Abstract
Advocacy is an increasingly important skill for neonatologists. As social factors play a greater influence on short & long-term newborn outcomes, neonatal physicians must be attentive to policy factors and work to ensure they benefit the health of both patients and the specialty. In this article, we review advocacy issues of current relevance to neonatal practice, including the “Born Alive Executive Order,” the “Newborn Screening Saves Lives Act,” subspecialty loan repayment and legislation related to donor human milk, as well as introduce topics further discussed as part of the American Academy of Pediatrics Section on Neonatal-Perinatal Medicine Advocacy Series.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Shah S, Brumberg HL. Advocating for advocacy in pediatrics: supporting lifelong career trajectories. Pediatrics. 2014;134:e1523–7.
Hubbard DK, Gievers L, Rao K, Zupancic JAF, Hoffman BD. A blueprint for advocacy in neonatology. Neoreviews. 2022;23:e74–e81.
American Academy of Pediatrics Section on Neonatal-Perinatal Medicine. Section on Neonatal Perinatal Medicine’s History. https://services.aap.org/en/community/aap-sections/sonpm/sonpms-history/. Accessed 18 Oct 2022.
McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff. 2002;21:78–93.
Roberts R. Reviews: health and social organization: towards a health policy for the 21st century. In: David Blane D, Brunner E, Wilkinson R, editors. London: Routledge; 1996
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2016. Natl Vital Stat Rep. 2018;67:1–55.
Martin JA, Hamilton BE, Osterman MJK. Births in the United States, 2017. National Center for Health Statistics Data Brief No. 318. 2018. https://www.cdc.gov/nchs/data/databriefs/db318.pdf. Accessed 22 Aug 2022.
Shah S, Friedman H. Medicaid and moms: the potential impact of expanding medicaid coverage to mother to 1 year after delivery. J Perinatol. 2022;42:819–24.
Daw JR, Sommers BD. Association of the affordable care act dependent coverage provision with prenatal care use and birth outcomes. JAMA. 2018;319:579–87.
Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352:2477–86.
Black MH, Chou H, Sacks DA, Dublin S, Lawrence JM, Harrison TN, et al. Prehypertension prior to or during early pregnancy is associated with increased risk for hypertensive disorders in pregnancy and gestational diabetes. J Hypertens. 2015;33:1860–7.
Idris I, Srinivasan R, Simm A. Maternal hypothyroidism in early and late gestation: effects on neonatal and obstetrical outcome. Clin Endorinol. 2005;63:560–5.
Myerson R, Crawford S, Wherry LR. Medicaid expansion increased preconception health counseling, folic acid intake, an postpartum contraception. Health Aff. 2020;39:1883–90.
Margerison CE, MacCallum CL, Chen J, Zamani-Hank Y, Kaestner R. Impacts of medicaid expansion on health among women of reproductive age. Am J Prev Med. 2020;58:1–11.
Weightman A, Morgan H, Shepherd M, Kitcher H, Roberts C, Dunstan F. Social inequality and infant health in the UK: Systematic review and meta-analyses. BMJ Open. 2012;2:e000964.
Larson CP. Poverty during pregnancy: Its effects on child health outcomes. Paediatr Child Health. 2007;12:673–77.
Brumberg HL, Shah S. Born early and born poor: an eco-bio-developmental model for poverty and preterm birth. J Neonatal Perinat Med. 2015;8:179–87.
DeFranco E, Lian M, Muglia L, Schootman M. Area-level poverty and preterm birth risk: A population-based multilevel analysis. BMC Public Health. 2008;8:316.
Leong M, Karr CJ, Shah SI, Brumberg HL. Before the first breath: why ambient air pollution and climate change should matter to neonatal-perinatal providers. J Perinatol. 2022:1–8.
Spittle A, Orton J, Anderson PJ, Boyd R, Doyle LW. Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database of Systematic Reviews 2015: CD005495. https://doi.org/10.1002/14651858.CD005495.pub4. Accessed 29 Oct 2022.
Minkovitz CS, Grason H, Solomon BS, Kuo AA, O’Connor KG. Pediatricians’ involvement in community child health from 2004 to 2010. Pediatrics. 2013;132:997–1005.
Accreditation Committee on Graduate Medical Education (ACGME) Program Requirements for Graduate Medical Education in Pediatrics. https://www.acgme.org/globalassets/pfassets/programrequirements/320_pediatrics_2022.pdf. Accessed 28 Oct 2022.
Carroll AE, Downs SM. Comprehensive cost-utility analysis of newborn screening strategies. Pediatrics 2006;117:S287–95.
Grosse SD, Van, Vliet G. Challenges in assessing the cost-effectiveness of newborn screening: the example of congenital adrenal hyperplasia. Int J Neonatal Screen. 2020;6:82.
Prosser LA, Grosse SD, Kemper AR, Tarini BA, Perrin JM. Decision analysis, economic evaluation, and newborn screening: challenges and opportunities. Genet Med. 2012;14:703–12.
Tarini BA, Simon NJ, Payne K, Gebremariam A, Rose A, Prosser LA. An assessment of public preferences for newborn screening using best-worst scaling. J Pediatr. 2018;201:62–68.
Alexander D, van Dyck PC. A vision of the future of newborn screening. Pediatrics. 2006;117:S350–4.
Waisbren SE, Albers S, Amato S, Ampola M, Brewster TG, Demmer L, et al. Effect of expanded newborn screening for biochemical genetic disorders on child outcomes and parental stress. JAMA. 2003;290:2564–72.
CDC. CDC grand rounds: newborn screening and improved outcomes. Morb Mortal Wkly Rep. 2012;61:390–3.
Centers for Disease Control and Prevention. Using tandem mass spectrometry for metabolic disease screening among newborns. MMWR Morb Mortal Wkly Rep. 2001;50:1–22.
Tarini BA. The current revolution in newborn screening. new technology, old controversies. Arch Pediatr AdolescMed. 2007;161:767–72.
House Resolution 482-Newborn Screening Saves Lives Reauthorization Act of 2021. https://www.congress.gov/bill/117th-congress/house-bill/482?q=%7B%22search%22%3A%5B%22HR+482+Newborn+Screening+Saves+Lives+Act%22%2C%22HR%22%2C%22482%22%2C%22Newborn%22%2C%22Screening%22%2C%22Saves%22%2C%22Lives%22%2C%22Act%22%5D%7D&s=1&r=1. Accessed 2 Nov 2022.
Health Resources and Services Administration, Advisory Committee on Heritable Disorders in Newborns and Children, Recommended Uniform Screening Panel, Previously Nominated Conditions. https://www.hrsa.gov/advisory-committees/heritable-disorders/rusp/previous-nominations. Accessed 2 Nov 2022.
Ross LF, Paquette ET. The complexities of ascertaining public preferences for newborn screening policies. J Pediatr. 2018;201:8–9.
Hughes R, Fix A. As advancements in treatment drive a newborn screening evolution, will states and the federal government be able to keep up? Health Aff Forefront. 2019. https://www.healthaffairs.org/do/10.1377/forefront.20190816.174106/full/#:~:text=This%20process%2C%20called%20newborn%20screening,that%20would%20otherwise%20go%20undetected. Accessed 2 Nov 2022.
Moyer VA, Calonge N, Teutsch SM, Botkin JR. Expanding newborn screening: process, policy, and priorities. Hastings Cent Rep. 2008;38:32–9.
Trump DJ. Executive Order 13952-Protecting Vulnerable Newborn and Infant Children. 2020. https://www.govinfo.gov/content/pkg/DCPD-202000725/pdf/DCPD-202000725.pdf
Supreme Court of the United States. Dobbs, State Health Officer of the Mississippi Department of Health, et al. v. Jackson Women’s Health Organization et al. https://www.supremecourt.gov/opinions/21pdf/19-1392_6j37.pdf
American Board of Pediatrics. Pediatric Subspecialists Age/Gender Distribution and Summary. Neonatal-Perinatal Medicine. https://www.abp.org/content/pediatric-subspecialists-agegender-distribution-and-summary. Accessed 2 Nov 2022.
Goodman DC, Fisher ES, Little GA, Stukel TA, Chang CH. The uneven landscape of newborn intensive care services: variation in the neonatology workforce. Eff Clin Pract. 2001;4:143–9.
Freed GL. The pediatric subspecialty workforce is more complex than meets the eye. JAMA Pediatr. 2021;175:1006–8.
Calonia J. What’s the average medical school debit in 2022? Forbes. 2022. https://www.forbes.com/advisor/student-loans/average-medical-school-debt/#:~:text=Average%20Medical%20School%20Debt%20for,said%20they%20had%20education%20debt. Accessed 2 Nov 2022.
Pisaniello MS, Asahina AT, Bacchi S, Wagner M, Perry SW, Won M, et al. Effect of medical student debt on mental health, academic performance and specialty choice: a systematic review. BMJ Open. 2019;9:e029980.
Catenaccio E, Rochlin JM, Simon HK. Association of lifetime earning potential and workforce distribution among pediatric subspecialists. JAMA Pediatr. 2021;175:1053–9.
Keller DM, Davis MM, Freed GL. Access to pediatric subspecialty care for children and youth: possible shortages and potential solutions. Pediatr Res. 2020;87:1151–2.
Keller D, Chamberlain LJ. Children and the Patient Protection and Affordable Care Act: opportunities and challenges in an evolving system. Acad Pediatr. 2014;14:225–33.
Shah S, Cheng TL. Optimizing the children’s hospitals graduate medical education payment program at a time of pediatric workforce challenges and health need. J Pediatr. 2022;245:4–6.e2.
Shah S, Kuo AA, Brumberg HL. First aid for Medicaid: losses in children’s health insurance. Pediatr Res. 2021;89:8–11.
Rose AT, Miller ER, Butler M, Eden C, Kim JH, Shah SI, et al. US state policies for Medicaid coverage of donor human milk. J Perinatol. 2022;42:829–34.
Houlahan C. HR 9196: access to donor milk safety act. https://www.congress.gov/117/bills/hr9196/BILLS-117hr9196ih.pdf. 7 Nov 2022.
Handley SC, Lorch SA. Regionalization of neonatal care: benefits, barriers, and beyond. J Perinatol. 2022;42:835–8.
Lewis T, Wade KC, Davis JM. Challenges and opportunities for improving access to approved neonatal drugs and devices. J Perinatol. 2022;42:825–8.
Arnautovic TI, Dammann CEL. The neonatal perspective of paid family medical leave (PFML). J Perinatol. 2022. https://doi.org/10.1038/s41372-021-01300-6
Author information
Authors and Affiliations
Contributions
SS outlined the manuscript, wrote the first draft, made substantial revisions and revised the manuscript. LL made critical revisions to the manuscript, and made substantial contributions to the concept of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shah, S., Lou, L. Advocacy in neonatology: current issues and introduction to the series. J Perinatol 43, 1050–1054 (2023). https://doi.org/10.1038/s41372-023-01615-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01615-6
This article is cited by
-
The National Academies of Sciences, Engineering, and Medicine recommendations on Medicaid parity and future of pediatric subspecialty workforce
Journal of Perinatology (2024)
-
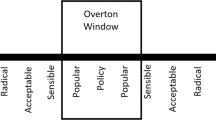
Buy-in and breakthroughs: the Overton window in neonatology for the resuscitation of extremely preterm infants
Journal of Perinatology (2023)