshly prepared endothelium monolayers from those vessels (Fig. 2a–l, respectively). Our results showed that LOX-1 expression was increased in arteries and veins from oxHDL-treated rats compared with those from HDL-treated or vehicle-treated rats. Because experiments were performed in nonpermeabilized tissues, the results showed principally LOX-1 changes at the cellular plasma membrane. During treatment, rats were subjected to systolic blood pressure determinations, and oxHDL-treated rats showed no change in systolic blood pressure compared with vehicle-treated rats. Furthermore, HDL-treated rats showed decreased systolic blood pressure compared with vehicle-treated and oxHDL-treated rats, similar to results by Speer et al. [19] (Supplementary Figure S2).
In vivo oxHDL administration increases LOX-1 expression at the endothelial cellular plasma membrane. Rats were intraperitoneally treated with vehicle (a, d, g and j), HDL (b, e, h and k), and oxHDL (c, f, i and l) for 24 h. After treatment, the aorta (a–c), renal artery (d–f), renal vein (g–i), and hepatic vein (j–l) were extracted and subjected to fluorescence immunohistochemistry to determine LOX-1 (green) expression. Immunohistochemistry was also performed using the endothelial protein VE-Cadherin (red). Nuclei were stained with Hoechst (Sigma). Scale bar = 50 μm. Representative images from western blot experiments performed to detect LOX-1 in the plasma membrane-rich fraction in RMECs from vehicle-treated, HDL-treated, and oxHDL-treated rats (m). Densitometric analyses of (m) are shown in (n). The protein levels were normalized against the Na+ pump. The data are expressed normalized to the vehicle condition (N = 3). Statistical differences were assessed using one-way analysis of variance (ANOVA) (Kruskal–Wallis), followed by Dunn’s post-hoc test. **P < 0.01. Graph bars show the means ± SD. Ox-HDL-induced Oct-1 (o) and NF-κB-p50 (p) mRNA expression was determined by RT-qPCR in RMECs from vehicle-treated, HDL-treated, and oxHDL-treated rats. The data are expressed normalized to the vehicle condition (N = 3). Statistical differences for HAEC and HUVEC samples were assessed by one-way analysis of variance (ANOVA) (Kruskal–Wallis) followed by Dunn’s post-hoc test. **P < 0.01. Graph bars show the means ± SD
Additionally, we extracted primary mesenteric endothelial cells (RMECs) from rats treated with oxHDL, native HDL, and vehicle to determine changes in LOX levels in the plasma membrane-rich fraction. In the extracted RMEC samples, we performed western blotting to assess whether oxHDL-treatment induced LOX-1 expression at the plasma membrane level. The results showed that LOX-1 expression was increased in RMECs from oxHDL-treated rats compared with that in HDL-treated or vehicle-treated rats (Fig. 2m, n). Because experiments were performed using plasma membrane-rich fractions, the results correspond principally to LOX-1 changes at the cellular plasma membrane. Fraction enrichment and purity were evaluated by measuring fraction-specific proteins (Supplementary Figure S1).
To assess whether oxHDL-treated rats showed increased LOX-1 activity, we measured mRNA levels of Oct-1 and NF-κB, which are transcription factors induced by downstream LOX-1 activation [24, 25, 31]. The results showed that the mRNA expression levels of both Oct-1 and NF-κB were increased in RMECs from oxHDL-treated rats compared with those from HDL-treated or vehicle-treated rats, suggesting that LOX-1 is more active in ECs from oxHDL-treated rats (Fig. 2o, p, respectively).
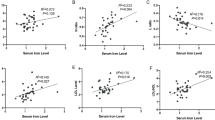
OxHDL increases LOX-1 expression at the cellular plasma membrane through the ROS/NOX-2 oxidase pathway
Taking into consideration that ROS are involved in several processes of protein expression and cellular localization, the involvement of these reactive molecules in the increase of LOX-1 expression at the cellular plasma membrane was analyzed. First, we assessed ROS generation induced by oxHDL with three different approaches, DCF, Amplex Red, and DHE/HPLC methods. HAEC and HUVEC exposed to oxHDL showed a strong increase in oxidative stress after 6 h of treatment (Fig. 3a–k). OxHDL-treated HAEC and HUVEC exposed to κ-carrageenan treatment abolished the oxHDL-induced ROS generation, confirming that LOX-1 is involved in this process (Fig. 3b–l). OxHDL-treated HAEC and HUVEC incubated with the NAD(P)H oxidase inhibitors DPI and apocynin showed an efficient inhibition of oxHDL-induced ROS generation (Fig. 3c–m), suggesting that NOX is involved.
OxHDL increases LOX-1 expression at the cellular plasma membrane through the ROS/NOX-2 pathway. Endothelial ROS were determined by means of the ROS-sensitive dye, DCF (a), Amplex red (f), and DHE/HPLC (k), in HAEC and HUVEC exposed to oxHDL (50 μg/ml) and HDL (50 μg/ml) for 0, 6, 12, 18, and 24 h (N = 6). Endothelial ROS were determined by means of the ROS-sensitive dye, DCF (b), Amplex red (g) and DHE/HPLC (l), in HAEC and HUVEC exposed to vehicle, oxHDL (50 μg/ml) and HDL (50 μg/ml) in the absence (–) or presence (+) of κ-carrageenan (250 μg/ml) for 6 h (N = 6). Endothelial ROS were determined by means of the ROS-sensitive dye, DCF (c), Amplex red (h), and DHE/HPLC (m), in HAEC and HUVEC exposed to vehicle and oxHDL (50 μg/ml) in the absence or presence of the NAD(P)H oxidase inhibitors DPI (10 μM) and Apocynin (10 mM) for 0, 6, 12, 18, and 24 h (N = 6). Endothelial ROS were determined by means of the ROS-sensitive dye, DCF (d and e), Amplex red (i and j) and DHE/HPLC (n and o), in HAEC and HUVEC exposed to vehicle and oxHDL (50 μg/ml) in the absence or presence of transfection with a siRNA against NOX-1 (siNOX1), NOX-2 (siNOX2), and NOX-4 (siNOX4) for 0, 6, 12, 18, and 24 h. Data are expressed normalized to 0 time (N = 6). Statistical differences for HAEC and HUVEC samples were assessed by a one-way analysis of variance (ANOVA) (Kruskal–Wallis) followed by Dunn’s post hoc test. *P < 0.05. Graph bars show the mean ± SD. LOX-1 expression was measured in the membrane-rich fraction from ECs exposed to HDL (50 μg/ml) and oxHDL (50 μg/ml) for 24 h in the absence (–) or presence (+) of NAC (5 mM) (p and q), GSH (1 mM) (r–s), DPI (10 μM) (t and u), and Apocynin (10 mM) (v–x) Data are expressed normalized to vehicle condition (N = 3). Statistical differences were assessed by a two-way analysis of variance (ANOVA) followed by Tukey post hoc test. **P < 0.01. Graph bars show the mean ± SD
To determine the participating of endothelial NOX isoform, we performed experiments using siRNA against the endothelial isoforms of NOX; NOX-1, NOX-2, and NOX-4 [32,33,34]. The results showed that both HUVEC and HAEC exposed to oxHDL and transfected with siRNA against NOX-2 failed to increase ROS levels. By contrast, oxHDL-treated HUVEC (Fig. 3d–n) and HAEC (Fig. 3e–o) and cells transfected with siRNA against NOX-1 and NOX-4 exhibited no change compared with the vehicle condition. Experiments performed using a nontargeting siRNA were used as a control and showed no differences compared with the vehicle condition (data not shown). These results showed that NOX-2, but not NOX-1 or NOX-4, participates in oxHDL-induced ROS generation in HUVEC and HAEC.
To investigate the participation of ROS in oxHDL-induced LOX-1 accumulation at the plasma membrane, ECs were exposed to oxHDL and HDL in the presence of the antioxidant NAC and the reducing agent GSH, and LOX-1 expression was measured in the plasma membrane-rich fraction. The plasma membrane fraction obtained from oxHDL-treated ECs treated with NAC (Fig. 3p, q) and GSH (Fig. 3r, s) showed a complete inhibition of oxHDL-induced LOX-1 expression. These results indicate that oxHDL increases LOX-1 expression at the plasma membrane by a mechanism mediated by oxidative stress generation. In addition to this, the plasma membrane-rich fraction obtained from oxHDL-treated ECs in the presence of the NAD(P)H oxidase inhibitors DPI (Fig. 3t, u) and apocynin (Fig. 3v–x) failed to increase LOX-1 expression. The cytosol-rich fraction exhibited no detectable change in the LOX-1 levels when HUVEC-derived ECs were exposed to NAC, GSH, DPI, and apocynin or were transfected with siRNAs against NOX isoforms (data not shown). These data suggest that the oxHDL-induced expression and localization of LOX-1 at the plasma membrane is dependent on NAD(P)H oxidase activity.
Finally, we wondered whether oxHDL modulates the mRNA expression of NOX isoforms. The results showed that HAEC and HUVEC treated with HDL and oxHDL increased the mRNA expression of NOX-2, but not NOX-1 and NOX-4 (Fig. 4a, b).
Oxidative stress increases LOX-1 expression at the cellular plasma membrane through the activation of NF-κB. Ox-HDL-induced NOX isoform mRNA expression was determined by RT-qPCR in HAEC (a) and HUVEC (b). Data are expressed normalized to HDL condition (N = 3). Statistical differences for HAEC and HUVEC samples were assessed by a one-way analysis of variance (ANOVA) (Kruskal–Wallis) followed by Dunn’s post hoc test. *P < 0.05. **P < 0.01. Graph bars show the mean ± SD. HAEC and HUVEC were exposed to H2O2 (0, 1, 10, 100 μM) (c and d) and GSSG (0, 0.02, 0.2, 2 mM) (e and f) for 24 h, and LOX-1 expression was analyzed. Data are expressed normalized to 0 μM H2O2 or GSSG (N = 5). Statistical differences were assessed by a one-way analysis of variance (ANOVA) (Kruskal–Wallis) followed by Dunn’s post hoc test. *P < 0.05, **P < 0.01. Graph bars show the mean ± SD. LOX-1 expression was measured in cytosol-rich and membrane-rich fractions from cells exposed to H2O2 (100 μM) (g–i) and GSSG (2 mM) (h–j) for 24 h. Protein levels were normalized against Na+ pump in the membrane-rich fraction. Data are expressed normalized to vehicle condition in the absence of stimuli (N = 4). LOX-1 expression was measured in the plasma membrane-rich fraction from ECs exposed to H2O2 (100 μM) and GSSG (2 mM) for 24 h in the absence (–) or presence (+) of the LOX-1 inhibitor κ-carrageenan (250 μg/ml) (k, l), the NF-κB inhibitor SC3060 (5 μM) (m, n), H2O2 (100 μM) (o, p) and GSSG (2 mM) (q, r). Data are expressed normalized to vehicle condition in the absence of stimuli (N = 4). Statistical differences were assessed by a two-way analysis of variance (ANOVA) followed by Tukey post hoc test. **P < 0.01. Graph bars show the mean ± SD
Oxidative stress increases LOX-1 expression at the plasma membrane through the activation of NF-κB but independent on LOX-1 interaction
Considering the results above, we were prompted to investigate whether oxidative stress is able to modulate LOX-1 expression and distribution. To that end, ECs were exposed to several concentrations of the oxidants H2O2 and oxidized glutathione (GSSG), and LOX-1 expression was measured. ECs showed a dose-dependent increase in LOX-1 expression when cells were exposed to H2O2 (Fig. 4c, d) and GSSG (Fig. 4e, f). Next, we tested whether oxidative stress promotes LOX-1 accumulation at the plasma membrane. ECs were exposed to H2O2 and GSSG, and then, LOX-1 expression was measured in the plasma membrane-rich and cytosol-rich fractions. The plasma membrane fraction obtained from ECs treated with H2O2 (Fig. 4g–i) and GSSH (Fig. 4h–j) showed an increase in LOX-1 expression, whereas the cytosol-rich fraction showed no change. These results indicate that both H2O2 and GSSG increase LOX-1 expression at the plasma membrane in ECs.
As a next step, H2O2-treated and GSSG-treated ECs were incubated with κ-carrageenan, and SC3060 to evaluate whether LOX-1 and NF-κB were involved in the effects of oxidative stress on LOX-1 expression at the cell plasma membrane. As shown in Fig. 4k, l, incubation with κ-carrageenan did not modify either the H2O2-induced or GSSG-induced LOX-1 increase at the plasma membrane, whereas SC3060 treatment entirely abolished both the H2O2-induced and GSSG-induced LOX-1 increase at the plasma membrane (Fig. 4m, n). These data suggest that oxidative stress increases LOX-1 expression at the plasma membrane through the activation of NF-κB but is independent of LOX-1 receptor interaction.
Because both oxidative stress and oxHDL increase LOX-1 expression at the plasma membrane, we were prompted to investigate the effects of oxidative stress and oxHDL together on LOX-1 expression in the membrane fraction. The membrane fraction from ECs exposed to H2O2 (Fig. 4o, p) and GSSG (Fig. 4q, r) did not show differences when in the presence or absence of oxHDL. The cytosol-rich fraction exhibited no detectable change in the LOX-1 level when HUVEC-derived ECs were exposed to H2O2 GSSG, κ-carrageenan and SC3060 (data not shown). These findings suggest that the mechanisms involved in the increased LOX-1 expression and localization triggered by either oxidative stress and oxHDL share the same intracellular pathway.
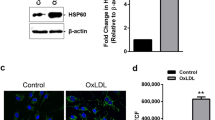
TNF-α increases LOX-1 expression at the cellular plasma membrane mediated by the TNF-α receptor activity and the ROS/NOX pathway and NF-κB activation
It has been reported that TNF-α increases the expression of LOX-1 in ECs [35]. In concordance, Fig. 5a, b showed that LOX-1 expression increases in a dose-dependent manner in ECs treated with TNF-α. Notably, TNF-α increases LOX-1 expression at the plasma membrane. Plasma membrane fraction obtained from ECs exposed to TNF-α showed a strong accumulation of LOX-1 expression, whereas the cytosol-rich fraction did not exhibit significant changes in LOX-1 expression (Fig. 5c, d). To study whether TNF-α receptor mediates the TNF-α-induced LOX-1 accumulation at the plasma membrane, ECs were exposed to TNF-α in the presence or absence of the TNF-α receptor inhibitor, SC-7050, and LOX-1 expression was measured in the plasma membrane-rich fraction. Plasma membrane fraction obtained from TNF-α-treated ECs with SC-7050 showed inhibition of the LOX-1 expression increase (Fig. 5e, f), indicating that TNF-α receptor is necessary for TNF-α-induced LOX-1 accumulation at the plasma membrane.
TNF-α increases LOX-1 expression at the cellular plasma membrane by a mechanism mediated by the TNF-α receptor activity and the ROS/NOX pathway and NF-κB activation. Cells were exposed to TNF-α and LOX-1 expression was analyzed. a Representative images from western blot experiments performed for detection of LOX-1 in the presence of TNF-α (0, 5, and 10 ng/ml) for 24 h. b Densitometric analyses of the experiments shown in a. Protein levels were normalized against tubulin, and data are expressed normalized to the TNF-α 0 ng/ml condition (N = 4). Statistical differences were assessed by a one-way analysis of variance (ANOVA) (Kruskal–Wallis) followed by Dunn’s post hoc test. *P < 0.05. **P < 0.01. Graph bars show the mean ± SD. c and d LOX-1 expression in plasma membrane-rich and cytosol-rich fractions from ECs exposed to TNF-α (10 ng/ml) for 24 h. Protein levels were normalized against Na+ pump in the membrane-rich fraction. Data are expressed normalized to vehicle condition (N = 3). e and f LOX-1 expression in the plasma membrane-rich fraction from ECs exposed to TNF-α (10 ng/ml) for 24 h in the absence (–) or presence (+) of the TNF-α receptor inhibitor, R7050 (5 μM) (N = 3). Data are expressed normalized to vehicle condition. Statistical differences were assessed by a two-way analysis of variance (ANOVA) followed by Tukey post hoc test. **P < 0.01. Graph bars show the mean ± SD. TNF-α-induced NOX isoform mRNA expression was determined by RT-qPCR in HAEC (g) and HUVEC (h). Data are expressed normalized to vehicle condition (N = 3). Statistical differences for HAEC and HUVEC samples were assessed by a one-way analysis of variance (ANOVA) (Kruskal–Wallis) followed by Dunn’s post hoc test. *P < 0.05. **P < 0.01. Graph bars show the mean ± SD. LOX-1 expression was measured in the plasma membrane-rich fraction from cells exposed to TNF-α 10 ng/ml for 24 h in the absence (–) or presence (+) of NAC (5 mM) (i, j), GSH (1 mM) (k, l), the NAD(P)H oxidase inhibitor DPI (10 μM) (m and n), NAD(P)H oxidase inhibitor Apocynin (10 mM) (o and p) and the NF-κB inhibitor SC3060 (5 μM) (q and r) for 24 h (N = 3). Statistical differences were assessed by a two-way analysis of variance (ANOVA) followed by Tukey post hoc test. **P < 0.01. Graph bars show the mean ± SD
Next, we wondered whether TNF-α modulates NOX isoform mRNA expression. The results showed that HAEC and HUVEC treated with TNF-α increased mRNA expression of NOX-2, but not that of NOX-1 and NOX-4 (Fig. 5g, h).
To investigate the participation of oxidative stress in TNF-α-induced LOX-1 accumulation at the plasma membrane, ECs were exposed to TNF-α in the presence of NAC and GSH, and then, LOX-1 expression was measured in the plasma membrane-rich fraction. Plasma membrane fraction obtained from TNF-α-treated ECs incubated with NAC (Fig. 5i, j) and GSH (Fig. 5k, l) showed a complete inhibition of the LOX-1 expression increase induced by TNF-α. These results indicate that the TNF-α-induced LOX-1 increase in the plasma membrane fraction is mediated by oxidative stress generation. Furthermore, plasma membrane fraction from TNF-α-treated ECs treated with TNF-α and incubated with the NAD(P)H oxidase inhibitors DPI (Fig. 5m, n) and apocynin (Fig. 5o, p) failed to increase LOX-1 expression. These data suggest that TNF-α-induced expression and membrane localization of LOX-1 at the plasma membrane are dependent on the NAD(P)H oxidase activity.
Next, we studied whether NF-κB participates in LOX-1 plasma membrane accumulation induced by TNF-α. Membrane fraction obtained from TNF-α-treated ECs in the presence SC3060 failed into increase LOX-1 expression (Fig. 5q, r), suggesting that NF-κB activation is required for TNF-α-induced accumulation of LOX-1 at the plasma membrane.
Cytosol-rich fraction exhibited no detectable change in the LOX-1 levels when HUVEC-derived ECs were exposed to Sc-7050, NAC, GSH, DPI, Apocynin, and SC3060 (data not shown).
OxHDL increases TNF-α expression through the activation of LOX-1 and NF-κB, but the TNF-α receptor is not required for an increase in oxHDL-induced LOX-1 at the plasma membrane
To test whether oxHDL exposure modulates TNF-α expression, we performed RT-qPCR to determine changes in TNF-α mRNA expression. OxHDL-treated ECs showed an increased TNF-α mRNA expression compared to HDL-treated or vehicle-treated ECs (Fig. 6a). Next, we wondered whether the oxHDL-induced TNF-α mRNA expression increase is mediated by LOX-1 receptor. To that end, ECs were exposed to oxHDL in the presence or absence of LOX-1 receptor blocker, κ-carrageenan, and TNF-α mRNA expression was measured. Treatment with κ-carrageenan completely abolished the TNF-α mRNA expression increase induced by oxHDL (Fig. 6b). Then, we tested whether NF-κB participates in the oxHDL-induced TNF-α mRNA expression increase. ECs exposed to oxHDL in the presence of NF-κB inhibitor, SC3060, failed to increase TNF-α mRNA expression (Fig. 6c), suggesting that NF-κB activation is required for TNF-α mRNA expression induced by oxHDL. These results suggest that oxHDL challenge increases TNF-α mRNA expression through the participation of LOX-1 receptor activity and NF-κB activation. To demonstrate that oxHDL administration induces TNF-α secretion, plasma samples from rats treated with HDL, oxHDL, and vehicle were subjected to TNF-α determination. The results showed a significant increase in the plasma TNF-α levels in oxHDL-treated rats compared with rats treated with vehicle or native HDL (Fig. 6d). This finding agrees with in vitro results showing increased TNF-α mRNA expression under the oxHDL condition.
OxHDL increases TNF-α expression through the activation of LOX-1 and NF-κB. a TNF-α mRNA expression measured in ECs exposed to HDL (50 μg/ml) and oxHDL (50 μg/ml) for 24 h. Data are expressed normalized to vehicle condition (N = 3). Statistical differences were assessed by a one-way analysis of variance (ANOVA) (Kruskal–Wallis) followed by Dunn’s post hoc test. **P < 0.01. Graph bars show the mean ± SD. b and c TNF-α mRNA expression was measured in ECs exposed to HDL (50 μg/ml) and oxHDL (50 μg/ml) for 24 h in the absence (–) or presence (+) of the LOX-1 inhibitor κ-carrageenan (250 μg/ml) (b) and the NF-κB inhibitor SC3060 (5 μM) (c). Data are expressed normalized to vehicle condition in the absence of stimuli (N = 3). Plasma TNF-α levels in rats treated with vehicle, HDL and oxHDL for 24 h. Data are expressed normalized to vehicle condition (N = 3). Statistical differences were assessed by a one-way analysis of variance (ANOVA) (Kruskal–Wallis) followed by Dunn’s post hoc test. **P < 0.01. Graph bars show the mean ± SD (d). LOX-1 expression was measured in the plasma membrane-rich fraction from ECs exposed to vehicle, HDL (50 μg/ml) and oxHDL (50 μg/ml) for 24 h in the absence (–) or presence (+) of the TNF-α receptor inhibitor, R7050 (5 μM) (e and f) and TNF-α 10 ng/ml (g and h) (N = 3). Statistical differences were assessed by a two-way analysis of variance (ANOVA) followed by Tukey post hoc test. **P < 0.01. Graph bars show the mean ± SD
Finally, we wondered whether TNF-α mediates the oxHDL-induced LOX-1 expression increase at the plasma membrane. To test that issue, oxHDL-treated ECs were incubated in the presence of TNF-α receptor inhibitor, SC-7050, and LOX-1 expression was measured. SC-7050 treatment did not affect the increase in LOX-1 expression in the plasma membrane fraction when ECs were exposed to oxHDL (Fig. 6e, f). This result suggests that TNF-α expression is not required for the increase in ox-HDL-induced LOX-1 expression at the plasma membrane. In addition to this, we explored the combined effect of oxHDL and TNF-α challenge in LOX-1 expression. To that end, oxHDL-treated ECs were exposed to TNF-α, and LOX-1 expression was measured. Interestingly, the membrane fraction from ECs exposed to oxHDL in combination with TNF-α showed a significant increase in LOX-1 expression (Fig. 6g, h), suggesting that TNF-α potentiates the oxHDL effect, but TNF-R participation is not required for oxHDL-induced LOX-1 expression increase.
Discussion
Endothelial dysfunction is a key event in the progression of several systemic inflammatory diseases [36]. Because current treatments are often not satisfactory, understanding the molecular pathways through which the crucial actors involved in these pathogenetic processes exert their effects is essential for improving treatments [37]. Here, we studied the action of the oxidized lipoprotein oxHDL on the expression of the plasma membrane receptor LOX-1, which mediates numerous deleterious effects in ECs. There is consensus that oxidized LDL is involved in the pathogenesis of various atherosclerosis-based cardiovascular diseases; however, the roles of oxidized HDL remain poorly understood.
In this study, we demonstrated that the oxidized form of HDL, oxHDL, increases LOX-1 expression in the EC plasma membrane. Interestingly, the native form of HDL does not increase LOX-1 expression in ECs, indicating that only the oxidized form is involved in modulating LOX-1 expression and promoting localization of LOX-1 at the plasma membrane. Furthermore, our results indicate that the increase in expression of oxHDL induced by LOX-1 is dependent on NOX-2/ROS activity and activation of the NF-κB pathway, which is potentiated by exposure to TNF-α, but TNF-R participation is not required for oxHDL-induced LOX-1 expression increase.
Control of LOX-1 cell localization by oxHDL is a finding of remarkable interest [38, 39]. Most studies showing LOX-1 expression increase do not describe changes in cellular localization upon stimulation [24, 25, 40]. Considering that LOX-1 is a membrane receptor, it is only functional when it reaches the plasma membrane [38, 39]. As our results showed, oxHDL challenge promotes localization to the endothelial plasma membrane. The oxHDL-induced LOX-1 plasma membrane localization could be a crucial step in allowing it to reach the plasma membrane and become a functional receptor. Changes in the distribution of LOX-1 could be correlated with detrimental effects on specific endothelial functions, such as endothelial monolayer permeability, hormone production, and nitric oxide secretion [41,42,43]. Certainly, further studies are needed to investigate this issue.
Several systemic inflammatory diseases, such as hypertension, diabetes, arthritis, atherosclerosis, obesity, and sepsis are associated with severe alterations in circulatory system function because circulating inflammatory mediators act on vascular tissue, extensively damaging blood circulation [7,8,9,10]. Systemic inflammatory diseases are characterized by the presence of inflammatory mediators, such as TNF-α, IL-1β, IL-6, transforming growth factor-β (TGF-β), and bacterial endotoxins into the blood flow [35]. In fact, during systemic inflammatory disease, interaction between inflammatory mediators and ECs is unavoidable and triggers severe endothelial dysfunction [7, 8, 10, 35, 44,45,46]. In addition, during systemic inflammation the production of ROS is also increased. The produced ROS modify several proteins through oxidation, altering their functions [11, 12, 47, 48]. In line with this, it has been reported that 15LO-modified HDL3 is also able to increase LOX-1 expression in ECs [25, 49]. Our findings showed that oxHDL, but not the native form HDL, is also able to increase the expression of LOX-1 in the EC plasma membrane (Fig. 7, no. 1). Similarly, as observed with oxLDL, oxHDL-induced LOX-1 increase is mediated by the interaction between oxHDL and LOX-1. This was demonstrated using the nonspecific but selective LOX-1 inhibitor, κ-carrageenan. Thus, it is possible that other mechanisms exist by which oxHDL could be internalized and exert its effects in ECs. However, using κ-carrageenan as a LOX-1 inhibitor is widespread and well documented [25]. Considering the limited specificity of κ-carrageenan, we were used the anti-LOX-1 blocking antibody, which is a specific strategy to inhibit LOX-1 [16, 21, 24, 50,51,52,53]. Thus, our results obtained using κ-carrageenan were confirmed by experiments using the anti-LOX-1 blocking antibody, which is a more specific strategy for LOX-1 inhibition.
Proposed model of oxHDL actions modulating LOX-1 expression and localization in ECs. oxHDL interacts with LOX-1 receptor (1) inducing an increase in ROS production (3) via NAD(P)H oxidase 2 isoform (2) and inducing downstream NF-κB activation (4). NF-κB also promotes LOX-1 over-expression (5) in a positive feedback loop. LOX-1 over-expression is also induced by presence of TNF-α (6) (through binding of TNF-α receptor), H2O2 (7) and GSSG (8), via NF-κB pathway
Because oxidation levels increase robustly during systemic inflammatory diseases, the participation of ROS in pathological activity has been well accepted [54, 55]. It has been reported that ROS can regulate gene expression and act as signaling molecules to modulate protein function [56,57,58,59,60,61]. H2O2 and other reactive intermediates are involved in the expression of a number of proteins, such as cyclooxygenase-2 and prostaglandins [62, 63], the proto-oncogenes c-jun, c-fos, and c-myc [64], TRP ion channels [65], the vascular cell adhesion molecule-1, and intercellular adhesion molecule-1 [66, 67], and also control the regulation of cell proliferation and survival, oncogene activation, immune response, apoptosis, and necrosis [67,68,69]. Here, ccontrol of LOX-1 expression is a ROS-dependent process since it was inhibited when antioxidant/reducing agents was used (Fig. 7, no. 2). These results are in accordance with those described previously in HUVEC [70, 71]. However, our data indicate that ROS production is an earlier event. On the other hand, ECs express the NOX type -1, -2 and -4, which generate superoxide anions. Experiments performed with siRNAs against the endothelial NOX isoforms indicated that NOX-2 is the source of generated ROS (Fig. 7, nos. 3, 7, and 8). It is well known that ROS support the activation and nuclear translocation of the transcription factor NF-κB. In accordance with this, oxHDL requires NF-κB activation for an increase in LOX-1 expression, indicating that the oxHDL-induced LOX-1 expression depends on gene expression (Fig. 7, nos. 4 and 5).
Pro-inflammatory cytokines increase during systemic inflammation and induce gene expression by NF-κB activation in ECs [72]. Inhibition of the cytokine receptor abolished the TNF-α-induced LOX-1 expression increase (Fig. 7, no. 6), which is accordance with the finding that pro-inflammatory cytokines increase LOX-1 expression [73,74,75]. Interestingly, TNF-α potentiates the effects of oxHDL, possibly by means of enhanced generation of ROS and the subsequent increased translocation of NF-κB to activate the LOX-1 gene transcription. However, the inhibition of the TNF-α receptor, TNF-R, did not modify the action of oxHDL in promoting the increase of LOX-1 at the plasma membrane.
In the context of systemic inflammatory diseases, endothelial dysfunction represents, at least in part, a suitable explanation for organ dysfunction during these diseases. Thus, translocation of LOX-1 to the plasma membrane could constitute a suitable mechanism for the induction of endothelial dysfunction by allowing ligand–receptor interaction. In this way, the increase of LOX-1 expression and its redistribution may work in a coordinated manner to localize a large amount of the receptor to the plasma membrane.
Change history
12 January 2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
15 January 2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Nestel PJ. Dietary cholesterol and plasma lipoproteins. Atherosclerosis. 1994;109:87.
Tall AR. Plasma high density lipoproteins: therapeutic targeting and links to atherogenic inflammation. Atherosclerosis. 2018;276:39–43.
Yan BP, Chiang F-T, Ambegaonkar B, et al. Low-density lipoprotein cholesterol target achievement in patients surviving an acute coronary syndrome in Hong Kong and Taiwan—findings from the Dyslipidemia International Study II. Int J Cardiol. 2018;265:1–5.
Miller GJ. High-density lipoprotein, low-density lipoprotein, and coronary heart disease. Thorax. 1978;33:137–9.
O’Connell BJ, Genest J. High-density lipoproteins and endothelial function. Circulation. 2001;104:1978–83.
Besler C, Heinrich K, Rohrer L, et al. Mechanisms underlying adverse effects of HDL on eNOS-activating pathways in patients with coronary artery disease. J Clin Invest. 2011;121:2693–708.
Ku IA, Imboden JB, Hsue PY, Ganz P. Rheumatoid arthritis: model of systemic inflammation driving atherosclerosis. Circ J. 2009;73:977–85.
Pinsky MR. Dysregulation of the immune response in severe sepsis. Am J Med Sci. 2004;328:220–9.
Pérez L, Muñoz-Durango N, Riedel CA, et al. Endothelial-to-mesenchymal transition: cytokine-mediated pathways that determine endothelial fibrosis under inflammatory conditions. Cytokine Growth Factor Rev. 2017;33:41–54.
Suboc TM, Dharmashankar K, Wang J, et al. Moderate obesity and endothelial dysfunction in humans: influence of gender and systemic inflammation. Physiol Rep. 2013;1:e00058.
Muller MM, Griesmacher A. Markers of endothelial dysfunction. Clin Chem Lab Med. 2000;38:77–85.
Zhang C. The role of inflammatory cytokines in endothelial dysfunction. Basic Res Cardiol. 2008;103:398–406.
Closa D, Folch-Puy E. Oxygen free radicals and the systemic inflammatory response. IUBMB Life. 2004;56:185–91.
Higashi Y, Noma K, Yoshizumi M, Kihara Y. Endothelial function and oxidative stress in cardiovascular diseases. Circ J. 2009;73:411–8.
Swindle EJ, Metcalfe DD. The role of reactive oxygen species and nitric oxide in mast cell-dependent inflammatory processes. Immunol Rev. 2007;217:186–205.
Pirillo A, Norata GD, Catapano AL. LOX-1, OxLDL, and atherosclerosis. Mediat Inflamm. 2013;2013:152786–12.
Tsimikas S, Miller YI. Oxidative modification of lipoproteins: mechanisms, role in inflammation and potential clinical applications in cardiovascular disease. Curr Pharm Des. 2011;17:27–37.
Shroff R, Speer T, Colin S, et al. HDL in children with CKD promotes endothelial dysfunction and an abnormal vascular phenotype. J Am Soc Nephrol. 2014;25:2658–68.
Speer T, Rohrer L, Blyszczuk P, et al. Abnormal high-density lipoprotein induces endothelial dysfunction via activation of toll-like receptor-2. Immunity. 2013;38:754–68.
Cominacini L, Pasini AF, Garbin U, et al. Oxidized low density lipoprotein (ox-LDL) binding to ox-LDL receptor-1 in endothelial cells induces the activation of NF-kappaB through an increased production of intracellular reactive oxygen species. J Biol Chem. 2000;275:12633–8.
Kataoka H, Kume N, Miyamoto S, et al. Expression of lectinlike oxidized low-density lipoprotein receptor-1 in human atherosclerotic lesions. Circulation. 1999;99:3110–7.
Honjo M, Nakamura K, Yamashiro K, et al. Lectin-like oxidized LDL receptor-1 is a cell-adhesion molecule involved in endotoxin-induced inflammation. Proc Natl Acad Sci USA. 2003;100:1274–9.
Mitra S, Goyal T, Mehta JL. Oxidized LDL, LOX-1 and atherosclerosis. Cardiovasc Drugs Ther. 2011;25:419–29.
Matsunaga T, Hokari S, Koyama I, et al. NF-kB activation in endothelial cells treated with oxidized high-density lipoprotein. Biochem Biophys Res Commun. 2003;303:313–9.
Pirillo A, Uboldi P, Ferri N, et al. Upregulation of lectin-like oxidized low density lipoprotein receptor 1 (LOX-1) expression in human endothelial cells by modified high density lipoproteins. Biochem Biophys Res Commun. 2012;428:230–3.
Kume N, Murase T, Moriwaki H, et al. Inducible expression of lectin-like oxidized LDL receptor-1 in vascular endothelial cells. Circ Res. 1998;83:322–7.
Edgell CJ, McDonald CC, Graham JB. Permanent cell line expressing human factor VIII-related antigen established by hybridization. Proc Natl Acad Sci USA. 1983;80:3734–7.
Scoccia AE, Molinuevo MS, McCarthy AD, Cortizo AM. A simple method to assess the oxidative susceptibility of low density lipoproteins. BMC Clin Pathol. 2001;1:1.
Lynch SM, Frei B. Reduction of copper, but not iron, by human low density lipoprotein (LDL). Implications for metal ion-dependent oxidative modification of LDL. J Biol Chem. 1995;270:5158–63.
Dikalov S, Griendling KK, Harrison DG. Measurement of reactive oxygen species in cardiovascular studies. Hypertension. 2007;49:717–27.
Chen J, Liu Y, Liu H, et al. Lectin-like oxidized low-density lipoprotein receptor-1 (LOX-1) transcriptional regulation by Oct-1 in human endothelial cells: implications for atherosclerosis. Biochem J. 2006;393:255–65.
Simon F, Stutzin A. Protein kinase C-mediated phosphorylation of p47phox modulates platelet-derived growth factor-induced H2O2 generation and cell proliferation in human umbilical vein endothelial cells. Endothelium. 2008;15:175–88.
Simon F, Fernández R. Early lipopolysaccharide-induced reactive oxygen species production evokes necrotic cell death in human umbilical vein endothelial cells. J Hypertens. 2009;27:1202–16.
Hwang J, Kleinhenz DJ, Lassègue B, et al. Peroxisome proliferator-activated receptor-gamma ligands regulate endothelial membrane superoxide production. Am J Physiol Cell Physiol. 2005;288:C899–905.
Hofnagel O. Proinflammatory cytokines regulate LOX-1 expression in vascular smooth muscle cells. Arterioscler Thromb Vasc Biol. 2004;24:1789–95.
Aird WC. The role of the endothelium in severe sepsis and multiple organ dysfunction syndrome. Blood. 2003;101:3765–77.
Pirillo A, Catapano AL, Norata GD. HDL in infectious diseases and sepsis. Handb Exp Pharmacol. 2015;224:483–508.
Moriwaki H, Kume N, Sawamura T, et al. Ligand specificity of LOX-1, a novel endothelial receptor for oxidized low density lipoprotein. Arterioscler Thromb Vasc Biol. 1998;18:1541–7.
Sawamura T, Kume N, Aoyama T, et al. An endothelial receptor for oxidized low-density lipoprotein. Nature. 1997;386:73–77.
Pirillo A, Reduzzi A, Ferri N, et al. Upregulation of lectin-like oxidized low-density lipoprotein receptor-1 (LOX-1) by 15-lipoxygenase-modified LDL in endothelial cells. Atherosclerosis. 2011;214:331–7.
Lubrano V, Balzan S. LOX-1 and ROS, inseparable factors in the process of endothelial damage. Free Radic Res. 2014;48:841–8.
Zhao W, Ma G, Chen X. Lipopolysaccharide induced LOX-1 expression via TLR4/MyD88/ROS activated p38MAPK-NF-κB pathway. Vasc Pharmacol. 2014;63:162–72.
Son JN, Lho Y, Shin S, et al. Carbamylated low-density lipoprotein increases reactive oxygen species (ROS) and apoptosis via lectin-like oxidized LDL receptor (LOX-1) mediated pathway in human umbilical vein endothelial cells. Int J Cardiol. 2011;146:428–30.
Elks CM, Francis J. Central adiposity, systemic inflammation, and the metabolic syndrome. Curr Protoc Cytom. 2010;12:99–104.
Echeverría C, Montorfano I, Tapia P, et al. Endotoxin-induced endothelial fibrosis is dependent on expression of transforming growth factors β1 and β2. Infect Immun. 2014;82:3678–86.
Becerra A, Rojas M, Vallejos A, et al. Endothelial fibrosis induced by suppressed STAT3 expression mediated by signaling involving the TGF-β1/ALK5/Smad pathway. Lab Invest. 2017;97:1033–46.
Montorfano I, Becerra A, Cerro R, et al. Oxidative stress mediates the conversion of endothelial cells into myofibroblasts via a TGF-β1 and TGF-β2-dependent pathway. Lab Invest. 2014;94:1068–82.
Echeverría C, Montorfano I, Sarmiento D, et al. Lipopolysaccharide induces a fibrotic-like phenotype in endothelial cells. J Cell Mol Med. 2013;17:800–14.
Cutuli L, Pirillo A, Uboldi P, et al. 15-lipoxygenase-mediated modification of HDL3 impairs eNOS activation in human endothelial cells. Lipids. 2014;49:317–26.
Chen M, Masaki T, Sawamura T. LOX-1, the receptor for oxidized low-density lipoprotein identified from endothelial cells: implications in endothelial dysfunction and atherosclerosis. Pharmacol Ther. 2002;95:89–100.
Spallarossa P, Fabbi P, Manca V, et al. Doxorubicin-induced expression of LOX-1 in H9c2 cardiac muscle cells and its role in apoptosis. Biochem Biophys Res Commun. 2005;335:188–96.
Xu S, Ogura S, Chen J, et al. LOX-1 in atherosclerosis: biological functions and pharmacological modifiers. Cell Mol Life Sci. 2013;70:2859–72.
Zuniga FA, Ormazabal V, Gutierrez N, et al. Role of lectin-like oxidized low density lipoprotein-1 in fetoplacental vascular dysfunction in preeclampsia. Biomed Res Int. 2014;2014:353616.
Prauchner CA. Oxidative stress in sepsis: pathophysiological implications justifying antioxidant co-therapy. Burns. 2017;43:471–85.
Weidenbusch M, Anders H-J. Tissue microenvironments define and get reinforced by macrophage phenotypes in homeostasis or during inflammation, repair and fibrosis. J Innate Immun. 2012;4:463–77.
Dominguez JH, Mehta JL, Li D, et al. Anti-LOX-1 therapy in rats with diabetes and dyslipidemia: ablation of renal vascular and epithelial manifestations. Am J Physiol Ren Physiol. 2008;294:F110–9.
Xu X, Gao X, Potter BJ, et al. Anti-LOX-1 rescues endothelial function in coronary arterioles in atherosclerotic ApoE knockout mice. Arterioscler Thromb Vasc Biol. 2007;27:871–7.
Ishino S, Mukai T, Kuge Y, et al. Targeting of lectinlike oxidized low-density lipoprotein receptor 1 (LOX-1) with 99mTc-labeled anti-LOX-1 antibody: potential agent for imaging of vulnerable plaque. J Nucl Med. 2008;49:1677–85.
Iwamoto S, Fujita Y, Kakino A, et al. An alternative protein standard to measure activity of LOX-1 ligand containing apoB (LAB)—utilization of anti-LOX-1 single- chain antibody fused to apoB fragment. J Atheroscler Thromb. 2011;18:818–28.
Hu W, Xie Q, Liu L, Xiang H. Enhanced bioactivity of the anti-LOX-1 scFv engineered by multimerization strategy. Appl Biochem Biotechnol. 2018;185:233–47.
Hu W, Xie Q, Xiang H. Improved scFv Anti-LOX-1 binding activity by fusion with LOX-1-binding peptides. Biomed Res Int. 2017;2017:8946935.
Dröge W. Free radicals in the physiological control of cell function. Physiol Rev. 2002;82:47–95.
Kunsch C, Medford RM. Oxidative stress as a regulator of gene expression in the vasculature. Circ Res. 1999;85:753–66.
Kiritoshi S, Nishikawa T, Sonoda K, et al. Reactive oxygen species from mitochondria induce cyclooxygenase-2 gene expression in human mesangial cells: potential role in diabetic nephropathy. Diabetes. 2003;52:2570–7.
Li DW, Spector A. Hydrogen peroxide-induced expression of the proto-oncogenes, c-jun, c-fos and c-myc in rabbit lens epithelial cells. Mol Cell Biochem. 1997;173:59–69.
Marshall JC. Inflammation, coagulopathy, and the pathogenesis of multiple organ dysfunction syndrome. Crit Care Med. 2001;29(7 Suppl):S99–106.
Ziesmann MT, Marshall JC. Multiple organ dysfunction: the defining syndrome of sepsis. Surg Infect. 2018;19:184–90.
Englert JA, Fink MP. The multiple organ dysfunction syndrome and late-phase mortality in sepsis. Curr Infect Dis Rep. 2005;7:335–41.
Baue AE. Sepsis, systemic inflammatory response syndrome, multiple organ dysfunction syndrome, and multiple organ failure: are trauma surgeons lumpers or splitters? J Trauma. 2003;55:997–8.
Fink MP. Nitric oxide synthase and vascular dysfunction in sepsis. Crit Care Med. 2014;42:1572–5.
Yaghi A, Paterson NA, McCormack DG. Vascular reactivity in sepsis: importance of controls and role of nitric oxide. Am J Respir Crit Care Med. 1995;151:706–12.
Hoover DB, Brown TC, Miller MK, et al. Loss of sympathetic nerves in spleens from patients with end stage sepsis. Front Immunol. 2017;8:1712.
Tracey KJ, Fong Y, Hesse DG, et al. Anti-cachectin/TNF monoclonal antibodies prevent septic shock during lethal bacteraemia. Nature. 1987;330:662–4.
Douzinas EE, Tsidemiadou PD, Pitaridis MT, et al. The regional production of cytokines and lactate in sepsis-related multiple organ failure. Am J Respir Crit Care Med. 1997;155:53–59.
Pinsky MR. Clinical studies on cytokines in sepsis: role of serum cytokines in the development of multiple-systems organ failure. Nephrol Dial Transplant. 1994;9(Suppl 4):94–98.
Acknowledgements
This work was supported by research grants from Fondo Nacional de Desarrollo Científico y Tecnológico—Fondecyt 1161288, 1160900, 11170840, and 1161646. Millennium Institute on Immunology and Immunotherapy P09-016-F. The Millennium Nucleus of Ion Channels-Associated Diseases (MiNICAD) is a Millennium Nucleus supported by the Iniciativa Científica Milenio of the Ministry of Economy, Development and Tourism (Chile). UNAB DI-741-15/N.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Pérez, L., Vallejos, A., Echeverria, C. et al. OxHDL controls LOX-1 expression and plasma membrane localization through a mechanism dependent on NOX/ROS/NF-κB pathway on endothelial cells. Lab Invest 99, 421–437 (2019). https://doi.org/10.1038/s41374-018-0151-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41374-018-0151-3
This article is cited by
-
Increased oxidative stress is associated with hyperandrogenemia in polycystic ovary syndrome evidenced by oxidized lipoproteins stimulating rat ovarian androgen synthesis in vitro
Endocrine (2024)
-
MicroRNA-33-5p inhibits cholesterol efflux in vascular endothelial cells by regulating citrate synthase and ATP-binding cassette transporter A1
BMC Cardiovascular Disorders (2021)
-
Lipoproteins and fatty acids in chronic kidney disease: molecular and metabolic alterations
Nature Reviews Nephrology (2021)
-
High-density lipoprotein-mediated cardioprotection in heart failure
Heart Failure Reviews (2021)