Abstract
Objective
Assess presence, durability, and neutralization capacity of SARS-CoV-2-specific antibodies in breastfeeding infants’ stool, mother’s plasma and milk following maternal vaccination.
Design
Thirty-seven mothers and 25 infants were enrolled between December 2020 and November 2021 for this prospective observational study. All mothers were vaccinated during lactation except three, which were vaccinated during pregnancy. Milk, maternal plasma, and infants’ stool was collected pre-vaccination and at periods up to 6 months following COVID-19 vaccine series initiation/completion. SARS-CoV-2 antibody levels and their neutralization capacities were assessed.
Results
SARS-CoV-2-specific IgA and IgG levels were higher in infant stool post-maternal vaccination amongst milk-fed compared to controls. Maternal SARS-CoV-2-specific IgA and IgG concentrations decreased over 6 months post-vaccination but remained higher than pre-vaccination levels. We observed improved neutralization capacity in milk and plasma after COVID-19 vaccination.
Conclusions
The presence of SARS-CoV-2-specific antibodies in infant stool following maternal vaccination offers further evidence of the lasting transfer of these antibodies through breastfeeding.
Similar content being viewed by others
Introduction
The grievous consequences of COVID-19 infection are widely known. With the upsurge of new variants [1], we have witnessed how COVID-19 has affected the US (United States) population, including pregnant women [2] and children [3].
Vaccination during pregnancy is known to generate functional anti-spike IgG antibodies in maternal circulation that are detectable in umbilical cord blood at birth and can protect the infant from COVID-19 [4,5,6,7]. Further, recent studies have demonstrated that COVID-19 infection, as well as vaccination against COVID-19, induces secretion of neutralizing SARS-CoV-2 IgA and IgG in human milk (HM) [8,9,10,11,12,13,14,15,16]. However, little is known about the transfer of neutralizing HM antibodies to breastfeeding infants.
HM has antimicrobial properties, evidenced by the decreased rate of infections and hospitalization among breastfeeding infants [17]. This can be attributed to molecules with immuno-protective functions within HM: immunoglobulins, lactoferrin, oligosaccharides, and cytokines, to name a few [18]. HM antibodies, in particular, sIgA, prevent the entry of microorganisms into the tissue by decreasing surface colonization and dampening penetration of potentially harmful organisms [19].
SARS-CoV-2 relies on its main receptor, angiotensin-converting enzyme 2 (ACE2), to enter cells, which is abundantly present in the human epithelia of the lung, small intestine, and colon [20, 21]. Reports have shown that a notable proportion of patients with COVID-19 develop gastrointestinal symptoms and nearly half of patients have detectable SARS-CoV-2 RNA in their fecal samples [22, 23].
To protect against SARS-CoV-2 infection, the immune system must mount a robust and specific response. In addition to SARS-CoV-2-specific antibody concentration, antibody specificity, affinity, and neutralizing capacity are also necessary to elicit a proper immune response. As such, we hypothesize that there is a transfer of neutralizing HM SARS-CoV-2 specific IgA and IgG to the intestinal tract of breast-fed infants that can protect them from COVID-19 infection. Together our results provide interesting insight into the relationship between the durability of maternal antibodies subsequent to vaccination, and the potential protection of breastfed infants.
Methods
Study design
This prospective observational study was conducted at the University of Florida under institutional review board approval (#IRB202003255). Thirty-seven breastfeeding mothers were recruited before or after COVID-19 vaccination with Pfizer/BioNTech, Moderna, or Johnson & Johnson from December 2020 to November 2021. All mothers were vaccinated during lactation except three, who were vaccinated during pregnancy. In June 2021, we added breastfeeding infant enrollment for stool collection. A total of 25 infants were enrolled from June to November 2021. Mothers contributed data at various time points up to 6 months after completing the series (8 mothers provided longitudinal HM and 7 provided plasma samples at pre-vaccination, post-1st dose, 7–30 days, and 6 months post-vaccination). Inclusion criteria included breastfeeding women 18 years and older, pre-or-post-COVID-19 vaccination, and providing informed consent.
Participants and procedures
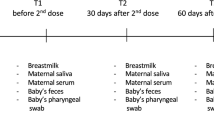
Recruitment methods included the University of Florida’s institutional e-mail listserv and advertising flyers posted in University of Florida facilities and the surrounding community. Up to 37 mothers and 25 infants were recruited at different time points; of those, 3 mother’s and 1 infant samples were not included in the analysis (1 mother stopped breastfeeding prior to first vaccination; and two participants received the J&J vaccine). Given significant differences in effectiveness and antibody response with J&J compared to mRNA vaccines, those two mother-infant dyads were excluded from the analysis. 96 maternal serum, 101 maternal milk, and 31 infant stool samples were collected up to 6-time points relative to COVID-19 vaccination completion: pre-vaccination, 15–30 days after the first vaccine dose (for participants receiving two-dose mRNA vaccines), and then at 7–30 days, 60–75 days, 90–105 days, and 6 months following 2-dose vaccination series completion. Not all participants contributed samples at every listed collection time point (Supplementary Table 1).
Participants completed a questionnaire collecting maternal/infant demographics, medical and family history, and vaccination side effects upon agreeing to participate.
Sample collection and processing
Maternal blood samples were collected via venipuncture or finger prick in ethylenediaminetetraacetic acid-coated (EDTA) tubes at the designated time points. Plasma was separated from cellular matter by centrifugation at 2000 × g for 10 min at 4 °C and then stored undiluted at −20 °C.
For milk, mothers were instructed to express samples of 10–30 ml. Samples were stored at −20 °C within 4 h after collection. The samples were aliquoted into 2 mL tubes, then centrifuged at 500 g for 15 min at 4 °C. Using a 21 G needle, the aqueous layer was separated from the fat layer and placed in a clean tube. This aqueous layer was then centrifuged at 3000 × g for 15 min at 4 °C. The final aqueous layer was removed and stored undiluted at −20 °C.
Stool samples were collected in diapers and dropped off either the same day or kept refrigerated overnight by participants before their collection appointments, then stored at −80 °C until further processing. Stool samples were then diluted with 2 mL DPBS, vortexed vigorously to achieve a homogenized sample, and centrifuged at 1500 × g for 20 min. The supernatant was then placed in a clean tube, vortexed, and centrifuged at 10,000 × g for 10 min. Supernatant was removed and stored undiluted at −20 °C.
SARS-CoV-2-specific IgA and IgG concentrations were measured in HM, plasma, and infant stool using previously-validated COVID-19 Human IgA and IgG ELISA kits (RayBiotech Life, Peachtree Corners, Georgia, USA) [10]. SARS-CoV-2-specific IgA samples were run at 1:500 dilution in plasma. SARS-CoV-2-specific IgG samples were run at 1:1000 dilution in plasma. SARS-CoV-2-specific IgA samples were run at 1:3 dilution in HM. SARS-CoV-2-specific IgG samples were run undiluted (1:1) in HM. SARS-CoV-2-specific IgA and IgG samples were run undiluted (1:1) in infant stool. We used 10 pre-COVID-era and 1 maternal pre-vaccination infants stool samples as negative controls. All samples were ran in duplicate.
To determine the neutralization capability of SARS-CoV-2 antibodies, we used an assay containing vesicular stomatitis virus (VSV) expressing the SARS-CoV-2 Wuhan-hu-1 wild type strain spike protein and green fluorescent protein (GFP) (VSV-gfp-SARS-CoV-2-S-gp) described in a previously published study [24]. Milk, plasma, or stool samples were mixed with VSV and later incubated with baby hamster kidney (BHK) cells expressing human ACE2 receptors. GFP frequency was measured by flow cytometry to quantify BHK-ACE2 cell infectivity. The raw GFP+ values of each sample were normalized to a scale of 0–100% infectivity using negative and positive controls (Supplementary Fig. 2). The normalized values were then used to make non-linear regression curves of infectivity, providing IC50 values for each sample. All samples were ran in duplicate.
Statistical analysis
The demographics and clinical features of the study sample were characterized via descriptive statistics. Medians with 25th and 75th percentiles (IQR1 and IQR3) were provided for log-transformed [10] SARS-CoV-2 specific milk, plasma, and stool IgA and IgG levels at all time points (Supplementary Table 1).
Mann–Whitney U-tests (unpaired, nonparametric, two-tailed) were used to compare antibody concentrations in infant stool after mother’s COVID-19 vaccination vs. pre-COVID era infant stool samples across available time points; and IC50 in milk and plasma pre-vaccination vs. 7–30 days post-2nd dose and six months post-vaccination series completion. Spearman correlation (two-tailed) was carried out to explore the relationship between log-transformed [10] SARS-CoV-2 specific IgA and IgG in milk, plasma, and infant stool at 6 months; and IgA and IgG in milk, plasma with IC50 in milk and plasma at three-time points (pre-vaccination, 7–30 days post-2nd dose, and six months post-vaccination series completion). Statistical test results were reported as p-values. Statistical analyses were performed using SPSS statistics software and GraphPad Prism 9 (GraphPad Software, La Jolla, CA, USA). All figures were created using GraphPad Prism 9. Center values of each figure were shown as geometric mean with geometric mean SD.
Results
Thirty-seven lactating women and 25 infants were enrolled in the study. Of those, 34 women and 24 infants were included in the statistical analysis (please refer to methods section); 8 women completed longitudinal samples for HM and 7 for plasma at pre-vaccination, post-1st dose, 15–30 days post-second dose, and 6 months after 2-dose vaccination series completion (Supplementary Fig. 1). Pre-vaccination samples consisted of 25 HM and 16 plasma samples; 6-month samples included 16 HM and 19 plasma samples. Thirty-one infant’s stools samples were collected up to 6 months post-vaccination. The study population consisted primarily of White non-Hispanic women in their mid-30s and their infants with a median infant age of 10 months at enrollment (Table 1).
SARS-CoV-2 IgA and IgG are present in the stool of breastfeeding infants after maternal COVID-19 vaccination and stool contents can neutralize the pseudovirus in vitro
We detected SARS-CoV-2 IgA and IgG in the stool of breastfeeding infants whose mothers received COVID-19 vaccination, with a statistically significant increase in IgG relative to negative controls (p = 0.08 and <0.0001 in IgA and IgG, respectively) (Fig. 1). Infant stool IgG concentrations were positively correlated with maternal plasma and HM IgG concentrations at six months post vaccination (p = 0.0475, R = 0.59 and p = 0.0092, R = 0.73, respectively) (Supplementary Table 2).
IC50: the lower the IC50, the stronger the neutralization capability. Concentration (unit/mL) listed in log10 form. Both antibody concentration comparison and IC50 statistical calculations are measured using Mann–Whitney unpaired, nonparametric test; the figure is shown as geometric mean and geometric SD.
Although breastfeeding infant’s stool, obtained both prior and subsequent to maternal vaccination could neutralize pseudovirus activity in vitro; the ability to neutralize pseudovirus activity was enhanced after maternal vaccination. Neutralization capacity is measured by the half-maximal inhibitory concentration (IC50): hence the lower the IC50, the stronger the neutralization capability. The geometric mean IC50 for infant stool samples after mother’s vaccination was 0.94 compared to a geometric mean IC50 of 1.90 in pre-COVID negative control samples (p = 0.4) (Fig. 1).
SARS-CoV-2 IgA concentrations in human milk and plasma appear to decline over time but remain higher than pre-vaccination 6 months after
SARS-CoV-2-specific IgA concentrations in milk and plasma declined 6 months after vaccination, but levels remain higher than the pre-vaccination value (Fig. 2). For milk, the median for log-transformed [10] SARS-CoV-2-IgA concentration was 1.3 unit/ml pre-vaccination versus 1.6 unit/ml six months post-vaccination. In plasma, the median for log-transformed [10] SARS-CoV-2-IgA concentrations was 3.3 unit/ml pre-vaccination, compared to 3.5 units/ml six months post-vaccination (Supplementary Table 1). Furthermore, the positivity rate decreased to 53% in milk and 77% in plasma at 6 months, from 88 and 87%, respectively, at 7–30 days post-vaccination (Supplementary Table 1).
SARS-CoV-2 IgG concentration appears to decline in plasma and to a lesser degree in human milk 6 months after COVID-19 vaccination
Although SARS-CoV-2 IgG decreased in HM 6 months after vaccination, values remained higher than pre-vaccination levels (Fig. 3). Median log-transformed [10] SARS-CoV-2-IgG concentrations in HM pre-vaccination were 0.08 units/ml, versus 0.6 units/ml six months post-vaccination (Supplementary Table 1). In plasma, we observed a steep decline in SARS-CoV-2 IgG six months after vaccination compared to immediately post second dose; however, the positivity rate remained 100% above the positive cutoff in milk and in plasma after 6 months (Supplementary Table 1).
For both milk and plasma, we noticed an overall decline in SARS-CoV-2 antibody levels at six months compared to 7–30 days post-vaccination. IgG concentration in HM and plasma appears to have a more dynamic predominant response to vaccination in comparison to IgA.
Human milk neutralizing activity
Human milk obtained from pre- and post-COVID-19 vaccinated individuals neutralized the viral binding of the pseudovirus VSV-gfp-SARS-CoV-2-S-gp to the BHK21-ACE2 cell line in vitro. The geometric mean IC50 (indicative of viral adherence to cells) for HM pre-vaccination was 0.14, compared to 0.03 six months post-vaccination (Fig. 4). The increase in HM neutralization capability after vaccination was statistically significant with a p-value of 0.05. There was heterogeneity in response, where roughly half of the participants had increased neutralization at six months compared to immediately post 2nd dose, and the other half had decreased neutralization at six months compared to post 2nd dose (Supplementary Fig. 3). This work supports current, published data that shows milk can neutralize SARS-CoV-2 in vitro after COVID-19 mRNA vaccination [8, 25] and highlight a novel finding: HM neutralizing capability to SARS-CoV-2 increased over the 6-month time span, even as SARS-CoV-2 specific antibody concentrations decreased.
In milk and plasma, neutralization is compared pre-vaccination, 7–10 days post 2nd dose, and six months post vaccination using the half-proximal inhibitory concentration (IC50). IC50 statistical calculations are measured using Mann–Whitney unpaired, nonparametric tests. Figures are shown as geometric mean. Line graphs represent non-linear regression models of inhibition at pre-vaccination (dotted, black line), 7–10 days post 2nd dose (solid, blue line), and six months post vaccination (solid, orange line).
Plasma neutralizing activity
We detected a statistically significant increase in plasma neutralization capability after COVID-19 vaccination (p < 0.0001) (Fig. 4). Before vaccination, the geometric mean IC50 in plasma was 0.5. The highest neutralization occurred 7–30 days after the second vaccine dose (IC50 = 0.001) and diminished six months after vaccination (IC50 = 0.036) while remaining above pre-vaccination levels. Neutralization capacity increased by 99% in plasma immediately post COVID-19 vaccination completion and remained statistically, significantly higher than pre-vaccination levels six months after vaccination (p = 0.002). The decline in neutralization is also observed in other studies that show neutralization in blood peaks roughly two weeks following the second dose but falls in vaccinated participants over time [26, 27].
Plasma neutralization (IC50) was statistically significantly correlated to plasma IgA concentrations 7–30 days post 2nd dose (R = −0.79, p = 0.009) (Supplementary Table 3). This means the higher the plasma SARS-CoV-2 IgA concentration, the higher the plasma neutralization.
Discussion
Infants are born with an immature immune system, and it has been well-established that breastfeeding protects them against respiratory infections [17,18,19]. Prior studies have shown a significant increase in neutralizing SARS-CoV-2 specific antibodies in HM after COVID-19 vaccination or infection, suggesting a possible transfer of these antibodies to breastfeeding infants [10, 11, 14,15,16, 28]. Our study is among the first to demonstrate the presence of SARS-CoV-2 antibodies in breastfeeding infants’ stools with improvement in infant’s stool SARS-CoV-2 specific neutralization capabilities following maternal SARS-CoV-2 vaccination. Despite not being statistically significant, in part due to a small sample size, our results further support the maternal/infant passive transfer of SARS-CoV-2 antibodies through HM.
SARS-CoV-2, like other coronaviruses, invades intestinal cells as they express high levels of ACE2, their receptor, causing inflammation, malabsorption, intestinal dysfunction, and diarrhea [21, 22]. The high sensitivity of epithelial cells to coronaviruses increases their replicative capacity. Furthermore, the pediatric population can shed SARS-CoV-2 RNA for up to several weeks in the stool after confirmed respiratory clearance [29]. Although additional confirmatory studies will be necessary, our results make it tempting to speculate that SARS-CoV-2 specific IgA and IgG, present in the human milk of vaccinated individuals, potentially block viral-ACE-2 receptors’ interactions within the infant’s intestinal mucosa.
It should be noted that HM was able to neutralize the pseudovirus in vitro even before vaccination. It has been established that antibodies can possess cross-reactivity to different human coronaviruses [30, 31]. Additionally, the extensive array of immune-protective molecules within HM (immunoglobulins, IgA secretory component, lactoferrin, oligosaccharides, blood-derived leukocytes) are also likely to contribute [17, 32, 33]. Once vaccination is administered to breastfeeding mothers, we observed an increase in HM neutralization capability in 50% of the samples at 6 months post-vaccination, despite a decrease in antibody levels; this could result from the specialization and affinity maturation of secreted antibodies in HM, as seen for SARS-CoV-2 IgG in plasma in a prior study [34].
These results lead us to hypothesize that secreted HM SARS-CoV-2 IgA and IgG may serve to neutralize the virus and offer immunologic protection to breastfeeding infants, potentially preventing SARS-CoV-2-ACE-2 interaction and reducing the severity of infection-related symptoms. However, up to date, no clinical correlation has been established between HM antibodies concentration and breastfeeding infants’ protection. Establishing a correlation between antibody levels/antibody neutralization and clinical efficacy is confounded by a number of factors including viral mutation rates, cellular (T cell-mediated) immunity, genetic factors, age, and the environment. A recent article, published by the laboratories of Drs. Triccas and Davenport in 2021 developed a modeling system to predict a correlation between in vitro neutralization levels and observed protection from SARS-CoV-2 infection [35]. In this paper, using modeling strategies, it was estimated that 20 and 3 percent of the mean convalescent SARS CoV-2 specific antibody levels were capable of providing 50% protection from detectable infection and severe infection respectively. It would be exciting to utilize such modeling strategies to establish correlates between in vitro neuralization assays using infant stool and clinical outcomes. Additionally, the true functionality of stool derived SARS-CoV-2 specific antibodies remains to be determined. Further studies, utilizing larger, more diverse, populations will bring clarity to these important clinical considerations.
Limitations
This study is among the first to suggest an effective transfer of HM SARS-CoV-2 IgA and IgG to breastfeeding infants’ gastrointestinal tract. There are limitations to some of the results. First, there was a small sample size and limited diversity in this cohort of mothers. Although participants contributed data at various time points, no subjects contributed on all occasions. Furthermore, whether infants or mothers might have had a previously undiagnosed COVID infection, and how this may have interfered with results, cannot be known. We did not test IgA secretory component, rather we assumed that IgA found in milk is majority secretory IgA. The mean age of our infant subjects was 10 months, with many of them having solid food their main source of nutrition and breastfeeding as supplementation; this in combination with small sample size might have interfered with the stool antibodies concentration and neutralization capacity results, since exclusively breastfeeding infants may have higher antibodies levels.
Data availability
The datasets generated during this study are available from the corresponding author upon reasonable request.
References
Tracking SARS-CoV-2 variants. 2021. https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/.
Chinn J, Sedighim S, Kirby KA, Hohmann S, Hameed AB, Jolley J, et al. Characteristics and outcomes of women with COVID-19 giving birth at US Academic Centers during the COVID-19 pandemic. JAMA Netw Open. 2021;4:e2120456–e2120456. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2782978.
Children and COVID-19: state-level data report. 2021. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/.
Beharier O, Mayo RP, Raz T, Sacks KN, Schreiber L, Suissa-Cohen Y, et al. Efficient maternal to neonatal transfer of antibodies against SARS-CoV-2 and BNT162b2 mRNA COVID-19 vaccine. J Clin Invest. 2021;131:e150319.
Shook LL, Atyeo CG, Yonker LM, Fasano A, Gray KJ, Alter G, et al. Durability of anti-spike antibodies in infants after maternal COVID-19 vaccination or natural infection. JAMA. 2022. https://jamanetwork.com/journals/jama/fullarticle/2788986.
Halasa NB, Olson SM, Staat MA, Newhams MM, Price AM, Boom JA, et al. Effectiveness of maternal vaccination with mRNA COVID-19 vaccine during pregnancy against COVID-19-associated hospitalization in infants aged. MMWR Morb Mortal Wkly Rep. 2022;71:264–70. https://pubmed.ncbi.nlm.nih.gov/35176002/.
Nir O, Schwartz A, Toussia-Cohen S, Leibovitch L, Strauss T, Asraf K, et al. Maternal-neonatal transfer of SARS-CoV-2 immunoglobulin G antibodies among parturient women treated with BNT162b2 messenger RNA vaccine during pregnancy. Am J Obstet Gynecol. 2022;4. https://pubmed.ncbi.nlm.nih.gov/34547533/.
Narayanaswamy V, Pentecost BT, Schoen CN, Alfandari D, Schneider SS, Baker R, et al. Neutralizing antibodies and cytokines in breast milk after coronavirus disease 2019 (COVID-19) mRNA vaccination. Obstet Gynecol. 2022;139:181–91. https://journals.lww.com/greenjournal/Fulltext/2022/02000/Neutralizing_Antibodies_and_Cytokines_in_Breast.6.aspx.
Gray KJ, Bordt EA, Atyeo C, Deriso E, Akinwunmi B, Young N, et al. Coronavirus disease 2019 vaccine response in pregnant and lactating women: a cohort study. Am J Obstet Gynecol. 2021;225:303.e1–303.e17. http://www.ajog.org/article/S0002937821001873/fulltext.
Valcarce V, Stafford LS, Neu J, Cacho N, Parker L, Mueller M, et al. Detection of SARS-CoV-2-specific IgA in the human milk of COVID-19 vaccinated lactating health care workers. 2021. https://www.liebertpub.com/doi/abs/10.1089/bfm.2021.0122.
Perl SH, Uzan-Yulzari A, Klainer H, Asiskovich L, Youngster M, Rinott E, et al. SARS-CoV-2-specific antibodies in breast milk after COVID-19 vaccination of breastfeeding women. JAMA. 2021. http://www.ncbi.nlm.nih.gov/pubmed/33843975.
Ramírez DSR, Pérez MML, Pérez MC, Hernández MIS, Pulido SM, Villacampa LP, et al. SARS-CoV-2 antibodies in breast milk after vaccination. Pediatrics. 2021;e2021052286. https://pediatrics.aappublications.org/content/early/2021/10/07/peds.2021-052286.
Pace RM, Williams JE, Järvinen KM, Belfort MB, Pace CDW, Lackey KA, et al. Characterization of sars-cov-2 rna, antibodies, and neutralizing capacity in milk produced by women with covid-19. MBio. 2021;12:1–11. https://mbio.asm.org/content/12/1/e03192-20.
Fox A, Marino J, Amanat F, Krammer F, Hahn-Holbrook J, Zolla-Pazner S, et al. Robust and specific secretory IgA against SARS-CoV-2 detected in human milk. iScience. 2020;23. https://pubmed.ncbi.nlm.nih.gov/33134887/.
Peng S, Zhu H, Yang L, Cao L, Huang X, Dynes M, et al. A study of breastfeeding practices, SARS-CoV-2 and its antibodies in the breast milk of mothers confirmed with COVID-19. Lancet Reg Heal West Pac. 2020;4:100045 https://doi.org/10.1016/j.lanwpc.2020.10.
Baird JK, Jensen SM, Urba WJ, Fox BA, Baird JR. SARS-CoV-2 antibodies detected in mother’s milk post-vaccination. J Hum Lact. 2021;37:492–8.
Atyeo C, Alter G. The multifaceted roles of breast milk antibodies. Cell. 2021;184:1486–99. https://pubmed.ncbi.nlm.nih.gov/33740451/.
Hassiotou F, Geddes DT, Hartmann PE. Cells in human milk: state of the science. J Hum Lact. 2013;29:171–82. https://pubmed.ncbi.nlm.nih.gov/23515088/.
Hassiotou F, Geddes DT. Immune cell-mediated protection of the mammary gland and the infant during breastfeeding. Adv Nutr. 2015;6:267–75. https://pubmed.ncbi.nlm.nih.gov/25979492/.
Hamming I, Timens W, Bulthuis M, Lely A, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631.
Jackson CB, Farzan M, Chen B, Choe H. Mechanisms of SARS-CoV-2 entry into cells. Nat Rev Mol Cell Biol. 2022;23:3.
Guo M, Tao W, Flavell RA, Zhu S. Potential intestinal infection and faecal–oral transmission of SARS-CoV-2. Nat Rev Gastroenterol Hepatol. 2021;18:1.
Wang Q, Li Y, Lung DC, Chan PT, Dung CH, Jia W, et al. Aerosol transmission of SARS-CoV-2 due to the chimney effect in two high-rise housing drainage stacks. J Hazard Mater. 2022;421:126799.
Woodford J, Sagara I, Dicko A, Zeguime A, Doucoure M, Kwan J, et al. Severe acute respiratory syndrome coronavirus 2 seroassay performance and optimization in a population with high background reactivity in Mali. J Infect Dis. 2021;224:2001–9. https://academic.oup.com/jid/article/224/12/2001/6382154.
Young BE, Seppo AE, Diaz N, Rosen-Carole C, Nowak-Wegrzyn A, Cruz Vasquez JM, et al. Association of human milk antibody induction, persistence, and neutralizing capacity with SARS-CoV-2 infection vs mRNA vaccination. JAMA Pediatr. 2022;176:159–68. https://jamanetwork.com/journals/jamapediatrics/fullarticle/2786219.
Evans JP, Zeng C, Carlin C, Lozanski G, Saif LJ, Oltz EM, et al. Neutralizing antibody responses elicited by SARS-CoV-2 mRNA vaccination wane over time and are boosted by breakthrough infection. Sci Transl Med. 2022. https://pubmed.ncbi.nlm.nih.gov/35166573/.
Gillot C, Favresse J, Maloteau V, Dogné JM, Douxfils J. Dynamics of neutralizing antibody responses following natural SARS-CoV-2 infection and correlation with commercial serologic tests. A reappraisal and indirect comparison with vaccinated subjects. Viruses. 2021;13. https://pubmed.ncbi.nlm.nih.gov/34835135/.
Gray KJ, Bordt EA, Atyeo C, Deriso E, Akinwunmi B, Young N, et al. COVID-19 vaccine response in pregnant and lactating women: a cohort study. Am J Obstet Gynecol. 2021;0. https://linkinghub.elsevier.com/retrieve/pii/S0002937821001873.
Hua CZ, Miao ZP, Zheng JS, Huang Q, Sun QF, Lu HP, et al. Epidemiological features and viral shedding in children with SARS-CoV-2 infection. J Med Virol. 2020;92:2804–12. https://onlinelibrary.wiley.com/doi/full/10.1002/jmv.26180.
Demers-Mathieu V, DaPra C, Mathijssen GB, Medo E. Previous viral symptoms and individual mothers influenced the leveled duration of human milk antibodies cross-reactive to S1 and S2 subunits from SARS-CoV-2, HCoV-229E, and HCoV-OC43. J Perinatol. 2021;41:952.
Demers-Mathieu V, Dapra C, Mathijssen G, Sela DA, Järvinen KM, Seppo A, et al. Human milk antibodies against S1 and S2 subunits from SARS-CoV-2, HCoV-OC43, and HCoV-229E in mothers with a confirmed COVID-19 PCR, viral SYMPTOMS, and unexposed mothers. Int J Mol Sci. 2021;22:1–13.
Perrier C, Sprenger N, Corthésy B. Glycans on secretory component participate in innate protection against mucosal pathogens*. J Biol Chem. 2006;281:14280–7. http://www.jbc.org/article/S0021925820780737/fulltext.
Mestecky J, Russell MW. Specific antibody activity, glycan heterogeneity and polyreactivity contribute to the protective activity of S-IgA at mucosal surfaces. Immunol Lett. 2009;124:57.
Moriyama S, Adachi Y, Sato T, Tonouchi K, Sun L, Fukushi S, et al. Temporal maturation of neutralizing antibodies in COVID-19 convalescent individuals improves potency and breadth to circulating SARS-CoV-2 variants. Immunity. 2021;54:1841.
Khoury DS, Cromer D, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat Med. 2021;27:1205–11.
Acknowledgements
Many thanks to the milk donors who made this work possible. We thank Dr. Adetola Louis-Jacques for the critical sample donation and Dr. Diana Taft for serving as scientific advisor. Thank you to Simi Ogundare for her technical expertise and the University of Florida Clinical Research Center for samples collection and providing care of study participants.
Funding
Children’s Miracle Network and The Gerber Foundation. Funding used for data processing methods and supplies expenses. There is no role of the funding source for writing the article or the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
LSS, MS: First author, literature search, study design, methodology, data collection, figures, data analysis, statistics, writing-original draft. VV, MD: First author, literature search, study design, project administration, data collection, data curation, writing-original draft, funding acquisition. MH, MD: Literature search, data collection, data analysis, writing original draft. JN, MD: Literature search, study design, supervision, writing-review and editing, funding acquisition. LP, PhD: Study design, writing-review and editing. MM, PhD: Formal analysis, writing-review and editing. VV: Data analysis. Taylor Gowen, MD: Data collection, writing-original draft, writing-review and editing. EC: Data collection. Ivan Kosik, PhD: Methodology, provided critical reagents, data interpretation. JWY, MD PhD: Methodology, provided critical reagents, data interpretation. MA, PhD: Provided critical reagents and equipment, assisted in data acquisition. NC, DO: Study design, writing-review and editing. NL, PhD: Data collection, data analysis. JLIII, PhD: Senior author. Literature search, study design, methodology, supervision, funding acquisition, writing-review and editing. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki and was approved by the University of Florida Institutional Review Board (#IRB202003255).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stafford, L.S., Valcarce, V., Henry, M. et al. Detection of SARS-CoV-2 IgA and IgG in human milk and breastfeeding infant stool 6 months after maternal COVID-19 vaccination. J Perinatol 43, 775–781 (2023). https://doi.org/10.1038/s41372-022-01581-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01581-5
This article is cited by
-
SARS-CoV-2 neutralizing antibody titers in maternal blood, umbilical cord blood, and breast milk
Journal of Perinatology (2024)
-
Editorial response to Cosentino and Marino RE: detection of SARS-CoV-2 IgA and IgG in human milk and breastfeeding infant stool 6 months after maternal COVID-19 vaccination
Journal of Perinatology (2023)
-
In response to Detection of SARS-CoV-2 IgA and IgG in human milk and breastfeeding infant stool 6 months after maternal COVID-19 vaccination
Journal of Perinatology (2023)