Abstract
Objective
Describe discrepancies between facilities’ self-reported level of neonatal care and Centers for Disease Control and Prevention Levels of Care Assessment ToolSM (CDC LOCATeSM)-assessed level.
Study design
CDC LOCATeSM data from 765 health facilities in the United States, including 17 states, one territory, one large multi-state hospital system, and one perinatal region within a state, was collected between 2016 and 2021 for this cross-sectional analysis.
Result
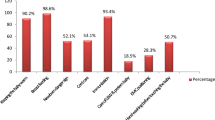
Among 721 facilities that self-reported level of neonatal care, 33.1% had discrepancies between their self-reported level and their LOCATeSM-assessed level. Among facilities with discrepancies, 75.3% self-reported a higher level of neonatal care than their LOCATeSM-assessed level. The most common elements contributing to discrepancies were limited specialty and subspecialty staffing, such as neonatology or neonatal surgery.
Conclusion
Results highlight opportunities for jurisdictions to engage with facilities, health systems, and partners about levels of neonatal care, and to collaborate to promote standardized systems of risk-appropriate care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to data being owned by participating jurisdictions, but are available from the corresponding author on reasonable request.
References
March of Dimes (2011) Toward improving the outcome of pregnancy III: Enhancing perinatal health through quality, safety and performance initiatives. https://www.marchofdimes.org/materials/toward-improving-the-outcome-of-pregnancy-iii.pdf. Accessed 28 May 2021.
Ryan Jr. GM (1975) Toward improving the outcome of pregnancy: Recommendations for the regional development of perinatal health services. Obs Gynecol. 46:375–84.
Little GA, Merenstein GB (1993) Toward improving the outcome of pregnancy, 1993: Perinatal regionalization revisited. Pediatrics 92:
American Academy of Pediatrics. Levels of neonatal care. Pediatrics. 2004;114:1341–7.
American Academy of Pediatrics; Committee on Fetus and Newborn. Levels of neonatal care. Pediatrics. 2012;130:587–97.
AAP Committee on Fetus and Newborn, ACOG Committee on Obstetric Practice (2017) Guidelines for Perinatal Care, 8th Edition.
Lasswell SM, Barfield WD, Rochat RW, Blackmon L. Perinatal regionalization for very low-birth-weight and very preterm infants: A meta-analysis. JAMA. 2010;304:992–1000.
Menard MK, Liu Q, Holgren EA, Sappenfield WM. Neonatal mortality for very low birth weight deliveries in South Carolina by level of hospital perinatal service. Am J Obstet Gynecol. 1998;179:374–81.
Kroelinger CD, Rice ME, Okoroh EM, DeSisto CL, Barfield WD. Seven years later: state neonatal risk-appropriate care policy consistency with the 2012 American Academy of Pediatrics policy. J Perinatol. 2021;42:595–602.
Kroelinger CD, Okoroh EM, Goodman DA, Lasswell SM, Barfield WD. Designation of neonatal levels of care: a review of state regulatory and monitoring policies. J Perinatol. 2020;40:369–76.
Catalano A, Bennett A, Busacker A, Carr A, Goodman D, Kroelinger C, et al. Implementing CDC’s Level of Care Assessment Tool (LOCATe): A national collaboration to improve maternal and child health. J Women’s Health. 2017;26:1265–9.
American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine, Kilpatrick SJ, Menard MK, Zahn CM, Callaghan WM. Obstetric Care Consensus #9: Levels of Maternal Care: (Replaces Obstetric Care Consensus Number 2, February 2015). Am J Obs Gynecol. 2019;221:B19–B30.
Centers for Disease Control and Prevention CDC Levels of Care Assessment Tool (CDC LOCATe). https://www.cdc.gov/reproductivehealth/maternalinfanthealth/cdc-locate/participating-state-success-stories.html. Accessed 21 Dec 2021.
Madni SA, Ewing AC, Beauregard JL, Brantley MD, Menard MK, Goodman DA. CDC LOCATe: Discrepancies between self-reported level of maternal care and LOCATe-assessed level of maternal care among 463 birth facilities. J Perinatol. 2021;42:589–94.
Georgia Department of Public Health Maternal and Neonatal Center Designation Program. https://dph.georgia.gov/maternal-and-neonatal-center. Accessed 7 Apr 2022.
Texas Department of State Health Services Neonatal System Development. https://www.dshs.texas.gov/emstraumasystems/neonatal.aspx. Accessed 11 Jan 2022.
Kattwinkel J, Perlman JM, Aziz K, Colby C, Fairchild K, Gallagher J, et al. Part 15: neonatal resuscitation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010. https://doi.org/10.1161/CIRCULATIONAHA.110.971119.
Ringer SA, Aziz K. Neonatal stabilization and postresuscitation care. Clin Perinatol. 2012;39:901–18.
Schwartz RM, Kellogg R, Muri JH. Specialty newborn care: trends and issues. J Perinatol. 2000;2000 208 20:520–9.
Goodman DC, Fisher ES, Little GA, Stukel TA, Chang CH. Are neonatal intensive care resources located according to need? Regional variation in neonatologists, beds, and low birth weight newborns. Pediatrics. 2001;108:426–31.
Goodman DC, Fisher ES, Little GA, Stukel TA, Chang CH, Schoendorf KC. The relation between the availability of neonatal intensive care and neonatal mortality. N Engl J Med. 2002;346:1538–44.
Van Otterloo LR, Connelly CD. Risk-appropriate care to improve practice and birth outcomes. J Obstet Gynecol Neonatal Nurs. 2018;47:661–72.
Acknowledgements
We want to thank the implementing agencies responsible for CDC LOCATeSM in each jurisdiction that provided CDC LOCATeSM data included in this analysis. Any published findings and conclusions do not necessarily represent the official position of the jurisdictions that participated in CDC LOCATeSM. This project was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between U.S. Department of Energy and the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Contributions
JW conceptualized and designed the work; acquired, analyzed, and interpreted the data; and drafted the manuscript. CD replicated the analysis and revised the manuscript critically for important intellectual content. AE and DG conceptualized and designed the work; acquired the data; and revised the manuscript critically for important intellectual content. SM, JB, and MB revised the manuscript critically for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wilkers, J.L., DeSisto, C.L., Ewing, A.C. et al. Levels of neonatal care among birth facilities in 20 states and other jurisdictions: CDC levels of care assessment toolSM (CDC LOCATeSM). J Perinatol 43, 484–489 (2023). https://doi.org/10.1038/s41372-022-01512-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01512-4
This article is cited by
-
Operationalizing risk-appropriate perinatal care in a rural US State: directions for policy and practice
BMC Health Services Research (2023)
-
Maternal and neonatal risk-appropriate care: gaps, strategies, and areas for further research
Journal of Perinatology (2023)
-
Critical care among newborns with and without a COVID-19 diagnosis, May 2020–February 2022
Journal of Perinatology (2023)