Abstract
Objective
Determine effect of at least 60 s delayed cord clamping (DCC) on postpartum hemorrhage and maternal estimated blood loss (EBL) in very low birth weight (VLBW) cesarean deliveries when compared to early cord clamping (ECC).
Study design
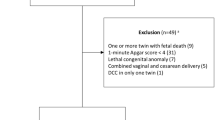
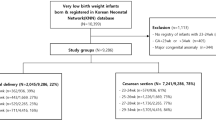
Retrospective study of VLBW infants at birth. Maternal pre- and post-operative hemoglobin, EBL, and neonatal outcomes were collected.
Results
In total, 620 VLBW infants (DCC = 166, ECC = 454) born to 545 mothers (DCC = 155, ECC = 390) were included. Maternal PPH between DCC was 8% versus ECC was 10% p = 0.52. There were no differences in estimated blood loss or rate of maternal blood transfusion between groups. The post-operative hemoglobin was lower in infants receiving ECC compared to DCC (10.4 [9.4–11.5] versus 10.8 [10.1–11.9] g/dl, p = 0.01). In comparing pre-operative to post-operative hemoglobin there was no difference between DCC and ECC (−1.2 [−2.0 to −0.3] versus −1.2 [−2.1 to −0.6] g/dl, p = 0.46).
Conclusion
DCC of at least 60 s did not increase maternal bleeding complications during VLBW cesarean delivery. To our knowledge, this retrospective study is the largest sample size to date of preterm cesarean deliveries to support maternal safety regarding bleeding complications after delayed cord clamping.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
A deidentified dataset is available by written request to the corresponding author.
References
Delayed Umbilical Cord Clamping After Birth. ACOG Committee Opinion, Number 814. Obstet Gynecol. 2020;136:e100–6.
WHO Guidelines Approved by the Guidelines Review Committee. Guideline: delayed umbilical cord clamping for improved maternal and infant health and nutrition outcomes. Geneva: World Health Organization Copyright (© World Health Organization 2014); 2014.
Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2:e323–33.
Practice Bulletin No. 183. Postpartum hemorrhage. Obstet Gynecol. 2017;130:e168–86.
McDonald SJ, Middleton P, Dowswell T, Morris PS. Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes. Cochrane Database Syst Rev. 2013;2013:Cd004074.
Purisch SE, Ananth CV, Arditi B, Mauney L, Ajemian B, Heiderich A, et al. Effect of delayed vs immediate umbilical cord clamping on maternal blood loss in term cesarean delivery: a randomized clinical trial. JAMA. 2019;322:1869–76.
Rabe H, Gyte GM, Díaz-Rossello JL, Duley L. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev. 2019;9:Cd003248.
Fogarty M, Osborn DA, Askie L, Seidler AL, Hunter K, Lui K, et al. Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis. Am J Obstet Gynecol. 2018;218:1–18.
Luthra G, Gawade P, Starikov R, Markenson G. Uterine incision-to-delivery interval and perinatal outcomes in transverse versus vertical incisions in preterm cesarean deliveries. J Matern-Fetal Neonatal Med. 2013;26:1788–91.
Morey SS. ACOG releases report on risk factors, causes and management of postpartum hemorrhage. Am Fam Physician. 1998;58:1002.
Prendiville WJ, Harding JE, Elbourne DR, Stirrat GM. The Bristol third stage trial: active versus physiological management of third stage of labour. BMJ. 1988;297:1295–300.
Callaghan WM, Kuklina EV, Berg CJ. Trends in postpartum hemorrhage: United States, 1994-2006. Am J Obstet Gynecol. 2010;202:353.e1–6.
Begley CM, Gyte GM, Devane D, McGuire W, Weeks A. Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev. 2011:Cd007412. https://doi.org/10.1002/14651858.CD007412.pub3.
Ruangkit C, Leon M, Hassen K, Baker K, Poeltler D, Katheria A. Maternal bleeding complications following early versus delayed umbilical cord clamping in multiple pregnancies. BMC Pregnancy Childbirth. 2018;18:131.
Chiruvolu A, Estes E, Stanzo KC, Desai S, Cornelius BC. The effects of placental transfusion on mothers. J Matern-Fetal Neonatal Med. 2022:1–6. https://doi.org/10.1080/14767058.2022.2032636. Online ahead of print.
Chantry CJ, Blanton A, Taché V, Finta L, Tancredi D. Delayed cord clamping during elective cesarean deliveries: results of a pilot safety trial. Matern Health Neonatol Perinatol. 2018;4:16.
Knol R, Brouwer E, van den Akker T, DeKoninck P, van Geloven N, Polglase GR, et al. Physiological-based cord clamping in very preterm infants—randomised controlled trial on effectiveness of stabilisation. Resuscitation. 2020;147:26–33.
Acknowledgements
ACK was supported by the Cushman Foundation, the Chuck and Ernestina Kreutzkamp Foundation and the Stephen and Lynne Doyle Foundation. We thank the following individuals for their expertise and assistance throughout all aspects of our study: Alexis Rosete, Kaitlyn Fitzgerald, Ana Morales, Elise Mischke, Lukas Linares, Marcie Portillo, and Kathy Arnell.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conceptualization, design, and review of the work. CS substantially contributed to data curation, drafting, and writing manuscript. SAS contributed to data curation and initial manuscript. DMP contributed to data analysis and manuscript revision. ACK co-wrote manuscript and gave final approval of this version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Salcido, C., Shahidi, S.A., Poeltler, D.M. et al. Maternal bleeding complications and neonatal outcomes following early versus delayed umbilical cord clamping in cesarean deliveries for very low birthweight infants. J Perinatol 43, 39–43 (2023). https://doi.org/10.1038/s41372-022-01558-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01558-4