Abstract
Objective
We compared the association of methadone, buprenorphine, and short-acting opioid exposure with newborn head circumference (HC) and birth weight (BW), and evaluated gestational age (GA) as a mediator.
Study design
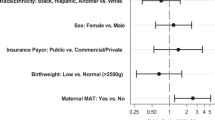
We included newborns born 2013–2018 identified by neonatal abstinence syndrome diagnosis code (N = 572) and birthday-matched unexposed controls (N = 571). Linear regressions of opioid exposure with HC and BW controlled for tobacco, marijuana, cocaine, gabapentin, cesarean section, Medicaid, and newborn sex, with mediation analysis by GA.
Result
Methadone was associated with 0.81 cm lower HC (95% CI = −1.22, −0.40) and 0.23 kg lower BW (95% CI = −0.35, −0.10) with approximately 24% and 41% mediated by GA, respectively. Buprenorphine and short acting opioids were not associated with HC or BW.
Conclusion
Methadone exposed newborns have smaller HC and lower BW not fully attributable to younger GA, suggesting a direct effect of methadone on intrauterine growth. Exploration of potential developmental consequences of this is urgently needed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Due to institutional guidelines on data sharing and resource barriers, we are not making our dataset public.
References
Villapiano NL, Winkelman TN, Kozhimannil KB, Davis MM, Patrick SW. Rural and Urban Differences in Neonatal Abstinence Syndrome and Maternal Opioid Use, 2004 to 2013. JAMA Pediatr. 2017;171:194–6.
Minozzi S, Amato L, Jahanfar S, Bellisario C, Ferri M, Davoli M. Maintenance agonist treatments for opiate-dependent pregnant women. Cochrane Database Syst Rev. 2020;11:CD006318.
Jones HE, O’Grady KE, Malfi D, Tuten M. Methadone maintenance vs. methadone taper during pregnancy: maternal and neonatal outcomes. Am J Addict. 2008;17:372–86.
Johnson RE, Jones HE, Fischer G. Use of buprenorphine in pregnancy: patient management and effects on the neonate. Drug Alcohol Depend. 2003;70:S87–101.
McQueen K, Murphy-Oikonen J. Neonatal Abstinence Syndrome. N Engl J Med. 2016;375:2468–79.
Jansson LM, Di Pietro JA, Elko A, Williams EL, Milio L, Velez M. Pregnancies exposed to methadone, methadone and other illicit substances, and poly-drugs without methadone: a comparison of fetal neurobehaviors and infant outcomes. Drug Alcohol Depend. 2012;122:213–9.
Coyle MG, Brogly SB, Ahmed MS, Patrick SW, Jones HE. Neonatal abstinence syndrome. Nat Rev Dis Prim. 2018;4:47.
Hirai AH, Ko JY, Owens PL, Stocks C, Patrick SW. Neonatal Abstinence Syndrome and Maternal Opioid-Related Diagnoses in the US, 2010-2017. JAMA. 2021;325:146–55.
Sirnes E, Oltedal L, Bartsch H, Eide GE, Elgen IB, Aukland SM. Brain morphology in school-aged children with prenatal opioid exposure: A structural MRI study. Early Hum Dev. 2017;106-107:33–9.
Merhar SL, Kline JE, Braimah A, Kline-Fath BM, Tkach JA, Altaye M, et al. Prenatal opioid exposure is associated with smaller brain volumes in multiple regions. Pediatr Res. 2021;90:397–402.
Towers CV, Hyatt BW, Visconti KC, Chernicky L, Chattin K, Fortner KB. Neonatal Head Circumference in Newborns With Neonatal Abstinence Syndrome. Pediatrics. 2019;143. Epub 2018 Dec 10.
Visconti KC, Hennessy KC, Towers CV, Howard BC. Chronic opiate use in pregnancy and newborn head circumference. Am J Perinatol. 2015;32:27–32.
Fill MA, Miller AM, Wilkinson RH, Warren MD, Dunn JR, Schaffner W, et al. Educational Disabilities Among Children Born With Neonatal Abstinence Syndrome. Pediatrics. 2018;142:e20180562.
Patrick SW, Dudley J, Martin PR, Harrell FE, Warren MD, Hartmann KE, et al. Prescription Opioid Epidemic and Infant Outcomes. Pediatrics. 2015;135:842–50.
Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal Abstinence Syndrome and Associated Health Care Expenditures: United States, 2000-2009. JAMA. 2012;307:1934–40.
Lindley AA, Benson JE, Grimes C, Cole TM 3rd, Herman AA. The relationship in neonates between clinically measured head circumference and brain volume estimated from head CT-scans. Early Hum Dev. 1999;56:17–29.
Aagaard K, Bach CC, Henriksen TB, Larsen RT, Matthiesen NB. Head circumference at birth and childhood developmental disorders in a nationwide cohort in Denmark. Paediatr Perinat Epidemiol. 2018;32:458–66.
Gampel SB, Nomura Y. Short and Long-Term Effects of Compromised Birth Weight, Head Circumference, and Apgar Scores on Neuropsychological Development. J Psychol Abnorm Child. 2014;3. Epub 2014 Aug 4.
Piske M, Homayra F, Min JE, Zhou H, Marchand C, Mead A, et al. Opioid Use Disorder and Perinatal Outcomes. Pediatrics. 2021;148. Epub 2021 Sep 3.
Brogly SB, Saia KA, Walley AY, Du HM, Sebastiani P. Prenatal buprenorphine versus methadone exposure and neonatal outcomes: systematic review and meta-analysis. Am J Epidemiol. 2014;180:673–86.
Corsi DJ, Hsu H, Fell DB, Wen SW, Walker M. Association of Maternal Opioid Use in Pregnancy With Adverse Perinatal Outcomes in Ontario, Canada, From 2012 to 2018. JAMA Netw Open 2020;3:e208256.
Miele MJ, Souza RT, Calderon IM, Feitosa FE, Leite DF, Rocha Filho EA, et al. Head circumference as an epigenetic risk factor for maternal nutrition. Front Nutr. 2022;9:867727.
Blair C, Raver CC. Poverty, Stress, and Brain Development: New Directions for Prevention and Intervention. Acad Pediatr. 2016;16:S30–6.
Schempf AH. Illicit Drug Use and Neonatal Outcomes: A Critical Review. Obstetrical Gynecol Surv. 2007;62:749–57.
Maeda A, Bateman BT, Clancy CR, Creanga AA, Leffert LR. Opioid Abuse and Dependence during Pregnancy: Temporal Trends and Obstetrical Outcomes. Anesthesiology. 2014;121:1158–65.
Šimič Klarić A, Tomić Rajić M, Tesari Crnković H. Timing of Head Circumference Measurement in Newborns. Clin Pediatrics. 2014;53:456–9.
Brogly SB, Hahn KA, Diaz SH, Werler M. Confounding of the Comparative Safety of Prenatal Opioid Agonist Therapy. J Addict Res Ther. 2015;6. Epub 2015 Dec 31.
Ahrens KA, McBride CA, O’Connor A, Meyer MC. Medication for Addiction Treatment and Postpartum Health Care Utilization Among Pregnant Persons With Opioid Use Disorder. J Addict Med. 2022;16:56–64.
de Castro A, Jones HE, Johnson RE, Gray TR, Shakleya DM, Huestis MA. Maternal methadone dose, placental methadone concentrations, and neonatal outcomes. Clin Chem. 2011;57:449–58.
Jones HE, Heil SH, Tuten M, Chisolm MS, Foster JM, O’Grady KE, et al. Cigarette smoking in opioid-dependent pregnant women: neonatal and maternal outcomes. Drug Alcohol Depend. 2013;131:271–7.
Cleary BJ, Donnelly J, Strawbridge J, Gallagher PJ, Fahey T, Clarke M, et al. Methadone dose and neonatal abstinence syndrome-systematic review and meta-analysis. Addiction 2010;105:2071–84.
Crocetti MT, Amin DD, Jansson LM. Variability in the evaluation and management of opiate-exposed newborns in Maryland. Clin Pediatr (Philos). 2007;46:632–5.
Patrick SW, Kaplan HC, Passarella M, Davis MM, Lorch SA. Variation in treatment of neonatal abstinence syndrome in US Children’s Hospitals, 2004–2011. J Perinatol. 2014;34:867–72.
Grossman MR, Lipshaw MJ, Osborn RR, Berkwitt AK. A Novel Approach to Assessing Infants With Neonatal Abstinence Syndrome. Hosp Pediatr. 2018;8:1–6.
Allocco E, Melker M, Rojas-Miguez F, Bradley C, Hahn KA, Wachman EM. Comparison of Neonatal Abstinence Syndrome Manifestations in Preterm Versus Term Opioid-Exposed Infants. Adv Neonatal Care. 2016;16:329–36.
Wilcox AJ, Weinberg CR, Basso O. On the pitfalls of adjusting for gestational age at birth. Am J Epidemiol. 2011;174:1062–8.
Jones HE, Kaltenbach K, Heil SH, Stine SM, Coyle MG, Arria AM, et al. Neonatal abstinence syndrome after methadone or buprenorphine exposure. N. Engl J Med. 2010;363:2320–31.
Schmid M, Kuessel L, Klein K, Metz V, Fischer G, Krampl-Bettelheim E. First-trimester fetal heart rate in mothers with opioid addiction. Addiction 2010;105:1265–8.
Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2004;3:CD002207.
Acknowledgements
We acknowledge Kate Ahrens for her significant contribution to study design and Kaitlin Ostrander, Isabel Wolfe, Rebecca Bell and Lilly Watson for their contributions to data collection.
Funding
Funding for this study was received from the Barbara Bush Children’s Health Scholarship Academy for data abstraction.
Author information
Authors and Affiliations
Contributions
AJC carried out all analyses of the data and did the majority of the manuscript writing. AKC, SMBG, and DFC conceptualized and designed this study, coordinated and supervised data collection, provided clinical expertise for appropriate analytical modeling, and reviewed and revised the manuscript. APP provided critical clinical expertise in the review and revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved as exempt research by the Maine Medical Center Institutional Review Board. This study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cutler, A.J., Cox, D.F., Gabrielson, S.M.B. et al. Association of medication-assisted treatment and short acting opioids with newborn head circumference and birth weight. J Perinatol 43, 277–282 (2023). https://doi.org/10.1038/s41372-022-01579-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01579-z
This article is cited by
-
Intrauterine Drug Exposure—What the Pediatrician Needs to Know. Part 1: General Overview, Transplacental Drug Transfer, Teratogenicity, and Fetal Alcohol Spectrum Disorder
Current Treatment Options in Pediatrics (2023)
-
Intrauterine Drug Exposure—What the Pediatrician Needs to Know
Current Treatment Options in Pediatrics (2023)