Abstract
Objective
Estimate hospital variation in echocardiography (echo) among very preterm infants.
Study design
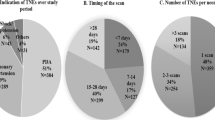
Retrospective cohort study of very preterm (<32 weeks) infants discharged between 2012 and 2019 from US children’s hospitals. Echo exposure was identified using daily billing, and hospital variation was estimated after adjustment for illness severity. Variation in very early echo use (<3 days of life) was compared to exposure to treatment of a patent ductus arteriosus (PDA), and other practice patterns.
Results
27,498 subjects across 39 children’s hospitals were included. Very early echo use had the greatest hospital variation (3–34%). Increasing very early echo use was not associated with PDA treatment (p = 0.93), but was associated with nitric oxide (p < 0.01) and vasoactive medications (p < 0.01).
Conclusions
Hospital variation in echo use among preterm infants was greatest in the first few days of life and was associated with increasing nitric oxide and vasoactive medication use. The impact of this variation on clinical outcomes is uncertain and warrants further investigation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Berwick DM. Avoiding overuse—the next quality frontier. Lancet. 2017;390:102–4.
Goodman DC. Unwarranted Variation in Pediatric Medical Care. Pediatr Clin North Am. 2009;56:745–55.
Wennberg JE. Unwarranted variations in healthcare delivery: implications for academic medical centres. Br Med J. 2002;325:961–4.
Goodman DC, Ganduglia-Cazaban C, Franzini L, Stukel TA, Wasserman JR, Murphy MA, et al. Neonatal Intensive Care Variation in Medicaid-Insured Newborns: a population-based study. J Pediatr. 2019;209:44–51.
Slaughter JL, Stenger MR, Reagan PB. Variation in the use of diuretic therapy for infants with bronchopulmonary dysplasia. Pediatrics. 2013;131:716–23.
Slaughter JL, Stenger MR, Reagan PB, Jadcherla SR. Neonatal Histamine-2 Receptor Antagonist and Proton Pump Inhibitor Treatment at United States Children’s Hospitals. J Pediatr. 2016;174:63–70.
Stenger MR, Slaughter JL, Kelleher K, Shepherd EG, Klebanoff MA, Reagan P, et al. Hospital variation in nitric oxide use for premature infants. Pediatrics. 2012;129:945–51.
Adams M, Bassler D, Bucher HU, Roth-Kleiner M, Berger TM, Braun J, et al. Variability of very low birth weight infant outcome and practice in swiss and US neonatal units. Pediatrics. 2018;141:e20173436.
Alleman BW, Bell EF, Li L, Dagle JM, Smith PB, Ambalavanan N, et al. Individual and center-level factors affecting mortality among extremely low birth weight infants. Pediatrics. 2013;132:e175–84.
Pierrat V, Burguet A, Marchand-Martin L, Cambonie G, Coquelin A, Roze JC, et al. Variations in patterns of care across neonatal units and their associations with outcomes in very preterm infants: the French EPIPAGE-2 cohort study. BMJ Open. 2020;10:e035075.
King BC, Richardson T, Patel RM, Lee HC, Bamat NA, Hall M, et al. Prioritization framework for improving the value of care for very low birth weight and very preterm infants. J Perinatol. 2021;41:2463–73.
King BC, Richardson T, Patel RM, Lee HC, Bamat NA, Patrick SW, et al. Cost of clinician-driven tests and treatments in very low birth weight and/or very preterm infants. J Perinatol. 2020;41:295–304.
Sankar MN, Bhombal S, Benitz WE. PDA: to treat or not to treat. Congenit Heart Dis. 2019;14:46–51.
Soll RF. Inhaled nitric oxide for preterm infants: what can change our practice? Pediatrics. 2018;141:e20174214.
O’Byrne ML, Millenson ME, Grady CB, Huang J, Bamat NA, Munson DA, et al. Trends in transcatheter and operative closure of patent ductus arteriosus in neonatal intensive care units: Analysis of data from the Pediatric Health Information Systems Database. Am Heart J. 2019;217:121–30.
Goodman D, Little G, Harrison W, Moen A, Mowitz M, Ganduglia-Cazaban C. (eds). The Dartmouth Atlas of Neonatal Intensive Care. The Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth, Lebanon, NH, 2019.
EL-Khuffash A, Bussmann N, Breatnach CR, Smith A, Tully E, Griffin J, et al. A Pilot Randomized Controlled Trial of Early Targeted Patent Ductus Arteriosus Treatment Using a Risk Based Severity Score (The PDA RCT). J Pediatr. 2021;229:127–33.
EL-Khuffash A, James AT, Corcoran JD, Dicker P, Franklin O, Elsayed YN, et al. A Patent Ductus Arteriosus Severity Score Predicts Chronic Lung Disease or Death before Discharge. J Pediatr. 2020;167:1354–61.
Rozé JC, Cambonie G, Marchand-Martin L, Gournay V, Durrmeyer X, Durox M, et al. Association between early screening for patent ductus arteriosus and in-hospital mortality among extremely preterm infants. J Am Med Assoc. 2015;313:2441–8.
Demauro SB, Cohen MS, Ratcliffe SJ, Abbasi S, Schmidt B. Serial echocardiography in very preterm infants: a pilot randomized trial. Acta Paediatr Int J Paediatr. 2013;102:1048–53.
Isayama T, Kusuda S, Adams M, Berti E, Battin M, Al E. International Variation in the Management of Patent Ductus Arteriosus and Its Association with Infant Outcomes: a survey and linked cohort study. J Pediatr. 2022;244:24–9.
Bussmann N, Smith A, Breatnach CR, McCallion N, Cleary B, Franklin O, et al. Patent ductus arteriosus shunt elimination results in a reduction in adverse outcomes: a post hoc analysis of the PDA RCT cohort. J Perinatol. 2021;41:127–33.
Hundscheid T, Donders R, Onland W, Kooi EMW, Vijlbrief DC, de Vries WB, et al. Multi-centre, randomised non-inferiority trial of early treatment versus expectant management of patent ductus arteriosus in preterm infants (the BeNeDuctus trial): statistical analysis plan. Trials. 2021;22:1–12.
Bell JL, Gupta S, Juszczak E, Hardy P, Linsell L. Baby-OSCAR: Outcome after Selective early treatment for Closure of patent ductus ARteriosus in preterm babies—a statistical analysis plan for short-term outcomes. Trials. 2021;22:1–13.
De Buyst J, Rakza T, Pennaforte T, Johansson AB, Storme L. Hemodynamic effects of fluid restriction in preterm infants with significant patent ductus arteriosus. J Pediatr. 2012;161:404–8.
Barrington KJ, Finer N, Pennaforte T. Inhaled nitric oxide for respiratory failure in preterm infants. Cochrane Database Syst Rev. 2017;1:CD000509.
Ahmed MS, Giesinger RE, Ibrahim M, Baczynski M, Louis D, McNamara KP, et al. Clinical and echocardiography predictors of response to inhaled nitric oxide in hypoxic preterm neonates. J Paediatr Child Health. 2019;55:753–61.
Papadhima I, Louis D, Purna J, Deshpande P, Diambomba Y, Lee S, et al. Targeted neonatal echocardiography (TNE) consult service in a large tertiary perinatal center in Canada. J Perinatol. 2018;38:1039–45.
Alammary D, Narvey M, Soni R, Elsayed Y, Louis D. Targeted neonatal echocardiography service in neonatal intensive care in Manitoba, Canada. J Perinatol. 2021;42:655–9.
Harabor A, Soraisham AS. Utility of targeted neonatal echocardiography in the management of neonatal illness. J Ultrasound Med. 2015;34:1259–63.
El-Khuffash A, Herbozo C, Jain A, Lapointe A, Mcnamara PJ. Targeted neonatal echocardiography (TnECHO) service in a Canadian neonatal intensive care unit: a 4-year experience. J Perinatol. 2013;33:687–90.
Giesinger RE, Stanford AH, Rios DR, Bhombal S, Fraga MV, Levy VY, et al. Targeted neonatal echocardiography in the United States of America: the contemporary perspective and challenges to implementation. Pediatr Res 2019 857. 2019;85:919–21.
Shwartz M, Young DW, Siegrist R. The ratio of costs to chargees: how good a basis for estimating costs? Inquiry. 1995;32:476–81.
Phibbs CS, Schmitt SK, Cooper M, Gould JB, Lee HC, Profit J, et al. Birth Hospitalization Costs and Days of Care for Mothers and Neonates in California, 2009-11. J Pediatr. 2019;204:118–25.
Russell RB, Green NS, Steiner CA, Meikle S, Howse JL, Poschman K, et al. Cost of hospitalization for preterm and low birth weight infants in the United States. Pediatrics. 2007;120:e1–9.
Hay S, Mowitz M, Dukhovny D, Viner C, Levin J, King B, et al. Unbiasing costs? An appraisal of economic assessment alongside randomized trials in neonatology. Semin Perinatol. 2021;45:151391.
Funding
American Academy of Pediatrics—Marshall Klaus Perinatal Research Award.
Author information
Authors and Affiliations
Contributions
All authors gave final approval of the version to be published. All authors agree to be accountable for all aspects of the work. Conceptualization/design/methodology: BCK, TR, JB, JS, JH. Investigation/formal analysis: BCK, TR, JB, JS, JH. Ppaer drafting: BCK, JS. Paper editing: BCK, TR, JB, JS, JH.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
King, B.C., Hagan, J., Richardson, T. et al. Hospital variation in neonatal echocardiography among very preterm infants at US children’s hospitals. J Perinatol 43, 181–186 (2023). https://doi.org/10.1038/s41372-022-01522-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01522-2
This article is cited by
-
NT-PROBNP as a screening tool for low-risk patent ductus arteriousus: a follow-up validation study
European Journal of Pediatrics (2023)