Abstract
Objective
To assess the association between cerebral saturation (crSO2) using Near-Infrared Spectroscopy (NIRS) and brain injury in extremely preterm infants.
Study design
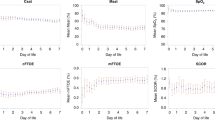
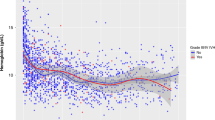
This retrospective study includes 62 infants (<28 weeks gestation) who underwent continuous NIRS monitoring in the first 5 days after birth. Median crSO2 were compared in 12 h increments between infants with and without germinal matrix/intraventricular hemorrhage (GM/IVH). crSO2 was also compared by IVH severity, onset, and by grade of injury on term equivalent MRI.
Results
After 48 h of life (HOL), infants with GM/IVH had significantly lower crSO2 than those without GM/IVH in analysis adjusted for potential confounding e.g., at 49–60 HOL (69.5 (66.2, 72.8) vs. 74.7 (71.8, 77.6), p = 0.023). There were no significant differences in crSO2 by IVH subcategory or injury severity on MRI.
Conclusion
Clinical use of NIRS has the potential to identify crSO2 patterns associated with development of GM/IVH.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bell EF, Hintz SR, Hansen NI, Bann CM, Wyckoff MH, DeMauro SB, et al. Mortality, In-Hospital Morbidity, Care Practices, and 2-Year Outcomes for Extremely Preterm Infants in the US, 2013-2018. JAMA. 2022;327:248–63.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal Outcomes of Extremely Preterm Infants From the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993–2012. JAMA. 2015;314:1039–51.
Gotardo JW, Volkmer NFV, Stangler GP, Dornelles AD, Bohrer BBA, Carvalho CG. Impact of peri-intraventricular haemorrhage and periventricular leukomalacia in the neurodevelopment of preterms: a systematic review and meta-analysis. PLoS ONE. 2019;14:e0223427.
Lin PY, Hagan K, Fenoglio A, Grant PE, Franceschini MA. Reduced cerebral blood flow and oxygen metabolism in extremely preterm neonates with low-grade germinal matrix- intraventricular hemorrhage. Sci Rep. 2016;6:25903.
Inder TE, Perlman JM, Volpe JJ. Chapter 24 - Preterm Intraventricular Hemorrhage/Posthemorrhagic Hydrocephalus. In: Volpe JJ, Inder TE, Darras BT, de Vries LS, du Plessis AJ, Neil JJ, et al. (eds). Volpe’s Neurology of the Newborn. 6th ed. Elsevier; 2018. pp 637–98.e621.
Pryds O. Control of cerebral circulation in the high-risk neonate. Ann Neurol. 1991;30:321–9.
Blankenberg FG, Loh NN, Norbash AM, Craychee JA, Spielman DM, Person BL, et al. Impaired cerebrovascular autoregulation after hypoxic-ischemic injury in extremely low-birth-weight neonates: detection with power and pulsed wave Doppler US. Radiology. 1997;205:563–8.
Lightburn MH, Gauss CH, Williams DK, Kaiser JR. Cerebral blood flow velocities in extremely low birth weight infants with hypotension and infants with normal blood pressure. J Pediatr. 2009;154:824–8.
Soul JS, Hammer PE, Tsuji M, Saul JP, Bassan H, Limperopoulos C, et al. Fluctuating pressure-passivity is common in the cerebral circulation of sick premature infants. Pediatr Res. 2007;61:467–73.
O’Leary H, Gregas MC, Limperopoulos C, Zaretskaya I, Bassan H, Soul JS, et al. Elevated cerebral pressure passivity is associated with prematurity-related intracranial hemorrhage. Pediatrics. 2009;124:302–9.
Meek JH, Tyszczuk L, Elwell CE, Wyatt JS. Low cerebral blood flow is a risk factor for severe intraventricular haemorrhage. Arch Dis Child: Fetal Neonatal Ed. 1999;81:F15–8.
Kluckow M, Evans N. Low superior vena cava flow and intraventricular haemorrhage in preterm infants. Arch Dis Child: Fetal Neonatal Ed. 2000;82:F188–94.
Alderliesten T, Lemmers PMA, Smarius JJM, Van De Vosse RE, Baerts W, Van Bel F. Cerebral oxygenation, extraction, and autoregulation in very preterm infants who develop peri-intraventricular hemorrhage. J Pediatr. 2013;162:698–704.e692
Noori S, McCoy M, Anderson MP, Ramji F, Seri I. Changes in cardiac function and cerebral blood flow in relation to peri/intraventricular hemorrhage in extremely preterm infants. J Pediatr. 2014;164:264–70.e261–3
El-Dib M, Soul JS. Monitoring and management of brain hemodynamics and oxygenation. Handb Clin Neurol. 2019;162:295–314.
Alderliesten T, Dix L, Baerts W, Caicedo A, van Huffel S, Naulaers G, et al. Reference values of regional cerebral oxygen saturation during the first 3 days of life in preterm neonates. Pediatr Res. 2016;79:55–64.
Zhang Y, Chan GS, Tracy MB, Lee QY, Hinder M, Savkin AV, et al. Cerebral near-infrared spectroscopy analysis in preterm infants with intraventricular hemorrhage. Conf Proc: Annu Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Annu Conf. 2011;2011:1937–40.
Katheria AC, Harbert MJ, Nagaraj SB, Arnell K, Poeltler DM, Brown MK, et al. The Neu-Prem Trial: Neuromonitoring of Brains of Infants Born Preterm During Resuscitation-A Prospective Observational Cohort Study. J Pediatr. 2018;198:209. e203
Baik N, Urlesberger B, Schwaberger B, Schmolzer GM, Avian A, Pichler G. Cerebral haemorrhage in preterm neonates: does cerebral regional oxygen saturation during the immediate transition matter? Arch Dis Child-Fetal Neonatal Ed. 2015;100:F422–7.
Verhagen EA, Ter Horst HJ, Keating P, Martijn A, Van Braeckel KNJA, Bos AF. Cerebral oxygenation in preterm infants with germinal matrix- intraventricular hemorrhages. Stroke. 2010;41:2901–7.
Vesoulis ZA, Whitehead HV, Liao SM, Mathur AM. The hidden consequence of intraventricular hemorrhage: persistent cerebral desaturation after IVH in preterm infants. Pediatr Res. 2021;89:869–77.
Sortica da Costa C, Cardim D, Molnar Z, Kelsall W, Ng I, Czosnyka M, et al. Changes in hemodynamics, cerebral oxygenation and cerebrovascular reactivity during the early transitional circulation in preterm infants. Pediatr Res. 2019;86:247–53.
Volpe JJ. Volpe’s neurology of the newborn, Sixth edition. edn. Philadelphia, PA: Elsevier; 2018.
Kidokoro H, Neil JJ, Inder TE. New MR imaging assessment tool to define brain abnormalities in very preterm infants at term. Am J Neuroradiol. 2013;34:2208–14.
Sorensen LC, Maroun LL, Borch K, Lou HC, Greisen G. Neonatal cerebral oxygenation is not linked to foetal vasculitis and predicts intraventricular haemorrhage in preterm infants. Acta Paediatr. 2008;97:1529–34.
Navikiene J, Virsilas E, Vankeviciene R, Liubsys A, Jankauskiene A. Brain and renal oxygenation measured by NIRS related to patent ductus arteriosus in preterm infants: a prospective observational study. BMC Pediatrics. 2021;21:559.
Lemmers PMA, Toet MC, Van Bel F. Impact of patent ductus arteriosus and subsequent therapy with indomethacin on cerebral oxygenation in preterm infants. Pediatrics. 2008;121:142–7.
Poon WB, Tagamolila V. Cerebral perfusion and assessing hemodynamic significance for patent ductus arteriosus using near infrared red spectroscopy in very low birth weight infants. J Matern-fetal neonatal Med: Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet. 2021;34:1645–50.
Evans N, Kluckow M. Early ductal shunting and intraventricular haemorrhage in ventilated preterm infants. Arch Dis Child Fetal Neonatal Ed. 1996;75:F183–6.
Rhee CJ, da Costa CS, Austin T, Brady KM, Czosnyka M, Lee JK. Neonatal cerebrovascular autoregulation. Pediatr Res. 2018;84:602–10.
Goddard Finegold J, Michael LH. Cerebral blood flow and experimental intraventricular hemorrhage. Pediatr Res. 1984;18:7–11.
Tortora D, Lo Russo FM, Severino M, Parodi A, Massirio P, Ramenghi LA, et al. Regional impairment of cortical and deep gray matter perfusion in preterm neonates with low-grade germinal matrix-intraventricular hemorrhage: an ASL study. Neuroradiology. 2020;62:1689–99.
Cimatti AG, Martini S, Galletti S, Vitali F, Aceti A, Frabboni G, et al. Cerebral Oxygenation and Autoregulation in Very Preterm Infants Developing IVH During the Transitional Period: a pilot study. Front Pediatrics. 2020;8:381.
Alderliesten T, van Bel F, van der Aa NE, Steendijk P, van Haastert IC, de Vries LS, et al. Low Cerebral Oxygenation in Preterm Infants Is Associated with Adverse Neurodevelopmental Outcome. J Pediatr. 2019;207:109–16.e102
Pansy J, Baik N, Schwaberger B, Scheuchenegger A, Pichler-Stachl E, Avian A, et al. Cerebral hypoxia during immediate transition after birth and short term neurological outcome. Early Hum Dev. 2017;110:13–5.
Pichler G, Urlesberger B, Baik N, Schwaberger B, Binder-Heschl C, Avian A, et al. Cerebral Oxygen Saturation to Guide Oxygen Delivery in Preterm Neonates for the Immediate Transition after Birth: A 2-Center Randomized Controlled Pilot Feasibility Trial. J Pediatr. 2016;170:73–8.e71-74
Hyttel-Sorensen S, Pellicer A, Alderliesten T, Austin T, Van Bel F, Benders M, et al. Cerebral near infrared spectroscopy oximetry in extremely preterm infants: Phase II randomised clinical trial. BMJ. 2015;350:g7635.
Plomgaard AM, Hagmann C, Alderliesten T, Austin T, van Bel F, Claris O, et al. Brain injury in the international multicenter randomized SafeBoosC phase II feasibility trial: cranial ultrasound and magnetic resonance imaging assessments. Pediatr Res. 2016;79:466–72.
Plomgaard AM, van Oeveren W, Petersen TH, Alderliesten T, Austin T, van Bel F, et al. The SafeBoosC II randomized trial: treatment guided by near-infrared spectroscopy reduces cerebral hypoxia without changing early biomarkers of brain injury. Pediatr Res. 2016;79:528–35.
Pichler G, Baumgartner S, Biermayr M, Dempsey E, Fuchs H, Goos TG, et al. Cerebral regional tissue Oxygen Saturation to Guide Oxygen Delivery in preterm neonates during immediate transition after birth (COSGOD III): an investigator-initiated, randomized, multi-center, multi-national, clinical trial on additional cerebral tissue oxygen saturation monitoring combined with defined treatment guidelines versus standard monitoring and treatment as usual in premature infants during immediate transition: study protocol for a randomized controlled trial. Trials. 2019;20:178.
Hansen ML, Pellicer A, Gluud C, Dempsey E, Mintzer J, Hyttel-Sørensen S, et al. Cerebral near-infrared spectroscopy monitoring versus treatment as usual for extremely preterm infants: a protocol for the SafeBoosC randomised clinical phase III trial. Trials. 2019;20:811.
Author information
Authors and Affiliations
Contributions
MED conceptualized and designed the study, drafted the initial paper, and reviewed and revised the paper. CM participated in research data acquisition, helped to draft the initial paper, and reviewed and revised the paper. JS assisted in data processing, helped to draft the initial paper, and reviewed and revised the paper. SC performed the statistical analyses, helped to draft the initial paper, and reviewed and revised the paper. SL, EH, and TS participated in research data acquisition and reviewed and revised the paper. KB, MAF, and JV provided guidance around the study design, and reviewed and revised the paper. TI helped to conceptualize and design the study and reviewed and revised the paper. All authors approved the final paper as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
MEl-D discloses he is the PI of an investigator-initiated research funded by Medtronic and served once on an advisory board for Radiometer but these are not related to this work. Other authors declare that they have no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
El-Dib, M., Munster, C., Sunwoo, J. et al. Association of early cerebral oxygen saturation and brain injury in extremely preterm infants. J Perinatol 42, 1385–1391 (2022). https://doi.org/10.1038/s41372-022-01447-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01447-w
This article is cited by
-
Three-dimensional cranial ultrasound and functional near-infrared spectroscopy for bedside monitoring of intraventricular hemorrhage in preterm neonates
Scientific Reports (2023)
-
Neuromonitoring in neonatal critical care part II: extremely premature infants and critically ill neonates
Pediatric Research (2023)