Abstract
Objective
To investigate the association between exposure to surgery under general anesthesia and brain abnormalities and neurodevelopmental outcomes in very preterm infants.
Study design
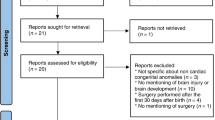
This prospective observational study includes 392 infants born at or below 32 weeks' gestational age. Participants completed brain MRI at term-equivalent age and Bayley-III assessment at 2 years corrected age. We evaluated the independent effects of surgery on brain MRI abnormalities and neurodevelopmental outcomes after propensity score matching.
Results
All infants completed brain MRI, and 341 (87%) completed neurodevelopmental testing. Forty-five received surgery. Surgery was associated with worse MRI abnormalities (p < 0.0001) but with none of the developmental outcomes after propensity score matching. The global brain abnormality score was associated with the Bayley Cognitive (p = 0.005) and Motor (p = 0.028) composite scores.
Conclusions
Very preterm infants exposed to surgery under general anesthesia were at higher risk of brain abnormalities on MRI at term.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Pierrat V, Marchand-Martin L, Marret S, Arnaud C, Benhammou V, Cambonie G, et al. Neurodevelopmental outcomes at age 5 among children born preterm: EPIPAGE-2 cohort study. BMJ. 2021;373:n741.
Pascal A, Govaert P, Oostra A, Naulaers G, Ortibus E, Van den Broeck C. Neurodevelopmental outcome in very preterm and very-low-birthweight infants born over the past decade: a meta-analytic review. Dev Med Child Neurol. 2018;60:342–55.
Spittle A, Orton J, Anderson PJ, Boyd R, Doyle LW. Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst Rev. 2015;2015:CD005495.
Linsell L, Malouf R, Morris J, Kurinczuk JJ, Marlow N. Risk factor models for neurodevelopmental outcomes in children born very preterm or with very low birth weight: a systematic review of methodology and reporting. Am J Epidemiol. 2017;185:601–12.
Back SA, Miller SP. Brain injury in premature neonates: a primary cerebral dysmaturation disorder? Ann Neurol. 2014;75:469–86.
Pironkova RP, Giamelli J, Seiden H, Parnell VA, Gruber D, Sison CP, et al. Brain injury with systemic inflammation in newborns with congenital heart disease undergoing heart surgery. Exp Ther Med. 2017;14:228–38.
Steinhorn R, McPherson C, Anderson PJ, Neil J, Doyle LW, Inder T. Neonatal morphine exposure in very preterm infants-cerebral development and outcomes. J Pediatr. 2015;166:1200–7.e4.
Duerden EG, Guo T, Dodbiba L, Chakravarty MM, Chau V, Poskitt KJ, et al. Midazolam dose correlates with abnormal hippocampal growth and neurodevelopmental outcome in preterm infants. Ann Neurol. 2016;79:548–59.
Duerden EG, Grunau RE, Guo T, Foong J, Pearson A, Au-Young S, et al. Early procedural pain is associated with regionally-specific alterations in thalamic development in preterm neonates. J Neurosci. 2018;38:878–86.
Matei A, Montalva L, Goodbaum A, Lauriti G, Zani A. Neurodevelopmental impairment in necrotising enterocolitis survivors: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2020;105:432–9.
Ene D, Der G, Fletcher-Watson S, O'Carroll S, MacKenzie G, Higgins M, et al. Associations of socioeconomic deprivation and preterm birth with speech, language, and communication concerns among children aged 27 to 30 months. JAMA Netw Open. 2019;2:e1911027.
Van't Hooft J, van der Lee JH, Opmeer BC, Aarnoudse-Moens CS, Leenders AG, Mol BW, et al. Predicting developmental outcomes in premature infants by term equivalent MRI: systematic review and meta-analysis. Syst Rev. 2015;4:71.
Filan PM, Hunt RW, Anderson PJ, Doyle LW, Inder TE. Neurologic outcomes in very preterm infants undergoing surgery. J Pediatr. 2012;160:409–14.
Walsh BH, Paul RA, Inder TE, Shimony JS, Smyser CD, Rogers CE. Surgery requiring general anesthesia in preterm infants is associated with altered brain volumes at term equivalent age and neurodevelopmental impairment. Pediatr Res. 2021;89:1200–7.
Parikh NA, Sharma P, He L, Li H, Altaye M, Priyanka Illapani VS, et al. Perinatal risk and protective factors in the development of diffuse white matter abnormality on term-equivalent age magnetic resonance imaging in infants born very preterm. J Pediatr. 2021;233:58–65.e53.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants. An evidence-based approach. Am J Respir Crit Care Med. 2019;200:751–9.
Parry G, Tucker J, Tarnow-Mordi W, UK Neonatal Staffing Study Collaborative Group. CRIB II: an update of the clinical risk index for babies score. Lancet. 2003;361:1789–91.
Roberts G, Howard K, Spittle AJ, Brown NC, Anderson PJ, Doyle LW. Rates of early intervention services in very preterm children with developmental disabilities at age 2 years. J Paediatr Child Health. 2008;44:276–80.
Lodha A, Sauve R, Chen S, Tang S, Christianson H. Clinical risk index for babies score for the prediction of neurodevelopmental outcomes at 3 years of age in infants of very low birthweight. Dev Med Child Neurol. 2009;51:895–900.
Horsch S, Hallberg B, Leifsdottir K, Skiold B, Nagy Z, Mosskin M, et al. Brain abnormalities in extremely low gestational age infants: a Swedish population based MRI study. Acta Paediatr. 2007;96:979–84.
Kaukola T, Kapellou O, Laroche S, Counsell SJ, Dyet LE, Allsop JM, et al. Severity of perinatal illness and cerebral cortical growth in preterm infants. Acta Paediatr. 2009;98:990–5.
Tamm L, Patel M, Peugh J, Kline-Fath BM, Parikh NA. Cincinnati Infant Neurodevelopment Early Prediction Study G. Early brain abnormalities in infants born very preterm predict under-reactive temperament. Early Hum Dev. 2020;144:104985.
Kidokoro H, Neil JJ, Inder TE. New MR imaging assessment tool to define brain abnormalities in very preterm infants at term. Am J Neuroradiol. 2013;34:2208–14.
Makropoulos A, Robinson EC, Schuh A, Wright R, Fitzgibbon S, Bozek J, et al. The developing human connectome project: a minimal processing pipeline for neonatal cortical surface reconstruction. Neuroimage. 2018;173:88–112.
Gousias IS, Rueckert D, Heckemann RA, Dyet LE, Boardman JP, Edwards AD, et al. Automatic segmentation of brain MRIs of 2-year-olds into 83 regions of interest. Neuroimage. 2008;40:672–84.
Jain VG, Kline JE, He L, Kline-Fath BM, Altaye M, Muglia LJ, et al. Acute histologic chorioamnionitis independently and directly increases the risk for brain abnormalities seen on magnetic resonance imaging in very preterm infants. Am J Obstet Gynecol. 2022;227:623.e1–13.
Bayley N. Bayley scales of infant and toddler development, third edition: Technical manual. San Antonio, TX: Harcourt Assessment, Inc.; 2006.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55.
Hansen BB, Klopfer SO. Optimal full matching and related designs via network flows. J Comput Graph Stat. 2006;15:609–27.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107.
Ramaswamy VV, Bandyopadhyay T, Nanda D, Bandiya P, Ahmed J, Garg A, et al. Assessment of postnatal corticosteroids for the prevention of bronchopulmonary dysplasia in preterm neonates: a systematic review and network meta-analysis. JAMA Pediatr. 2021;175:e206826.
Moran MM, Gunn-Charlton JK, Walsh JM, Cheong JLY, Anderson PJ, Doyle LW, et al. Associations of neonatal noncardiac surgery with brain structure and neurodevelopment: a prospective case-control study. J Pediatr. 2019;212:93–101.e2.
Stolwijk LJ, Keunen K, de Vries LS, Groenendaal F, van der Zee DC, van Herwaarden MYA, et al. Neonatal surgery for noncardiac congenital anomalies: neonates at risk of brain injury. J Pediatr. 2017;182:335–341.e1.
Morriss FH Jr, Saha S, Bell EF, Colaizy TT, Stoll BJ, Hintz SR, et al. Surgery and neurodevelopmental outcome of very low-birth-weight infants. JAMA Pediatr. 2014;168:746–54.
Gano D, Andersen SK, Glass HC, Rogers EE, Glidden DV, Barkovich AJ, et al. Impaired cognitive performance in premature newborns with two or more surgeries prior to term-equivalent age. Pediatr Res. 2015;78:323–9.
Jansen L, van Steenis A, van den Berg-Huysmans AA, Wiggers-de Bruine ST, Rijken M, de Vries LS, et al. Associations between neonatal magnetic resonance imaging and short- and long-term neurodevelopmental outcomes in a longitudinal cohort of very preterm children. J Pediatr. 2021;234:46–53.e2.
Brouwer MJ, Kersbergen KJ, van Kooij BJM, Benders M, van Haastert IC, Koopman-Esseboom C, et al. Preterm brain injury on term-equivalent age MRI in relation to perinatal factors and neurodevelopmental outcome at two years. PLoS ONE. 2017;12:e0177128.
Acknowledgements
We sincerely thank the parents of infants that participated in our study and the Cincinnati Infant Neurodevelopment Early Prediction Study (CINEPS) Investigators. We also greatly appreciate the support of our NICU fellows, nurses, and staff, and most importantly, all the study families that made this research possible.
Funding
Supported by the National Institutes of Health from the National Institute of Neurological Disorders and Stroke (R01-NS094200, R01-NS096037, and R01-EB029944) to NAP and from the National Center for Advancing Translational Sciences (2UL1TR001425-05A1) to KK.
Author information
Authors and Affiliations
Contributions
KK analyzed and interpreted data and cowrote the article. CL and SE analyzed and interpreted data and were involved in critical revisions. BMKF and SJ collected data and were involved in critical revisions. NAP designed the study, analyzed, and interpreted data, and cowrote the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kojima, K., Liu, C., Ehrlich, S. et al. Early surgery in very preterm infants is associated with brain abnormalities on term MRI: a propensity score analysis. J Perinatol 43, 877–883 (2023). https://doi.org/10.1038/s41372-023-01645-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01645-0