Abstract
Objective
To assess the association of NICU occupancy with probability of discharge and length of stay (LOS) among infants born <33 weeks gestational age (GA).
Study design
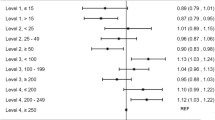
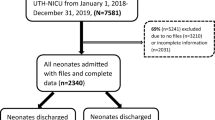
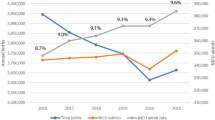
Retrospective study of 3388 infants born 23–32 weeks GA, admitted to five Level 3/4 NICUs (2014-2018) and discharged alive. Standardized ratios of observed-to-expected number of discharges were calculated for each quintile of unit occupancy. Multivariable linear regression models were used to assess the association between occupancy and LOS.
Results
At the lowest unit occupancy quintiles (Q1 and Q2), infants were 12% and 11% less likely to be discharged compared to the expected number. At the highest unit occupancy quintile (Q5), infants were 20% more likely to be discharged. Highest occupancy (Q5) was also associated with a 4.7-day (95% CI 1.7, 7.7) reduction in LOS compared Q1.
Conclusion
NICU occupancy was associated with likelihood of discharge and LOS among infants born <33 weeks GA.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data for this study cannot be shared publicly as it is bound by confidentiality agreements governed by hospital and government privacy offices. Aggregate data may be made available from the corresponding author [MB] on reasonable request.
References
Beltempo M, et al. on behalf of the Canadian Neonatal Network Annual Report Committee. Canadian Neonatal Network 2020 Annual report. Toronto, Ontario; 2021.
Lee SK, Beltempo M, McMillan DD, Seshia M, Singhal N, Dow K, et al. Outcomes and care practices for preterm infants born at less than 33 weeks’ gestation: a quality-improvement study. CMAJ. 2020;192:E81–E91.
Lee HC, Bennett MV, Schulman J, Gould JB, Profit J. Estimating length of stay by patient type in the neonatal intensive care unit. Am J Perinatol. 2016;33:751–7.
Seaton SE, Barker L, Draper ES, Abrams KR, Modi N, Manktelow BN. Estimating neonatal length of stay for babies born very preterm. Arch Dis Child Fetal Neonatal Ed. 2019;104:F182–f186.
Seaton SE, Draper ES, Adams M, Kusuda S, Håkansson S, Helenius K, et al. Variations in neonatal length of stay of babies born extremely preterm: an international comparison between iNeo networks. J Pediatr. 2021;233:26–32.e26.
Seaton SE, Barker L, Jenkins D, Draper ES, Abrams KR, Manktelow BN. What factors predict length of stay in a neonatal unit: a systematic review. BMJ Open. 2016;6:e010466.
Melnyk BM, Feinstein NF, Alpert-Gillis L, Fairbanks E, Crean HF, Sinkin RA, et al. Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics. 2006;118:e1414–1427.
Profit J, McCormick MC, Escobar GJ, Richardson DK, Zheng Z, Coleman-Phox K, et al. Neonatal intensive care unit census influences discharge of moderately preterm infants. Pediatrics. 2007;119:314–9.
COMMITTEE ON FETUS AND NEWBORN, Barfield WD, Papile L-A, Baley JF, Benitz W, Cummings J. et al. Levels of neonatal care. Pediatrics. 2012;130:587–97.
Rizzolo A, Shah PS, Bertelle V, Makary H, Ye XY, Abenhaim HA, et al. Association of timing of birth with mortality among preterm infants born in Canada. J Perinatol. 2021;41:2597–606.
Beltempo M. Rapport sur l’évaluation des besoins régionaux en néonatologie au Québec. Rapport produit pour le Ministère de la santé et des Services sociaux du Québec. Montréal, QC, Canada; 2021.
Canadian Neonatal Network. Abstarctor’s Manual v2.1.2. 2014. http://www.canadianneonatalnetwork.org/portal/CNNHome/Publications.aspx.
Shah PS, Seidlitz W, Chan P, Yeh S, Musrap N, Lee SK, et al. Internal audit of the Canadian neonatal network data collection system. Am J Perinatol. 2017;34:1241–9.
Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M, et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics. 2001;108:E35.
Beltempo M, Shah PS, Ye XY, Afifi J, Lee S, McMillan DD, et al. SNAP-II for prediction of mortality and morbidity in extremely preterm infants. J Matern Fetal Neonatal Med. 2019;32:2694–701.
Ahmed N, Devitt KS, Keshet I, Spicer J, Imrie K, Feldman L, et al. A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg. 2014;259:1041–53.
McHugh MD, Aiken LH, Sloane DM, Windsor C, Douglas C, Yates P. Effects of nurse-to-patient ratio legislation on nurse staffing and patient mortality, readmissions, and length of stay: a prospective study in a panel of hospitals. Lancet. 2021;397:1905–13.
Cho E, Park J, Choi M, Lee HS, Kim EY. Associations of nurse staffing and education with the length of stay of surgical patients. J Nurs Scholarsh. 2018;50:210–8.
Lemieux-Bourque C, Piedboeuf B, Gignac S, Taylor-Ducharme S, Julien AS, Beltempo M. Comparison of three nursing workload assessment tools in the neonatal intensive care unit and their association with outcomes of very preterm infants. Am J Perinatol. 2022;39:640–5.
Lee HC, Bennett MV, Schulman J, Gould JB. Accounting for variation in length of NICU stay for extremely low birth weight infants. J Perinatol. 2013;33:872–6.
Puthattayil ZB, Luu TM, Beltempo M, Cross S, Pillay T, Ballantyne M, et al. Risk factors for re-hospitalization following neonatal discharge of extremely preterm infants in Canada. Paediatr Child Health. 2021;26:e96–e104.
Mosquera RA, Avritscher EB, Samuels CL, Harris TS, Pedroza C, Evans P, et al. Effect of an enhanced medical home on serious illness and cost of care among high-risk children with chronic illness: a randomized clinical trial. JAMA. 2014;312:2640–8.
Shah PS, Mirea L, Ng E, Solimano A, Lee SK. Canadian Neonatal N. Association of unit size, resource utilization and occupancy with outcomes of preterm infants. J Perinatol. 2015;35:522–9.
Beltempo M, Lacroix G, Cabot M, Blais R, Piedboeuf B. Association of nursing overtime, nurse staffing and unit occupancy with medical incidents and outcomes of very preterm infants. J Perinatol. 2018;38:175–80.
Sherenian M, Profit J, Schmidt B, Suh S, Xiao R, Zupancic JA, et al. Nurse-to-patient ratios and neonatal outcomes: a brief systematic review. Neonatology. 2013;104:179–83.
Rogowski JA, Staiger D, Patrick T, Horbar J, Kenny M, Lake ET. Nurse staffing and NICU infection rates. JAMA Pediatr. 2013;167:444–50.
Blayney MC, Donaldson L, Smith P, Wallis C, Cole S, Lone NI. Intensive care unit occupancy and premature discharge rates: a cohort study assessing the reporting of quality indicators. J Crit Care. 2020;55:100–7.
Fergusson NA, Ahkioon S, Ayas N, Dhingra VK, Chittock DR, Sekhon MS, et al. Association between intensive care unit occupancy at discharge, afterhours discharges, and clinical outcomes: a historical cohort study. Can J Anaesth. 2020;67:1359–70.
Vollam S, Dutton S, Lamb S, Petrinic T, Young JD, Watkinson P. Out-of-hours discharge from intensive care, in-hospital mortality and intensive care readmission rates: a systematic review and meta-analysis. Intensive Care Med. 2018;44:1115–29.
Acknowledgements
The authors gratefully acknowledge all site investigators and abstractors of the Canadian Neonatal Network. We also thank the staff at the Maternal-Infant Care (MiCare) Research Centre at Mount Sinai Hospital, Toronto, ON for organizational support of the Canadian Neonatal Network.
Funding
MB holds an Early Career Investigator Grant from the CIHR Institute of Human Development, Child and Youth Health (IHDCYH), a Research Grant Funding from the FRSQ Clinical Research Scholar Career Award Junior 1, and an Early Career Investigator Grant from the Montreal Children’s Hospital Foundation.
Author information
Authors and Affiliations
Consortia
Contributions
MB conceptualized and designed the study, drafted the manuscript, and adjusted the manuscript according to the comments of co-authors. SP collected and analyzed the data, contributed to study design and critically reviewed the manuscript. AL, SM, VB and BP provided administrative support for data access. ES, GL, AL, STD, SM, VB and BP provided review and critical appraisal of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Beltempo, M., Sargi, E., Patel, S. et al. Neonatal intensive care unit occupancy rate and probability of discharge of very preterm infants. J Perinatol 43, 490–495 (2023). https://doi.org/10.1038/s41372-022-01596-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01596-y