Abstract
Objectives
(1) Assess effects of a modified Family Integrated Care (FICare) model on U.S. Neonatal Intensive Care Unit (NICU) parents; (2) Evaluate NICU nurses’ perspectives.
Design
Case -control design with parental stress assessed before and after NICU-wide FICare implementation using Parent Stressor Scale: NICU (PSS:NICU) questionnaire. In addition, stratification by degree of participation evaluated associations with parental stress, parental-staff communication and discharge readiness. Questionnaires captured nursing perspectives on FICare.
Results
79 parents (88%) participated prior to FICare; 90 (90%) after. Parent stress was lower (p < 0.001) with FICare. Parents learning 5–15 infant-care skills had lower stress compared to those learning <5 (p = 0.008). Parent utilization of an educational app was associated with improved communication frequency (p = 0.007) and quality (p = 0.012). Bedside NICU nurses reported multiple positive associations of FICare for parents and staff.
Conclusions
Any degree of FICare participation decreases parental stress; increased participation has multiple positive associations.
Similar content being viewed by others
Introduction
There is evidence that a collaborative approach between families and healthcare teams can improve outcomes for patients, families and clinicians while simultaneously decreasing healthcare costs and optimizing healthcare resources [1, 2]. Patient- and family-centered care (PFCC) is an approach, endorsed by American Academy of Pediatrics, that was developed to guide the delivery of collaborative healthcare in pediatric care settings. It is a philosophy of care recognizing that the family is the child’s primary source of support and should serve as an integral partner with the healthcare team. The main focus of PFCC is respect, dignity, information sharing, and family participation [1, 3].
General principles of PFCC have been adopted to varying degrees in neonatal intensive care units (NICUs) across the United States (US) in response to what parents often describe as an environment that is stressful and overwhelming [4,5,6,7,8,9,10,11,12,13,14,15,16,17]. However, currently, there is no standardized practice model in the US which fully incorporates parents as members of the care team. Family Integrated Care (FICare) is a novel approach utilized in other countries that is based on PFCC principles but provides a practice framework to integrate parents as care team members [18,19,20,21,22,23,24,25,26].
The original FICare model – introduced in Canada, Australia and New Zealand – requires parents commit 6 h per day, 5 days per week to infant care participation in the NICU. It consists of: (1) environmental resources designed to enhance parent involvement in caregiving while supporting prolonged parental presence in the NICU, (2) NICU team training and support, (3) Parent psychoeducational support including classes and mentorship at bedside, and parents delivering as much infant care as able with nursing supervision/support, (4) Frequent transparent facilitated communication with parents (For example: parent participation in daily rounds), (5) Design and implementation of all key components in partnership with families [20, 21].
Studies conducted in those countries, as well as in others with similar healthcare systems, reported numerous positive effects of FICare participation including increased infant weight gain and exclusive breastfeeding rates, reduced length of stay, improved parent confidence and increased involvement in newborn care, better parental-newborn bonding, as well as lower parental stress, lower anxiety and lower paternal depressive symptoms [20, 22,23,24,25,26]. Similarly, follow-up studies showed improved behavioral skills and outcomes, improved neurodevelopmental outcomes, and lower maternal stress scores at 18 months post-conceptual age [27,28,29,30]. There were no reported adverse effects [20, 22,23,24,25,26].
With the exception of a handful of states offering limited and varying benefits, universal paid family and medical leave policies or free early childcare for older children is not available to new parents in the US. Consequently, while there is some ongoing work examining the feasibility and acceptability of the FICare model in the US, the effects of an adapted model that may be better suited to US parents is currently unknown [31]. Therefore, the aim of this study was to explore the effects of a FICare model modified to include most parents in a typical US NICU setting. Specifically, we examined our model’s effects on parental stress levels, parent-staff communication, and parent readiness for discharge home. In addition, we explored nursing perspectives on the model, as they are key stakeholders in any new bedside-centered care model.
Methods
Study setting and design
This study was conducted at a community hospital that has approximately 3200 deliveries and 450 NICU admissions per year. The Level III NICU has 30 beds and admits 30 – 50 very low birth weight infants annually. The majority (>90%) of admissions are inborn and 10% of infants are transferred to other facilities prior to discharge home. Infants are cared for by a staff of eleven neonatologists, five neonatal nurse practitioners (NNPs), eight pediatric/neonatal certified respiratory therapists, and seventy registered bedside nurses. There are two NICU lactation consultants, two speech pathology consultants, two nutritionists, two occupational therapists and one social worker available daily. No physicians in training participate in patient care. As standard practice, parents are not offered overnight stays due to a lack of private rooms in the unit.
Beginning in September 2019 the modified FICare model was implemented in the NICU after a 12 month preparatory and staff training period and was offered to families prior to mothers’ discharge home. It consists of similar elements as described in the original RCT, but without any required number of days/hours for parents to participate [20, 21].
The educational program consists of one-on-one bedside teaching by different disciplines (i.e., nursing, nutritionists, etc.) as well as utilization of a mobile phone application (app), SSH NICU FIcare South Shore Health System App, designed and built by in-house NICU staff while incorporating feedback from former NICU parents [21]. The app serves as a supplemental educational resource for parents and is divided into seven sections: Orientation to FICare, Feeding Your Baby, Developmental Care, Basic Skills, Lactation Support, Discharge, and Taking Care of You. Each section concludes with an optional quiz parents can complete at their leisure. The app does not feature any report back or communication with staff capabilities and completion of the educational sections is not a requirement for participation in the FICare program. It is offered to all families during prenatal consultation, if conducted, or shortly after an infant’s NICU admission.
Additional elements of the program emphasize “hands-on skills coaching” at the bedside by nurses as well as daily or near-daily parental participation in multidisciplinary rounds either in person or by speaker phone (chosen based on solicited feedback from NICU parents who overwhelmingly preferred to receive phone calls from the rounding team over tele-video calls).
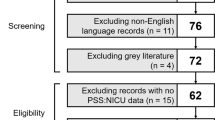
After FICare had been established for 16 months, the research team utilized a quantitative questionnaire case-control design to evaluate the effects of the program (Fig. 1). Parental stress levels after FICare implementation were compared to controls who had completed the same parent stress questionnaire prior to FICare implementation as part of another study [32]. Stress, parent-staff communication, and readiness for discharge home were further stratified by the level of parental involvement in FICare. FICare participating parents were also given anonymous questionnaires aimed at exploring their opinions of the program. At the end of the parent recruitment period, nursing staff were given electronic questionnaires to share their perspectives on the program’s effects.
Parental stress levels measured prior to FICare implementation as part of another study compared to parental stress levels after FICare implemention. PSS: NICU questionnaire utilized to capture parental stress levels prior and after FICare implementation. Additional questionnaires utilized to capture effects of degree participation in FICare on stress levels, communication and discharge readiness.
Participant recruitment and data collection
Data was collected between February and September 2021. IRB approval was obtained prior to commencement of participant recruitment.
We utilized a standard survey approach (without incentives) with three prospective questionnaires given to parents at various time points (Fig. 1). All parents of infants admitted to the NICU for at least 7 days were eligible to participate. Exclusion criteria included non-English speaking parents, those younger than 18 years of age and NICU length of stay <7 days. Study personnel identified and approached eligible parents on infant day of life 30 or within 7 days of anticipated discharge, whichever came first. Following consent, they were offered the first questionnaire either on paper or electronically built into the REDCap data capture tool hosted by Boston Children’s Hospital [33]. Study participation was anonymous, therefore each parent was assigned a unique identification number to connect all survey tools and track response rates. Paper survey responses were entered into REDCap by study stuff and data entry accuracy was checked by a second team member. Parents received one in-person reminder by study personnel within 48 h from initial invitation.
All nurses working in the NICU during the study period were eligible to participate. Nurses were sent an e-mail link to the electronic questionnaire and received two e-mail reminders for completion. Responses were hosted by REDCap and were anonymous [33].
Data collection instruments and timing of administration
Figure 1 details the study timeline and survey instruments used. Parent questionnaires used in both periods used the validated tool, Parent Stressor Scale: NICU (PSS: NICU, version 2015) to measure parental stress. The PSS: NICU consists of 26 items, which form three subscales assessing stress related to infant appearance and behavior (14 items), parental role alteration (7 items) and sights and sounds in the NICU (5 items). The PSS: NICU has good concurrent and predictive validity and is internally consistent with Cronbach alpha ranging from 0.73 to 0.94. All de novo questionnaires were refined through iterative panel review by experienced survey researchers and content experts. The resulting surveys underwent content validity testing with two neonatologists and a biostatistician as well as cognitive validity pretesting by parents and nurses. Survey instruments are available as Online Supplementary Material 1.
The “Infant Care Bedside Skills Checklist” and the “Discharge Skills Checklist” were utilized as a measure of degree of parental participation and a measure of discharge readiness, respectively. The fifteen bedside skills were infant bathing, checking PG tube placement, PG feeding, administering PG medications, taking vital signs, taking temperature, kangaroo care, dressing, swaddling, oral feeding, administering oral medications, checking breastmilk labels, warming milk, weighing infants, diaper care. The six discharge skills were discharge class completion, discussing safe sleep, discussing home feeding plan, learning milk preparation, reinforcing oral medication administration, and discussing follow-up appointments.
Definitions
Degree of parental participation in FICare was defined by: (1) frequency of parental participation in rounds measured by aggregate sum of answers to ordinal scale questions (4 = always, 1 = never); (2) frequency of app utilization by aggregate sum of answers to ordinal scale questions (3 = every day, 1 = less than once a week) and; (3) infant care bedside skills checklist completion.
Parent-staff communication frequency was defined as frequency of parental communication with eight clinicians measured by aggregate sum of answers to ordinal scale questions reflecting perceived communication (4 = always, 1 = never). Parent-staff communication quality was defined consistency and clarity in answering parents’ questions by nurses, nurse practitioners and physicians as measured by aggregate of two variables captured by responses to the statements: “Answers to my questions were easy to understand” and “I received consistent information from…”
Parent discharge readiness was defined by: (1) completion of the discharge skills checklist captured by aggregate score of completing up to six items; (2) parental confidence in seven infant care skills measured by aggregate score and; (3) aggregate score of five questions on the post-discharge follow-up questionnaire.
Data analysis
Sample sizes were based on ability to test for a difference of 10 points on the PSS:NICU scale utilizing a non-parametric test (Wilcoxon-Mann-Whitney). Group sample sizes of 80 parents achieved 100% power to detect a difference of 10.0 points at the 0.050 significance level (alpha) using a two-sided Mann-Whitney Test.
The PSS:NICU was scored according to proprietary scoring guidelines [8, 34, 35]. PSS variables were found to be non-normal; Wilcoxon and other nonparametric tests were used for all continuous variables. Fisher’s exact test was used for all contingency table analysis. Parent and nursing perceptions questions and demographic questions were summarized by the counts and percentage of responses. Linear regression models of stress were adjusted by gestational age, financial demands, and time for commute to hospital.
Results
Seventy-nine parents completed the PSS: NICU survey prior to FICare implementation (88% response rate) and ninety parents completed it after (90% response rate). There were no significant differences in parental demographic characteristics or infants’ gestational ages, birth weights and severity of infant illness between groups (Table 1). Additionally, during both study periods no infants were discharged home requiring supplemental oxygen. NICU-wide, four infants during the pre-Ficare time period had a diagnosis of chronic lung disease, three were diagnosed with severe (Grade III or IV) intraventricular hemorrhage (IVH) and two had severe retinopathy of prematurity (ROP.) During the recruitment period following FIcare implementation, no infants in the NICU had a diagnosis of chronic lung disease, two had severe IVH and none were diagnosed with severe ROP.
Parental stress
Parental stress scores after FICare implementation (FICare group) were significantly lower compared to the pre-implementation group (median PSS:NICU score 61.5 (IQR 51, 73) vs 94 (IQR 75.9, 112) respectively, p < 0.001). Additionally, scores in all three subscales were significantly lower in the FICare group (p < 0.001) (Fig. 2).
The scatter plots represent the distribution of individual PSS scores for each group. The box plots that overlay the scatter plots present median (center line), first and third quartiles (lower and upper ends of each box, Q1, Q3). The outer “whiskers” at each end represent 1.5 times the interquartile range (Q3–Q1) above and below Q1 and Q3, respectively. The lack of overlap between the two boxplots reflects the significancy of difference between PSS scores between the two groups (p < 0.001).
Parental stress within FICare group stratified by degree of participation
Within the FICare group, parents who learned more than five infant care bedside skills had significantly lower stress levels (median PSS:NICU score 58.0 (IQR 44.0, 63.0)), compared to those who learned 1–5 skills (median PSS:NICU score 64.5 (IQR 57.10, 78.50), p = 0.008)).
Sixty-nine of 74 (93%) of parents reported always participating in daily multidisciplinary rounds and sixty-five (88%) of parents reported utilizing the educational app during NICU stay. Neither parental frequency of participation in daily rounds or frequency of mobile app usage were found to have further stratification effects on parental stress.
With respect to demographic confounders within the FICare group, parents who reported difficult financial demands and those who had to travel more than 30 min from home to hospital had significantly higher PSS:NICU scores (p < 0.005 and p < 0.001, respectively) (Table 2). Additionally, mothers/pregnant persons versus fathers/partners and those who self-identified their race as white were found to have higher stress scores (p = 0.02 and p < 0.001, respectively). There were no associations found between parental stress and infant gestational age, length of stay or birth weight.
Parent-staff communication
Effects of degree of parental participation in FICare on parent-staff communication were captured by Parental FICare Questionnaire (Fig. 1). Increased parental utilization of the mobile app significantly increased parent-staff communication frequency (coefficient estimate: 4.9, p = 0.007). Increased mobile app utilization also increased positive scores of parent-reported communication quality (coefficient estimate: 1.8, p = 0.012).
Statistical analysis of the association between communication and parent participation in rounds was not found to be meaningful, as parents overwhelmingly participated in rounds.
Discharge readiness (Fig. 1)
Increased frequency of parent-staff communication was significantly associated with parental completion of a pre-discharge checklist (coefficient estimate: 0.58, p < 0.001). None of the other variables, including participation in rounds, utilization of the FICare app or completion of the infant care bedside skills list was found to have a statistically significant effect on parent-reported discharge readiness.
Nurses’ perspectives
Fifty-one bedside nurses completed surveys (73% response rate). They reported multiple positive effects of FICare implementation in the NICU for both parents and staff with no reported negative effects (Table 3). With respect to their own work, nurses did not believe that FICare increased nursing work-related stress (p = 0.009) but did report that it resulted in an increase in nursing job-satisfaction (p = 0.0001). They also reported that FICare improved their perceptions of parental readiness for discharge (p < 0.0001) and parental confidence to take their infant home (p < 0.0001) as well as made it easier for nurses to discharge infants home (p < 0.001).
Discussion
To our knowledge, this is the first completed study examining the effects of implementing a modified FICare model in a US NICU. FICare originated in countries where universal healthcare and extended parental leave (currently up to 18 months in Canada) are the norm and parents commit to be present in the hospital for very extended periods of time (6–8 h a day 5 days a week) in order to participate [20]. Since current policies and social realities make this requirement of parents unfeasible in many, if not most, US healthcare settings, we modified our model to be able to include any family regardless of how much time they are able to participate and supplement in-person experiences with a non-interactive educational mobile app and daily telephone rounds. Even with these modifications, we found significant positive effects for both parents and nurses after implementation.
Overall, we found that parents’ stress scores were significantly lower after NICU-wide implementation of FICare. These stress scores were further decreased by increased participation in learning infant care bedside skills. Other than FICare, no other major changes had been made in the NICU between the two recruitment periods that could potentially explain this difference in scores. We believe this effect is especially notable given that the FICare group was recruited during the COVID-19 pandemic when strict hospital visitor restrictions, parental isolation and increased reported stress levels in the overall population could have dampened these positive findings [36].
Various components of our FICare model seemed to have positive effects on specific aspects of parental experiences and responses. First, parent-staff communication frequency and quality were both found to be significantly improved with increased utilization of the mobile app. We hypothesize that this may be related to improved parental knowledge and/or feelings of empowerment, stimulating questions from parents for staff. Additionally, by providing parents with an easily-accessible reference of information to peruse at their leisure, it is possible their feelings of being overwhelmed by complex medical information may be lessened.
Parental participation at daily rounds was overwhelmingly high with 93% of parents reporting that they always participated. While this made attempts at intragroup statistical stratification less meaningful, we can extrapolate that the very high parental participation implies that parents find the activity beneficial in that it offers a regularly scheduled opportunity for communication. Importantly, we have shown that including parents daily in rounds is feasible, even when parents may not be able to be present in-person.
While we did not find that increased participation in FICare improved parent-reported readiness for discharge within the FICare group, nurses overwhelmingly perceived that this care model improved parental confidence and discharge readiness and made it easier to discharge an infant home compared to before FICare implementation. This suggests that there may indeed be a benefit with respect to discharge readiness that we were not able to capture in our study. A future randomized controlled trial may be better able to elucidate such an effect.
Within the FICare group, parents with difficult financial demands and those who had to travel further distances to the hospital reported higher stress levels. This suggests that while utilizing a mobile app or calling parents on the phone for daily rounds are beneficial to the overall parent population, they do not completely mitigate the effects of certain socioeconomic and demographic stressors. These variables highlight specific areas in which more attention needs to be paid when implementing new care models or policies either in hospitals or larger communities, including but not limited to recent trends in regionalization of pediatric inpatient and specialty care [37,38,39].
Finally, our study found that nurses reported multiple positive effects of FICare. Importantly, they did not report that it increased their work-load, which is a balancing measure that should be considered when implementing new programs in any healthcare setting.
Our results should be considered in light of a few limitations. With respect to potential confounding variables that could have affected outcomes between the two groups, as mentioned above, the current study was conducted during the COVID-19 pandemic. During that time, up to two parents, but no other visitors, were allowed to care for their infants from 8am–8pm. The pre-FICare group was recruited pre-pandemic and therefore was allowed unrestricted visits of parents and other family members 24 h per day. While this difference could be perceived as a limitation, for the reasons stated above, it might alternatively make our results even more meaningful. Additionally, our study population was mostly white and highly educated; parents less than 18 years old were excluded due to IRB approval limitations and the very small population of teenage parents in our NICU. This makes our findings less generalizable to more diverse patient populations. Finally, we acknowledge that parents were approached for study participation by research team members who were also part of the infants’ clinical team. This may have introduced bias in parental responses, however non-clinical personnel were not available to consent or administer anonymous questionnaires.
Conclusions
In conclusion, our study found that a modified FICare model in a US NICU setting has utility, with positive effects on parents and nurses. Any degree of participation in FICare significantly decreases parental stress levels and increased participation in hands-on care and utilization of educational materials has additional benefits. Future studies should examine the effects of our modified model in more diverse patient populations and in settings that include medical trainees. Additionally, work can be done exploring resource utilization and the potential for cost-effectiveness.
Data availability
The datasets generated during and analyzed during the current study are not publicly available due to IRB restrictions but are available from the corresponding author on reasonable request.
References
American Academy of Pediatrics, Committee on Hospital Care and Institute for Patient- and Family-Centered Care. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129:394–404.
Meert KL, Clark J, Eggly S. Family-centered care in the pediatric intensive care unit. Pediatr Clin North Am. 2013;60:761–72.
Everhart JL, Haskell H, Khan A. Patient- and family-centered care: leveraging best practices to improve the care of hospitalized children. Pediatr Clin North Am. 2019;66:775–89.
Moore KA, Coker K, DuBuisson AB, Swett B, Edwards WH. Implementing potentially better practices for improving family-centered care in neonatal intensive care units: successes and challenges. Pediatrics. 2003;111:e450–60.
Gooding JS, Cooper LG, Blaine AI, Franck LS, Howse JL, Berns SD. Family support and family-centered care in the neonatal intensive care unit: origins, advances, impact. Semin Perinatol. 2011;35:20–8. https://doi.org/10.1053/j.semperi.2010.10.004.
Turner M, Chur-Hansen A, Winefield H, Stanners M. The assessment of parental stress and support in the neonatal intensive care unit using the Parent Stress Scale - Neonatal Intensive Care Unit. Women Birth. 2015;28:252–8.
Woodward LJ, Bora S, Clark CA, Montgomery-Hönger A, Pritchard VE, Spencer C, et al. Very preterm birth: maternal experiences of the neonatal intensive care environment. J Perinatol. 2014;34:555–61.
Shields-Poe D, Pinelli J. Variables associated with parental stress in neonatal intensive care units. Neonatal Netw. 1997;16:29–37.
Miles MS, Funk SG, Kasper MA. The neonatal intensive care unit environment: sources of stress for parents. AACN Clin Issues Crit Care Nurs. 1991;2:346–54.
Dudek-Shriber L. Parent stress in the neonatal intensive care unit and the influence of parent and infant characteristics. Am J Occup Ther. 2004;58:509–20.
Miles MS, Holditch-Davis D. Parenting the prematurely born child: pathways of influence. Semin Perinatol. 1997;21:254–66.
Haward MF, Lantos J, Janvier A, POST Group. Helping Parents Cope in the NICU. Pediatrics. 2020;145:e20193567. https://doi.org/10.1542/peds.2019-3567.
Bernardo J, Rent S, Arias-Shah A, Hoge MK, Shaw RJ. Parental stress and mental health symptoms in the NICU: recognition and interventions. Neoreviews. 2021;22:e496–505. https://doi.org/10.1542/neo.22-8-e496.
Lotterman JH, Lorenz JM, Bonanno GA. You can’t take your baby home yet: a longitudinal study of psychological symptoms in mothers of infants hospitalized in the NICU. J Clin Psychol Med Settings. 2019;26:116–22. https://doi.org/10.1007/s10880-018-9570-y.
Treyvaud K. Parent and family outcomes following very preterm or very low birth weight birth: a review. Semin Fetal Neonatal Med. 2014;19:131–5. https://doi.org/10.1016/j.siny.2013.10.008.
Roque ATF, Lasiuk GC, Radünz V, Hegadoren K. Scoping review of the mental health of parents of infants in the NICU. J Obstet Gynecol Neonatal Nurs. 2017;46:576–87. https://doi.org/10.1016/j.jogn.2017.02.005.
Pham T, Hua A, Li D, Bar S, Spinazzola R, Milanaik R. Leading stress factors reported by parents of NICU infants. Pediatrics. 2018;141:533. https://doi.org/10.1542/peds.141.1MA6.533.
Franck LS, O’Brien K. The evolution of family-centered care: from supporting parent-delivered interventions to a model of family integrated care. Birth Defects Res. 2019;111:1044–59.
Franck LS, Waddington C, O’Brien K. Family integrated care for preterm infants. Crit Care Nurs Clin North Am. 2020;32:149–65.
O’Brien K, Robson K, Bracht M, Cruz M, Lui K, Alvaro R, et al. FICare Study Group and FICare Parent Advisory Board. Effectiveness of Family Integrated Care in neonatal intensive care units on infant and parent outcomes: a multicenter, multinational, cluster-randomized controlled trial. Lancet Child Adolesc Health. 2018;2:245–54.
SSH NICU FICare South Shore Health System App. http://familyintegratedcare.com/implementing-ficare/program-development/.
Fraser C, Harrison CM. Family-integrated care for preterm infants in China. Arch Dis Child Educ Pr Ed. 2021;26:2021–321842. https://doi.org/10.1136/archdischild-2021-321842.
He SW, Xiong YE, Zhu LH, Lv B, Gao XR, Xiong H, et al. Impact of family integrated care on infants’ clinical outcomes in two children’s hospitals in China: a pre-post intervention study. Ital J Pediatrics. 2018;44:65.
Benzies KM, Aziz K, Shah V, Faris P, Isaranuwatchai W, Scotland J, et al. Alberta FICare Level II NICU Study Team. Effectiveness of Alberta Family Integrated Care on infant length of stay in level II neonatal intensive care units: a cluster randomized controlled trial. BMC Pediatrics. 2020;20:535.
Broom M, Parsons G, Carlisle H, Kecskes Z, Thibeau S. Exploring parental and staff perceptions of the family-integrated care model: a qualitative focus group study. Adv Neonatal Care. 2017;17:e12–9.
van Veenendaal NR, van Kempen AAMW, Broekman BFP, de Groof F, van Laerhoven H, van den Heuvel MEN, et al. Association of a zero-separation neonatal care model with stress in mothers of preterm infants. JAMA Netw Open. 2022;5:e224514.
Church PT, Grunau RE, Mirea L, Petrie J, Soraisham AS, Synnes A, et al. Family Integrated Care (FICare): Positive impact on behavioural outcomes at 18 months. Early Hum Dev. 2020;151:105196.
Synnes AR, Petrie J, Grunau RE, Church P, Kelly E, Moddemann D, et al. Canadian Neonatal Network Investigators; Canadian Neonatal Follow-Up Network Investigators. Family integrated care: very preterm neurodevelopmental outcomes at 18 months. Arch Dis Child Fetal Neonatal Ed. 2022;107:76–81.
Mclean MA, Scoten OC, Yu W, Ye XY, Petrie J, Church PT, et al. Lower maternal chronic physiological stress and better child behavior at 18 months: follow-up of a cluster randomized trial of neonatal intensive care unit family integrated care. J Pediatrics. 2022;243:107–15:e4.
Banerjee J, Aloysius A, Mitchell K, Silva I, Rallis D, Godambe SV, et al. Improving infant outcomes through implementation of a family integrated care bundle including a parent supporting mobile application. Arch Dis Child Fetal Neonatal Ed. 2020;105:172–7.
Franck LS, Kriz RM, Bisgaard R, Cormier DM, Joe P, Miller PS, et al. Comparison of family centered care with family integrated care and mobile technology (mFICare) on preterm infant and family outcomes: a multi-site quasi-experimental clinical trial protocol. BMC Pediatr. 2019;19:469. https://doi.org/10.1186/s12887-019-1838-3.
Kubicka Z, Zahr E, Clark P, Williams D, Berbert L, Arzuaga B. Use of an internet camera system in the neonatal intensive care unit: parental and nursing perspectives and its effects on stress. J Perinatol. 2021;41:2048–56.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG, et al. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42:377–81.
Miles MS, Funk SG, Carlson J. Parental stressor scale: neonatal intensive care unit (PSS: NICU). Nurs Res. 1993;42:148–52.
Franck LS, Cox S, Allen A, Winter I. Measuring neonatal intensive care unit-related parental stress. J Adv Nurs. 2005;49:608–15.
Flaskerud JH. Stress in the age of COVID-19. Issues Ment Health Nurs. 2021;42:99–102. https://doi.org/10.1080/01612840.2020.1829217.
Salazar JH, Goldstein SD, Yang J, Gause C, Swarup A, Hsiung GE, et al. Regionalization of pediatric surgery: trends already underway. Ann Surg. 2016;263:1062–6.
Cushing AM, Bucholz E, Michelson KA. Trends in regionalization of emergency care for common pediatric conditions. Pediatrics. 2020;145:e20192989.
Riese J, Alverson B. The role of financial drivers in the regionalization of pediatric care. Pediatrics. 2021;148:e2021050432.
Acknowledgements
We wish to thank the many parents who reviewed drafts of the materials contained in the FICare app as well as the neonatal nurse practitioners, NICU nurses, occupational therapists, speech language pathologists, lactation consultants, respiratory therapists, dieticians and pharmacists who created the FICare app contents. We also wish to thank Luke Poppish who moved the FICare app into production. In addition, we would like to thank NICU nurses and parents participating in the study.
Funding
There was no funding source for this project with the exception of financial support coming from the Department of Pediatrics at South Shore Hospital (Department Chair, Mark Waltzman, MD) limited to the following: a senior statistician from Institutional Centers for Clinical and Translational Studies at Boston Children’s Hospital, David N. Williams, MA, PhD received compensation for his involvement in all aspects from the initial questionnaire design, edits, data analysis.
Author information
Authors and Affiliations
Contributions
ZK and BA conceptualized and designed the study, designed the data collection instruments, coordinated and supervised data collection, recruited patients, collected data, drafted the initial manuscript, and reviewed and revised the manuscript. JF, EZ, AD, DP, TR and ML contributed to designing the study, participated in patient recruitment, data collection, and reviewed and revised the manuscript. DW conceptualized and designed the study, contributed to designing questionnaires, carried out the initial and final statistical analyses, and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kubicka, Z., Fiascone, J., Williams, D. et al. Implementing modified family integrated care in a U.S. neonatal intensive care unit: nursing perspectives and effects on parents. J Perinatol 43, 503–509 (2023). https://doi.org/10.1038/s41372-023-01601-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01601-y