Abstract
Objective
To describe the incidence, trends, management’s variability and short-term outcomes of preterm infants with severe post-hemorrhagic ventricular dilatation (sPHVD).
Methods
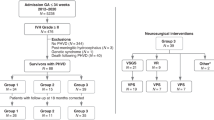
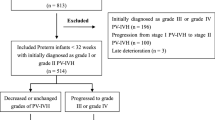
We reviewed infants <33 weeks’ gestation who had PHVD and were admitted to the Canadian Neonatal Network between 2010 and 2018. We compared perinatal characteristics and short-term outcomes between those with sPHVD and those with mild/moderate PHVD and those with and without ventriculo-peritoneal (VP) shunt.
Results
Of 29,417 infants, 2439 (8%) had PHVD; rate increased from 7.3% in 2010 to 9.6% in 2018 (P = 0.005). Among infants with PHVD, sPHVD (19%) and VP shunt (29%) rates varied significantly across Canadian centers and between geographic regions (P < 0.01 and P = 0.0002). On multivariable analysis, sPHVD was associated with greater mortality, seizures and meningitis compared to mild/moderate PHVD.
Conclusions
Significant variability in sPHVD and VP shunt rates exists between centers and regions in Canada. sPHVD was associated with increased mortality and morbidities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Shah PS, Lui K, Sjörs G, Mirea L, Reichman B, Adams M, et al. Neonatal outcomes of very low birth weight and very preterm neonates: an international comparison. J Pediatr. 2016;177:144–52.e6.
Lui K, Lee SK, Kusuda S, Adams M, Vento M, Reichman B, et al. Trends in outcomes for neonates born very preterm and very low birth weight in 11 high-income countries. J Pediatr. 2019;215:32–40.e14.
Leijser LM, de Vries LS. Preterm brain injury: Germinal matrix-intraventricular hemorrhage and post-hemorrhagic ventricular dilatation. Handb Clin Neurol. 2019;162:173–99.
Inder TE, Perlman JM, Volpe JJ. Chapter 24 - Preterm Intraventricular Hemorrhage/Posthemorrhagic Hydrocephalus. In: Volpe JJ, Inder TE, Darras BT, de Vries LS, du Plessis AJ, Neil JJ, et al, editors. Volpe’s Neurology of the Newborn (Sixth Edition). Amsterdam: Elsevier; 2018. 637–98.e21.
Shankaran S, Bajaj M, Natarajan G, Saha S, Pappas A, Davis AS, et al. Outcomes following post-hemorrhagic ventricular dilatation among infants of extremely low gestational age. J Pediatr. 2020;226:36–44.e3.
Adams-Chapman I, Hansen NI, Stoll BJ, Higgins R, Network NR. Neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics. 2008;121:e1167–77.
Radic JA, Vincer M, McNeely PD. Outcomes of intraventricular hemorrhage and posthemorrhagic hydrocephalus in a population-based cohort of very preterm infants born to residents of Nova Scotia from 1993 to 2010. J Neurosurg Pediatr. 2015;15:580–8.
Srinivasakumar P, Limbrick D, Munro R, Mercer D, Rao R, Inder T, et al. Posthemorrhagic ventricular dilatation impact on early neurodevelopmental outcome. Am J Perinatol. 2013;30:207–14.
Christian EA, Jin DL, Attenello F, Wen T, Cen S, Mack WJ, et al. Trends in hospitalization of preterm infants with intraventricular hemorrhage and hydrocephalus in the United States, 2000-2010. J Neurosurg Pediatr. 2016;17:260–9.
Synnes AR, Macnab YC, Qiu Z, Ohlsson A, Gustafson P, Dean CB, et al. Neonatal intensive care unit characteristics affect the incidence of severe intraventricular hemorrhage. Med Care. 2006;44:754–9.
Riva-Cambrin J, Shannon CN, Holubkov R, Whitehead WE, Kulkarni AV, Drake J, et al. Center effect and other factors influencing temporization and shunting of cerebrospinal fluid in preterm infants with intraventricular hemorrhage. J Neurosurg Pediatr. 2012;9:473–81.
Obeid R, Chang T, Bluth E, Forsythe C, Jacobs M, Bulas D, et al. The use of clinical examination and cranial ultrasound in the diagnosis and management of post-hemorrhagic ventricular dilation in extremely premature infants. J Perinatol. 2018;38:374–80.
Brouwer MJ, de Vries LS, Pistorius L, Rademaker KJ, Groenendaal F, Benders MJ. Ultrasound measurements of the lateral ventricles in neonates: why, how and when? A systematic review. Acta Paediatr. 2010;99:1298–306.
Levene MI. Measurement of the growth of the lateral ventricles in preterm infants with real-time ultrasound. Arch Dis Child. 1981;56:900–4.
Davies MW, Swaminathan M, Chuang SL, Betheras FR. Reference ranges for the linear dimensions of the intracranial ventricles in preterm neonates. Arch Dis Child Fetal Neonatal Ed. 2000;82:F218–23.
Reeder JD, Kaude JV, Setzer ES. The occipital horn of the lateral ventricles in premature infants. Ultrasonographic Study Eur J Radio. 1983;3:148–50.
Radhakrishnan R, Brown BP, Kralik SF, Bain D, Persohn S, Territo PR, et al. Frontal occipital and frontal temporal horn ratios: Comparison and validation of head ultrasound-derived indexes with MRI and ventricular volumes in infantile ventriculomegaly. AJR Am J Roentgenol. 2019;213:925–31.
Kennedy CR, Ayers S, Campbell MJ, Elbourne D, Hope P, Johnson A. Randomized, controlled trial of acetazolamide and furosemide in posthemorrhagic ventricular dilation in infancy: follow-up at 1 year. Pediatrics. 2001;108:597–607.
Whitelaw A, Lee-Kelland R. Repeated lumbar or ventricular punctures in newborns with intraventricular haemorrhage. Cochrane Database Syst Rev. 2017;4:CD000216.
Whitelaw A, Jary S, Kmita G, Wroblewska J, Musialik-Swietlinska E, Mandera M, et al. Randomized trial of drainage, irrigation and fibrinolytic therapy for premature infants with posthemorrhagic ventricular dilatation: developmental outcome at 2 years. Pediatrics. 2010;125:e852–8.
Wang JY, Amin AG, Jallo GI, Ahn ES. Ventricular reservoir versus ventriculosubgaleal shunt for posthemorrhagic hydrocephalus in preterm infants: Infection risks and ventriculoperitoneal shunt rate. J Neurosurg Pediatr. 2014;14:447–54.
Mahoney L, Luyt K, Harding D, Odd D. Treatment for post-hemorrhagic ventricular dilatation: A multiple-treatment meta-analysis. Front Pediatr. 2020;8:238.
Lai GY, Chu-Kwan W, Westcott AB, Kulkarni AV, Drake JM, Lam SK. Timing of temporizing neurosurgical treatment in relation to shunting and neurodevelopmental outcomes in posthemorrhagic ventricular dilatation of prematurity: A meta-analysis. J Pediatr. 2021;234:54–64.e20.
Mauer UM, Unterreithmeir L, Jahn A, Wagner W, Kunz U, Schulz C. A survey on current practice in the neurosurgical management of preterm infants with posthemorrhagic hydrocephalus in Germany. J Neurol Surg A Cent Eur Neurosurg. 2013;74:82–6.
Brouwer AJ, Brouwer MJ, Groenendaal F, Benders MJ, Whitelaw A, de Vries LS. European perspective on the diagnosis and treatment of posthaemorrhagic ventricular dilatation. Arch Dis Child Fetal Neonatal Ed. 2012;97:F50–5.
Bassan H, Eshel R, Golan I, Kohelet D, Ben Sira L, Mandel D, et al. Timing of external ventricular drainage and neurodevelopmental outcome in preterm infants with posthemorrhagic hydrocephalus. Eur J Paediatr Neurol. 2012;16:662–70.
Cizmeci MN, Groenendaal F, de Vries LS. Timing of intervention for posthemorrhagic ventricular dilatation: An ongoing debate. J Pediatr. 2021;234:14–6.
Leijser LM, Miller SP, van Wezel-Meijler G, Brouwer AJ, Traubici J, van Haastert IC, et al. Posthemorrhagic ventricular dilatation in preterm infants: When best to intervene? Neurology. 2018;90:e698–e706.
Cizmeci MN, Groenendaal F, Liem KD, van Haastert IC, Benavente-Fernández I, van Straaten HLM, et al. Randomized Controlled Early versus Late Ventricular Intervention Study in Posthemorrhagic Ventricular Dilatation: Outcome at 2 Years. J Pediatr. 2020;226:28–35.e3.
Canadian Neonatal Network Abstractor’s Manual v.3.0.0 2019. 1–94.
Shah PS, Seidlitz W, Chan P, Yeh S, Musrap N, Lee SK, et al. Internal Audit of the Canadian neonatal network data collection system. Am J Perinatol. 2017;34:1241–9.
Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M, et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics 2001;108:E35.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: A study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Ment LR, Bada HS, Barnes P, Grant PE, Hirtz D, Papile LA, et al. Practice parameter: neuroimaging of the neonate: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 2002;58:1726–38.
Grasby DC, Esterman A, Marshall P. Ultrasound grading of cerebral ventricular dilatation in preterm neonates. J Paediatr Child Health. 2003;39:186–90.
Dover DC, Schopflocher DP. Using funnel plots in public health surveillance. Popul Health Metr. 2011;9:58.
Spiegelhalter DJ. Funnel plots for comparing institutional performance. Stat Med. 2005;24:1185–202.
Costeloe KL, Hennessy EM, Haider S, Stacey F, Marlow N, Draper ES. Short term outcomes after extreme preterm birth in England: comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). BMJ. 2012;345:e7976.
Ancel PY, Goffinet F, Kuhn P, Langer B, Matis J, Hernandorena X, et al. Survival and morbidity of preterm children born at 22 through 34 weeks’ gestation in France in 2011: results of the EPIPAGE-2 cohort study. JAMA Pediatr. 2015;169:230–8.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010;443:443–56.
Ahn SY, Shim SY, Sung IK. Intraventricular hemorrhage and post hemorrhagic hydrocephalus among very-low-birth-weight infants in Korea. J Korean Med Sci. 2015;30:S52–8.
Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007;196:147–e1-8.
Klinger G, Osovsky M, Boyko V, Sokolover N, Sirota L, Lerner-Geva L, et al. Risk factors associated with post-hemorrhagic hydrocephalus among very low birth weight infants of 24-28 weeks gestation. J Perinatol. 2016;36:557–63.
Sarkar S, Bhagat I, Dechert R, Schumacher RE, Donn SM. Severe intraventricular hemorrhage in preterm infants: comparison of risk factors and short-term neonatal morbidities between grade 3 and grade 4 intraventricular hemorrhage. Am J Perinatol. 2009;26:419–24.
Brouwer A, Groenendaal F, van Haastert IL, Rademaker K, Hanlo P, de Vries L. Neurodevelopmental outcome of preterm infants with severe intraventricular hemorrhage and therapy for post-hemorrhagic ventricular dilatation. J Pediatr. 2008;152:648–54.
Wellons JC, Shannon CN, Holubkov R, Riva-Cambrin J, Kulkarni AV, Limbrick DD, et al. Shunting outcomes in posthemorrhagic hydrocephalus: results of a Hydrocephalus Clinical Research Network prospective cohort study. J Neurosurg Pediatr. 2017;20:19–29.
Wellons JC, Shannon CN, Kulkarni AV, Simon TD, Riva-Cambrin J, Whitehead WE, et al. Hydrocephalus clinical research network. A multicenter retrospective comparison of conversion from temporary to permanent cerebrospinal fluid diversion in very low birth weight infants with posthemorrhagic hydrocephalus. J Neurosurg Pediatr. 2009;4:50–5.
Christian EA, Melamed EF, Peck E, Krieger MD, McComb JG. Surgical management of hydrocephalus secondary to intraventricular hemorrhage in the preterm infant. J Neurosurg Pediatr. 2016;17:278–84.
Ingram MC, Huguenard AL, Miller BA, Chern JJ. Poor correlation between head circumference and cranial ultrasound findings in premature infants with intraventricular hemorrhage. J Neurosurg Pediatr. 2014;14:184–9.
Acknowledgements
The authors gratefully acknowledge all site investigators and abstractors of the Canadian Neonatal Network (CNN). We thank the staff at the Maternal-infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, Ontario, Canada for organizational support. We also thank Heather McDonald Kinkaid, PhD, a scientific writer at MiCare, for editorial support in preparing this manuscript.
Funding
The project described in this manuscript was conducted with no specific financial support. No honorarium, grant, or other form of payment was given to anyone to produce this manuscript. Organizational support for the Canadian Neonatal Network™ was provided by the Maternal-infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, Ontario, Canada. MiCare is supported by the Canadian Institutes of Health Research (CIHR) (CTP 87518) and Mount Sinai Hospital. PS holds a CIHR Applied Research Chair in Reproductive and Child Health Services and Policy Research (APR-126340).
Author information
Authors and Affiliations
Consortia
Contributions
JA conceptualized and designed the study, drafted the manuscript, and adjusted the manuscript according to the comments of co-authors. WE and PS overviewed the study design and interpretation of data and provided critical revision of the manuscript for important intellectual content. PS and XY had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the analysis. All authors provided review and critical appraisal of the manuscript and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Role of the Study Sponsors: The funders played no role in the design or conduct of the study; the collection, management, analysis, or interpretation of the data; the writing, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Afifi, J., Shah, P.S., Ye, X.Y. et al. Epidemiology of post-hemorrhagic ventricular dilatation in very preterm infants. J Perinatol 42, 1392–1399 (2022). https://doi.org/10.1038/s41372-022-01483-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01483-6