Abstract
Objectives
To evaluate variability in antibiotic duration for necrotizing enterocolitis (NEC) and associated clinical outcomes.
Study design
Five-hundred ninety-one infants with NEC (315 medical; 276 surgical) were included from 22 centers participating in Children’s Hospitals Neonatal Consortium (CHNC). Multivariable analyses were used to determine predictors of variability in time to full feeds (TFF) and length of stay (LOS).
Results
Median (IQR) antibiotic duration was 12 (9, 17) days for medical and 17 (14, 21) days for surgical NEC. Wide variability in antibiotic use existed both within and among centers. Duration of antibiotic therapy was associated with longer TFF in both medical (OR 1.04, 95% CI [1.01, 1.05], p < 0.001) and surgical NEC (OR 1.02 [1, 1.03] p = 0.046); and with longer LOS in medical (OR 1.03 [1.02, 1.04], p < 0.001) and surgical NEC (OR 1.01 [1.01, 1.02], p = 0.002).
Conclusion
Antibiotic duration for both medical and surgical NEC remains variable within and among high level NICUs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All data relevant to the study are included in the article. Requests for additional material can be made to IA at iahmad@choc.org.
References
Horbar JD, Carpenter JH, Badger GJ, Kenny MJ, Soll RF, Morrow KA, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics. 2012;129:1019–26.
Johnson TJ, Patel AL, Jegier BJ, Engstrom JL, Meier PP. Cost of morbidities in very low birth weight infants. J Pediatr. 2013;162:243–49.e1.
Yee WH, Soraisham AS, Shah VS, Aziz K, Yoon W, Lee SK, et al. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics. 2012;129:e298–304.
Shulhan J, Dicken B, Hartling L, Larsen BM. Current knowledge of necrotizing enterocolitis in preterm infants and the impact of different types of enteral nutrition products. Adv Nutr. 2017;8:80–91.
Niño DF, Sodhi CP, Hackam DJ. Necrotizing enterocolitis: new insights into pathogenesis and mechanisms. Nat Rev Gastroenterol Hepatol. 2016;13:590–600.
Lin PW, Stoll BJ. Necrotising enterocolitis. Lancet. 2006;368:1271–83.
Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med. 2011;364:255–64.
Neu J, Pammi M. Necrotizing enterocolitis: the intestinal microbiome, metabolome and inflammatory mediators. Semin Fetal Neonatal Med. 2018;23:400–5.
Neu J. Necrotizing enterocolitis: the mystery goes on. Neonatology. 2014;106:289–95.
Blackwood BP, Hunter CJ, Grabowski J. Variability in antibiotic regimens for surgical necrotizing enterocolitis highlights the need for new guidelines. Surg Infect. 2017;18:215–20.
Murphy C, Nair J, Wrotniak B, Polischuk E, Islam S. Antibiotic treatments and patient outcomes in necrotizing enterocolitis. Am J Perinatol. 2020;37:1250–7.
Gibson MK, Crofts TS, Dantas G. Antibiotics and the developing infant gut microbiota and resistome. Curr Opin Microbiol. 2015;27:51–56.
Jasani B, Patole S. Standardized feeding regimen for reducing necrotizing enterocolitis in preterm infants: an updated systematic review. J Perinatol. 2017;37:827–33. https://doi.org/10.1038/jp.2017.37.
Murthy K, Dykes FD, Padula MA, Pallotto EK, Reber KM, Durand DJ, et al. The Children’s Hospitals Neonatal Database: an overview of patient complexity, outcomes and variation in care. J Perinatol. 2014;34:582–6.
Shah D, Sinn JK. Antibiotic regimens for the empirical treatment of newborn infants with necrotising enterocolitis. Cochrane Database Syst Rev. 2012:CD007448. https://doi.org/10.1002/14651858.CD007448.pub2.
Morowitz MJ, Poroyko V, Caplan M, Alverdy J, Liu DC. Redefining the role of intestinal microes in the pathogenesis of necrotizing enterocolitis. Pediatrics. 2010;125:777–85.
Coggins SA, Wynn JL, Weitkamp JH. Infectious causes of necrotizing enterocolitis. Clin Perinatol. 2015;42:133–54.
Bizzarro MJ, Ehrenkranz RA, Gallagher PG. Concurrent bloodstream infections in infants with necrotizing enterocolitis. J Pediatr. 2014;164:61–6.
Clark RH, Gordon P, Walker WM, Laughon M, Smith PB, Spitzer AR. Characteristics of patients who die of necrotizing enterocolitis. J Perinatol. 2012;32:199–204.
Mollitt DL, Tepas JJ, Talbert JL. The microbiology of neonatal peritonitis. Arch Surg. 1988;123:176–9.
Smith B, Bodé S, Petersen BL, Jensen TK, Pipper C, Kloppenborg J, et al. Community analysis of bacteria colonizing intestinal tissue of neonates with necrotizing enterocolitis. BMC Microbiol. 2011;11:73.
Good M, Sodhi CP, Hackam DJ. Evidence-based feeding strategies before and after the development of necrotizing enterocolitis. Expert Rev Clin Immunol. 2014;10:875–84.
Arbra CA, Oprisan A, Wilson DA, Ryan RM, Lesher AP. Time to reintroduction of feeding in infants with nonsurgical necrotizing enterocolitis. J Pediatr Surg. 2018;53:1187–91.
Bohnhorst B, Müller S, Dördelmann M, Peter CS, Petersen C, Poets CF. Early feeding after necrotizing enterocolitis in preterm infants. J Pediatr. 2003;143:484–7.
Brotschi B, Baenziger O, Frey B, Bucher HU, Ersch J. Early enteral feeding in conservatively managed stage II necrotizing enterocolitis is associated with a reduced risk of catheter-related sepsis. J Perinat Med. 2009;37:701–5.
Hock AM, Chen Y, Miyake H, Koike Y, Seo S, Pierro A. Initiation of enteral feeding after necrotizing enterocolitis. Eur J Pediatr Surg. 2018;28:44–50.
Patel EU, Wilson DA, Brennan EA, Lesher AP, Ryan RM. Earlier re-initiation of enteral feeding after necrotizing enterocolitis decreases recurrence or stricture: a systemis review and meta-analysis. J Perinatol. 2020;40:1679–87.
Cheah IGS. Economic assessment of neonatal intensive care. Transl Pediatr. 2019;8:246–56.
Schimpl G, Höllwarth ME, Fotter R, Becker H. Late intestinal strictures following successful treatment of necrotizing enterocolitis. Acta Paediatr Suppl. 1994;396:80–3.
Phad N, Trivedi A, Todd D, Lakkundi A. Intestinal strictures post-necrotising enterocolitis: clinical profile and risk factors. J Neonatal Surg. 2014;3:44.
Schwartz MZ, Hayden CK, Richardson CJ, Tyson KR, Lobe TE. A prospective evaluation of intestinal stenosis following necrotizing enterocolitis. J Pediatr Surg. 1082;17:764–70.
Janik JS, Ein SH, Mancer K. Intestinal stricture after necrotizing enterocolitis. J Pediatr Surg. 1981;16:438–43.
Zhang H, Chen J, Wang Y, Deng C, Li L, Guo C. Predictive factors and clinical practice profile for strictures post-necrotising enterocolitis. Medicine. 2017;96:e6273.
Pammi M, Cope J, Tarr PI, Warner BB, Morrow AL, Mai V, et al. Intestinal dysbiosis in preterm infants preceding necrotizing enterocolitis: a systematic review and meta-analysis. Microbiome. 2017;5:31.
Warner BB, Deych E, Zhou Y, Hall-Moore C, Weinstock GM, Sodergren E, et al. Gut bacteria dysbiosis and necrotising enterocolitis in very low birthweight infants: a prospective case-control study. Lancet. 2016;387:1928–36.
Esaiassen E, Fjalstad JW, Juvet LK, van den Anker JN, Klingenberg C. Antibiotic exposure in neonates and early adverse outcomes: a systematic review and meta-analysis. J Antimicrob Chemother. 2017;72:1858–70.
Cotten CM, Taylor S, Stoll B, Goldberg RN, Hansen NI, Sánchez PJ, et al. Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics. 2009;123:58–66.
Miller J, Tonkin E, Damarell RA, McPhee AJ, Suganuma M, Suganuma H, et al. A systematic review and meta-analysis of human milk feeding and morbidity in very low birth weight infants. Nutrients. 2018;10:707.
Andorsky DJ, Lund DP, Lillehei CW, Jaksic T, Dicanzio J, Richardson DS, et al. Nutritional and other postoperative management of neonates with short bowel syndrome correlates with clinical outcomes. J Pediatr. 2001;139:27–33.
Acknowledgements
Jeanette Asselin, David Durand (ex officio), Francine Dykes (ex officio), Jacquelyn Evans, Karna Murthy (Chair), Michael Padula, Eugenia Pallotto, Theresa Grover, Beverly Brozanski, and Anthony Piazza, Kristina Reber and Billie Short are members of the Children’s Hospitals Neonatal Consortium, Inc. For more information, please contact: support@thechnc.org. We are indebted to the following institutions that serve the infants and their families, and these institutions also have invested in and continue to participate in the Children’s Hospital’s Neonatal Database (CHND). The site sponsors/contributors for the CHND are also included: 1. Children’s Healthcare of Atlanta, Atlanta, GA (Francine Dykes, Anthony Piazza). 2. Children’s Healthcare of Atlanta at Scottish Rite (Gregory Sysyn). 3. Children’s Hospital of Alabama, Birmingham, AL (Carl Coghill, Allison Black). 4. Le Bonheur Children’s Hospital, Memphis, TN (Ramasubbareddy Dhanireddy). 5. Children’s Hospital Boston, Boston, MA (Anne Hansen, Tanzeema Houssain). 6. Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL (Karna Murthy, Gustave Falciglia). 7. Cincinnati Children’s Hospital, Cincinnati, OH (Beth Haberman, Breda Poindexter, Amy Nathan, Kristin Nelson, Paul Kingma, Stefanie Riddle, Stephanie Merhar). 8. Nationwide Children’s Hospital, Columbus, OH (Kristina Reber). 9. Children’s Medical Center, Dallas, TX (Rashmin Savani, Luc Brion, Noorjahan Ali). 10. Children’s Hospital Colorado, Aurora, CO (Theresa Grover). 11. Children’s Hospital of Michigan, Detroit, MI (Girija Natarajan). 12. Cook Children’s Health Care System, Fort Worth, TX (Jonathan Nedrelow, Annie Chi, Yvette Johnson). 13. Texas Children’s Hospital, Houston, TX (Gautham Suresh). 14. Riley Children’s Hospital, Indianapolis, IN (William Engle, Lora Simpson, Gregory Sokol). 15. Children’s Mercy Hospitals & Clinics, Kansas City, MO (Eugenia Pallotto). 16. Arkansas Children’s Hospital, Little Rock, AR (Robert Lyle, Becky Rogers). 17. Children’s Hospital Los Angeles, Los Angeles, CA (Steven Chin, Rachel Chapman). 18. American Family Children’s Hospital, Madison, WI (Jamie Limjoco, Lori Haack). 19. Children’s Hospital & Research Center Oakland, Oakland, CA (David Durand, Jeanette Asselin, Art D’Harlingue, Priscilla Joe). 20. The Children’s Hospital of Philadelphia, Philadelphia, PA (Jacquelyn Evans, Michael Padula, David Munson). 21. Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA (Toby Yanowitz). 22. St. Louis Children’s Hospital, St Louis, MO (Tasmin Najaf, Rakesh Rao). 23. All Children’s Hospital, St. Petersburg, FL (Victor McKay). 24. Rady Children’s Hospital, San Diego, CA (Mark Speziale, Brian Lane, Laural Moyer). 25. Children’s National Medical Center, Washington, DC (Billie Short). 26. AI DuPont Hospital for Children, Wilmington, DE (Kevin Sullivan). 27. Primary Children’s Medical Center, Salt Lake City, UT (Con Yee Ling, Shrena Patel). 28. Children’s Hospital of Wisconsin, Milwaukee, WI (Michael Uhing, Ankur Datta). 29. Children’s Hospital of Omaha (Lynne Willett, Nicole Birge). 30. Florida Hospital for Children (Rajan Wadhawan). 31. Seattle Children’s Hospital, Seattle, WA (Elizabeth Jacobsen-Misbe, Robert DiGeronimo, Zeenia Billimoria). 32. Hospital for Sick Children, Toronto, ON (Kyong-Soon Lee).
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed intellectually to the conception of the study and provided critical inputs during the CHNC NEC work group meetings. IZ conducted data analysis, IA and TY drafted the initial manuscript, and all authors helped revised the manuscript as well as reviewed the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the Children’s Hospitals Neonatal Consortium NEC Focus Group are listed below Acknowledgements.
Rights and permissions
About this article
Cite this article
Ahmad, I., Premkumar, M.H., Hair, A.B. et al. Variability in antibiotic duration for necrotizing enterocolitis and outcomes in a large multicenter cohort. J Perinatol 42, 1458–1464 (2022). https://doi.org/10.1038/s41372-022-01433-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01433-2
This article is cited by
-
Cholestasis is associated with a higher rate of complications in both medical and surgical necrotizing enterocolitis
Journal of Perinatology (2024)
-
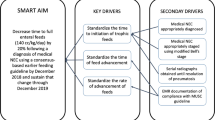
A quality improvement initiative standardizing the antibiotic treatment and feeding practices in patients with medical necrotizing enterocolitis
Journal of Perinatology (2024)