Abstract
Objectives
To determine the prevalence of perinatal factors associated with brachial plexus birth injury (BPBI) in affected infants and their relationship with BPBI severity.
Study design
Retrospective study of BPBI infants prospectively enrolled in a multicenter registry. The prevalence of perinatal factors was calculated. Infants were stratified by injury severity and groups were compared to determine the association of severity and perinatal factors.
Results
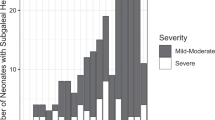
Seven-hundred-ninety-six BPBI infants had a mean 4.2 ± 1.6 perinatal factors. Nearly all (795/796) reported at least one factor, including shoulder dystocia(96%), no clavicle fracture (91%), difficult delivery(84%), parity >1(61%) and birthweight >4000 g(55%). Ten-percent (74/778) had Horner’s syndrome and 28%(222/796) underwent nerve surgery. Birth asphyxia and NICU admission were significantly associated with injury severity.
Conclusions
NICU admission and asphyxia were associated with BPBI severity. An improved understanding of the relationship between perinatal factors and BPBI severity may be used to guide early referral to BPBI providers and support prevention efforts.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article and/or its supplementary material files. Further enquiries can be directed to the corresponding author.
References
Foad SL, Mehlman CT, Ying J. The epidemiology of neonatal brachial plexus palsy in the United States. J Bone Jt Surg Am. 2008;90:1258–64. https://doi.org/10.2106/JBJS.G.00853.
DeFrancesco CJ, Shah DK, Rogers BH, Shah AS. The epidemiology of brachial plexus birth palsy in the United States: Declining incidence and evolving risk factors. J Pediatr Orthop. 2019;39:e134–40. https://doi.org/10.1097/BPO.0000000000001089.
Hoeksma AF, ter Steeg AM, Nelissen RGHH, van Ouwerkerk WJR, Lankhorst GJ, de Jong BA. Neurological recovery in obstetric brachial plexus injuries: an historical cohort study. Dev Med Child Neurol. 2004;46:76–83. https://doi.org/10.1017/s0012162204000179.
Pondaag W, Malessy MJA, van Dijk JG, Thomeer RTWM. Natural history of obstetric brachial plexus palsy: a systematic review. Dev Med Child Neurol. 2004;46:138–44. https://doi.org/10.1017/s0012162204000258.
Foad SL, Mehlman CT, Foad MB, Lippert WC. Prognosis following neonatal brachial plexus palsy: an evidence-based review. J Child Orthop. 2009;3:459–63. https://doi.org/10.1007/s11832-009-0208-3.
Annika J, Paul U, Anna-Lena L. Obstetric brachial plexus palsy—A prospective, population-based study of incidence, recovery and long-term residual impairment at 10 to 12 years of age. Eur J Paediatr Neurol EJPN J Eur Paediatr Neurol Soc. 2019;23:87–93. https://doi.org/10.1016/j.ejpn.2018.06.006.
Lagerkvist AL, Johansson U, Johansson A, Bager B, Uvebrant P. Obstetric brachial plexus palsy: a prospective, population-based study of incidence, recovery, and residual impairment at 18 months of age. Dev Med Child Neurol. 2010;52:529–34. https://doi.org/10.1111/j.1469-8749.2009.03479.x.
Hogendoorn S, van Overvest KLJ, Watt I, Duijsens AHB, Nelissen RGHH. Structural changes in muscle and glenohumeral joint deformity in neonatal brachial plexus palsy. J Bone Jt Surg Am. 2010;92:935–42. https://doi.org/10.2106/JBJS.I.00193.
McDaid PJ, Kozin SH, Thoder JJ, Porter ST. Upper extremity limb-length discrepancy in brachial plexus palsy. J Pediatr Orthop. 2002;22:364–6.
Strömbeck C, Fernell E. Aspects of activities and participation in daily life related to body structure and function in adolescents with obstetrical brachial plexus palsy: a descriptive follow-up study. Acta Paediatr Oslo Nor 1992 2003;92:740–6. https://doi.org/10.1080/08035250310002416.
van der Holst M, Groot J, Steenbeek D, Pondaag W, Nelissen RG, Vliet Vlieland TP. Participation restrictions among adolescents and adults with neonatal brachial plexus palsy: the patient perspective. Disabil Rehabil. 2018;40:3147–55. https://doi.org/10.1080/09638288.2017.1380717.
Manske MC, Abaraca NE, Letzelter JP, James MA. Patient Reported Outcomes Measurement Information System (PROMIS) Scores for children with brachial plexus birth injury. J Pediatr Orthop. 2021;41:171–6.
Akel BS, Öksüz Ç, Oskay D, Fırat T, Tarakcı E, Leblebicioğlu G. Health-related quality of life in children with obstetrical brachial plexus palsy. Qual Life Res Int J Qual Life Asp Treat Care Rehabil. 2013;22:2617–24. https://doi.org/10.1007/s11136-013-0369-x.
Partridge C, Edwards S. Obstetric brachial plexus palsy: increasing disability and exacerbation of symptoms with age. Physiother Res Int J Res Clin Phys Ther. 2004;9:157–63. https://doi.org/10.1002/pri.319.
Pondaag W, Malessy MJA. Evidence that nerve surgery improves functional outcome for obstetric brachial plexus injury. J Hand Surg Eur Vol. 2021;46:229–36. https://doi.org/10.1177/1753193420934676.
Nayak A, D’Souza A, Bhat AK, Rao A, Acharya AM. Role of early referral and surgical intervention in brachial plexus birth palsy: awareness among obstetricians and pediatricians in a teaching hospital. Int Q Community Health Educ. 2020;40:363–6. https://doi.org/10.1177/0272684X19883523.
Patra S, Narayana Kurup JK, Acharya AM, Bhat AK. Birth brachial plexus palsy: a race against time. BMJ Case Rep. 2016;2016:bcr2016215996 https://doi.org/10.1136/bcr-2016-215996.
Azzi AJ, Aubin-Lemay C, Kvann JC, Retrouvey H, Aldekhayel S, Zadeh T. Prompt referral in the nonoperative treatment of obstetrical brachial plexus injuries. Plast Reconstr Surg Glob Open. 2017;5:e1587 https://doi.org/10.1097/GOX.0000000000001587.
Executive summary: Neonatal brachial plexus palsy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Neonatal Brachial Plexus Palsy. Obstet Gynecol. 2014;123:902–4. https://doi.org/10.1097/01.AOG.0000445582.43112.9a.
Guidelines for Referral to Pediatric Surgical Specialists. HealthyChildren.org. Accessed January 14, 2022. https://www.healthychildren.org/English/family-life/health-management/pediatric-specialists/Pages/Guidelines-for-Referral-to-Pediatric-Surgical-Specialists.aspx.
Coroneos CJ, Voineskos SH, Christakis MK, Thoma A, Bain JR, Brouwers MC. Obstetrical brachial plexus injury (OBPI): Canada’s national clinical practice guideline. BMJ Open. 2017;7:e014141 https://doi.org/10.1136/bmjopen-2016-014141.
Gilbert WM, Nesbitt TS, Danielsen B. Associated factors in 1611 cases of brachial plexus injury. Obstet Gynecol. 1999;93:536–40. https://doi.org/10.1016/s0029-7844(98)00484-0.
Lalka A, Gralla J, Sibbel SE, Brachial plexus birth injury: epidemiology and birth weight impact on risk factors. J Pediatr Orthop. Published online August, 2019. https://doi.org/10.1097/BPO.0000000000001447.
Abzug JM, Mehlman CT, Ying J. Assessment of current epidemiology and risk factors surrounding brachial plexus birth palsy. J Hand Surg. 2019;44:515.e1–e10. https://doi.org/10.1016/j.jhsa.2018.07.020.
Freeman MD, Goodyear SM, Leith WM. A multistate population-based analysis of linked maternal and neonatal discharge records to identify risk factors for neonatal brachial plexus injury. Int J Gynaecol Obstet Organ Int Fed Gynaecol Obstet 2017;136:331–6. https://doi.org/10.1002/ijgo.12059.
Bauer AS, Kalish LA, Adamczyk MJ, Bae DS, Cornwall R, James MA, et al. Microsurgery for brachial plexus injury before versus after 6 months of age: results of the multicenter treatment and outcomes of Brachial Plexus Injury (TOBI) Study. J Bone Joint Surg Am. Published online November, 2019. https://doi.org/10.2106/JBJS.18.01312.
Chauhan SP, Rose CH, Gherman RB, Magann EF, Holland MW, Morrison JC. Brachial plexus injury: a 23-year experience from a tertiary center. Am J Obstet Gynecol. 2005;192:1795–1800. https://doi.org/10.1016/j.ajog.2004.12.060.
Fogel I, Katz A, Sela HY, Lebel E. Brachial plexus birth palsy: incidence, natural-course, and prognostic factors during the first year of life. J Perinatol J Calif Perinat Assoc. 2021;41:1590–4. https://doi.org/10.1038/s41372-021-00972-4.
Chauhan SP, Blackwell SB, Ananth CV. Neonatal brachial plexus palsy: incidence, prevalence, and temporal trends. Semin Perinatol. 2014;38:210–8. https://doi.org/10.1053/j.semperi.2014.04.007.
Christoffersson M, Rydhstroem H. Shoulder dystocia and brachial plexus injury: a population-based study. Gynecol Obstet Invest. 2002;53:42–47. https://doi.org/10.1159/000049410.
Mollberg M, Hagberg H, Bager B, Lilja H, Ladfors L. High birthweight and shoulder dystocia: the strongest risk factors for obstetrical brachial plexus palsy in a Swedish population-based study. Acta Obstet Gynecol Scand. 2005;84:654–9. https://doi.org/10.1111/j.0001-6349.2005.00632.x.
Coroneos CJ, Voineskos SH, Coroneos MK, Alolabi N, Goekjian SR, Willoghby LI, et al. Obstetrical brachial plexus injury: burden in a publicly funded, universal healthcare system. J Neurosurg Pediatr. 2016;17:222–9. https://doi.org/10.3171/2015.6.PEDS14703.
Malessy MJA, Pondaag W, Yang LJS, Hofstede-Buitenhuis SM, le Cessie S, van Dijk JG. Severe obstetric brachial plexus palsies can be identified at one month of age. PloS One. 2011;6:e26193 https://doi.org/10.1371/journal.pone.0026193.
Gherman RB, Ouzounian JG, Satin AJ, Goodwin TM, Phelan JP. A comparison of shoulder dystocia-associated transient and permanent brachial plexus palsies. Obstet Gynecol. 2003;102:544–8. https://doi.org/10.1016/s0029-7844(03)00660-4.
Zuarez-Easton S, Zafran N, Garmi G, Hasanein J, Edelstein S, Salim R. Risk factors for persistent disability in children with obstetric brachial plexus palsy. J Perinatol J Calif Perinat Assoc. 2017;37:168–71. https://doi.org/10.1038/jp.2016.195.
Wilson TJ, Chang KWC, Chauhan SP, Yang LJS. Peripartum and neonatal factors associated with the persistence of neonatal brachial plexus palsy at 1 year: a review of 382 cases. J Neurosurg Pediatr. 2016;17:618–24. https://doi.org/10.3171/2015.10.PEDS15543.
Pondaag W, Allen RH, Malessy MJA. Correlating birthweight with neurological severity of obstetric brachial plexus lesions. BJOG Int J Obstet Gynaecol. 2011;118:1098–103. https://doi.org/10.1111/j.1471-0528.2011.02942.x.
Shah AS, Kalish LA, Bae DS, Peljovich AE, Cornwall R, Bauer AS, et al. Early predictors of microsurgical reconstruction in brachial plexus birth palsy. Iowa Orthop J. 2019;39:37–43.
Bellew M, Kay SP. Early parental experiences of obstetric brachial plexus palsy. J Hand Surg Edinb Scotl 2003;28:339–46. https://doi.org/10.1016/s0266-7681(03)00081-0.
Clarke HM, Curtis CG. An approach to obstetrical brachial plexus injuries. Hand Clin. 1995;11:563–80.
Waters PM. Comparison of the natural history, the outcome of microsurgical repair, and the outcome of operative reconstruction in brachial plexus birth palsy. J Bone Jt Surg Am. 1999;81:649–59. https://doi.org/10.2106/00004623-199905000-00006.
Borschel GH, Clarke HM. Obstetrical brachial plexus palsy. Plast Reconstr Surg. 2009;124:144e–155e. https://doi.org/10.1097/PRS.0b013e3181a80798.
Squitieri L, Larson BP, Chang KWC, Yang LJS, Chung KC. Medical decision-making among adolescents with neonatal brachial plexus palsy and their families: a qualitative study. Plast Reconstr Surg. 2013;131:880e–7e. https://doi.org/10.1097/PRS.0b013e31828bd52b.
Bellew M, Kay SP, Webb F, Ward A. Developmental and behavioural outcome in obstetric brachial plexus palsy. J Hand Surg Edinb Scotl 2000;25:49–51. https://doi.org/10.1054/jhsb.1999.0331.
Funding
This work was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1 TR001860 and linked award KL2 TR001859. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
MCM: responsible for study conception and design, assisted in data interpretation; prepared original manuscript and subsequent revisions; has approved final manuscript and agrees to be responsible for all aspects of this work. PEM: performed the statistical analyses and interpretation; performed critical analysis of the manuscript for intellectual content; has approved final manuscript and agrees to be responsible for all aspects of this work. ASB: responsible for study conception, assisted in data interpretation, performed critical analysis of the manuscript for intellectual content; has approved final manuscript and agrees to be responsible for all aspects of this work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
This research was conducted in accordance with the World Medical Association Declaration of Helsinki.
Consent to participate
Written informed consent was obtained from a parent/legal guardian for subjects to participate in the TOBI (Treatment and Outcomes of Brachial plexus Injury) registry. As part of the consent form, patients/parents were informed that the data collected would be used to provide valuable information about long-term outcomes of BPBI in order to inform better treatment options for patients in the future. For this reason the Institutional Review Board at Boston Children’s Hospital determined that the present study using data from the TOBI registry met the regulatory requirements necessary in order to obtain a waiver of informed consent/authorization.
Study approval statement
This study protocol was reviewed and approved by the Institutional Review Board at Boston Children’s Hospital, protocol number IRB-P00034806.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Manske, M.C., Miller, P.E. & Bauer, A.S. Prevalence of perinatal factors in infants with brachial plexus birth injuries and their association with injury severity. J Perinatol 43, 578–583 (2023). https://doi.org/10.1038/s41372-022-01594-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01594-0