Abstract
Introduction
Racial disparity exists in U.S. neonatal mortality; Black, non-Hispanic neonates are at higher risk of death. We aim to examine overall and race-specific neonatal mortality within the Military Health System (MHS).
Methods
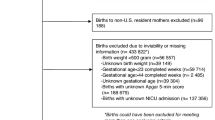
Retrospective cohort study of infants delivered within the MHS between 2013–2015. Variables were extracted from the Military Health System Data Repository.
Results
There were 320,283 live births within the MHS from 2013–2015; 588 neonates died, a death rate of 1.84/1000. Cohort neonatal mortality and incidence of preterm delivery (7.2%) were lower than concurrent U.S. statistics. Black, non-Hispanic neonates had a 2-fold increased risk of death (OR: 2.11; 95% CI 1.73–2.56, p < 0.001) over White, non-Hispanic neonates. Officer versus enlisted rank conferred no difference in neonatal mortality (OR: 0.88; 95% CI 0.74–1.03).
Conclusion
Neonatal mortality within the MHS is lower than in the U.S. Despite universal insurance coverage and access to care, racial disparity persists. Risk of death is not modified by socioeconomic status. These findings highlight the need for critical examination of healthcare equity within neonatal-perinatal medicine.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Available upon request
References
Ely DM, Driscoll AK. Infant mortality in the United States, 2017: Data from the period linked birth/infant death file. Natl Vital- Stat Rep. 2019;68:1–20.
UNICEF, UNICEF Global Databases; Child mortality estimates: Country-specific neonatal mortality rate. Available at https://data.unicef.org/topic/child-survival/neonatal-mortality/, accessed September, 2022.
Govande V, Ballard AR, Koneru M, Beeram M. Trends in the neonatal mortality rate in the last decade with respect to demographic factors and health care resources. Bayl Univ Med Cent Proc. 2015;28:304–6.
Matthews TJ, MacDorman MF, Thoma ME. Infant mortality statistics from the 2013 period linked birth/infant death data set. Natl Vital- Stat Rep. 2015;64:1–30.
Euro-Peristat Project. European Perinatal Health Report. Core indicators of the health and care of pregnant women and babies in Europe in 2015. November 2018. Available at www.europeristat.com
MacDorman MF, Mathews TJ. Behind international rankings of infant mortality: how the United States compares with Europe. NCHS Data Brief. 2009;23:1–8.
Mathews TJ, Driscoll AK. Trends in infant mortality in the United States, 2005-2014. NCHS Data Brief. 2017;279:1–8.
Grobman WA, Parker CB, Willinger M, Wing DA, Silver RM, Wapner RJ, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (nuMoM2b) Network*. Racial Disparities in Adverse Pregnancy Outcomes and Psychosocial Stress. Obstet Gynecol. 2018;131:328–35.
Wallace ME, Mendola P, Kim SS, Epps N, Chen Z, Smarr M, et al. Racial/ethnic differences in preterm perinatal outcomes. Am J Obstet Gynecol. 2017;216:306.e1–306.
He X, Akil L, Aker WG, Hwang HM, Ahmad HA. Trends in infant mortality in the United States: a brief study of the Southeastern states from 2005-2009. Int J Enivorn Res Public Health. 2015;12:4908–20.
Elder TE, Goddeeris JH, Haider SJ. Racial and ethnic infant mortality gaps and the role of socio-economic status. Labour Econ. 2016;43:42–54.
Matoba N, Collins JW Jr. Racial disparity in infant mortality. Semin Perinatol. 2017;41:354–9.
Owens-Young J, Bell CN. Structural racial inequities in socioeconomic status, urban-rural classification and infant mortality in US counties. Ethn Dis. 2020;30:389–98.
DHA. (2022). Patient Care Numbers for the Military Health System. Defense Health Agency. Available at https://www.health.mil/Military-Health-Topics/MHS-Toolkits/Media-Resources/Media-Center/Patient-Care-Numbers-for-the-MHS, accessed September, 2022.
DHA. (2021). Evaluation of the TRICARE Program: Fiscal Year 2021 Report to Congress. Access, Cost, and Quality Data through Fiscal Year 2020. Washington, DC: Defense Health Agency. Available at https://www.health.mil/I-Am-A/Media/Media-Center/MHS-Health-Facilities, accessed September, 2022.
GAO. (2016). Availability and quality measurement of women’s health care services in US Military Hospitals. (GAO-16-596). U.S. GAO. Available at https://www.gao.gov/assets/gao-16-596.pdf, accessed September, 2022.
Engelhardt K, Hisle-Gorman E, Gorman GH, Dobson NR. Lower preterm birth rates but persistent racial disparities in an open-access health care system. Mil Med. 2018;183:e570–e575.
Rawlings JS, Weir MR. Race- and rank-specific infant mortality in a US military population. Am J Dis Child. 1992;146:313–6.
Alexander GR, Baruffi G, Mor JM, Kieffer EC, Hulsey TC. Multiethnic variations in the pregnancy outcomes of military dependents. Am J Public Health. 1993;83:1721–5.
Stahlman S, Witkop CT, Clark LL, Taubman SB. Pregnancies and live births, active component service women, U.S. Armed Forces, 2012-2016. MSMR 2017;24:2–9.
Office of the Secretary of Defense. Maternal and infant mortality rates in the military health system. 2019. Requested by: Conference Report 115-874, Page 861 to Accompany the John S. McCain National Defense Authorization Act for Fiscal Year 2019 (Public Law 115-232).
Thakrar AP, Forrest AD, Maltenfort MG, Forrest CB. Child mortality in the US and 19 OECD comparator nations: A 50-year time-trend analysis. Health Aff (Millwood). 2018;37:140–9.
MacDorman MF, Matthews TJ, Mohangoo AD, Zeitlin J. International comparisons of infant mortality and related factors: United States and Europe, 2010. Natl Vital- Stat Rep. 2014;63:1–6.
Vintzileos AM, Ananth CV, Smulian JC, Scorza WE, Knuppel RA. The impact of prenatal care on neonatal deaths in the presence and absence of antenatal high-risk conditions. Am J Obstet Gynecol. 2002;186:1011–6.
Bhatt CB, Beck-Sagué CM. Medicaid expansion and infant mortality in the United States. Am J Public Health. 2018;108:565–7.
Morriss FH Jr. Increased risk of death among uninsured neonates. Health Serv Res. 2013;48:1232–55.
Debiec KE, Paul KJ, Mitchell CM, Hitti JE. Inadequate prenatal care and risk of preterm delivery among adolescents: a retrospective study over 10 years. Am J Obstet Gynecol. 2010;203:122.e1–6.
Vintzileos AM, Ananth CV, Smulian JC, Scorza WE, Knuppel RA. The impact of prenatal care in the United States on preterm births in the presence and absence of antenatal high-risk conditions. Am J Obstet Gynecol. 2002;187:1254–7.
Partridge S, Balayla J, Holcroft CA, Abenhaim HA. Inadequate prenatal care utilization and risks of infant mortality and poor birth outcome: a retrospective analysis of 28,729,765 U.S. deliveries over 8 years. Am J Perinatol. 2012;29:787–93.
Singh GK, Yu SM. Infant Mortality in the United States, 1915-2017: Large social inequalities have persisted for over a century. Int J MCH AIDS. 2019;8:19–31.
Alexander GR, Wingate MS, Bader D, Kogan MD. The increasing racial disparity in infant mortality rates: composition and contributors to recent US trends. Am J Obstet Gynecol. 2008;198:51.e1–9.
MacDorman MF, Mathews TJ. Understanding racial and ethnic disparities in U.S. infant mortality rates. NCHS Data Brief. 2011;74:1–8.
Pabayo R, Cook DM, Harling G, Gunawan A, Rosenquist NA, Muennig P. State-level income inequality and mortality among infants born in the United States 2007-2010: A Cohort Study. BMC Public Health. 2019;19:1333.
Braveman PA, Heck K, Egerter S, Marchi KS, Dominguez TP, Cubbin C, et al. The role of socioeconomic factors in Black-White disparities in preterm birth. Am J Public Health. 2015;105:694–702.
Kothari CL, Paul R, Dormitorio B, Ospina F, James A, Lenz D, et al. The interplay of race, socioeconomic status and neighborhood residence upon birth outcomes in a high black infant mortality community. SSM Popul Health. 2016;2:859–67.
Colen CG, Geronimus AT, Bound J, James SA. Maternal upward socioeconomic mobility and black-white disparities in infant birthweight. Am J Public Health. 2006;96:2032–9.
Montoya-Williams D, Fraiman YS, Pena MM, Burris HH, Pursley DM. Antiracism in the field of neonatology: A foundation and concrete approaches. Neoreviews. 2022;21:e1–e12.
Haas DM, Parker CB, Marsh DJ, Grobman WA, Ehrenthal DB, Greenland P, et al. Association of adverse pregnancy outcomes with hypertension 2 to 7 Years Postpartum. J Am Heart Assoc. 2019;8:e013092.
Manuck TA. Racial and ethnic differences in preterm birth: A complex, multifactorial problem. Semin Perinatol. 2017;41:511–8.
Hall C, Romano CJ, Bukowinski AT, Gumbs GR, Dempsey KN, Poole AT, et al. Severe maternal morbidity among women in the U. S. military, 2003-2015. Am J Perinatol. 2021. https://doi.org/10.1055/s-0041-1740248. Epub ahead of print.
Braveman P, Dominguez TP, Burke W, Dolan SM, Stevenson DK, Jackson FM, et al. Explaining the Black-White disparity in preterm birth: A consensus statement from a multi-disciplinary scientific work group convened by the March of Dimes. Front Reprod Health. 2021;3:684207.
Saluja B, Bryant Z. How Implicit bias contributes to racial disparities in maternal morbidity and mortality in the United States. J Women’s Health (Larchmt). 2021;30:270–3.
Chin MH, Walters AE, Cook SC, Huang ES. Interventions to reduce racial and ethnic disparities in health care. Med Care Res Rev. 2007;64:7S–28S.
Acknowledgements
N/A
Author information
Authors and Affiliations
Contributions
RJV designed the study, participated in analysis, contributed to manuscript creation and revision; MN participated in analysis, contributed to manuscript creation and revision; GHR designed the study, participated in analysis, contributed to manuscript creation and revision; JKA designed the study, performed statistical analysis, contributed to manuscript creation and revision; CMD designed the study, participated in analysis, contributed to manuscript creation and revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was deemed exempt by the Brooke Army Medical Center Institutional Review Board (reference number C.2019.096n).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vereen, R.J., Nestander, M., Haischer-Rollo, G. et al. Neonatal mortality and disparities within the military health system. J Perinatol 43, 496–502 (2023). https://doi.org/10.1038/s41372-022-01598-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01598-w